1. Introduction
Dieulafoy's disease, initially described as
‘exulceratio simplex’ (1) in 1897,
is an acute luminal hemorrhage caused by the rupture of a feeding
artery under the actions of external factors, or spontaneous
rupture owing to vascular malformations of the gastrointestinal,
biliary or bronchial wall; the feeding artery does not taper to
capillaries after entering the submucosa, but remains constant in
diameter and protrudes from the intestinal lumen. After >100
years of revisions and improved understanding, the disease was
renamed as Dieulafoy's disease.
Dieulafoy's disease of the bronchus was first
described by Sweerts et al (2) in 1995, and to date, <100 cases have
been reported worldwide. However, as the condition is
under-recognized and frequently underdiagnosed, the actual
incidence is likely to be much higher. Therefore, it is necessary
to increase our awareness of Dieulafoy's disease of the bronchus,
which is considered to be one of the primary causes of massive
hemoptysis (3). Although the
natural history, diagnosis and preferred treatment of the disease
are still unclear, Dieulafoy's disease of the bronchus is believed
to be caused by both congenital (2)
and acquired factors (4). In
previous years, the awareness of the disease and associated
techniques of diagnosis and treatment have continued to improve,
and novel diagnostic technologies have been increasingly applied.
The present review summarizes the research advances in Dieulafoy's
disease of the bronchus.
2. Methods
The terms ‘bronchial OR bronchus’ AND ‘dieulafoy OR
dieulafoy's’ were searched in the PubMed and Embase databases,
covering the period between January 1985 and December 2019.
Literature associated with a definitive diagnosis or a high
suspicion of Dieulafoy's disease of the bronchus was screened, with
abstracts of meetings excluded. There were no limitations on the
language of the publications. A manual search was then conducted
according to the reference lists of the published articles.
3. Pathogenesis
Dieulafoy's disease of the bronchus is
pathologically characterized by the rupture and bleeding of a
dilated or abnormal artery in the bronchial submucosa. The dilated
or abnormal artery passes through the bronchial wall next to the
bronchial cavity, and is surrounded by a thin mucosal epithelial
layer. Abnormal vessels predominantly branch from the bronchial
artery system and rarely from the pulmonary artery (5).
The pathogenesis of bronchial Dieulafoy's disease
remains to be clarified. Most researchers believe that the disease
is congenital, while others believe that it is acquired or is
simply an abnormality of normal blood vessels (2,4-6).
The etiology and pathogenesis of Dieulafoy's disease of the
bronchus may be associated with congenital abnormalities of
bronchial and pulmonary arteries, chronic inflammation or injury of
the airway, and is also considered to be associated with long-term
heavy smoking (7). Almost half of
the patients are smoking or had smoked in our study (31 of the 74
patients had a history of smoking). Parrot et al (7) reported the cases of seven patients
with Dieulafoy's disease of the bronchus, all of whom were
long-term heavy smokers (mean smoking capacity, 49 packs/year),
which supports the aforementioned findings. Moreover, some patients
had a history of tuberculosis (6 of the 74 patients developed
tuberculosis), indicating a possible association with inflammatory
injury in tuberculosis or stretching and dilation of the bronchial
artery (7). In addition, 15
patients developed other respiratory diseases and two patients had
a history of cardiovascular disease (8). These findings indicate that
Dieulafoy's disease of the bronchus may be associated with a
history of basic diseases, especially respiratory diseases such as
tuberculosis (9-12),
pneumonia (13,14) and bronchiectasis (15).
4. Incidence
In total, 74 cases of bronchial Dieulafoy's disease
have been identified in the past 20 years since the first reported
case in 1995 (2,4-44).
Owing to the substantially low incidence of Dieulafoy's disease of
the bronchus, there have been no statistical reports of its exact
incidence. Among the patients reported, the youngest was 5 years
old, and the oldest was 85 years old. Subjects aged 30-70 years
were at a high risk, accounting for 80% of the total patients
(Table I). The male-to-female
incidence ratio was ~2:1 (45 male vs. 24 female patients), although
the reason for the sex differences in Dieulafoy's disease of the
bronchus is not clear.
 | Table IClinical features of bronchial
Dieulafoy's disease. |
Table I
Clinical features of bronchial
Dieulafoy's disease.
| | Treatment type and
outcome | |
|---|
| Authors, year | Age, years | Sex | Clinical
manifestations | Smoker | History of
hemoptysis | Localization of
hemoptysis | Embolization | Surgery | Medicine | Follow-up
period | Ref. |
|---|
| Sweerts et
al, 1995 | 35 | Female | Massive
hemoptysis | No | Yes | RLL | Failure | Success | NM | 4 months | (2) |
| | 59 | Male | Hemoptysis and
melaena | Yes | No | RLL | NM | Success | NM | NM | |
| Antoune et
al, 1998 | 45 | Male | Hemoptysis | NM | NM | RUL | NM | NM | NM | NM | (42) |
| | 56 | Male | Hemoptysis | NM | NM | LLL | NM | NM | NM | NM | |
| | 69 | Male | Hemoptysis | NM | NM | RUL | NM | NM | NM | NM | |
| van der Werf et
al, 1999 | 70 | Female | Acute lobar
pneumonia | Yes | Nes | LUL | Failure | Failure | Failure | NM | (16) |
| Stoopen et
al, 2001 | 51 | Male | Profuse hemoptysis
and epistaxis | Yes | NM | RML, RLL | NM | Success | NM | NM | (17) |
| Hope-Gill and
Prathibha, 2002 | 49 | Male | Increasing
hemoptysis | Yes | No | RML | Success | NM | NM | 12 months | (9) |
| Bhatia et
al, 2003 | 42 | Male | Recurrent
hemoptysis | Yes | No | LUL | Success | NM | NM | NM | (10) |
| Kuzucu et
al, 2005 | 28 | Male | Massive
hemoptysis | Yes | Yes | LLL | NM | Success | NM | 12 months | (11) |
| | 45 | Male | Massive
hemoptysis | Yes | Yes | RML | NM | Success | NM | 5 months | |
| Pomplun and Sheaff,
2005 | 32 | Male | Massive
hemoptysis | NM | No | RUL | Failure | Success | NM | NM | (5) |
| Loschhorn et
al, 2006 | 47 | Female | Hemoptysis | No | No | RML | NM | Success | NM | 6 years | (18) |
| | 52 | Female | Coughed up several
clots of blood | No | No | RLL | Success | NM | NM | NM | |
| Xie et al,
2006 | 28 | Female | Hemoptysis | No | No | LLL | NM | NM | Success | 5 years | (25) |
| Savale et
al, 2007 | 30 | NM | Hemoptysis | NM | Yes | NM | Failure | Success | NM | 47±35 months | (19) |
| | 31 | NM | Hemoptysis | NM | Yes | NM | Failure | Success | NM | 47±35 months | |
| | 32 | NM | Hemoptysis | NM | Yes | NM | Failure | Success | NM | 47±35 months | |
| | 33 | NM | Hemoptysis | NM | Yes | NM | Failure | Success | NM | 47±35 months | |
| | 34 | NM | Hemoptysis | NM | Yes | NM | Failure | Success | NM | 47±35 months | |
| Rennert et
al, 2007 | 51 | Male | Hemoptysis | Yes | Yes | LLL | NM | Success | NM | NM | (43) |
| Fields and De
Keratry, 2008 | 47 | Male | Hemoptysis | Yes | Yes | LMB | Success | NM | NM | 8 months | (44) |
| Parrot et
al, 2008 | 69 | Male | Hemoptysis | Yes | Yes | RUL | Success | NM | NM | 31 months | (7) |
| | 45 | Male | Hemoptysis | Yes | Yes | RUL | Success | NM | NM | 49 months | |
| | 54 | Male | Hemoptysis | Yes | No | LLL | Success | NM | NM | 96 months | |
| | 57 | Female | Hemoptysis | Yes | Yes | LUL | Success | NM | NM | 28 months | |
| | 49 | Male | Hemoptysis | Yes | No | LUL | Success | NM | NM | 25 months | |
| | 38 | Male | Hemoptysis | Yes | No | RLL | Success | NM | NM | 6 months | |
| | 68 | Female | Hemoptysis | Yes | Yes | RUL | Failure | Failure | Failure | 12 months | |
| Gharagozloo et
al, 2008 | 51 | Male | Hemoptysis | Yes | Yes | LLL | NM | Success | NM | NM | (13) |
| D'Souza and Sharma,
2010 | 63 | Female | Bronchiectasis and
chronic bronchitis | NM | NM | RML | NM | NM | NM | NM | (20) |
| Gurioli et
al, 2010 | 65 | Male | NM | No | NM | RLL | NM | NM | NM | NM | (21) |
| Barisione et
al, 2012 | 57 | Female | Massive
hemoptysis | No | Yes | RML or RLL | Success | NM | NM | NM | (6) |
| Kolb et al,
2012 | 44 | Female | Recurrent
hemoptysis | No | Yes | RML | Success | NM | NM | NM | (22) |
| Trisolini et
al, 2013 | 66 | Female | Recurrent
pneumonias | No | No | LLL | NM | Success | NM | NM | (15) |
| Yang et al,
2013) | 41 | Male | Repeated
hemoptysis | No | Yes | RML | Success | NM | NM | NM | (26) |
| | 36 | Male | Pulmonary
infection | NM | NM | RML, RLL | Failure | Failure | Failure | NM | |
| | 61 | Male | Hemoptysis (4
days) | NM | NM | RUL | NM | Success | NM | 5 years | |
| Fang et al,
2014 | 13 | Male | Massive
hemoptysis | No | Yes | RML, RLL | NM | Success | NM | 5 months | (23) |
| Smith et al,
2014 | 30 | Male | Massive
hemoptysis | No | Yes | RLL | NM | Success | NM | 22 months | (4) |
| Liu et al,
2014 | 18 | Female | Hemoptysis | No | Yes | RLL | NM | Success | NM | 60 months | (39) |
| | 23 | Male | Hemoptysis | Yes | No | LUL | NM | NM | Success | | |
| | 31 | Male | Cough and
hemoptysis | Yes | No | RLL | Success | NM | NM | 12 months | |
| | 33 | Female | Cough and
hemoptysis | No | Yes | RLL | Success | NM | Failure | 13 months | |
| | 36 | Female | Cough and
hemoptysis | No | Yes | RLL | Success | NM | Failure | 14 months | |
| | 47 | Female | Right chest
pain | No | No | RML | NM | NM | Success | 31 months | |
| Dalar et al,
2015 | 28 | Male | Recurrent
hemoptysis | Yes | Yes | LUL | Success | NM | NM | 2 years | (24) |
| Xia et al,
2015 | 31 | Male | Hemoptysis | Yes | NM | RML | Failure | Success | NM | 84 months | (40) |
| | 21 | Male | Hemoptysis | Yes | NM | RML | Failure | Success | NM | 73 months | |
| | 85 | Male | Hemoptysis | Yes | NM | LUL | Failure | Success | NM | 20 months | |
| | 63 | Male | Hemoptysis | No | NM | Lingula | NM | Success | NM | 70 months | |
| Padilla-Serrano
et al, 2015 | 49 | Female | Cough and abundant
blood expectoration | Yes | Yes | RLL | Success | NM | NM | Until 2015 | (41) |
| Hadjiphilippou
et al, 2017 | 47 | Male | Recurrent
hemoptysis | Yes | Yes | RLL | Success | NM | NM | NM | (28) |
| Madan et al,
2017 | 26 | Male | Hemoptysis | No | Yes | RLL | Success | NM | NM | 6 months | (29) |
| Niu et al,
2017 | 5 | Female | Hemoptysis | No | Yes | RUL | NM | NM | Success | 12 months | (30) |
| Wadji and
Farahzadi, 2017 | 16 | Female | Massive
hemoptysis | No | No | RLL | NM | Success | NM | 18 months | (31) |
| Yang et al,
2017 | 60 | Female | Frequent
hemoptysis | No | Yes | NM | Success | NM | NM | Until 2017 | (32) |
| Bonnefoy et
al, 2018 | 66 | Male | Massive hemoptysis,
acute respiratory failure | NM | NM | RUL | NM | Success | NM | 6 months | (33) |
| Minchole et
al, 2018 | 67 | Male | Dry cough and
progressive dyspnea | Yes | No | RML | NM | NM | Success | NM | (34) |
| Pan et al,
2018 | 76 | Female | Cough | No | NM | RUL, RML | NM | Success | NM | NM | (12) |
| | 66 | Male | Hemoptysis | Yes | NM | RUL, RML, RLL,
LLL | NM | NM | Success | NM | |
| | 51 | Male | Cough, sputum and
fever | Yes | NM | RUL, RML | NM | Success | NM | NM | |
| | 36 | Male | Frequent lung
infections | No | NM | RLL | NM | NM | Success | NM | |
| | 61 | Male | Hemoptysis | No | NM | RML | NM | NM | Success | NM | |
| | 41 | Male | Hemoptysis | Yes | NM | RML, RLL | NM | NM | Success | NM | |
| Sheth et al,
2018 | 51 | Female | Hemoptysis | No | NM | LLL | Success | NM | NM | 2 years | (8) |
| | 67 | Male | Hemoptysis | Yes | Yes | LLL | Success | NM | NM | 6 months | |
| Wang et al,
2018 | 21 | Female | Massive
hemoptysis | No | Yes | RLL | Success | NM | NM | 13months | (35) |
| Chen et al,
2019 | 18 | Female | Hemoptysis | No | Yes | RLL | Success | NM | NM | Until 2019 | (36) |
| | 72 | Female | Cough and abundant
blood expectoration | No | Yes | RLL | Failure | Failure | Failure | NM | |
| | 38 | Male | Recurrent
hemoptysis | No | Yes | LL | Success | NM | NM | 2 years | |
| Tang et al,
2019 | 67 | Male | Cough and
hemoptysis | NM | No | RML | Success | NM | NM | Until 2019 | (37) |
| White et al,
2019 | 69 | Male | Hemoptysis | No | Yes | RLL | Success | NM | NM | 6 months | (38) |
| Zhou et al,
2019 | 62 | Male | Intermittent
hemoptysis | Yes | Yes | LLL | Success | NM | NM | NM | (14) |
5. Lesion site
A total of 74 cases of Dieulafoy's disease of the
bronchus were summarized, including 48 in the right bronchus (19 in
the right lower lobe, 12 in the right middle lobe, 9 in the right
upper lobe, 5 in the right lower and middle lobes, 2 in the right
middle and upper lobes, and 1 in the entire right lung), 20 in the
left bronchus (11 in the left lower lobe, 1 in the left main
bronchus, 7 in the left upper lobe, and 1 in the left lung), 1 in
the lingula, and 6 in an unspecified location. An analysis of the
reported cases revealed that Dieulafoy's disease of the bronchus
commonly occurs in the right bronchus, and that patients with
lesions in the right bronchus account for approximately two-thirds
of the total cases. These differences may be due to the anatomical
characteristics of the bronchi. The right bronchus is short and
thick so that foreign bodies are more likely to enter and cause
infection, one of the potential causes of Dieulafoy's disease of
the bronchus. Therefore, biopsies should be performed with caution
to prevent hemorrhage in patients with cryptogenic hemoptysis if a
lesion (especially in the right bronchus) with similar
manifestations to Dieulafoy's disease is demonstrated by
bronchoscopy.
6. Clinical manifestations
Recurrent hemoptysis is a common symptom of
Dieulafoy's disease of the bronchus. The maximum amount of
hemoptysis has been reported as 2,000 ml, and is often without an
obvious cause (14). A previously
reported patient with Dieulafoy's disease presented with chest pain
and no hemoptysis; the latter only occurred after bronchoscopic
biopsy, and a definitive diagnosis was established by bronchial
angiography (39). Indeed, patients
with Dieulafoy's disease frequently visit the hospital with a cough
(12,36), infection (12,20) or
respiratory failure (33,34). In conclusion, the clinical symptoms
of Dieulafoy's disease of the bronchus are non-specific. Therefore,
physicians should not only pay more attention to patients with
massive hemoptysis, but also focus on patients with recurrent
respiratory symptoms.
7. Auxiliary examination
In Dieulafoy's disease of the bronchus, chest X-rays
and computed tomography (CT) scans are rarely positive for symptoms
other than the manifestation of an intrapulmonary hemorrhage and
the original lung disease. Only a few cases of endobronchial
nodules have been identified by chest CT examination (17). By contrast, multi-slice CT
angiography can clearly indicate the shape and direction of
bronchial pulmonary vessels, which may detect a tortuous and
dilated bronchial artery (22), and
may also demonstrate well-enhanced endobronchial nodules (25).
Owing to cryptogenic hemoptysis, most patients who
undergo bronchoscopic examination and bronchoscopy demonstrate
massive endobronchial hemorrhage, which may even be accompanied by
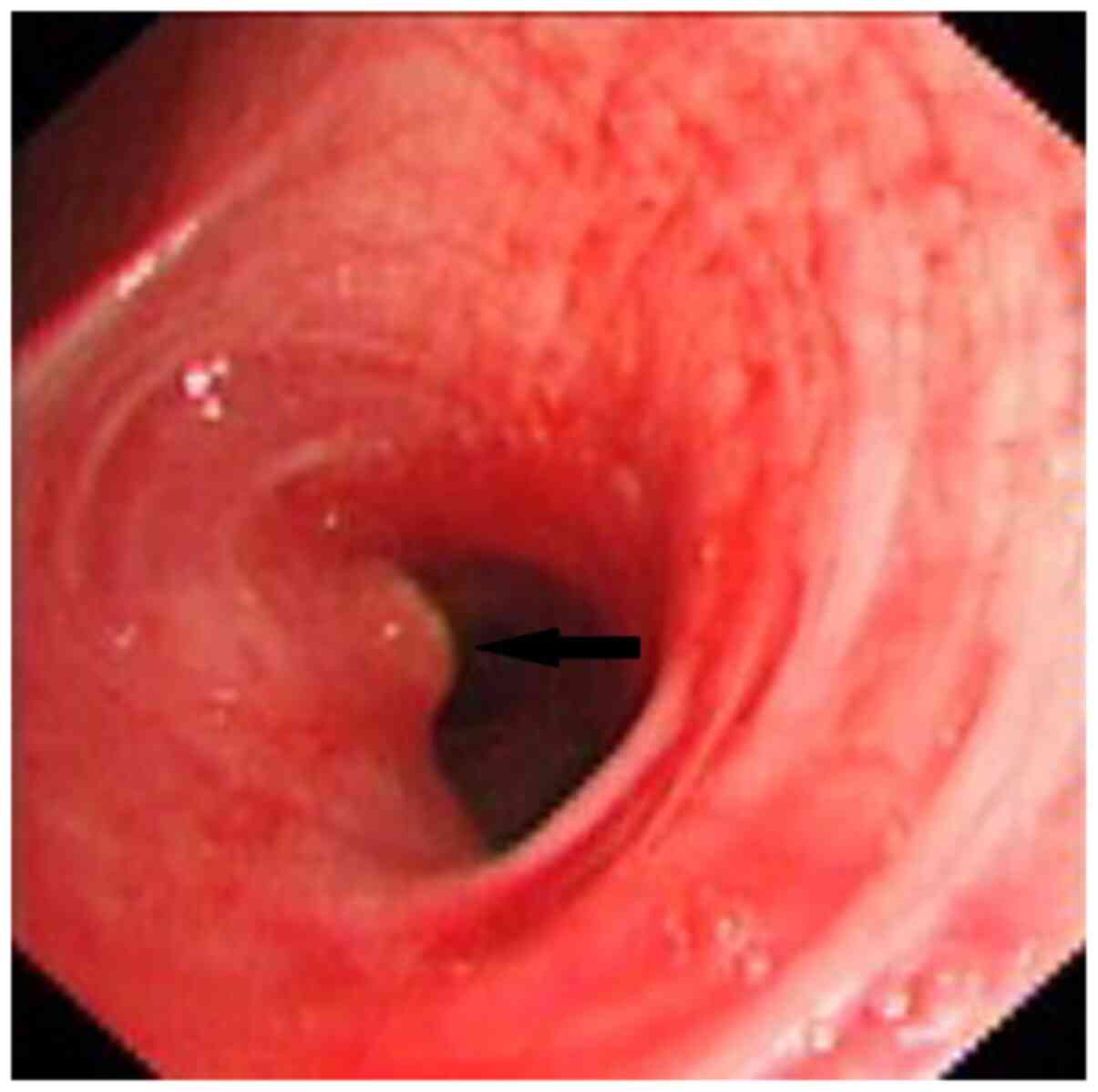
blood clot formation (12,36). Mucosal nodular projections can be a
few millimeters in diameter and height with a smooth surface
(36). The lesion may also be
congested and rough, with slight vascular pulsation in specific
cases. Sometimes the protruding surface is coated with yellow-white
exudate forming a ‘little white hat’-like shape, easily
misdiagnosed as an endobronchial tumor nodule (7) (Fig.
1). The nodule may show as a neoplasm-like granulation nodule,
leading to local obstruction of the bronchial lumen and causing
obstructive pneumonia. If the nodule is mistaken for a neoplasm,
subsequent biopsy may lead to a large hemorrhage and death by
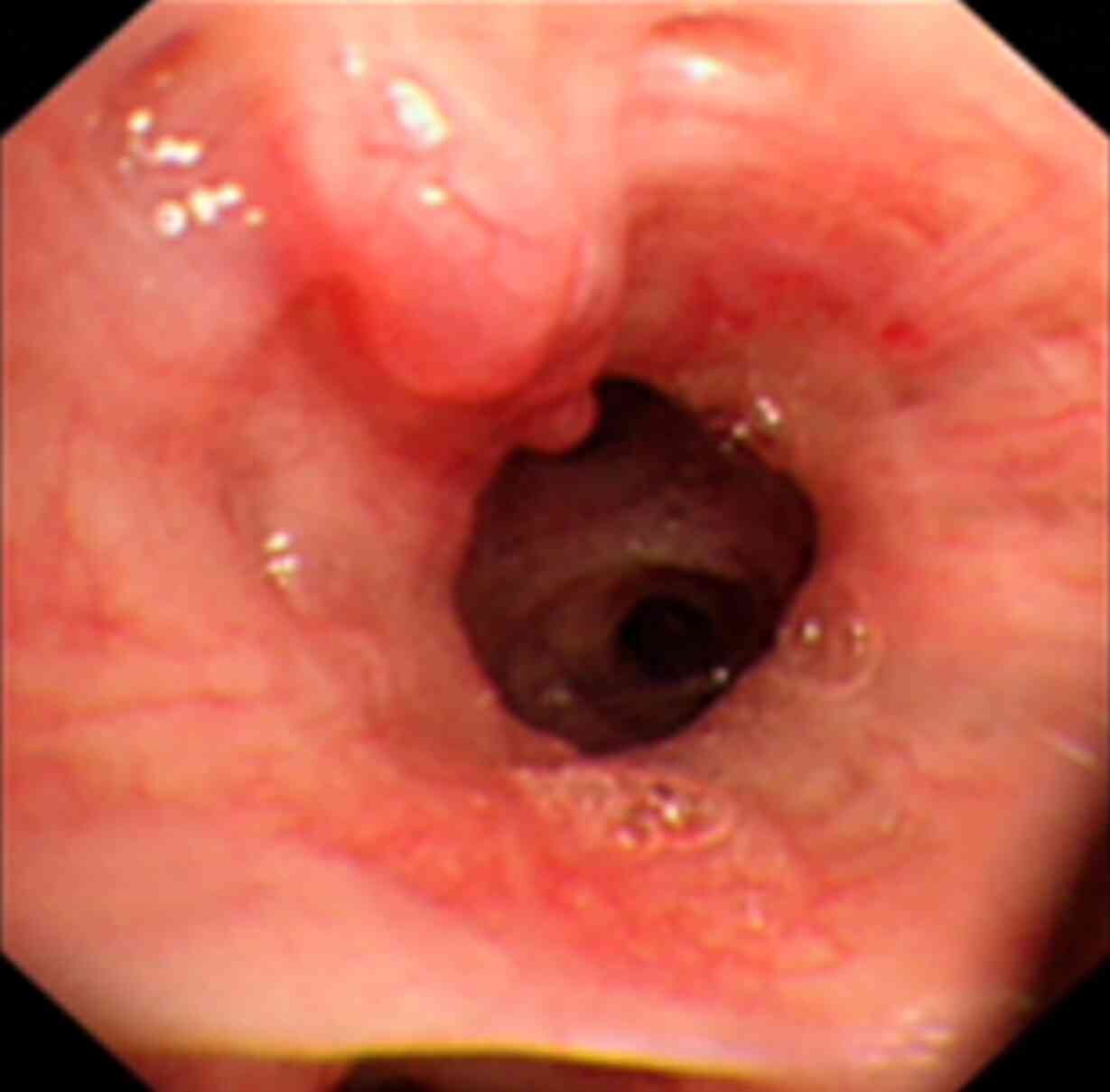
suffocation. Abnormal vessels in the submucosa can be tortuous and
dilated, and with a worm-like shape (Fig. 2), sometimes with fork-like ‘twigs’.
This type of case is easily mistaken for submucosal tumor
infiltration, and subsequent biopsies may lead to fatal hemorrhage.
As the bronchial cavity is filled with blood and blood clots, it is
difficult to find a small mucosal protrusion, or the mucosal
protrusion is localized below the subsegmental bronchus and thus
cannot be seen by conventional bronchoscopy.
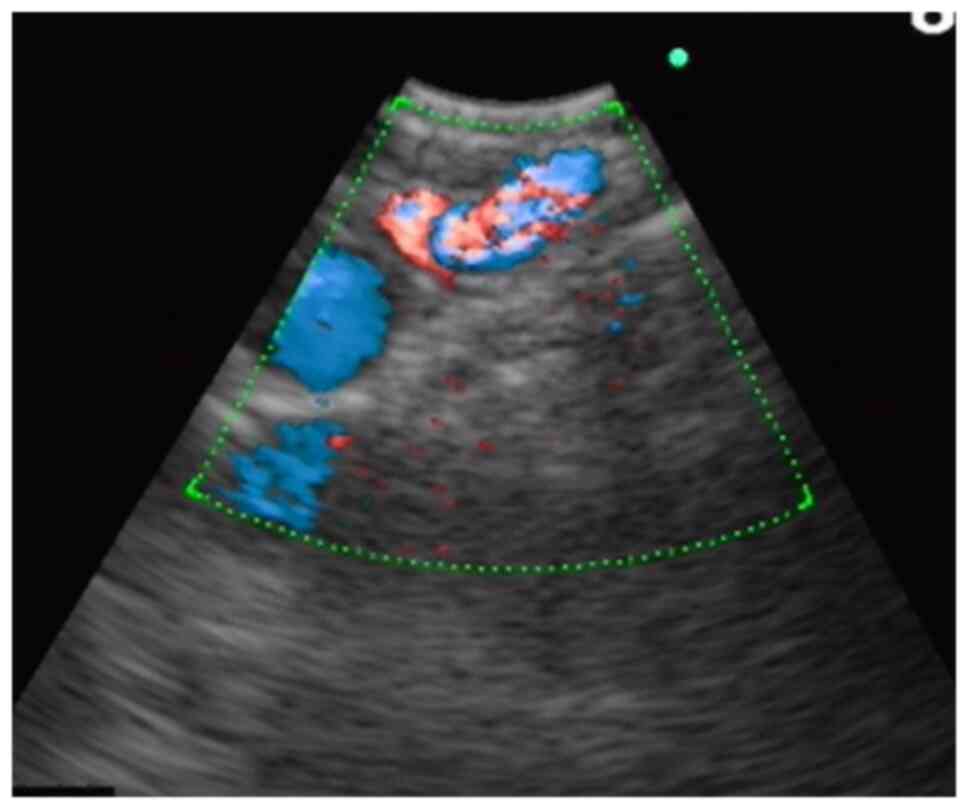
Bronchial angiography contributes to the diagnosis
of Dieulafoy's disease of the bronchus. Bronchial angiography shows
a rich blood supply in the corresponding site of the lesion
(23); the bronchial artery is
tortuous, dilated and deformed, with signs of bleeding (Fig. 3).
An endobronchial ultrasound can be used to clarify
the nature of any endobronchial protrusion. This technique helps to
clarify the nature of the nodular lesion and provides clues for
disease diagnosis. The major manifestation is a fluid echo-free
zone in the submucosal lesion, and the Doppler mode can be used to
detect blood flow (21) (Fig. 4).
8. Diagnosis
The possibility of Dieulafoy's disease of the
bronchus should be considered in patients with hemoptysis when
chest X-ray and CT examinations demonstrate no obvious
abnormalities other than pulmonary hemorrhage. Dieulafoy's disease
of the bronchus is largely diagnosed according to the presentations
of bronchoscopy, bronchial angiography and pathology of surgical or
autopsy specimens. Numerous researchers consider that pathological
examination of biopsies, surgical or autopsy specimens is required
for a definite diagnosis. However, there are no uniform diagnostic
criteria, and since pathological biopsies can lead to fatal
hemorrhages, the need for pathological diagnosis remains
controversial. In some cases, the diagnosis is based on the
manifestations revealed by bronchoscopy and bronchial angiography
(24,25,39).
Endobronchial ultrasonography (EBUS) is a new diagnostic method
used to detect the lesions of Dieulafoy's disease (21).
Bronchoscopy
Under bronchoscopy, a mucosal protrusion a few
millimeters in diameter and height is visible in the corresponding
site of the bleeding bronchus. On the top of the protrusion, the
mucosa turns white without a pulsating sensation; the surrounding
mucosa may be normal or slightly congested. In some cases, abnormal
blood vessels within the submucosa are tortuous and dilated in an
earthworm-like pattern, sometimes presenting with a purple nodular
shape (39). To prevent
uncontrollable hemorrhage, caution must be taken during biopsy if
Dieulafoy's disease is suspected (based on the results of
bronchoscopy). Yang et al (26) analyzed the clinical data of 22
patients with Dieulafoy's disease, including 12 with hemorrhage
during biopsy. Bleeding stopped in eight patients after local
hemostasis, and in two after lobectomy of the diseased lobe;
another two patients died of massive hemorrhage. The remaining 10
patients did not undergo bronchoscopic biopsy. Our previous study
reported the cases of six patients, including two undergoing
bronchoscopic biopsy, both of whom suffered hemorrhage; the maximum
amount of hemorrhage was ~1,000 ml, and bleeding stopped in both
cases after selective bronchial artery embolization (39). Since 2014, with an improvement of
the understanding of Dieulafoy's disease, biopsy has been avoided
for nodules suspected to be caused by Dieulafoy's disease in the
trachea (23,41), which has effectively reduced the
probability of massive hemorrhage in Dieulafoy's disease.
Bronchial angiography
As aforementioned, bronchial angiography can be used
to indicate the rich blood supply to the corresponding site of the
lesion. The bronchial artery is tortuous, dilated and deformed,
with signs of bleeding (39).
Multi-slice CT angiography of the
bronchial or pulmonary artery
This technique is used to visualize an abnormal
bronchial artery associated with tortuosity and dilation (22), and sometimes detects well-enhanced
endobronchial nodules (25). A CT
value of >100 for the enhanced lesion should be considered to
indicate a vascular lesion.
Endobronchial ultrasound
When convex probe EBUS is used to detect blood flow
within a lesion, it often shows a fluid echo-free zone in
submucosal lesions; the blood flow can be displayed in the color or
energy Doppler mode (21). Owing to
its large diameter, convex probe EBUS cannot reach the upper lobe
bronchus or segmental bronchus. Alternatively, radial probe EBUS
can be used to examine the lesion. However, the latter approach has
no Doppler mode and thus cannot determine blood flow within the
lesion. Nonetheless, radial probe EBUS can indicate an echo-free
zone, which may be considered for vascular lesions in patients with
hemoptysis.
Narrow-band imaging
Wang et al (45) reported that narrow band imaging
(NBI) can display endobronchial lesions such as bronchial
artery-pulmonary artery fistulae. Thickened blood vessels and
capillaries are tortuous and disordered in the submucosa of the
lesion site. However, there have been no studies to assess the
diagnostic value of NBI in Dieulafoy's disease.
Pathological examination
Pathology or autopsy pathology presents with
arterial malformation in the bronchial submucosa. The tortuous,
dilated, deformed artery forms small nodules coated with bronchial
mucosa, protrudes from the bronchial lumen, and is only a few
millimeters in diameter and height. In some cases, deformed blood
vessels have an opening within the bronchial lumen, or the diseased
bronchus is surrounded by rich blood vessels, some of which invade
the bronchial wall and directly reach the submucosa (5). A diagnosis of Dieulafoy's disease
depends on the results of pathological examination. However, since
this can easily lead to massive bleeding, its use has been limited.
Therefore, the incidence of Dieulafoy's disease may have been
underestimated.
9. Differential diagnosis
Dieulafoy's disease and endobronchial hemorrhagic
lesions are primarily distinguished by differential diagnosis.
Additionally, the disease must be distinguished from early
endobronchial cancer to avoid misdiagnosis.
Bronchial arteriovenous malformation
(46)
Bronchial arteriovenous malformation can manifest as
an endobronchial vascular lesion. The presence of abnormal blood
vessels in the lesion can be demonstrated by EBUS or NBI, but it is
difficult to distinguish via bronchoscopy. Bronchial angiography
can be used to clarify the communication between the bronchial
artery and the pulmonary circulation or cavernous hemangioma.
Bronchial artery aneurysm (47)
Bronchial artery aneurysm can manifest as an
endobronchial vascular lesion. This condition can be distinguished
from Dieulafoy's disease by bronchial angiography or multi-slide CT
angiography as an aneurysm-like dilation of the bronchial
artery.
Lobular capillary hemangioma (48)
This condition has no typical symptoms other than
hemoptysis. Intraluminal neoplasms can be seen under bronchoscopy.
Ulcers and bleeding are visible on the surface and are difficult to
distinguish from Dieulafoy's disease of the bronchus. The
differential diagnosis primarily relies on pathological
examination.
Tracheal capillary hemangioma
(49)
In general, tracheal capillary hemangioma is similar
to tracheal lobular capillary hemangioma and Dieulafoy's disease of
the bronchus in terms of clinical manifestations, laboratory
examination results, imaging and endoscopy. The differential
diagnosis primarily relies on pathological examination.
Early cancer
If Dieulafoy's disease is suspected based on
bronchoscopy, and the possibility of early cancer cannot be ruled
out, NBI and EBUS may be used to determine the presence of
thickened and abnormally tortuous and disordered vessels within the
lesion. Fluorescence bronchoscopy preliminarily determines the
malignancy of the lesion.
10. Treatment and prognosis
Existing methods for the treatment of Dieulafoy's
disease of the bronchus include conservative internal medication,
selective bronchial artery embolization (SBAE), pulmonary lobectomy
and argon plasma coagulation via bronchoscopy. Currently, SBAE is
the preferred surgical approach, and lobectomy of the diseased lobe
is used following embolization failure or recurrent
post-embolization hemoptysis. Only one case of argon plasma
coagulation via bronchoscopy has been reported (24).
Medication
As the condition presents with bleeding caused by
the rupture of the bronchial or pulmonary artery, internal
treatment with hemostatic agents often has poor efficacy for
Dieulafoy's disease of the bronchus (39). However, for individual patients,
pituitrin and thrombin may occasionally demonstrate good
therapeutic effects (30).
Bronchoscopic treatment
Topical application of hemostatic drugs under
bronchoscopy also has poor efficacy. To date, only Dalar et
al (24) has reported the
success of treating one patient with Dieulafoy's disease of the
bronchus by argon plasma coagulation via bronchoscopy. However, the
patient underwent no bronchial angiography or pathological
diagnosis, and Dieulafoy's disease of the bronchus was diagnosed
based solely on the presentations under bronchoscopy. Thus, the
diagnosis of that patient remains controversial. In Dieulafoy's
disease, once blood vessels rupture and bleed, the hemorrhage is
fast and massive, resulting in an unclear field of view under
bronchoscopy. Hence, it is our belief that bleeding from
Dieulafoy's disease is not suited to dotted electrocoagulation and
superficial hemostasis by argon-beam-coagulator burning, laser
treatment and freezing under bronchoscopy. Nevertheless, this
approach is feasible to remove blood clots that block the bronchial
lumen and to clarify the bleeding site under bronchoscopy, thereby
determining the lesion site for bronchial angiography or surgery.
The use of a Dumon silicone stent for compression was reported in a
patient with Dieulafoy's disease of the left main bronchus, and the
patient was followed up for 8 months without recurrent hemorrhage
(44). This study indicated that
hemostasis by stent compression may be an alternative treatment
option. Additionally, a bronchoscopic balloon can be used to
compress the bronchus at the bleeding site to provide preparation
time for SBAE. For the treatment of gastrointestinal Dieulafoy's
disease, coagulant injection under digestive endoscopy can be used
for hemostasis. However, no study has reported the use of this
method for Dieulafoy's disease of the bronchus, thus the
feasibility, safety and efficacy of the method are currently
undetermined.
SBAE
The SBAE procedure is effective in most patients
with Dieulafoy's disease of the bronchus; however, hemoptysis may
recur after surgery. Bhatia et al (10) reported the case of one patient with
recurrent hemorrhage who had undergone SBAE seven times. Patients
with abnormal blood vessels from the pulmonary artery are often
non-responsive to SBAE. In our previous repor (39), all six patients with Dieulafoy's
disease of the bronchus underwent SBAE at the corresponding site of
hemorrhage. Hemorrhage was stopped in one patient following SBAE,
who then underwent a pulmonary lobectomy; the other five patients
all underwent SBAE and were followed up for 1 to 5 years.
Furthermore, hemoptysis was not recurrent in four of the patients,
though one patient did experience relapse.
Surgical treatment
In cases of SBAE failure, SBAE for hemoptysis
relapse or no SBAE treatment, a lobectomy may be performed at the
corresponding site of the lesion. Hemoptysis is unlikely to recur
following resection of the diseased lung lobe. In a report by Yang
et al (26), 13 patients
underwent lobectomy of the diseased lobe; 12 did not experience
recurrent hemoptysis, and one died due to hemorrhage after
bronchoscopic biopsy, but not due to surgery.
11. Conclusions
Dieulafoy's disease of the bronchus lacks
specificity in clinical symptoms and primarily presents as massive
hemoptysis, although other respiratory or cardiovascular symptoms
may also occur. Due to its relative rarity, respiratory physicians
currently lack sufficient awareness of Dieulafoy's disease of the
bronchus, thus the disease is likely to be missed or misdiagnosed.
Serious consequences may result if attention is not paid to the
diagnosis and treatment process. In particular, when local
protrusion changes are found in the lumen during routine
bronchoscopy, physicians perform routine biopsies which can cause
fatal bleeding. Therefore, to rule out the possibility of
Dieulafoy's disease of the bronchus, bronchial angiography,
multi-slice CT angiography, EBUS and NBI examinations must be
considered for patients undergoing bronchoscopy who present with
cryptogenic hemoptysis and/or smooth protrusion within the
bronchial lumen resembling Dieulafoy's disease (even those who do
not experience hemoptysis). Biopsy must be prohibited if bronchial
angiography demonstrates: i) The presence of a bronchial artery
with abnormal tortuosity and dilation, as well as rupture and
bleeding at the lesion site; ii) an enhanced CT value >100 for
the lesion; or iii) EBUS and NBI results of abnormal blood flow
within the lesion. Caution must be taken during bronchoscopic
operations, such as biopsy and brushing, to prevent asphyxial
hemorrhage. At present, SBAE and pulmonary lobectomy are the
primary treatment methods for Dieulafoy's disease of the bronchus,
although conservative drug treatment and flexible bronchoscope
argon plasma coagulation have also been successfully used. SBAE can
retain part of the function of the diseased lung, but may result in
relapse following treatment. Lobectomy is a radical cure for
Dieulafoy's disease, although complete removal of the diseased lung
may affect the patient's quality of life. Thus, clinicians must
assess the advantages and disadvantages, and select the most
appropriate treatment method depending on the physical
manifestations of each patient.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Special and
Joint Program of the Yunnan Provincial Science and Technology
Department and Kunming Medical University [grant no.
2018FE001(-206)], the Yunnan Health Training Project of High Level
Talents (grant no. and H-2018095), the Young Academic and Technical
Leaders of Yunnan Province (grant no. 2017HB053), the Science and
Technology Program for Public Wellbeing of Yunnan Province (grant
no. 2014RA020).and the Famous Doctors of High-level Talent Training
Support Program of Yunnan Province (grant nos. YNWR-MY-2020-013 and
YNWR-MY-2020-027).
Availability of data and materials
Not applicable.
Authors' contributions
XX and JY were the primary contributors to the
writing of the manuscript. SX and JL contributed to the diagnosis
and differential diagnosis of bronchial Dieulafoy's disease. YD
designed the study and made important revisions to the manuscript.
Data authentication is not applicable. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patients provided consent for publication of the
figures included in the manuscript.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dieulafoy G: Exulceratio simplex: Surgical
intervention in overwhelming haematemesis following simple
exulceration of the stomach. Bull Acad Med. 49:49–84. 1898.
|
|
2
|
Sweerts M, Nicholson AG, Goldstraw P and
Corrin B: Dieulafoy's disease of the bronchus. Thorax. 50:697–698.
1995.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Qian X, Du Q, Wei N, Wang M, Wang H and
Tang Y: Bronchial Dieulafoy's disease: A retrospective analysis of
73 cases. BMC Pulm Med. 19(104)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Smith B, Hart D and Alam N: Dieulafoy's
disease of the bronchus: A rare cause of massive hemoptysis.
Respirol Case Rep. 2:55–56. 2014.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Pomplun S and Sheaff MT: Dieulafoy's
disease of the bronchus: An uncommon entity. Histopathology.
46:598–599. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Barisione EE, Ferretti GG, Ravera SS and
Salio MM: Dieulafoy's disease of the bronchus: A possible mistake.
Multidiscip Respir Med. 7(40)2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Parrot A, Antoine M, Khalil A, Théodore J,
Mangiapan G, Bazelly B and Fartoukh M: Approach to diagnosis and
pathological examination in bronchial Dieulafoy disease: A case
series. Respir Res. 9(58)2008.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sheth HS, Maldonado F and Lentz RJ: Two
cases of Dieulafoy lesions of the bronchus with novel comorbid
associations and endobronchial ablative management. Medicine
(Baltimore). 97(e9754)2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hope-Gill B and Prathibha BV:
Bronchoscopic and angiographic findings in Dieulafoy's disease of
the bronchus. Hosp Med. 63:178–179. 2002.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bhatia P, Hendy MS, Li-Kam-Wa E and Bowyer
PK: Recurrent embolotherapy in Dieulafoy's disease of the bronchus.
Can Respir J. 10:331–333. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kuzucu A, Gürses I, Soysal O, Kutlu R and
Ozgel M: Dieulafoy's disease: A cause of massive hemoptysis that is
probably underdiagnosed. Ann Thorac Surg. 80:1126–1128.
2005.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pan F, Wang F, Liu Z, Yuan F, Sun KK, Gao
ZC and Sun Y: The computed tomography angiography features of
Dieulafoy disease of the bronchu]. Zhonghua Jie He He Hu Xi Za Zhi.
41:949–953. 2018.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
13
|
Gharagozloo F, Rennert D, Margolis M,
Tempesta B, Schwartz A, Cole V and Wang KP: Dieulafoy lesion of the
bronchus: Review of the literature and report of the 13th case. J
Bronchol. 15:38–40. 2008.
|
|
14
|
Zhou P, Yu W, Chen K, Li X and Xia Q: A
case report and review of literature of Dieulafoy's disease of
bronchus: A rare life-threatening pathologic vascular condition.
Medicine (Baltimore). 98(e14471)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Trisolini R, Cancellieri A and Patelli M:
Life-threatening bleeding after endobronchial biopsy in a patient
with bronchiectasis. Am J Respir Crit Care Med. 188:e9–e10.
2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
van der Werf TS, Timmer A and Zijlstra JG:
Fatal haemorrhage from Dieulafoy's disease of the bronchus. Thorax.
54:184–185. 1999.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Stoopen E, Baquera-Heredia J, Cortes D and
Green L: Dieulafoy's disease of the bronchus in association with a
paravertebral neurilemoma. Chest. 119:292–294. 2001.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Löschhorn C, Nierhoff N, Mayer R,
Zaunbauer W, Neuweiler J and Knoblauch A: Dieulafoy's disease of
the lung: A potential disaster for the bronchoscopist. Respiration.
73:562–565. 2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Savale L, Parrot A, Khalil A, Antoine M,
Théodore J, Carette MF, Mayaud C and Fartoukh M: Cryptogenic
hemoptysis: From a benign to a life-threatening pathologic vascular
condition. Am J Respir Crit Care Med. 175:1181–1185.
2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
D'Souza F and Sharma R: Dieulafoy's
disease of the bronchus. Pathology. 42:683–684. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gurioli C, Casoni GL, Gurioli C,
Tomassetti S, Romagnoli M, Ravaglia C and Poletti V: Endobronchial
ultrasound in Dieulafoy's disease of the bronchus: An additional
application of EBUS. Monaldi Arch Chest Dis. 73:166–168.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kolb T, Gilbert C, Fishman EK, Terry P,
Pearse D, Feller-Kopman D and Yarmus L: Dieulafoy's disease of the
bronchus. Am J Respir Crit Care Med. 186(1191)2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Fang Y, Wu Q and Wang B: Dieulafoy's
disease of the bronchus: Report of a case and review of the
literature. J Cardiothorac Surg. 9(191)2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Dalar L, Sökücü SN, Özdemir C, Büyükkale S
and Altın S: Endobronchial argon plasma coagulation for treatment
of Dieulafoy disease. Respir Care. 60:e11–e13. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Xie BS, Chen YS, Lin MF, Huang QH and Lin
ZS: Dieulafoy's disease of the bronchus: A case report and review
of the literature. Zhonghua Jie He He Hu Xi Za Zhi. 29:801–803.
2006.PubMed/NCBI(In Chinese).
|
|
26
|
Yang RH, Li JF, Liu J, Sun KK, Cao ZL and
Gao ZC: Dieulafoy disease of the bronchus: 3 cases report with
literature review. Zhonghua Jie He He Hu Xi Za Zhi. 36:577–580.
2013.PubMed/NCBI(In Chinese).
|
|
27
|
Liu FL, Chen EG, Zhou P, Jin M, Yang L and
Ying KJ: Tracheal lobular capillary hemangioma: Two case report and
review of the literature. Zhonghua Jie He He Hu Xi Za Zhi.
33:849–852. 2010.PubMed/NCBI(In Chinese).
|
|
28
|
Hadjiphilippou S, Shah PL, Rice A, Padley
S and Hind M: Bronchial dieulafoy lesion. A 20-year history of
unexplained hemoptysis. Am J Respir Crit Care Med.
195(397)2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Madan K, Dhungana A, Hadda V, Mohan A and
Guleria R: Flexible bronchoscopic argon plasma coagulation for
management of massive hemoptysis in bronchial Dieulafoy's disease.
Lung India. 34:99–101. 2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Niu HL, Yi P, Wang H, Wang FH, Liu W, Gao
Q, Chen ZR, Xia JQ and Zeng RX: Infantile Dieulafoy's disease of
bronchus: Report of a case. Zhonghua Bing Li Xue Za Zhi.
46:731–732. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
31
|
Wadji MB and Farahzadi A: Dieulafoy's
disease of the bronchial tree: A case report. Sao Paulo Med J.
135:396–400. 2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Yang D, Rong C, Gu J, Xu L, Zhang J, Zhang
G and Shen C: Dieulafoy disease of the trachea with recurrent
episodes of massive hemoptysis: A case report. Medicine
(Baltimore). 96(e5855)2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Bonnefoy V, Garnier M, Tavolaro S, Antoine
M, Assouad J, Fartoukh M and Gibelin A: Bronchial Dieulafoy's
disease: Visualization of embolization particles in bronchial
aspirate. Am J Respir Crit Care Med. 198:954–955. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Mincholé E, Penin RM and Rosell A: The
utility of linear endobronchial ultrasound for the incidental
finding of Dieulafoy disease of the bronchus. J Bronchology Interv
Pulmonol. 25:e48–e50. 2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Wang F, Kuang TG, Wang JF and Yang YH: A
rare cause of recurrent fatal hemoptysis: Dieulafoy's disease of
the bronchus. Chin Med J (Engl). 131:2758–2759. 2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Chen W, Chen P, Li X, Gao X and Li J:
Clinical characteristics and treatments for bronchial Dieulafoy's
disease. Respir Med Case Rep. 26:229–235. 2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Tang P, Wu T, Li C, Lv C, Huang J, Deng Z
and Ding Q: Dieulafoy disease of the bronchus involving bilateral
arteries: A case report and literature review. Medicine
(Baltimore). 98(e17798)2019.PubMed/NCBI View Article : Google Scholar
|
|
38
|
White C, Ottaviano P, Munn N, Shweihat Y
and Zeid F: Massive hemoptysis due to recurrence of bronchial to
pulmonary vascular malformation: A case report. Respir Med Case
Rep. 26:248–250. 2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Liu Y, Li Y, Xing X, Xiao Y, Li Z, Yang Y
and Wu X: Diagnosis and treatment of Dieulafoy's disease of the
bronchus. China J Endosc. 20:795–799. 2014.
|
|
40
|
Xia XD, Ye LP, Zhang WX, Wu CY, Yan SS,
Weng HX, Lin J, Xu H, Zhang YF, Dai YR, et al: Massive cryptogenic
hemoptysis undergoing pulmonary resection: Clinical and
pathological characteristics and management. Int J Clin Exp Med.
8:18130–18136. 2015.PubMed/NCBI
|
|
41
|
Padilla-Serrano A, Estrella-Palomares V,
Martinez-Palacios B and Gonzalez-Spinola J: A case of massive
hemoptysis related to a smoking-history: An acquired form of the
Dieulafoy's disease? Rev Port Pneumol. 21:276–279. 2015.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Antoune M, Maniacal G, Bazelly B, et al:
Dieulafoy's vascular malformation of the bronchus report of 3
cases. In: 1998 Annual Meeting of the United States and Canada
Academy of Pathology. 11(171)1998.
|
|
43
|
Rennert D, Gharagozloo F, Schwartz AM,
Margolis M, Tempesta B and Wu J: Dieulafoy's lesion of the
bronchus: Report of a case and review of the literature. Pathol
Case Rev. 12:93–95. 2007.
|
|
44
|
Fields EL and De Keratry DR: Dieulafoy
disease of the bronchus: Case report and presentation of a novel
therapeutic modality. J Bronchology Interv Pulmonol. 15:107–109.
2008.
|
|
45
|
Wang T, Zhang J, Wang Y, Pei Y, Xu M and
Zhang C: Diagnosis of bronchial artery - pulmonary artery fistula
by the combination of narrow band imaging with bronchial
arteriography: A case report. Zhonghua Jie He He Hu Xi Za Zhi.
38:148–149. 2015.
|
|
46
|
Sharifi M, Messersmith R, Newman B, Chung
Y and Lakier JB: Bronchial arteriovenous malformation in a child
with hemoptysis. A case report. Angiology. 47:203–209.
1996.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Cerezo Lajas A, Rodríguez Guzmán MDC and
de Miguel Díez J: Left Bronchial Artery Aneurysm. Arch
Bronconeumol. 55(215)2019.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
48
|
Dermawan JK, Ko JS and Billings SD:
Intravascular Lobular Capillary Hemangioma (Intravascular Pyogenic
Granuloma): A Clinicopathologic Study of 40 Cases. Am J Surg
Pathol: Jun 2, 2020 (Epub ahead of Print). doi:
10.1097/PAS.0000000000001509.
|
|
49
|
Özgül MA, Tanrıverdi E, Gül Ş, Asuk ZY,
Acat M, Abbaslı K, Fener NA and Çetinkaya E: A Rare Cause of
Hemoptysis in Childhood: Tracheal Capillary Hemangioma. Turk Thorac
J. 18:131–133. 2017.PubMed/NCBI View Article : Google Scholar
|