Introduction
According to the World Health Organization (WHO),
5.8 million people die each year as a result of injuries, being
responsible for 10% of the world's mortality (1). Despite the burden, there are
disparities, globally, regarding trauma care (2).
Liver trauma is not an uncommon lesion with
life-threatening potential in trauma patients, which can be managed
with either operative or non-operative strategy, according to the
severity, patient characteristics and trauma mechanism (3,4).
An increased non-surgical approach has been noted
(5). However, the management is
challenged by the lack of definitive studies and by the worldwide
heterogeneity (6). Therapy
management is difficult, being complicated by the risk of
hemorrhagic shock, liver failure, sepsis and organ dysfunction. The
decision is to be made by a multidisciplinary team able to deal
with a complex patient: intensive care unit (ICU) specialists,
surgeons of different specialties, interventional radiologist in
specialized tertiary center. Usually, these complex patients are
managed according to local logistics and personnel resources, being
addressed either in specialized trauma centers, but also in county
hospitals in accordance with the clinical status or transport
availability. When considered appropriate, these patients are
transferred to a hepatic center (7).
The objective of this study was to analyze the
outcomes of the patients with post-traumatic liver injury requiring
secondary ICU hospitalization in a non-emergency liver center from
Romania after initial stabilization in county hospitals.
Patients and methods
Study design and data collection
This study is a monocentric, retrospective,
observational study, designed in a clinical center for
hepatobiliary surgery. Patients with hepatic trauma after car
accident, admitted between 2015 and 2019, were included. The data
were collected using the electronic medical record as the patients'
paper charts. There were 5 females and 7 males with a mean age of
27 years and a mean body mass index (BMI) of 23.1
kg/m2.
The following variables were noted: age, sex,
intubation status at admission, Acute Physiology and Chronic Health
Evaluation (APACHE) II score at admission, BMI, trauma-admission
time, admission-surgery time, surgical procedure before transfer
(in the primary hospital), injury severity score (ISS),
Sepsis-related Organ Failure Assessment (SOFA) at 24, 48 and 72 h
postadmission respectively, norepinephrine (NE) infusion rate at
admission, and postoperatively, the need for continuous veno-venous
hemodiafiltration (CVVHDF), preoperative standard blood analysis,
thromboelastographic analysis before, during and after surgery,
perioperative lactate dynamics, need of preoperative transfusion,
if reintervention was needed, type of surgery, duration of surgery,
blood products needed during and after surgery, hours of mechanical
ventilation cumulated during the ICU admission, and the length of
ICU stay.
The standard blood analysis consisted of: full blood
cell count, liver enzymes, urea nitrogen (BUN), creatinine, total
bilirubin (TB), fibrinogen, thromboelastographic parameters. We
considered the following surgery types: demeshing (after successful
meshing in primary hospitals, where they were initially admitted),
partial liver resection, or partial liver resection with
supplementary surgical procedures to other abdominal or thoracic
organs.
We considered blood products and antifibrinolytics
administered during ICU stay and included separately all of the
following: erythrocyte concentrate, fresh frozen plasma (FFP),
platelet concentrate (PC), fibrinogen, and tranexamic acid.
Ethic statement
All clinical procedures were carried out with the
approval of the local Ethics Committee of ‘Fundeni’ Clinical
Institute (Romania) for clinical trials in accordance with the
European Communities Council Directive 2001/20/EC and with respect
to personal data privacy, European Directive 95/46/EC. Written
informed consent was obtained from all patients prior to
publication.
Data analysis
Data analysis and graphical representations were
performed using GraphPad Prism 6.00 (GraphPad Software Inc.).
For the correlative data, we used a linear
correlation model, between the number of hospitalization days as
outcome variable and all other variables as independent variables.
The Spearman correlation coefficient, r, was determined. We stated
a r value between -0.3 and 0.3 to have negligible correlative
effect.
Furthermore, for the qualitative independent
variables, which influenced statistically significantly the number
of hospitalization days, we compared the median of the
hospitalization days between groups (with or without the specified
independent variable) using Mann-Whitney test analysis after
assessing the groups for normal distribution using histograms, D'
Agostino-Pearson omnibus normality test and Shapiro-Wilk test. A
two-sided P-value <0.05 was considered statistically
significant.
Results
A total of 12 patients were enrolled and 11 were
included in the analysis, considering that for 1 patient the data
collection was incomplete.
Correlations between the length of ICU
stay and the independent variables considered
The length of ICU hospitalization was found to
depend mainly on intubation status at admission [rho (r)=0.6992,
P=0.0303], the cumulative number of mechanical ventilation hours
(r=0.6713, P=0.0273), preoperative fibrinogen values (r=0.7301,
P=0.0208) and the NE intraoperative use (r=0.8157, P=0.0087). The
Spearman correlation coefficient, rho, and P-value for each
correlation between the length of ICU hospitalization and those
independent variables considered to have a potential correlative
effect (Spearman correlation coefficient outside the interval
-0.3-0.3) are documented in Table
I.
 | Table ICorrelations between the length of ICU
stay and the independent variables considered. |
Table I
Correlations between the length of ICU
stay and the independent variables considered.
| Characteristics | Rho (r) | P-value |
|---|
| Duration of
mechanical ventilation (h) | 0.6713 | 0.0273 |
| Trauma admission
time | -0.3936 | 0.2937 |
| Admission-surgery
time | -0.3929 | 0.2889 |
| ISS | 0.5576 | 0.0786 |
| SOFA (admission) | 0.3733 | 0.2574 |
| SOFA (72 h after
admission) | 0.3801 | 0.2787 |
| Intubation
status | 0.6992 | 0.0303 |
| Hgb | 0.3262 | 0.3561 |
| Platelet count | 0.5338 | 0.1184 |
| Fibrinogen | 0.7301 | 0.0208 |
| INR | -0.3497 | 0.3251 |
| CT fib | -0.3172 | 0.4554 |
| Lactate at
admission | -0.4356 | 0.2123 |
| Transfusion on
admission | -0.3619 | 0.3061 |
| Revision surgery | 0.3016 | 0.4121 |
| PC transfusion | 0.6292 | 0.1071 |
| NE intraoperative
use | 0.8157 | 0.0087 |
| CVVHDF | 0.5238 | 0.1556 |
| Postoperative
transfusion | 0.5036 | 0.1762 |
| ASA | 0.3304 | 0.3245 |
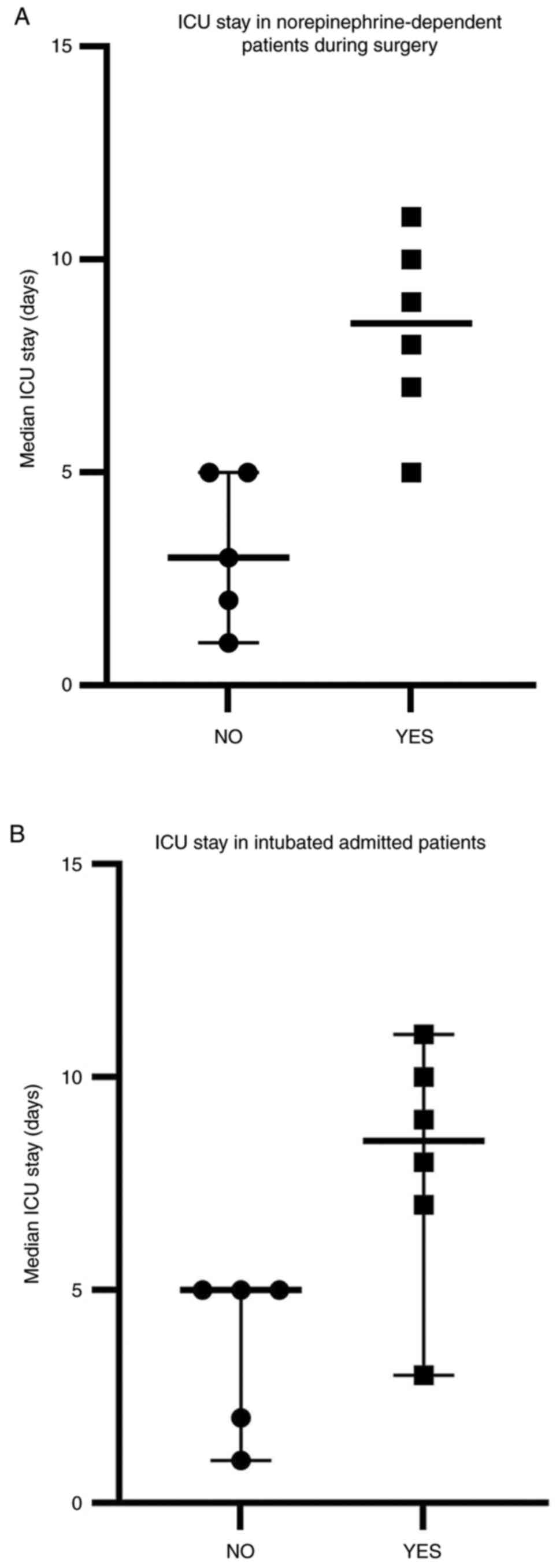
Comparative analysis of the length of
ICU stay considering the intubation status at admission and the use
of NE intraoperatively
The median hospitalization days was increased in
admitted intubated patients and in patients who received NE during
surgery (r=0.81, P=0.0087) (Table
I). The data are represented in Fig. 1. The graphs represent the ranks,
median and 95% CI of the groups. The median ICU stay in patients
with no NE during surgery was 3 days (95% CI: 2.14-6.65) compared
with those patients, who needed NE during surgery: 8 days (95% CI:
4.9-23.1) (Fig. 1A). The median ICU
stay in non-intubated patients at admission was 5 days (95% CI:
2.18-7.02), while for those intubated at admission was 8 days (95%
CI: 4.53-23.14) (Fig. 1B).
Discussion
The analysis included all the patients treated after
initial stabilization in a highly specialized center from Eastern
Europe. The small number of patients precluded any inference about
mortality. Thus, we used as the main outcome, the length of ICU
stay. According to the literature, there are various major risk
factors associated with mortality in this clinical setting:
multiple trauma, extra-abdominal lesions, initial systolic blood
pressure, initial base deficit, the Glasgow Coma Scale, injury
type, number of resected segments, and intraoperative blood loss
(8).
We observed that patients, who needed intraoperative
vasopressors, had a longer ICU stay, despite the fact that no
patient needed norepinephrine after the surgical procedure,
probably a marker of severity.
The use of vasopressors is a straight-forward
decision in patients with profound hypotension in order to maintain
an adequate perfusion pressure in vital organs (9,10).
Their use should be, however, timely-limited until the main cause
is identified and treated. In accordance with advanced trauma life
support management, the use of vasopressors (especially
norepinephrine) in the early stage of trauma could be deleterious
(11). Fluid resuscitation should
be prioritized in order to maintain the main blood pressure in
hemorrhagic shock. The extensive use of vasopressors
intraoperatively impairs microcirculation and oxygen balance to the
vital organs, thus increasing the fatality risk (12).
Considering that our patients were fluid
resuscitated prior to admission, we could advocate that the
norepinephrine-dependent patients were either inadequately
fluid-resuscitated and/or had a more complex liver trauma, who
needed even more blood products and crystalloids, although these
two factors were not associated, in our study, with a prolonged ICU
stay. Microcirculation impairments or the degree of systemic
inflammation due to norepinephrine use could be consequences of
prolonged ICU stay. Our data are in accordance with Uchida et
al, who showed that the use of norepinephrine could increase
the mortality rate/ICU stay (13).
Prehospital airway protection by means of
endotracheal intubation in trauma patients is a debated issue in
the literature (14). The actual
guidelines promote the early endotracheal intubation in polytrauma
patients, especially those with thorax, abdominal and/or head
injury. The decision to intubate at the scene or in the ER
department should be guided by the type of trauma (15). Avoiding hypoxia along with
maintaining airway patency in this patient subgroup is crucial. The
long-term beneficial effect, is, however, controversial (16).
Little is known about early intubation in patients
with isolated traumatic liver injury. In our study, the patients
with isolated liver trauma, who were intubated in prehospital
settings, had a longer stay in the ICU. This finding could be
explained due to various reasons: residual sedation with consequent
postoperative prolonged weaning, increased personnel infrastructure
and time-consuming perioperative diagnostic and therapeutic
maneuvers related to the complexity of the case, difficulties in
prehospital ICU bed allocation process, and overall case severity.
Our results are in contradiction with Gravesteijn et al
(16). Their study suggested that
patients with abdominal trauma had a better functional outcome if
intubated in prehospital settings. Further observational
prospective studies are needed to evaluate this clinical approach.
Additionally, we observed that ventilation hours were correlated
with the ICU length of stay. This finding could be a consequence of
a prolonged weaning time, acquired muscle weakness and
intubation-related nursing impairments.
Mechanical ventilation time in trauma patients has
been also shown to have other detrimental effects such as: longer
ICU stay and hospital stay, higher rates of tracheostomy and
mortality (17).
Fibrinogen may be reduced following traumatic injury
due to loss from hemorrhage, increased consumption and reduced
synthesis (18). Plasma fibrinogen
levels have been found to decrease earlier than other hemostasis
parameters in trauma patients (e.g., platelet count, prothrombin
time, activated partial thromboplastin time). There are three
proposed mechanisms for plasma fibrinogen decrease: coagulation
activation-induced consumption, hyper-fibrino(geno)lysis-induced
degradation, and dilution by infusion/transfusion. Initial
fibrinogen levels less than the normal range are independently
associated with higher in-hospital mortality in trauma patients
(19).
In liver trauma patients, because of the destruction
of the liver parenchyma, plasma fibrinogen levels can be
furthermore decreased, leading to fibrinogen concentrate
substitution therapy (20).
In this study, the patients with a high fibrinogen
concentration at admission had a prolonged length of ICU stay.
These results are in contradiction with other research (18), but there are some possible
explanations. The rise of fibrinogen levels from day 2 onwards can
be attributed to an upregulated fibrinogen synthesis in the liver,
occurring as part of the acute phase response after tissue injury
(4).
This result draws our attention to the role of
fibrinogen as part of the acute phase response after tissue
injury.
Study limitations
Our study has some inherent limits. First, we
analyzed only a limited number of patients, who were presented to
our service. This aspect had known consequences on the statistical
analysis and conclusions. Secondly, the study design was
retrospective and monocentric. Thus, no causality can be affirmed.
In addition, some data before admission were not available for
analysis and discussion for some patients. Despite these evident
flaws, we have to state that our hospital is the main national
center in hepatic surgery, serving the entire nation of Romania.
Consequently, even in small numbers, our results have a national
epidemiological interest, considering both the Romanian population,
but also the Romanian healthcare organization.
This aspect is of interest, opening insights of a
local Eastern European experience, but it mau also represent a
further limit. The trauma transfusion guidelines can be applied in
an unpredictable manner, particularly in small provincial
hospitals.
In conclusion, our study revealed the experience in
a national center for liver surgery, from the intensive care
perspective, in isolated liver trauma, proving that intubation
status at admission, intraoperative norepinephrine use, mechanical
ventilation hours and plasma fibrinogen are deleterious independent
variables which correlates with the ICU length of stay. Further
large prospective studies are needed in order to confirm these
results.
Acknowledgements
The authors would like to thank Artsiom Klimko for
his help with manuscript reviewing.
Funding
Funding: No funding was received.
Availability of data and materials
Due to confidentiality reasons, data generated or
analyzed during this study are not included in this published
article.
Authors' contributions
SI performed the statistical analysis, wrote and
reviewed the manuscript, and designed the study. SA wrote the
manuscript, collected the data, and designed the study. MC
collected the data, contributed to manuscript writing, designed the
study; CM contributed to the manuscript writing and to study
design. LM collected the data and contributed to the study design.
CB reviewed the manuscript and data collection. DI contributed to
the manuscript writing and to the literature and manuscript
reviewing. DEG contributed to the manuscript writing and to the
literature and manuscript reviewing. GD coordinated the study,
contributed to the study design and reviewed the manuscript. All
authors agreed on the final form of the manuscript for
publication.
Ethics approval and consent to
participate
This study was approved by the local Ethics
Committee of ‘Fundeni’ Clinical Institute (Romania). Written
informed consent was obtained from all patients prior to
publication.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization (WHO) (2010)
Injuries and Violence: The Facts. World Health Organization,
Geneva, 2010, https://www.who.int/violence_injury_prevention/en/.
|
|
2
|
Sakran JV, Greer SE, Werlin E and McCunn
M: Care of the injured worldwide: Trauma still the neglected
disease of modern society. Scand J Trauma Resusc Emerg Med.
20(64)2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Park KB, You DD, Hong TH, Heo JM and Won
YS: Comparison between operative versus non-operative management of
traumatic liver injury. Korean J Hepatobiliary Pancreat Surg.
19:103–108. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Coccolini F, Coimbra R, Ordonez C, Kluger
Y, Vega F, Moore EE, Biffl W, Peitzman A, Horer T, Abu-Zidan FM, et
al: Liver trauma: WSES 2020 guidelines. World J Emerg Surg.
15(24)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
David Richardson J, Franklin GA, Lukan JK,
Carrillo EH, Spain DA, Miller FB, Wilson MA, Polk HC Jr and Flint
LM: Evolution in the management of hepatic trauma: A 25-year
perspective. Ann Surg. 232:324–330. 2000.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cirocchi R, Trastulli S, Pressi E,
Farinella E, Avenia S, Morales Uribe CH, Botero AM and Barrera LM:
Non-operative management versus operative management in high-grade
blunt hepatic injury. Cochrane Database Syst Rev. (issue
8)(CD010989)2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Popescu I, Ionescu M, Braşoveanu V,
Hrehoreţ D, Copca N, Lupaşcu C, Botea F, Dorobanţu B, Alexandrescu
S, Grigorie M, et al: The Romanian national program for liver
transplantation -852 procedures in 815 patients over 17 years
(2000-2017): A continuous evolution to success. Chirurgia (Bucur).
112:229–243. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Chen RJ, Fang JF, Lin BC, Hsu YP, Kao JL
and Chen MF: Factors determining operative mortality of grade V
blunt hepatic trauma. J Trauma. 49:886–891. 2000.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Scheeren WL and Saugel B: Management of
Intraoperative Hypotension: Prediction, prevention and
personalization. In: Annual Update in Intensive Care and Emergency
Medicine. Vincent JL (ed). Springer, p89-97, 2018.
|
|
10
|
Gupta B, Garg N and Ramachandran R:
Vasopressors: Do they have any role in hemorrhagic shock? J
Anaesthesiol Clin Pharmacol. 33:3–8. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Van der Linden P: Management of
uncontrolled hemorrhagic shock: Toward a new clinical approach.
Anesthesiology. 107:529–530. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Arabi Y, Venkatesh S, Haddad S, Al
Shimemeri A and Al Malik S: A prospective study of prolonged stay
in the intensive care unit: Predictors and impact on resource
utilization. Int J Qual Health Care. 14:403–410. 2002.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Uchida K, Nishimura T, Hagawa N, Kaga S,
Noda T, Shinyama N, Yamamoto H and Mizobata Y: The impact of early
administration of vasopressor agents for the resuscitation of
severe hemorrhagic shock following blunt trauma. BMC Emerg Med.
20(26)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rubenson Wahlin R, Nelson DW, Bellander
BM, Svensson M, Helmy A and Thelin EP: Prehospital intubation and
outcome in traumatic brain injury-assessing intervention efficacy
in a modern trauma cohort. Front Neurol. 9(194)2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Pepe PE, Roppolo LP and Fowler RL:
Prehospital endotracheal intubation: Elemental or detrimental? Crit
Care. 19(121)2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Gravesteijn BY, Sewalt CA, Nieboer D,
Menon DK, Maas A, Lecky F, Klimek M and Lingsma HF: CENTER-TBI
collaborators. Tracheal intubation in traumatic brain injury: A
multicentre prospective observational study. Br J Anaesth.
125:505–517. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Okabe Y: Risk factors for prolonged
mechanical ventilation in patients with severe multiple injuries
and blunt chest trauma: A single center retrospective case-control
study. Acute Med Surg. 5:166–172. 2018.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
McQuilten ZK, Wood EM, Bailey M, Cameron
PA and Cooper DJ: Fibrinogen is an independent predictor of
mortality in major trauma patients: A five-year statewide cohort
study. Injury. 48:1074–1081. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Hayakawa M: Dynamics of fibrinogen in
acute phases of trauma. J Intensive Care. 5(3)2017.
|
|
20
|
Schlimp CJ, Ponschab M, Voelckel W,
Treichl B, Maegele M and Schöchl H: Fibrinogen levels in trauma
patients during the first seven days after fibrinogen concentrate
therapy: A retrospective study. Scand J Trauma Resusc Emerg Med.
24(29)2016.PubMed/NCBI View Article : Google Scholar
|