Introduction
During pregnancy, the pyelocaliceal system undergoes
volume changes by pyelocaliceal dilation of approximately 15 mm for
the right kidney and 5 mm for the left kidney (1). Maternal ureterohydronephrosis is one
of the most common anatomical changes during pregnancy. It occurs
in 43-100% of pregnant women, being more evident in the third
trimester (2). Anatomical changes
of the pyelocaliceal system begin in the second month of pregnancy
and can reach a 2-cm dilation. Over 85% of pregnant women have the
right ureter constantly more dilated than the left ureter (3). Some researchers suggest that the
dilation on the right side is caused by mechanical compression due
to an enlarged uterus and the position of the right ureter in
relation with iliac and ovarian vessels. The left ureter has a
greater angle in the pelvic region, which is parallel with pelvic
vessels. This asymmetry in the right and left ureteral dilation
could not be attributed to hormonal changes (3).
The aim of the present study was to evaluate the
stages of UHN during pregnancy, depending on the gestational age,
and to monitor the symptomatology and adequate management. The
study highlighted the existence of an association between
gestational age and UHN grading.
Patients and methods
Patient details
The aim of the present study was to investigate the
relationship between the gestational age, the stage of UHN and
symptomatology, and to evaluate the proper management of this
special condition, mainly in the presence of complications. The
values for gestational age were between 23 and 38 weeks of
pregnancy, with a mean age of pregnancy of 30.98 weeks and standard
deviation of 4.14 weeks.
The study included 58 pregnant women (age range,
16-45 years of age with a mean age of 30.25 years) with UHN
followed for 1 year (January 2017-January 2018), following
hospitalization at the Departments of Nephrology and Obstetrics and
Gynecology of Constanta County Emergency Hospital. Biological (from
blood and urine samples) and imagistic data were collected using
mainly abdominal ultrasonography. Magnetic resonance imaging (MRI)
was performed only in a few, exceptional cases. Some pregnant women
needed reassessments during the same hospitalization due to
association of complications.
The present study was approved by the local Ethics
Commission of Constanta County Emergency Hospital, Romania (no.
3/24.02.2017).
Methods
Information was carefully collected and recorded in
the database, including clinical-biological and imaging data,
diagnosis, therapy approached, gestational age, age of pregnant
women, past medical disease and complications. As an imaging
method, ultrasound (Hitachi-ProSound F37 ultrasound device), which
is a rapid, reliable, accessible diagnostic tool and does not
involve the risk of irradiation for the mother and fetus was
utilized. Information was collected on the size and position of the
kidneys, the degree of hydronephrosis and the echogenicity of the
renal parenchyma. The degree of hydronephrosis was classified as
follows: i) grade I: minimal changes in urinary stasis; ii) grade
II: slight dilation of the renal pelvis involving major calyces;
iii) grade III: moderate dilation of the renal pelvis involving
major and minor calyces; iv) stage IV: severe dilation with
compression on the renal parenchyma (4).
Acute kidney injury (AKI) was defined as oliguria
and an increase in serum creatinine of >0.3 mg/dl in over 48 h
(Kidney Disease Improving Global Outcomes definition).
Statistical analysis
The results of the present study were analyzed with
IBM SPSS Statistics 23 program (IBM Corp.). The procedures used
were descriptive statistics (for characterizing discrete and
continuous variables defined in the database), graphs,
non-parametric statistical tests (Chi-squared test for the
association, the z test to compare two proportions). The
significance level used was α=0.05. A P-value less than α and a
test statistic that falls in the critical region were the reason
for rejecting the null hypothesis in favor of the alternative
hypothesis.
Results
UHN and gestational age
A total of 58 pregnant women presenting with
different degrees of symptomatic UHN were included in the studied
group. Of these, 14 cases (24.14%) were in the second trimester of
pregnancy and 44 (75.86%) in the third trimester of pregnancy.
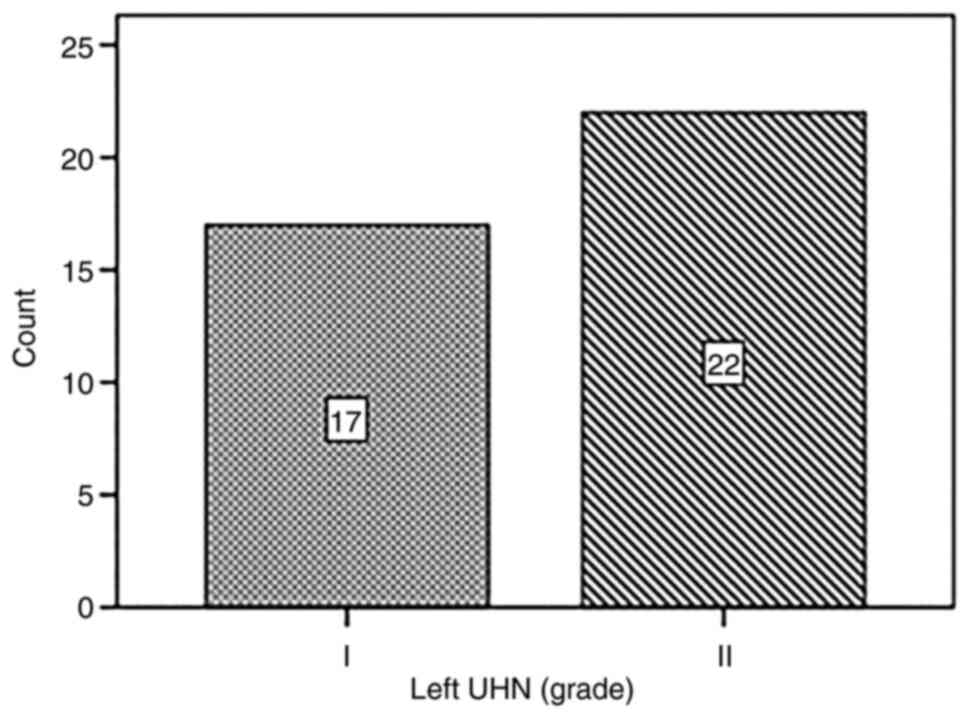
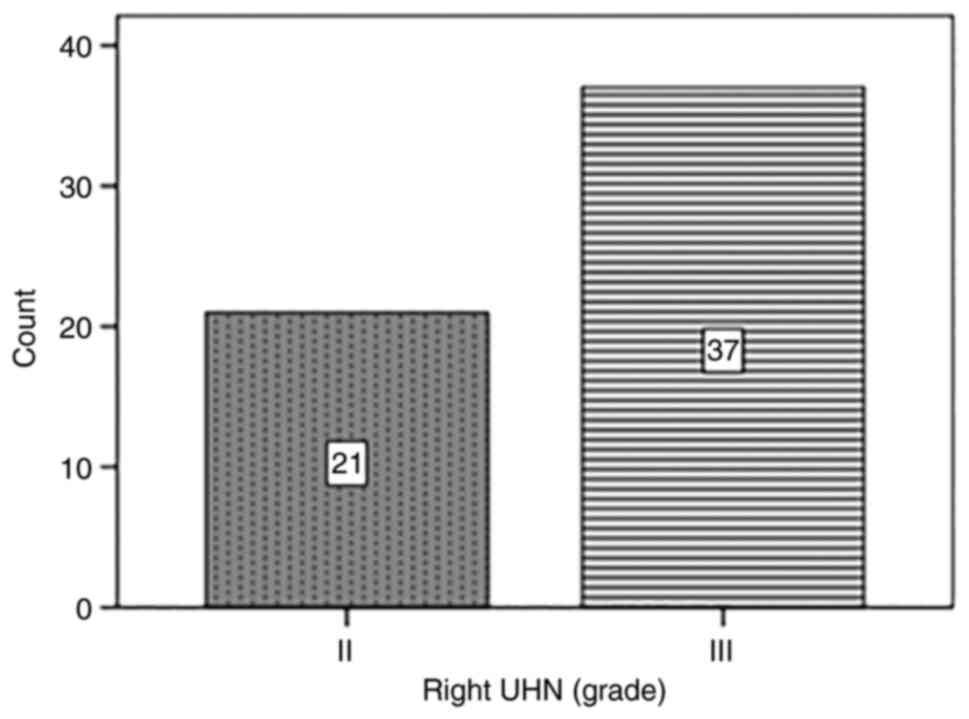
According to the location and grade of UHN, 39 women (67.24%) out
of 58 had left UHN (17 cases with grade I and 22 cases with grade
II) and all 58 women had right UHN (21 cases with grade II and 37
cases grade III). Distribution of the cases with UHN (left/right)
depending on grade (I, II, III) is shown in Figs. 1 and 2.
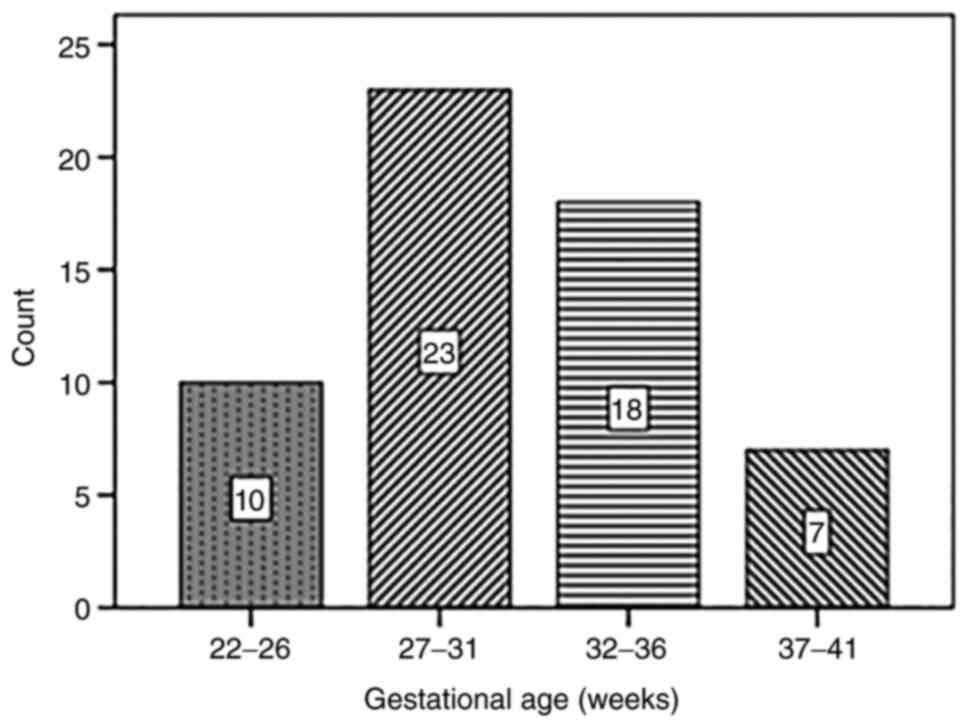
The values for gestational age were between 23 and
38 weeks of pregnancy, with a mean age of pregnancy of 30.98 weeks
and standard deviation of 4.14 weeks. According to gestational age,
10 pregnant women were in the 22- to 26-week group, 23 women in the
27- to 31-week group, 18 women in the 32- to 36-week group and 7
women in the 37- to 41-week group. Distribution of the 58 cases
according to gestational age (weeks) is shown in Fig. 3.
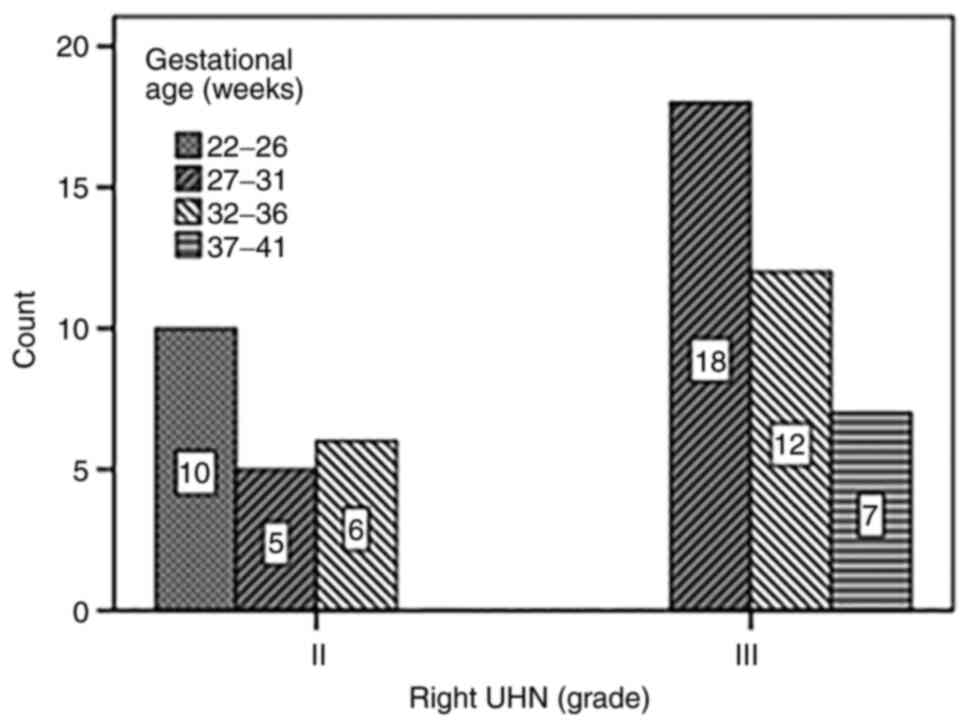
Distribution of pregnant women in the study group
according to the right UHN grade vs. gestational age is presented
in Fig. 4. A significant
association (χ2calc=23.741, df=3, P<0.001
<α=0.05, Chi-squared test for association) was found between the
gestational age and the right UHN grade. From the 58 pregnant women
with right UHN, 21 (36.2%) of them were of right UHN grade (II) and
distributed according to the gestational age as follows: 17.2% (10
pregnant women) in the 22- to 26-week group, 8.6% (5 pregnant
women) in the 27- to 31-week group, and 10.3% (6 pregnant women) in
the 32- to 36-week group. The highest proportion of pregnant women
with right UHN grade (II) was associated with the 22- to 26-week
group (P<0.05) which makes this gestational age interval more
specific for right UHN grade (II). The remaining 37 (63.8%)
pregnant women had right UHN grade (III): 31.0% (18 pregnant women)
in the 27- to 31-week group, 20.7% (12 pregnant women) in the 32-
to 36-week group and 12.1% (7 pregnant women) in the 37- to 41-week
group. As we previously stated, the highest proportion of pregnant
women with right UHN grade (III) was associated with the 27- to
31-week group (P<0.05) which makes this gestational age interval
more specific for right UHN grade (III). These data suggest that
right UHN grade increases with gestational age.
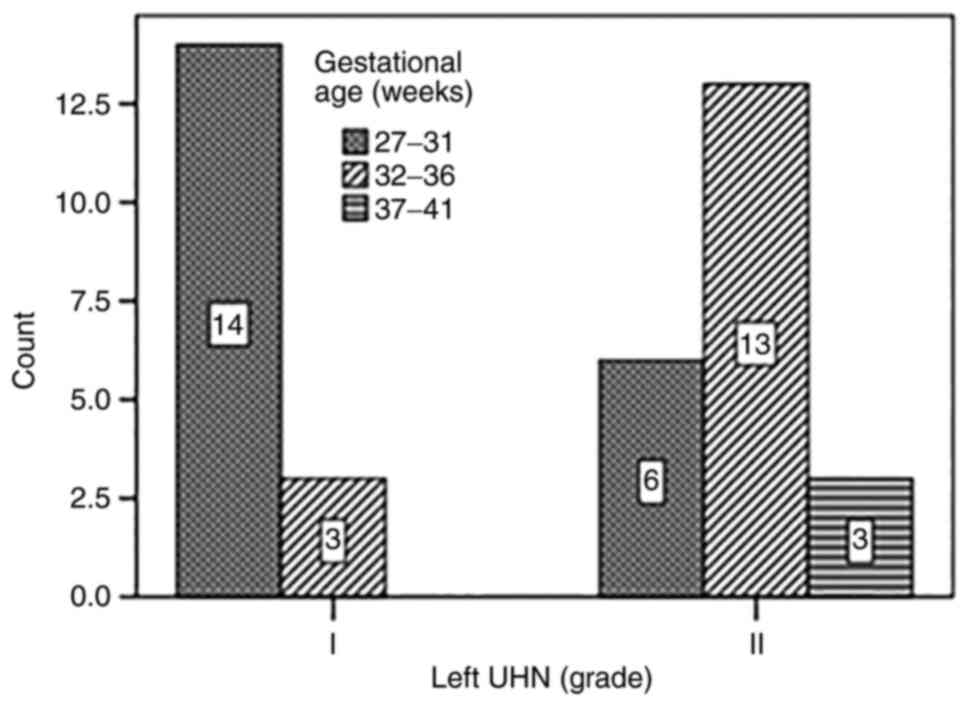
Distribution of pregnant women in the study group
according to the left UHN grade vs. gestational age is presented in
Fig. 5. A significant association
(χ2calc=12.006, df=2, P=0.002 <α=0.05,
CHI-squared test for association) was found between the gestational
age (weeks) and the left UHN grade. From the 39 pregnant women with
left UHN, 17 (43.6%) of them had left UHN grade (I) and were
distributed according to the gestational age as follows: 35.9% (14
pregnant women) in the 27- to 31-week group and 7.7% (3 pregnant
women) in the 32- to 36-week group. The highest proportion of
pregnant women with left UHN grade (I) was associated with the 27-
to 31-week group (P<0.05) which makes this gestational age
interval more specific for left UHN grade (I). The remaining 22
(56.4%) pregnant women had left UHN grade (II): 15.4% (6 pregnant
women) in the 27- to 31-week group, 33.3% (13 pregnant women) in
the 32- to 36-week group and 7.7% (3 pregnant women) in the 27- to
31-week group. As previously stated, the highest proportion of
pregnant women with right UHN grade (II) was associated with the
32- to 36-week group (P<0.05) which makes this gestational age
interval more specific for left UHN grade (II). These data suggest
that left UHN grade increases with gestational age.
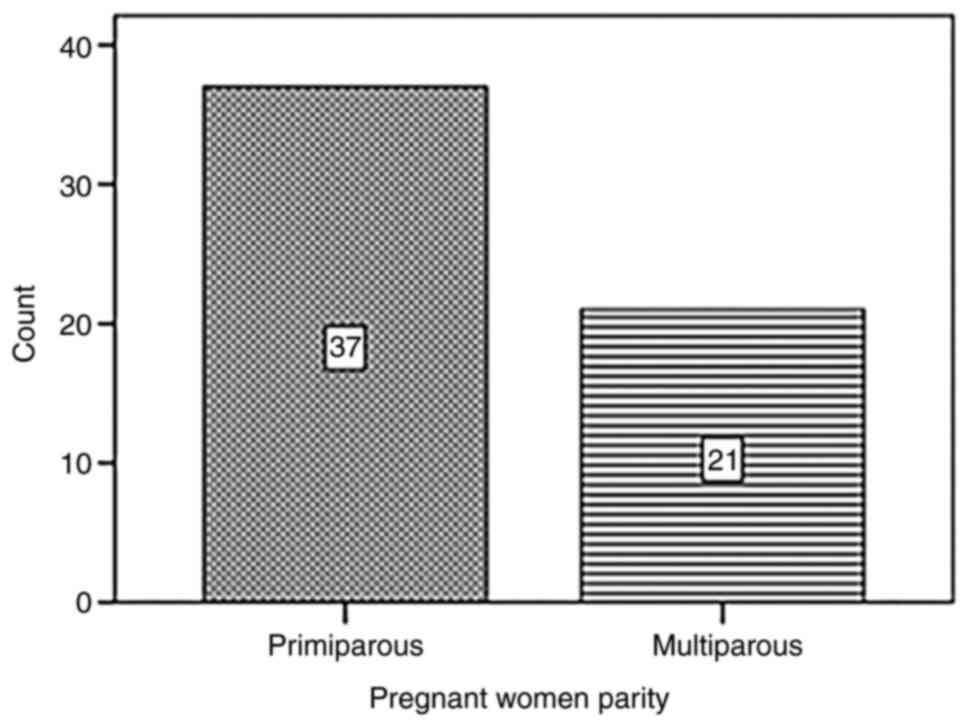
Parity
The distribution of the studied group depending on
parity is shown in Fig. 6. A total
of 37 women (63.79%) were primiparous and 21 (36.21%) were
multiparous.
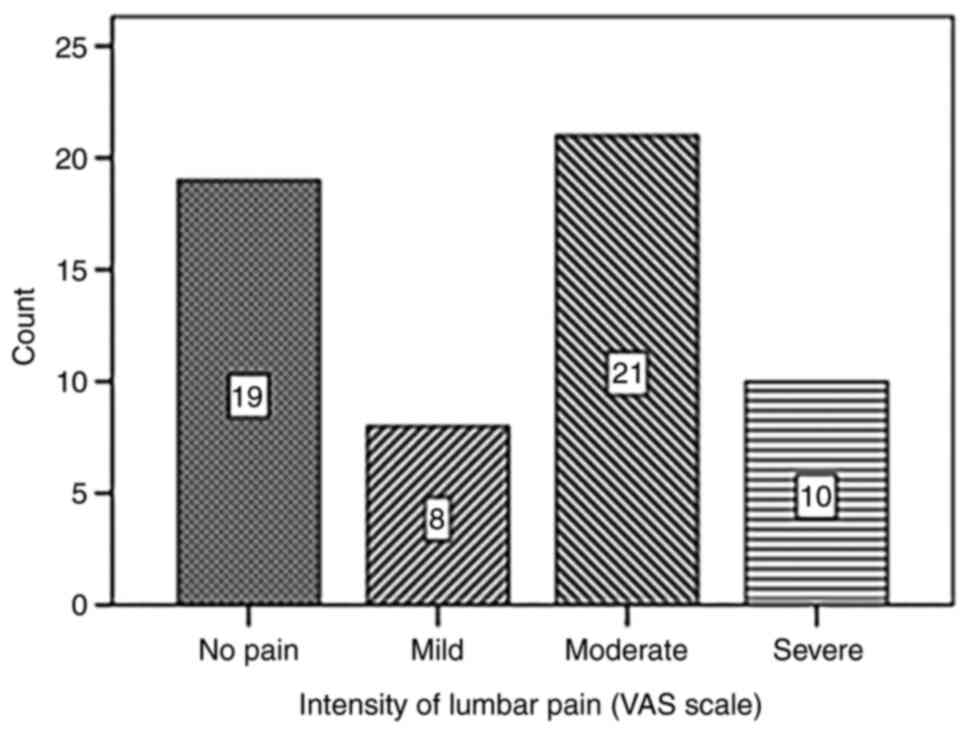
Intensity of lumbar pain
From the 58 pregnant women, 67.24% (39 cases) had
lumbar pain as clinical manifestation and motif of presentation to
the hospital. According to the intensity of lumbar pain: 19% of
women did not complain about lumbar pain, 8 (13.79%) women had mild
lumbar pain, 21 (36.21%) women had moderate lumbar pain and 10
(17.24%) women had severe lumbar pain. Distribution of the studied
group depending on the intensity of lumbar pain (VAS scale) is
shown in Fig. 7.
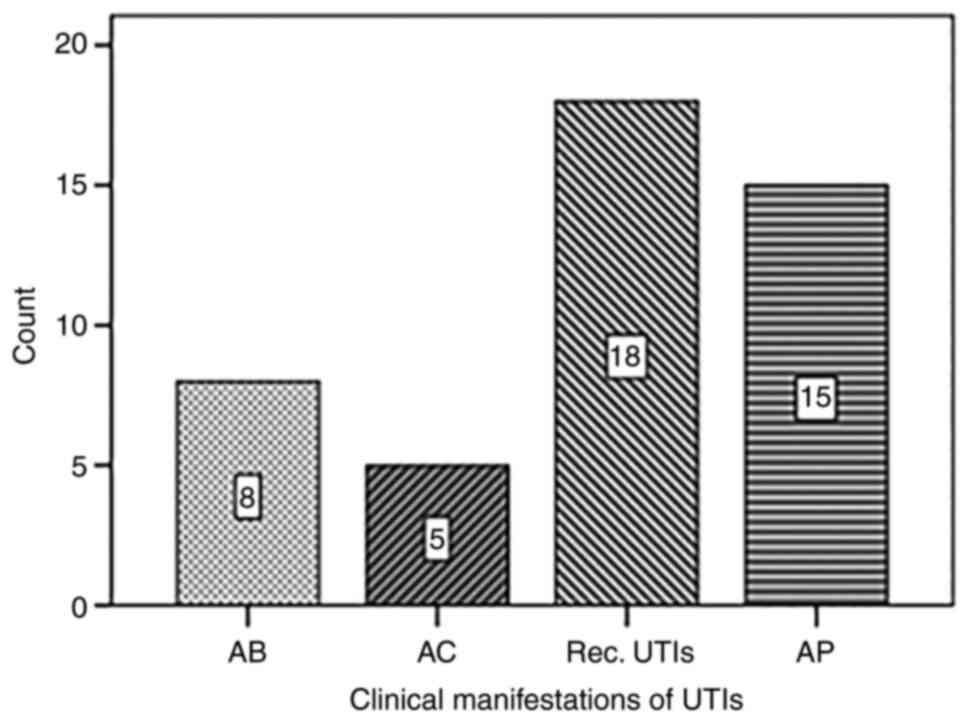
Clinical evolution of UHN
In the studied group, UHN was associated with
complications, including upper urinary tract infection (UTIs)
(79.31%; 46 cases) or acute kidney injury (12.07%; 7 cases).
According to clinical manifestations of UTIs, from the 46 pregnant
women, 8 (13.79%) cases had asymptomatic bacteriuria (AB), 5
(8.62%) cases had acute cystitis (AC), 18 (31.03%) cases had
recurrent urinary tract infections (Rec. UTIs) and 15 (25.86%)
cases had acute pyelonephritis (AP). Depending on clinical
manifestations of the urinary tract infection, pregnant women could
be distributed as shown in Fig.
8.
Therapeutic management
Two patients with AKI recovered after ureteral stent
insertion, 2 after withdrawal of NSAIDs and small doses of
corticosteroids and 3 needed emergency delivery. Conservatory
treatment was administered to all the patients and was represented
by analgesics, antibiotics, adjuvant therapy and hydration.
Additionally, 96.55% (56 cases) of the studied group, responded to
the conservatory therapy and the symptomatology was ameliorated in
those 56 cases, only 2 cases needed ureteral stent insertion.
Discussion
Hydronephrosis is a common anatomical change in the
evolution of pregnancy, occurring in 68-100% of cases of pregnant
women after the 20th week of pregnancy (5-7).
Sometimes, unilateral or bilateral ureterohydronephrosis (UHN) may
be a pathological sign of obstruction due to lithiasis or
inflammatory diseases with stenosis, such as tuberculosis. In the
present study, 58 cases of pregnant women presenting UHN were
included. Depending on the trimester of pregnancy, the frequency
was 24.14% (14 cases) in the second trimester and 74.86% (44 cases)
in the first trimester. No cases of UHN were identified in the
first trimester of pregnancy. These data confirmed the literature
evidence highlighting that UHN is rare in the first part of the
pregnancy, and more frequent in the second and third trimester of
pregnancy (2,5,6,8).
Abdominal ultrasonography is the most common imaging
examination used during pregnancy, offering important information
about kidneys such as anatomical changes, location of UHN, degree
of echogenicity of the renal parenchyma and presence of renal and
ureteral stones. Other imaging methods can be used, such as MRI,
but ultrasound is the most widely used due to the fact there is no
irradiation for mother and fetus, also being a relatively
inexpensive technique, with high availability (9). In the present study, ultrasound
examination was performed in all 58 pregnant women. Right UHN was
present in all pregnant women included in the study, and left UHN
was present in 67.24% (39 cases). These findings confirm the
previously reported data according to which UHN has an increased
frequency in pregnancy, being more predominant on the right side
(1,10-12).
The literature suggests the following physiological
factors responsible for UHN occurrence in pregnancy: i) hormonal
factors: progesterone relaxes the ureteral smooth muscle (3); ii) obstructive factors: extrinsic
ureteral compression, anatomical changes being more obvious on the
right side due to the oblique axis of the uterus, but also because
of the anatomical position of the ureters in the pelvic area
(13); iii) dilated iliac vessels:
enlargement of the uterus leading to compression of the iliac
vessels resulting in their dilation, and ureteral compression
(14); iv) parity: UHN is more
pronounced in primiparous women, possibly due to lax tissue muscle,
which is more developed in multiparous women (15).
The anatomical changes are more obvious on the right
kidney; literature data suggest a frequency of over 85% of the
cases (10,16). In the studied group, it was observed
that right UHN was detected in all 58 cases (100%), compared with
the left UHN (67.24%), or associated with the right UHN in the
studied group. These findings could be due to the dextrorotation of
the pregnant uterus and the compression of the right ureter by the
iliac and ovarian vessels (17).
The right ureter crosses the iliac and ovarian vessels at a
narrower angle in the pelvic area than the angle of left ureter,
which runs parallel to them (14).
Although it is believed that the effect of progesterone in the
smooth muscle relaxation may explain the dilation of the
pyelocaliceal system, this theory cannot explain the asymmetric
dilation of the two uretero-pelvic regions (17,18).
Depending on the side and grade of UHN, frequency of grade III was
63.76% and grade II was 36.21% in the 58 pregnant women with right
UHN; the frequency of grade II was 56.21% and grade I was 43.59% in
39 pregnant women with left UHN. It is observed again that the
right side is more affected, including grade III of UHN, a grade
that is not observed at the left side, with no cases of grade III
described.
Our data suggest that grade of left and right UHN
increased with gestational age, this fact in the literature data
being attributed to the increase of uterine volume, as the
pregnancy progresses. Sala and Rubi in their study (17) also suggested extrinsic compression
as a cause of UHN during pregnancy. Our studied group included UHN
grade I, II or III, there were no cases of grade IV, which is in
agreement with Karabulut et al (9) and Dawood et al (18).
Findings suggest that UHN appears more frequently in
the primiparous pregnant women compared to multiparous pregnant
women (7,19,20).
Analyzing the data from the present study, the frequency of
primiparous was 63.79% (37 pregnant women) and multiparous was
36.21% (21 pregnant women) from a total of 58 patients, which
suggests that primiparous are more susceptible to develop UHN. The
literature does not provide clear explanations for this phenomenon,
but according to author Dwan the renal system of primiparous
pregnant women has less lax muscle tissue than multiparous women
(15). This possible association of
UHN with patient's parity was also described in the study of
Faundes et al. A significant association was found only in
the third trimesters, suggesting that abdominal muscles of
primiparous women are more tonic, which leads to compression of the
ureters (2).
The most common symptom reported in UHN is lumbar
pain on the affected kidney (7).
According to the VAS scale, in our studied group 19% were
asymptomatic, 13.79% had mild pain, 36.21% moderate pain and 17.24%
had severe lumbar pain. From the 58 pregnant women, 79.31% (46
cases) were complicated with urinary tract infections (UTI) with
different clinical manifestations. The most frequent clinical
manifestation was recurrent UTIs (31.03%; 18 cases) followed by
acute pyelonephritis (25.86%; 15 cases). There were also
asymptomatic bacteriuria (13.79%; 8 cases) and acute cystitis
(8.62%; 5 cases). Acute pyelonephritis and recurrent urinary tract
infections are the most frequent clinical manifestations associated
with UHN described in the literature during pregnancy (7,21,22).
Symptomatic UHN may also be associated with acute renal
insufficiency or ureteral stones as complications of this condition
(21,23). In the present study, we found 8
(13.79%) pregnant women with ureteral lithiasis and 7 (12.07%)
pregnant women with acute kidney insufficiency (AKI), as
complications of UHN.
The majority of cases of symptomatic UHN during
pregnancy have a positive response on conservative treatment, only
10% requiring urological surgery with stent insertion due to
significant lumbar pain (7). Among
the studied group 96.55% (56 cases) of the studied group, responded
to analgesic therapy, antibiotics and hydration, supporting
existing data from the literature. Improvement occurs within 2-3
days after starting the treatment (7,21). If
no improvement is evident, urological surgery with stent insertion
under spinal anesthesia with cystoscopic guidance or Cesarean
delivery if the fetal development condition allows (23,24).
From the studied group, only 2 pregnant women (3.45%) with severe
lumbar pain needed stent insertion, which ameliorated the
symptomatology that initially did not respond to conservatory
treatment. Once the ureteral stent is inserted, it can be left in
position for 20 weeks and removed after birth (25). The ureteral stent is usually well
tolerated by pregnant women; there are only few cases that require
their removal due to complications such recurrent infections or
pelvic pain (25). The 2 cases of
pregnant women with UHN and stent insertion did not have severe
complications, such as urosepsis, the ureteral stents being removed
immediately after delivery.
Abdominal ultrasonography has limits in detecting
ureteral anatomical changes, especially in obese pregnant women
with abdominal meteorism, which can lead to kidney image
misinterpretation. CT scan has a 100% specificity for visualizing
kidney stones in all areas of the urinary tract, but in pregnant
women cannot be used because of its maternal and fetal risks. MRI
does not use ionizing radiation like CT scan and has lower accuracy
in detecting small stones (26).
The limitation of the present study was the use of ultrasound in
all 58 cases, and no MRI investigations in order to have a more
clear etiology of urinary tract obstruction in selected cases
(uterine compression/kidney stones).
Another limitation of the present study was the
non-homogeneous collection of used data registration, because we
had to register mixed data, obtained from medical files of
hospitalizations of pregnant women, combined with electronical
documents from the ‘Constanta County Emergency Hospital’ and/or
other laboratories and private hospitals where patients were
checked before. In these situations, some data could be omitted,
leading to underestimation of some complications such as urinary
tract infection or spontaneous elimination of kidney stones.
In summary, ureterohydronephrosis is a common
anatomical change in pregnancy and is dependent on the gestational
age, but could be a pathological condition, associated with the
ureteral migration of renal stones. The grade of right or left UHN
increases progressively with gestational age. Parity influences the
development of UHN; primiparous pregnant women are more susceptible
to develop a more severe grade of UHN. The most common symptom of
hydronephrosis during pregnancy is lumbar pain, which can have
different types of intensity (usually moderate to severe). UHN may
be complicated with lower or upper urinary tract infection, or even
with acute renal insufficiency, a situation that requires urgent,
appropriate management. Ureteral stone can be another complication
and requires a different approach. Conservatory treatment during
symptomatic and complicated UHN is efficient in most cases,
otherwise urological interventions with ureteral stent insertion
must be initiated, as these treatments are effective and safe both
for mother and child.
Acknowledgements
This work was supported by the project
ANTREPRENORDOC, in the framework of Human Resources Development
Operational Programme 2014-2020.
Funding
The study was financed by the European Social Fund under the
contract number 36355/23.05.2019 HRD OP/380/6/13-SMIS Code:
123847.
Availability of data and materials
Data used in the current original study were
obtained from patient archive files at Constanta County Emergency
Hospital, Romania. Any further information regarding the present
study is available from the corresponding author upon reasonable
request.
Authors' contributions
EC established the design of the study and collected
data from patients included in the study. AMPC and LCP contributed
to the analysis and interpretation of the data and performed the
statistics. AMPC was involved in the drafting of the manuscript. EC
and LAT contributed to analysis and writing of the Results and
Discussion sections including the literature data and translated it
and prepared for publishing. LAT and LCP confirm the authenticity
of data. EC, LAT, AMPC and LCP read and approved the final
manuscript.
Ethics approval and consent to
participate
The data of the present study were approved by the
local Ethics Commission of Constanta County Emergency Hospital,
Romania (no. 3/24.02.2017).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fried AM, Woodring JH and Thompson DJ:
Hydronephrosis of pregnancy: A prospective sequential study of the
course of dilatation. J Ultrasound Med. 2:255–259. 1983.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Faundes A, Bricola-Filho M and Pinto e
Silva JL: Dilatation of the urinary tract during pregnancy:
Proposal of a curve of maximal caliceal diameter by gestational
age. Am J Obstet Gynecol. 178:1082–1086. 1998.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Schulman A and Herlinger H: Urinary tract
dilatation in pregnancy. Br J Radiol. 48:638–645. 1975.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Onen A: Grading of hydronephrosis: An
ongoing challenge. Front Pediatr. 8(458)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Meares EM Jr: Urologic surgery during
pregnancy. Clin Obstet Gynecol. 21:907–920. 1978.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Fainstat T: Ureteral dilatation in
pregnancy: A review. Obstet Gynecol Surv. 18:845–860.
1963.PubMed/NCBI
|
|
7
|
Puškar D, Balagović I, Filipović A,
Knezović N, Kopjar M, Huis M and Gilja I: Symptomatic physiologic
hydronephrosis in pregnancy: Incidence, complications and
treatment. Eur Urol. 39:260–263. 2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
The S and Chan L: OP21.05: Pelvicalyceal
dilatation in maternal kidneys during normal pregnancy-an uncommon
finding? Ultrasound Obstet Gynecol. 30:529. 2007.
|
|
9
|
Karabulut N, Baki Yaǧci A and Karabulut A:
Renal vein Doppler ultrasound of maternal kidneys in normal second
and third trimester pregnancy. Br J Radiol. 76:444–447.
2003.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Peake SL, Roxburgh HB and Langlois SL:
Ultrasonic assessment of hydronephrosis of pregnancy. Radiology.
146:167–170. 1983.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Cietak KA and Newton JR: Serial
qualitative maternal nephrosonography in pregnancy. Br J Radiol.
58:399–404. 1985.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ciciu E, Pașatu-Cornea AM and Tuta LA:
Mo117 the impact of gestational age on anatomical and physiological
changes of the upper urinary tract during pregnancy. Nephrol
Dialysis Transplantation: May 29, 2021 (Epub ahead of print).
|
|
13
|
Rasmussen PE and Nielsen FR:
Hydronephrosis during pregnancy: A literature survey. Eur J Obstet
Gynecol Reprod Biol. 27:249–259. 1988.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Cheung KL and Lafayette RA: Renal
physiology of pregnancy. Adv Chronic Kidney Dis. 20:209–214.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Dawn CS: Textbook of Obestetrics and
Neonatology. 11th edition. Pratap Medical Publishers, New Delhi,
1995.
|
|
16
|
Schneider DH, Eichner E and Gordon MB: An
attempt at production of hydronephrosis of pregnancy, artificially
induced. Am J Obstet Gynecol. 65:660–665. 1953.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sala NL and Rubí RA: Ureteral function in
pregnant women. II. Ureteral contractility during normal pregnancy.
Am J Obstet Gynecol. 99:228–236. 1967.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Dawood S, Amin S and ShekhMuhammed S:
Sonographic evaluation of maternal kidneys in normal pregnancy.
Zanco J Med Sci. 19:880–885. 2015.
|
|
19
|
Eckford SD and Gingell JC: Ureteric
obstruction in pregnancy-diagnosis and management. Br J Obstet
Gynaecol. 98:1137–1140. 1991.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zwergel T, Lindenmeir T and Wullich B:
Management of acute hydronephrosis in pregnancy by ureteral
stenting. Eur Urol. 29:292–297. 1996.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Tsai YL, Seow KM, Yieh CH, Chong KM, Hwang
JL, Lin YH and Huang LW: Comparative study of conservative and
surgical management for symptomatic moderate and severe
hydronephrosis in pregnancy: A prospective randomized study. Acta
Obstet Gynecol Scand. 86:1047–1050. 2007.PubMed/NCBI View Article : Google Scholar
|
|
22
|
McGready R, Wuthiekanun V, Ashley EA, Tan
SO, Pimanpaanrak M, Viladpai-Nguen SJ, Jesadapanpong W, Blacksell
SD, Proux S, Day NP, et al: Diagnostic and treatment difficulties
of pyelonephritis in pregnancy in resource-limited settings. Am J
Trop Med Hyg. 83:1322–1329. 2010.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Rosenberg E, Sergienko R, Abu-Ghanem S,
Wiznitzer A, Romanowsky I, Neulander EZ and Sheiner E:
Nephrolithiasis during pregnancy: Characteristics, complications,
and pregnancy outcome. World J Urol. 29:743–747. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Çeçen K and Ülker K: The comparison of
double J stent insertion and conservative treatment alone in severe
pure gestational hydronephrosis: A case controlled clinical study.
ScientificWorldJournal. 2014(989173)2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Haleblian G, Kijvikai K, de La Rosette J
and Preminger G: Ureteral stenting and urinary stone management: A
systematic review. J Urol. 179:424–430. 2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
MacNeily AE, Goldenberg SL, Allen GJ,
Ajzen SA and Cooperberg PL: Sonographic visualization of the ureter
in pregnancy. J Urol. 146:298–301. 1991.PubMed/NCBI View Article : Google Scholar
|