1. Introduction
Pulmonary embolism (PE) is characterized by
pulmonary circulation and respiratory dysfunction caused by various
emboli (1). The clinical symptoms
of PE include chest pain, hemoptysis and dyspnea. An analysis of
vital registration data between 2013 and 2015 from the WHO
Mortality Database revealed that, between the ages of 15 and 55,
8-13 per 1,000 women and 2-7 per 1,000 men in Europe die due to PE
per year (2). The rapid
advancement of medical diagnostic technologies has resulted in a
progressive increase in the rate of PE diagnosis. Recent years have
demonstrated a substantial improvement in the prognosis of PE due
to early effective interventions, such as hemodynamics and
respiratory support, anticoagulation therapy and reperfusion
therapy, which have decreased the mortality rate of acute PE
(3).
Although symptoms can generally be improved within
3-6 months following effective treatment, most acute PE survivors
are at risk of long-term adverse outcomes, such as impaired quality
of life and activity tolerance (4-6).
The past few decades have mainly focused on diagnosis and
in-hospital treatment; thus, by ignoring rehabilitation importance,
long-term adverse symptoms have remained unaddressed (7). Sequential therapy for patients with
PE outside hospital and at home is equally important, which to a
certain extent could effectively reduce thrombosis recurrence and
improve prognosis.
In 2019, European Society of Cardiology guidelines
for diagnosis and management of acute PE recommended an effective
follow-up strategy for patients with persistent symptoms following
PE, including exercise rehabilitation, treatment of comorbidities,
behavioral education and modulation of risk factors (3). As an important component of chronic
lung disease management, pulmonary rehabilitation is mainly used
for patients with chronic obstructive pulmonary disease (COPD)
(8), which can improve their
long-term physical and mental conditions, and quality of life
(9-12).
A retrospective study determined that initiating pulmonary
rehabilitation within 3 months after hospitalization was
significantly associated with lower mortality risk at 1 year of
discharge from the index hospitalization for patients with COPD
(13).
Recently, applying pulmonary rehabilitation to
patients with other types of pulmonary diseases (such as PE) has
garnered considerable attention from clinicians (14,15).
Similar to COPD, patients with PE experience varying degrees of
respiratory symptoms and impaired motor function (16). A Chinese study conducted a 6-week
low-intensity exercise training program on 80 patients with acute
PE. The findings indicated that exercise training was beneficial to
patient recovery (17).
Unfortunately, to the best of our knowledge, there remains no
unified standard of long-term rehabilitation for patients with PE
and only a few studies have investigated the efficacy and safety of
rehabilitation after PE (14,18,19).
The present review detailed the etiology, pathogenesis and
susceptibility factors of PE, post-PE syndrome and clinical
application of pulmonary rehabilitation in patients with PE. The
details of the literature search strategy are presented in Data S1.
2. Etiology, pathogenesis and susceptibility
factors of PE
Venous thromboembolism (VTE) is a multifactorial
disease that involves deep vein thrombosis and PE, which is caused
by congenital or acquired pathophysiological changes that result in
venous blood flow disturbance or arrest (20). Typically, PE is caused when
pulmonary artery blockage, caused by a venous embolus in the lower
extremities, falls off, resulting in dysfunction of the pulmonary
circulation and the right atrium (21).
PE might share the pathogenic factors with VTE,
which can be roughly divided into congenital and acquired factors
(22). A previous statement
revealed that certain genetic factors may increase VTE and PE
risks, such as factor V Leiden mutations, activated protein C
resistance, prothrombin (factor II) G20210A mutation, protein S
deficiency and antithrombin deficiency (23). The acquired risk factors include
postoperative states, pregnancy, malignancy and age (24). Major trauma, surgery, lower-limb
fractures, joint replacements and spinal cord injury are also
strong risk factors for PE (3).
3. Post-PE syndrome
Following the occurrence of acute PE, ~50% of
patients experience a series of clinical manifestations, such as
persistent dyspnea and impaired activity tolerance and quality of
life due to abnormal pulmonary hemodynamics, gas exchange and
cardiopulmonary function (25,26).
If the residual symptoms and defects are not effectively improved,
they eventually lead to chronic thromboembolic pulmonary
hypertension (CTEPH) and even death. In China, 614 cases of acute
PE were followed up for a median of 3.3 years, the results of which
revealed that the 1-, 2- and 3-year cumulative incidences of CTEPH
were 0.8, 1.3 and 1.7%, respectively (27). A meta-analysis also revealed that
up to 3% of patients with PE suffer from CTEPH (28).
In 2014, Klok et al (29) first proposed the concept of
‘post-PE syndrome’, which guides the long-term monitoring,
management and follow-up of patients with PE. Its definition
specifically refers to clinical syndromes lasting >3 months
following acute PE occurrence and are mainly manifested by dyspnea,
activity limitation and decline in physical function status or
quality of life (29). The
occurrence and development of post-PE syndrome are mainly
influenced by residual thrombosis after PE, hemodynamic changes and
changes in cardiopulmonary function (29). After receiving appropriate
treatment, up to 50% of patients continue to experience these
residual symptoms and defects (30). For instance, compared with the
general population and matched controls, patients with a history of
PE have a reduced functional capacity and persistent dyspnea,
resulting in impaired health-related quality of life (26).
In recent years, the occurrence of such clinical
sequelae has garnered increasing attention (31-33).
The prospective multicenter cohort study (Evaluation of Long-term
Outcomes after Pulmonary Embolism study) revealed that 46.8% of
patients with PE had movement limitation, dyspnea and reduced
quality of life at the onset of a 1-year follow-up. In addition,
male sex, low age of onset, high BMI and smoking history were
independent predictors of post-PE syndrome (34,35).
According to a Follow-up after Acute Pulmonary Embolism study, the
median PE-quality of life score decreased from 3 to 12 months (from
19.4 to 13.0%) (36). To reverse
this trend, a multidisciplinary team (including physicians,
qualified nurses and other associated professionals) should provide
comprehensive treatment for patients with PE during hospitalization
and after discharge, and also optimize long-term management to
improve prognosis.
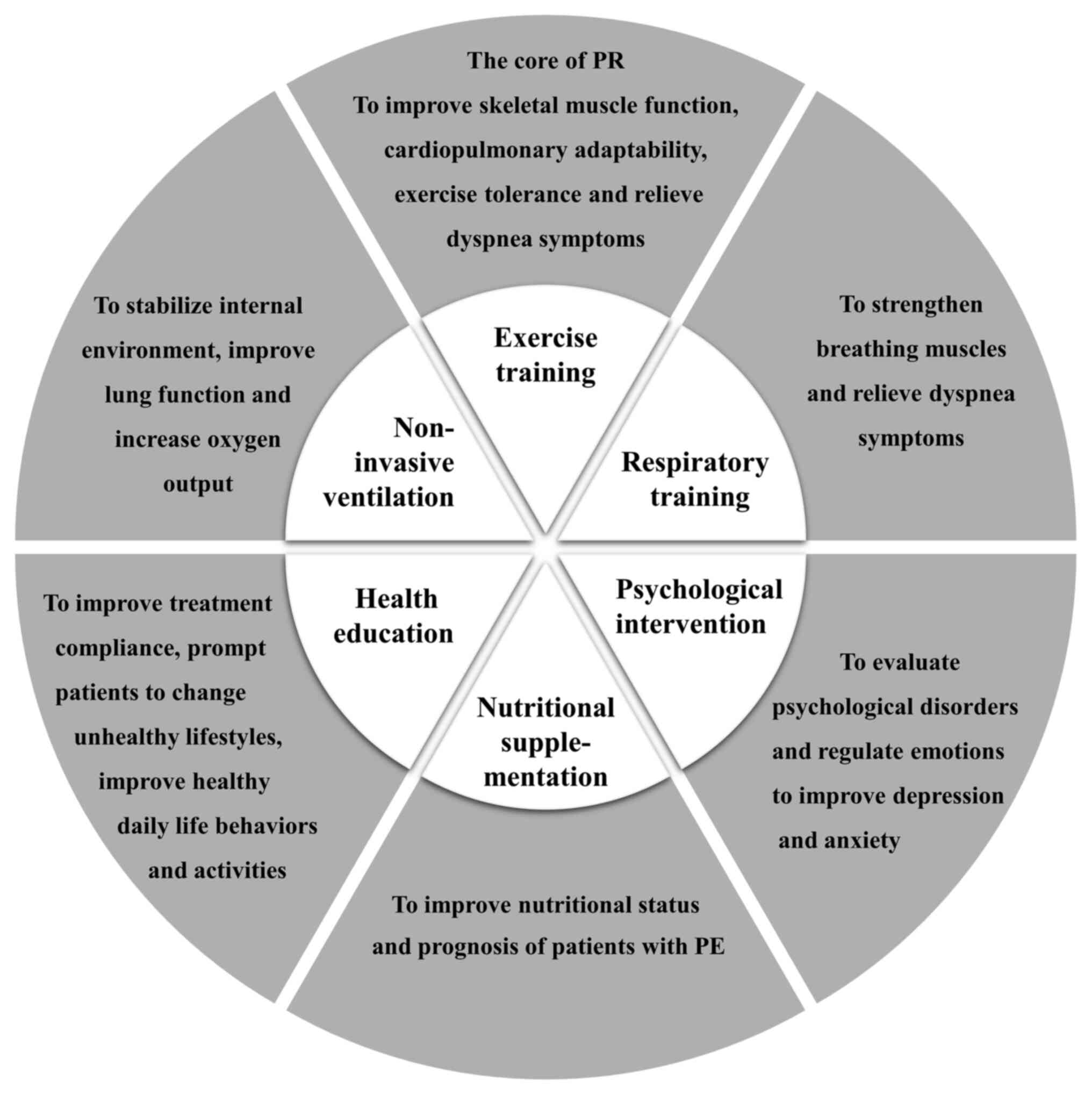
4. Pulmonary rehabilitation
Pulmonary rehabilitation is a comprehensive
intervention program that combines multiple measures and
disciplines, including but not limited to exercise training,
education and behavioral changes (Fig.
1) (37). Its objectives are
to enhance the physical and mental status of patients with chronic
respiratory diseases, and promote long-term health (38). Although pulmonary rehabilitation is
mainly applied in patients with COPD, it also includes patients
with other chronic respiratory diseases, such as asthma, pulmonary
hypertension, interstitial lung disease, pneumoconiosis and even
those with end-stage lung disease (37).
Exercise training
As the core of pulmonary rehabilitation therapy,
exercise training can improve skeletal muscle function,
cardiopulmonary adaptability and exercise tolerance while also
relieving dyspnea symptoms. The content of exercise training is
diverse, including interval training and resistance training.
Notably, exercise training should ensure the rationality of the
training program, allowing for smooth long-term and stable training
and thereby improving the effect of the training.
The exercise training can be divided into upper and
lower limb muscle strength training. Upper limb training includes
dumbbell lifting and chest expansion exercises, whereas lower limb
training includes walking, cycling, straight leg raising exercises
and knee extension training. The Pulmonary Rehabilitation
Guidelines of the American Thoracic Society and the European
Respiratory Society revealed that lower extremity muscle exercise
is important in improving the dyspnea symptoms of patients and
enhancing exercise endurance (8).
Moreover, upper limb training can improve fatigue. Therefore, upper
and lower extremity muscle exercises should be simultaneously
conducted to improve the effectiveness of exercise therapy.
Respiratory training
Respiratory training is an important component of
pulmonary rehabilitation since it focuses on strengthening
breathing muscles. Load training can drill the inspiratory
auxiliary muscles and diaphragm muscles to increase endurance and
the strength of muscles, thereby improving respiration. Several
studies have demonstrated that respiratory training can
significantly increase the maximum inspiratory pressure and maximum
tidal volume for patients with chronic respiratory diseases,
eventually improving their inspiratory muscle endurance, exercise
endurance and quality of life (39-41).
For patients with PE, respiratory exercises should be performed if
the condition permits. According to rehabilitation physician
assessment, patients with PE may benefit from increasing their
breathing muscle training or exercising with a breathing training
device, improving breathing endurance and relieving dyspnea
symptoms (42,43).
Non-invasive ventilation
Non-invasive ventilation is a common pulmonary
rehabilitation measure, which can stabilize internal environment,
improve lung function and increase oxygen output (44). Applying non-invasive ventilation in
patients with COPD has been developed, and studies have
demonstrated its significant beneficial impact on quality of life
by improving exercise capacity, respiratory function and reducing
dynamic malignant inflation and dyspnea (44,45).
A novel form of home non-invasive ventilation has emerged, bringing
convenience to the pulmonary rehabilitation of patients (46). However, non-invasive ventilation
also has certain risks, such as diaphragm damage (47). As a result, exploring solutions to
reduce mechanical ventilation injuries is required in the
future.
Health education
Health education is a systematic, planned and
organized process for educating patients on the disease itself and
how to prevent embolism recurrences, as well as the significance of
pulmonary rehabilitation treatment (37). Health education can enable patients
to clarify treatment methods and precautions of the disease and
improve their consciousness of respiratory rehabilitation and
exercise training. It can also motivate patients to regulate
medication and develop healthy living habits, thereby delaying the
decline in lung function (48).
Therefore, it is important to provide adequate health education for
patients to improve treatment compliance, prompt patients to change
unhealthy lifestyles and improve healthy daily life behaviors or
activities (49).
Psychological intervention
Due to long-term suffering, patients frequently
exhibit depression or irritability in addition to physical
discomfort (50,51). The majority of patients with acute
PE are afraid of the direct trauma caused by the disease and the
potential for death. Even survivors will experience long-term
psychological imbalances due to their fear of recurrence, which
eventually results in lifestyle and behavioral changes (30,52).
An observational study of patients with acute PE with a median
follow-up of 60 months revealed that patients usually experience
changes in behavior, reduced physical activity and even
post-traumatic stress (53). A
nested qualitative study was conducted to observe the thoughts,
feelings and experiences of patients throughout the early stages of
acute PE recovery and to explore strategies for restoring daily
life behavior and physical activity (54). During hospitalization, clinical
symptoms are gradually alleviated with the help of professional
doctors and nurses. However, after being discharged from hospital,
they may continue to experience anxiety due to a lack of
opportunity for close communication with specialists (54). A systematic review and
meta-analysis revealed that patients with mental illnesses are at
increased risk of VTE due to hypercoagulability and stasis
(55). This is a vicious circle
that not only aggravates symptoms of PE but also deteriorates the
mental state. Accordingly, mental health cannot be ignored during
the PE treatment process. In pulmonary rehabilitation, patients
should learn to better regulate their emotions to improve their
depression and anxiety, such as training on emotional awareness,
selecting and attending to stressors and modulating emotional
reactions (56). In addition,
physicians should routinely evaluate whether patients have
psychological disorders.
Nutritional supplementation
In addition to the gradual decrease of lung function
in patients with PE, malnutrition is a typical complication,
impairing the disease's outcome (57). Therefore, nutritional assessment
and intervention should be initiated promptly for patients with PE.
Previous studies suggested that patients should achieve nutritional
interventions by adjusting their diet, such as low-carbohydrate and
high-protein diets supplemented with potassium, magnesium,
phosphorus, zinc and other trace elements and vitamins (58,59).
Increased protein intake in the diet increases the total muscle
mass, which improves respiratory muscle function (57). However, there are currently few
studies on nutritional interventions for patients with PE.
Therefore, additional research is required to confirm the impact of
nutritional interventions on patient recovery in order to
rationally apply nutritional interventions in the future.
In summary, pulmonary rehabilitation requires
interdisciplinary collaboration to provide a full range of
interventions for patients with PE regarding disease management,
symptom alleviation, respiratory function maintenance,
psychological intervention and nutritional supplementation.
American College of Chest Physicians/American Association of
Cardiovascular and Pulmonary Rehabilitation proposes that the
content of level A in pulmonary rehabilitation is exercise
training. Level B is non-invasive ventilation, breathing muscle
exercises and health education, whereas level C is nutritional
supplementation (60).
Furthermore, clinicians should choose appropriate individualized
treatment methods to improve dyspnea and functional ability and,
thus, reintegrate patients into daily life.
5. Clinical implications of pulmonary
rehabilitation
As the importance of rehabilitation in the long-term
management of PE has been recognized by the international
community, it has gradually become more prevalent in clinical
practice. Appropriate pulmonary rehabilitation could relieve acute
symptoms and prevent or improve post-PE syndrome. However, the
current data on pulmonary rehabilitation are limited in patients
with PE (Table I).
 | Table IClinical implications of pulmonary
rehabilitation for patients with PE. |
Table I
Clinical implications of pulmonary
rehabilitation for patients with PE.
| Author | Year | Region | Research type | Rehabilitation
program | Results | (Refs.) |
|---|
| Lakoski et
al | 2015 | USA | Randomized clinical
trial | The program
included exercise training and a behavioral weight loss program
focused on moderate-intensity, high-volume physical activity to
increase energy expenditure and promote weight loss | Early initiation of
exercise training improved physical activity and fitness without
adverse events | (18) |
| Noack et
al | 2015 | Germany | Retrospective
study | A 3-week in-patient
rehabilitation program including Nordic walking, medical training
therapy, intensive gymnastics/exercise and pulmonological
functional exercise | The standard
rehabilitation program after PE was safe | (61) |
| Amoury et
al | 2018 | Germany | Prospective
study | A personalized
rehabilitation program, including exercise training, breathing
training, attending seminars and lectures, and psychosocial
support | Mortality and other
serious event rates (hospital admission, bleeding complications and
thromboembolic events) were low during hospital admission and in
the 12-month follow-up period | (63) |
| Rolving et
al | 2020 | Denmark | Randomized clinical
trial | A brief nurse
consultation and an 8-week home-based exercise program | Exercise capacity
and dyspnea symptoms did not improve. No additional adverse events
were documented | (64) |
| Nopp et
al | 2020 | Austria | Prospective
study | Endurance, strength
and inspiratory muscle training over at least 6 weeks (three times
a week for 3-4 h); individualized patient education including
disease- and medical treatment-specific seminars, nutritional
counseling and smoking cessation sessions | The 6 min walk
experiment demonstrated improved results. Maximum strength,
endurance and inspiratory muscle strength was also improved. The
health of 78% of patients improved during long-term follow-up | (19) |
| Cires-Drouet et
al | 2020 | USA | Prospective
study | A 3-month exercise
program (exercise training was conducted in three phases) | Low-to-moderate
intensity exercise therapy was safe after acute PE | (62) |
| Boon et
al | 2021 | Netherlands | Observational
cohort study | A 12-week
out-patient pulmonary rehabilitation program, including endurance
exercise training, strength exercise training, pulmonologist
consultation, physiotherapist consultation | Improved training
intensity, PE-specific quality of life, fatigue and functional
status | (14) |
| Haukeland-Parker
et al | 2021 | Norway | Randomized control
trial | A basic pulmonary
rehabilitation program consisting of a supervised, out-patient
exercise program for 1 h twice weekly for eight weeks and an
educational session | The trial has not
been completed | (65) |
After 3 months of follow-up, a randomized clinical
trial for patients with acute VTE revealed that neither the
exercise intervention group nor the control group experienced
serious adverse events (18). In
addition, the exercise intervention group had a significantly
reduced BMI and significantly increased physical activity and
maximum oxygen consumption compared with the control group. Nopp
et al (19) revealed that
the exercise capacity of 22 patients with PE exhibiting persistent
symptoms and undergoing an out-patient multi-professional 6-week
pulmonary rehabilitation program were significantly improved. In
the Netherlands, an observational cohort study revealed that a
12-week out-patient pulmonary rehabilitation program that included
sports and psychological counseling, effectively improved patient
symptoms (14). Noack et al
(61) retrospectively analyzed the
role of a 3-week in-patient rehabilitation program for patients
with PE, which suggested that pulmonary rehabilitation programs
following PE might be considered safe. Low-to-moderate-intensity
exercise therapy following acute PE is considered safe in the
United States (62). German
researchers have established a personalized exercise and
rehabilitation program for intermediate- and high-risk patients
with PE based on their clinical characteristics (physical fitness,
primary disease severity, comorbidities and other confounding
factors) (63). The results
indicated no serious adverse events during rehabilitation
processes, such as bleeding, rehospitalization or death due to VTE.
Furthermore, the mortality rate of patients receiving
rehabilitation during hospitalization and at 12 months follow-up
was 0 and 5.7%, respectively. This prospective study demonstrated
that pulmonary rehabilitation is both safe and effective for
patients with PE (63), implying
the potential application value of pulmonary rehabilitation.
However, the conclusion was limited by the small number of patients
and the lack of a control group. Large-scale prospective studies
are required to identify the benefits of pulmonary rehabilitation
for patients with PE.
Rolving et al (64) conducted a randomized controlled
trial on patients that were newly diagnosed with PE to study the
effect of rehabilitation intervention on early physical fitness and
quality of life. After 8 weeks of home-based exercise with nurse
consultation, the results indicated that home-based exercise did
not further improve exercise capacity or dyspnea symptoms of
patients with PE but also did not cause additional adverse events.
Nevertheless, this trial had a short follow-up time and included
patients with newly diagnosed PE. For newly diagnosed patients with
PE, their acute symptoms can be relieved after active early
clinical intervention (7). As the
disease continues, the impact of rehabilitation therapy on patients
with PE may become increasingly evident (64). A two-center randomized controlled
trial is ongoing (Clinical Trial no. NCT03405480). The intervention
involves individually adapted exercises based on existing pulmonary
rehabilitation programs (relaxation, interval and resistance
training) and an educational session (8 weeks). The physical
capacity, dyspnea and quality of life of intervention and control
groups were compared after 12 and 36 weeks (65).
6. Discussion
As a cardiovascular disease, PE is a common
emergency in internal medicine, ranking third in terms of mortality
after myocardial infarction and stroke in China (from 1997 to 2008)
and Europe (in 2014) (66,67). With the continuous advancement of
medical standards, clinicians not only focus on early diagnosis and
treatment of PE but also on long-term prognosis (68). Although the majority of patients
with PE resume their daily routines within 6 months to 1 year after
discharge, their daily activities remain limited and maintaining
adequate physical activity is difficult (54). As a result, new guidelines
emphasize the need for rehabilitation during long-term follow-up of
patients with PE (3).
As an inexpensive and high-efficiency treatment
strategy, pulmonary rehabilitation can significantly improve
dyspnea symptoms, overall health and exercise endurance in patients
with PE (64). However, due to
short application time of pulmonary rehabilitation in patients with
PE, no unified rehabilitation model and evaluation criteria have
been developed. According to current research results, pulmonary
rehabilitation therapy will have no adverse outcomes in patients
with PE (62). While the
effectiveness is questionable, the majority of research suggests
that pulmonary rehabilitation is feasible for patients with PE to
improve exercise capacity, relieve dyspnea symptoms and enhance
quality of life. Unfortunately, these studies generally suffer from
small sample sizes and short follow-up times. In the future, more
large-sample, multicenter and rigorous trials are required to
investigate more optimized pulmonary rehabilitation programs.
The content of the pulmonary rehabilitation project
has garnered particular attention. Exercise training is dominant in
pulmonary rehabilitation therapy and works to improve the exercise
capabilities of patients to a certain extent (69). There are still some patients who do
not improve their lung function with training, and other
interventions including health education and psychological
intervention, should be implemented to improve pulmonary
rehabilitation's effectiveness (37). A previous study demonstrated that
<50% of patients can maintain pulmonary rehabilitation for >1
year (70). For instance, in the
implementation plan of pulmonary rehabilitation, continuous
exercise training (usually walking and cycling) is important for
maintaining benefits and reducing readmission rates (71). It implies that future
rehabilitation approaches should prioritize exercise status while
also emphasizing health education and psychological counseling for
patients with PE. Moreover, previous studies were mainly performed
to assess whether the safety and effectiveness of pulmonary
rehabilitation program can be adapted to patients with PE or not.
Future research should focus on comparing the efficacy and safety
of different pulmonary rehabilitation programs head-to-head in
patients with PE.
As a serious adverse reaction after a PE, CTEPH can
develop into right-sided heart failure, which has a poor prognosis
(72). Some researchers have
incorporated pulmonary rehabilitation into the treatment plan of
patients with CTEPH. A preliminary investigation revealed that
home-based, closely supervised pulmonary rehabilitation therapy can
safely improve exercise capacity and health-related quality of life
in patients with CTEPH (73). In
addition, a retrospective analysis demonstrated that a 3-week
structured in-patient program (including incremental exercise
training, abdominal, upper and lower limb muscle activities,
education, nutritional programs and psychosocial counseling) can
improve exercise capacity for patients with CTEPH following
pulmonary endarterectomy (74).
For inoperable CTEPH, 12 weeks of rehabilitation training following
balloon pulmonary angioplasty can significantly improve athletic
performance and heart failure symptoms with a good safety level
(75). The available evidence
indicates that patients with acute PE and CTEPH (advanced stage)
can benefit from pulmonary rehabilitation.
According to our current knowledge, there are still
some unanswered questions: i) Whether the acute period or the
stable period is the most beneficial time to allow for pulmonary
rehabilitation in patients with PE; ii) whether the intensity of
exercise training is comparable to or less than that of daily
activities; iii) what duration pulmonary rehabilitation should
occur for; and iv) new interventions for patients with PE should be
explored in addition to the above six interventions (exercise
training, respiratory training, non-invasive ventilation, health
education, psychological intervention and nutritional
supplementation).
7. Conclusion
Pulmonary rehabilitation is an emerging field to be
applied in studying patients with PE. Nevertheless, there are
presently few studies available on this topic and sufficiently
powerful randomized controlled trials are limited. The existing
evidence suggests that pulmonary rehabilitation is a potential
treatment for alleviating post-PE syndrome, which improves the
quality of life and prognosis of patients with PE. More and
high-quality prospective studies are required to provide stronger
evidence.
Supplementary Material
Methodology. PubMed and Embase
databases were used to search for relevant articles. The following
search strategies were used for PubMed: (‘Pulmonary Embolism’
[Mesh]) AND (‘rehabilitation’ [Mesh]) and for Embase: (‘pulmonary
embolism’:ti,ab,kw AND ‘rehabilitation’:ti,ab,kw). Articles were
included if they described the treatment of patients with PE for
pulmonary rehabilitation. The observation indicators and the year
of publication were not limited. Abstracts, case reports and
conference summary were excluded. A total of 715 studies were
identified from the two databases. After evaluation of the titles
and full texts of articles, eight studies were included for the
present review.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by grants from the
Medical Health Science and Technology Project of Zhejiang Province
(grant nos. 2020KY817 and 2021KY281) and Ningbo Natural Science
Foundation Project (grant no. 202003N4274).
Availability of data and materials
Not applicable.
Authors' contributions
AY contributed to conception, design and final
approval of the submitted version. WD, WL, JC, WH and AY
contributed to completing the table, and writing and revising the
paper. All authors have read and approved the final manuscript.
Data sharing is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhou H, Tang Y, Wang L, Shi C, Feng Y and
Yi Q: Risk factors associated with long-term mortality in patients
with pulmonary embolism and the predictive value of Charlson
comorbidity index. Zhonghua Yi Xue Za Zhi. 96:273–276.
2016.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
2
|
Barco S, Mahmoudpour SH, Valerio L, Klok
FA, Münzel T, Middeldorp S, Ageno W, Cohen AT, Hunt BJ and
Konstantinides SV: Trends in mortality related to pulmonary
embolism in the European region, 2000-15: Analysis of vital
registration data from the WHO mortality database. Lancet Respir
Med. 8:277–287. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Konstantinides SV, Meyer G, Becattini C,
Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings
CS, Jiménez D, et al: 2019 ESC guidelines for the diagnosis and
management of acute pulmonary embolism developed in collaboration
with the European Respiratory Society (ERS): The task force for the
diagnosis and management of acute pulmonary embolism of the
European society of cardiology (ESC). Eur Respir J.
54(1901647)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Huisman MV, Barco S, Cannegieter SC, Le
Gal G, Konstantinides SV, Reitsma PH, Rodger M, Vonk Noordegraaf A
and Klok FA: Pulmonary embolism. Nat Rev Dis Primers.
4(18028)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ghanima W, Wik HS, Tavoly M, Enden T and
Jelsness-Jørgensen LP: Late consequences of venous thromboembolism:
Measuring quality of life after deep vein thrombosis and pulmonary
embolism. Thromb Res. 164:170–176. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Klok FA, van Kralingen KW, van Dijk AP,
Heyning FH, Vliegen HW, Kaptein AA and Huisman MV: Quality of life
in long-term survivors of acute pulmonary embolism. Chest.
138:1432–1440. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Konstantinides SV, Torbicki A, Agnelli G,
Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M,
Kucher N, et al: 2014 ESC guidelines on the diagnosis and
management of acute pulmonary embolism. Eur Heart J. 35:3033–3069,
3069a-3069k. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Spruit MA, Singh SJ, Garvey C, ZuWallack
R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, et
al: An official American thoracic society/European respiratory
society statement: Key concepts and advances in pulmonary
rehabilitation. Am J Respir Crit Care Med. 188:e13–e64.
2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Güell MR, Cejudo P, Ortega F, Puy MC,
Rodríguez-Trigo G, Pijoan JI, Martinez-Indart L, Gorostiza A, Bdeir
K, Celli B and Galdiz JB: Benefits of long-term pulmonary
rehabilitation maintenance program in patients with severe chronic
obstructive pulmonary disease. Three-year follow-up. Am J Respir
Crit Care Med. 195:622–629. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Liu X, Wu W, Li N, Li P, Wang Z and Shan
C: Effects of water-based Liuzijue exercise on peak exercise
capacity, functional exercise capacity, and quality of life in
people with COPD. Clin Respir J. 15:956–966. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zhu Y, Zhu Y, Zhu Y, Ren Q and Zhou T: An
analysis of the dynamic changes in the self-efficacy and quality of
life of elderly patients with chronic obstructive pulmonary disease
following community-based rehabilitation. Am J Transl Res.
13:2745–2751. 2021.PubMed/NCBI
|
|
12
|
Vogelmeier CF, Criner GJ, Martinez FJ,
Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M,
Fabbri LM, et al: Global strategy for the diagnosis, management,
and prevention of chronic obstructive lung disease 2017 report.
GOLD executive summary. Am J Respir Crit Care Med. 195:557–582.
2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lindenauer PK, Stefan MS, Pekow PS, Mazor
KM, Priya A, Spitzer KA, Lagu TC, Pack QR, Pinto-Plata VM and
ZuWallack R: Association between initiation of pulmonary
rehabilitation after hospitalization for COPD and 1-year survival
among medicare beneficiaries. JAMA. 323:1813–1823. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Boon GJAM, Janssen SMJ, Barco S, Bogaard
HJ, Ghanima W, Kroft LJM, Meijboom LJ, Ninaber MK, Nossent EJ,
Spruit MA, et al: Efficacy and safety of a 12-week outpatient
pulmonary rehabilitation program in Post-PE syndrome. Thromb Res.
206:66–75. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Nolan CM, Polgar O, Schofield SJ, Patel S,
Barker RE, Walsh JA, Ingram KA, George PM, Molyneaux PL, Maher TM
and Man WD: Pulmonary rehabilitation in idiopathic pulmonary
fibrosis and COPD: A propensity matched real-world study. Chest,
Oct 23, 2021 (Epub ahead of print).
|
|
16
|
Nilsson LT, Andersson T, Larsen F, Lang
IM, Liv P and Söderberg S: Dyspnea after pulmonary embolism: A
nation-wide population-based case-control study. Pulm Circ.
11(20458940211046831)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wang Z, Sun Y and An Y: Reduced exercise
training on the rehabilitation status of patients with acute
pulmonary embolism. Sci Technol Eng. 17:154–159. 2017.(In
Chinese).
|
|
18
|
Lakoski SG, Savage PD, Berkman AM,
Penalosa L, Crocker A, Ades PA, Kahn SR and Cushman M: The safety
and efficacy of early-initiation exercise training after acute
venous thromboembolism: A randomized clinical trial. J Thromb
Haemost. 13:1238–1244. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Nopp S, Klok FA, Moik F, Petrovic M, Derka
I, Ay C and Zwick RH: Outpatient pulmonary rehabilitation in
patients with persisting symptoms after pulmonary embolism. J Clin
Med. 9(1811)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lin HY, Lin CY and Shen MC: Review article
inferior vena cava thrombosis: A case series of patients observed
in Taiwan and literature review. Thromb J. 19(43)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Panahi L, Udeani G, Horseman M, Weston J,
Samuel N, Joseph M, Mora A and Bazan D: Review of medical therapies
for the management of pulmonary embolism. Medicina (Kaunas).
57(110)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Depietri L, Marietta M, Scarlini S,
Marcacci M, Corradini E, Pietrangelo A and Ventura P: Clinical
impact of application of risk assessment models (Padua prediction
score and improve bleeding score) on venous thromboembolism, major
hemorrhage and health expenditure associated with pharmacologic VTE
prophylaxis: A ‘real life’ prospective and retrospective
observational study on patients hospitalized in a single internal
medicine unit (the STIME study). Intern Emerg Med. 13:527–534.
2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
From the American Association of
Neurological Surgeons (AANS), American Society of Neuroradiology
(ASNR), Cardiovascular and Interventional Radiology Society of
Europe (CIRSE), Canadian Interventional Radiology Association
(CIRA), Congress of Neurological Surgeons (CNS), European Society
of Minimally Invasive Neurological Therapy (ESMINT), European
Society of Neuroradiology (ESNR), European Stroke Organization
(ESO), Society for Cardiovascular Angiography and Interventions
(SCAI), Society of Interventional Radiology (SIR) et al.
Multisociety consensus quality improvement revised consensus
statement for endovascular therapy of acute ischemic stroke. Int J
Stroke. 13:612–632. 2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Goldhaber SZ: Risk factors for venous
thromboembolism. J Am Coll Cardiol. 56:1–7. 2010.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Klok FA, Tijmensen JE, Haeck ML, van
Kralingen KW and Huisman MV: Persistent dyspnea complaints at
long-term follow-up after an episode of acute pulmonary embolism:
Results of a questionnaire. Eur J Intern Med. 19:625–629.
2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Tavoly M, Utne KK, Jelsness-Jørgensen LP,
Wik HS, Klok FA, Sandset PM and Ghanima W: Health-related quality
of life after pulmonary embolism: A cross-sectional study. BMJ
Open. 6(e013086)2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yang S, Yang Y, Zhai Z, Kuang T, Gong J,
Zhang S, Zhu J, Liang L, Shen YH and Wang C: Incidence and risk
factors of chronic thromboembolic pulmonary hypertension in
patients after acute pulmonary embolism. J Thorac Dis. 7:1927–1938.
2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Ende-Verhaar YM, Cannegieter SC, Vonk
Noordegraaf A, Delcroix M, Pruszczyk P, Mairuhu AT, Huisman MV and
Klok FA: Incidence of chronic thromboembolic pulmonary hypertension
after acute pulmonary embolism: A contemporary view of the
published literature. Eur Respir J. 49(1601792)2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Klok FA, van der Hulle T, den Exter PL,
Lankeit M, Huisman MV and Konstantinides S: The post-PE syndrome: A
new concept for chronic complications of pulmonary embolism. Blood
Rev. 28:221–226. 2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Hunter R, Lewis S, Noble S, Rance J and
Bennett PD: ‘Post-thrombotic panic syndrome’: A thematic analysis
of the experience of venous thromboembolism. Br J Health Psychol.
22:8–25. 2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Fabyan KD and Holley AB: Postpulmonary
embolism syndrome. Curr Opin Pulm Med. 27:335–341. 2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Boon GJAM, Huisman MV and Klok FA:
Determinants and management of the post-pulmonary embolism
syndrome. Semin Respir Crit Care Med. 42:299–307. 2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Alonso-Martínez JL, Anniccherico-Sánchez
FJ and Urbieta-Echezarreta MA: The post-pulmonary embolism (post-PE
syndrome). Eur J Intern Med. 76:127–129. 2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kahn SR, Hirsch AM, Akaberi A, Hernandez
P, Anderson DR, Wells PS, Rodger MA, Solymoss S, Kovacs MJ, Rudski
L, et al: Functional and exercise limitations after a first episode
of pulmonary embolism: Results of the ELOPE prospective cohort
study. Chest. 151:1058–1068. 2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kahn SR, Akaberi A, Granton JT, Anderson
DR, Wells PS, Rodger MA, Solymoss S, Kovacs MJ, Rudski L, Shimony
A, et al: Quality of life, dyspnea, and functional exercise
capacity following a first episode of pulmonary embolism: Results
of the ELOPE cohort study. Am J Med. 130:990.e9–990.e21.
2017.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Valerio L, Barco S, Jankowski M,
Rosenkranz S, Lankeit M, Held M, Gerhardt F, Bruch L, Ewert R,
Faehling M, et al: Quality of life 3 and 12 months following acute
pulmonary embolism: Analysis from a prospective multicenter cohort
study. Chest. 159:2428–2438. 2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Shenoy MA and Paul V: Pulmonary
rehabilitation. In: StatPearls, Treasure Island (FL), StatPearls
Publishing, 2021.
|
|
38
|
Jiang Y, Guo J, Sun P, Chen Z, Liu F, Wang
S and Ding Z: Perceptions and experiences of older patients and
healthcare professionals regarding shared decision-making in
pulmonary rehabilitation: A qualitative study. Clin Rehabil.
35:1627–1639. 2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Silva IS, Fregonezi GA, Dias FA, Ribeiro
CT, Guerra RO and Ferreira GM: Inspiratory muscle training for
asthma. Cochrane Database Syst Rev. 2013(CD003792)2013.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Arnedillo A, Gonzalez-Montesinos JL,
Fernandez-Santos JR, Vaz-Pardal C, España-Domínguez C,
Ponce-González JG and Cuenca-García M: Effects of a rehabilitation
programme with a nasal inspiratory restriction device on exercise
capacity and quality of life in COPD. Int J Environ Res Public
Health. 17(3669)2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
McCreery JL, Mackintosh KA, Mills-Bennett
R and McNarry MA: The effect of a high-intensity PrO2Fit
inspiratory muscle training intervention on physiological and
psychological health in adults with bronchiectasis: A mixed-methods
study. Int J Environ Res Public Health. 18(3051)2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Zampogna E, Zappa M, Spanevello A and
Visca D: Pulmonary rehabilitation and asthma. Front Pharmacol.
11(542)2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Bernardi E, Pomidori L, Bassal F, Contoli
M and Cogo A: Respiratory muscle training with normocapnic
hyperpnea improves ventilatory pattern and thoracoabdominal
coordination, and reduces oxygen desaturation during endurance
exercise testing in COPD patients. Int J Chron Obstruct Pulmon Dis.
10:1899–1906. 2015.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Fekete M, Kerti M, Fazekas-Pongor V,
Balazs P, Csizmadia Z, Nemeth AN, Tarantini S and Varga JT: Effect
of interval training with non-invasive ventilation in severe
chronic obstructive pulmonary disease-a prospective cohort study
with matched control group. Ann Palliat Med. 10:5289–5298.
2021.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Cortegiani A, Longhini F, Madotto F, Groff
P, Scala R, Crimi C, Carlucci A, Bruni A, Garofalo E, Raineri SM,
et al: High flow nasal therapy versus noninvasive ventilation as
initial ventilatory strategy in COPD exacerbation: A multicenter
non-inferiority randomized trial. Crit Care. 24(692)2020.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Ergan B, Oczkowski S, Rochwerg B, Carlucci
A, Chatwin M, Clini E, Elliott M, Gonzalez-Bermejo J, Hart N, Lujan
M, et al: European respiratory society guidelines on long-term home
non-invasive ventilation for management of COPD. Eur Respir J.
54(1901003)2019.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Padilha GA, Horta LF, Moraes L, Braga CL,
Oliveira MV, Santos CL, Ramos IP, Morales MM, Capelozzi VL,
Goldenberg RC, et al: Comparison between effects of pressure
support and pressure-controlled ventilation on lung and
diaphragmatic damage in experimental emphysema. Intensive Care Med
Exp. 4(35)2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Roberts NJ, Kidd L, Kirkwood K, Cross J
and Partridge MR: How is the education component of pulmonary
rehabilitation delivered in practice-is it patient-centred? Clin
Respir J. 15:835–842. 2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Janssen SM, Vliet Vlieland TP, Volker G,
Spruit MA and Abbink JJ: Pulmonary rehabilitation improves
self-management ability in subjects with obstructive lung disease.
Respir Care. 66:1271–1281. 2021.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Popa-Velea O and Purcarea VL:
Psychological intervention-a critical element of rehabilitation in
chronic pulmonary diseases. J Med Life. 7:274–281. 2014.PubMed/NCBI
|
|
51
|
Habib GMM, Rabinovich R, Divgi K, Ahmed S,
Saha SK, Singh S, Uddin A, Uzzaman MN and Pinnock H: Systematic
review of clinical effectiveness, components, and delivery of
pulmonary rehabilitation in low-resource settings. NPJ Prim Care
Respir Med. 30(52)2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Højen AA, Dreyer PS, Lane DA, Larsen TB
and Sørensen EE: Adolescents' and young adults' lived experiences
following venous thromboembolism: ‘It will always lie in wait’.
Nurs Res. 65:455–464. 2016.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Noble S, Lewis R, Whithers J, Lewis S and
Bennett P: Long-term psychological consequences of symptomatic
pulmonary embolism: A qualitative study. BMJ Open.
4(e004561)2014.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Rolving N, Brocki BC and Andreasen J:
Coping with everyday life and physical activity in the aftermath of
an acute pulmonary embolism: A qualitative study exploring
patients' perceptions and coping strategies. Thromb Res.
182:185–191. 2019.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Kowal C, Peyre H, Amad A, Pelissolo A,
Leboyer M, Schürhoff F and Pignon B: Psychotic, mood, and anxiety
disorders and venous thromboembolism: A systematic review and
meta-analysis. Psychosom Med. 82:838–849. 2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Wierenga KL, Fresco DM, Alder M, Sattar A
and Moore SM: Preliminary efficacy of an emotion regulation
intervention on physical activity and depressive and anxious
symptoms in individuals in cardiac rehabilitation. J Cardiovasc
Nurs, Jul 23, 2021 (Online ahead of print).
|
|
57
|
Mete B, Pehlivan E, Gülbaş G and Günen H:
Prevalence of malnutrition in COPD and its relationship with the
parameters related to disease severity. Int J Chron Obstruct Pulmon
Dis. 13:3307–3312. 2018.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Miki K and Maekura R: Nutrition management
for COPD. Nihon Rinsho. 74:801–806. 2016.PubMed/NCBI(In Japanese).
|
|
59
|
Hsieh MJ, Yang TM and Tsai YH: Nutritional
supplementation in patients with chronic obstructive pulmonary
disease. J Formos Med Assoc. 115:595–601. 2016.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Ries AL, Bauldoff GS, Carlin BW, Casaburi
R, Emery CF, Mahler DA, Make B, Rochester CL, Zuwallack R and
Herrerias C: Pulmonary rehabilitation: Joint ACCP/AACVPR
evidence-based clinical practice guidelines. Chest. 131 (5
Suppl):4S–42S. 2007.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Noack F, Schmidt B, Amoury M, Stoevesandt
D, Gielen S, Pflaumbaum B, Girschick C, Völler H and Schlitt A:
Feasibility and safety of rehabilitation after venous
thromboembolism. Vasc Health Risk Manag. 11:397–401.
2015.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Cires-Drouet RS, Mayorga-Carlin M,
Toursavadkohi S, White R, Redding E, Durham F, Dondero K, Prior SJ,
Sorkin JD and Lal BK: Safety of exercise therapy after acute
pulmonary embolism. Phlebology. 35:824–832. 2020.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Amoury M, Noack F, Kleeberg K, Stoevesandt
D, Lehnigk B, Bethge S, Heinze V and Schlitt A: Prognosis of
patients with pulmonary embolism after rehabilitation. Vasc Health
Risk Manag. 14:183–187. 2018.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Rolving N, Brocki BC, Bloch-Nielsen JR,
Larsen TB, Jensen FL, Mikkelsen HR, Ravn P and Frost L: Effect of a
physiotherapist-guided home-based exercise intervention on physical
capacity and patient-reported outcomes among patients with acute
pulmonary embolism: A randomized clinical trial. JAMA Netw Open.
3(e200064)2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Haukeland-Parker S, Jervan Ø, Johannessen
HH, Gleditsch J, Stavem K, Steine K, Spruit MA, Holst R, Tavoly M,
Klok FA and Ghanima W: Pulmonary rehabilitation to improve physical
capacity, dyspnea, and quality of life following pulmonary embolism
(the PeRehab study): Study protocol for a two-center randomized
controlled trial. Trials. 22(22)2021.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Yang Y, Liang L, Zhai Z, He H, Xie W, Peng
X and Wang C: Investigators for National Cooperative Project for
Prevention and Treatment of PTE-DVT. Pulmonary embolism incidence
and fatality trends in chinese hospitals from 1997 to 2008: A
multicenter registration study. PLoS One. 6(e26861)2011.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Becattini C, Agnelli G, Lankeit M, Masotti
L, Pruszczyk P, Casazza F, Vanni S, Nitti C, Kamphuisen P, Vedovati
MC, et al: Acute pulmonary embolism: Mortality prediction by the
2014 European society of cardiology risk stratification model. Eur
Respir J. 48:780–786. 2016.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Sandal A, Korkmaz ET, Aksu F, Köksal D,
Toros Selçuk Z, Demir AU, Emri S and Çöplü L: Performance of
pulmonary embolism severity index in predicting long-term mortality
after acute pulmonary embolism. Anatol J Cardiol. 25:544–554.
2021.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Xu L, Fu C, Zhang Q, He C and Wei Q: The
effectiveness of exercise training in treating venous
thromboembolism: A systematic review. Phys Sportsmed. 49:1–11.
2021.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Spencer LM and McKeough ZJ: Maintaining
the benefits following pulmonary rehabilitation: Achievable or not?
Respirology. 24:909–915. 2019.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Alison JA, McKeough ZJ, Johnston K,
McNamara RJ, Spencer LM, Jenkins SC, Hill CJ, McDonald VM, Frith P,
Cafarella P, et al: Australian and New Zealand pulmonary
rehabilitation guidelines. Respirology. 22:800–819. 2017.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Catella-Chatron J, Merah A, De Magalhaes
E, Moulin N, Accassat S, Duvillard C, Mismetti P and Bertoletti L:
Chronic thromboembolic pulmonary hypertension suspicion after
pulmonary embolism in cancer patients. Respir Med Res. 76:34–37.
2019.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Inagaki T, Terada J, Tanabe N, Kawata N,
Kasai H, Sugiura T, Shigeta A, Asano Y, Murata A, Tsushima K, et
al: Home-based pulmonary rehabilitation in patients with inoperable
or residual chronic thromboembolic pulmonary hypertension: A
preliminary study. Respir Investig. 52:357–364. 2014.PubMed/NCBI View Article : Google Scholar
|
|
74
|
La Rovere MT, Pinna GD, Pin M, Bruschi C,
Callegari G, Zanotti E, D'Armini A and Ambrosino N: Exercise
training after pulmonary endarterectomy for patients with chronic
thromboembolic pulmonary hypertension. Respiration. 97:234–241.
2019.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Fukui S, Ogo T, Takaki H, Ueda J, Tsuji A,
Morita Y, Kumasaka R, Arakawa T, Nakanishi M, Fukuda T, et al:
Efficacy of cardiac rehabilitation after balloon pulmonary
angioplasty for chronic thromboembolic pulmonary hypertension.
Heart. 102:1403–1409. 2016.PubMed/NCBI View Article : Google Scholar
|