Introduction
Among all pediatric benign bone tumor lesions,
osteochondroma has the highest incidence, being estimated at
~20-35% of all pediatric benign tumors, or ~10-15% of all bone
tumor lesions (benign, tumor-like or malignant) (1-3).
This pathology is characterized by a bone outgrowth covered by
cartilaginous tissue that is localized on the external surface of
the bone. The lesion is distinguished by the presence of its own
medullary cavity, which is continued within the main bone medullary
cavity. The bone tissue found in the structure of the lesion
results from the endochondral ossification of the cartilage of
origin (4). Osteochondromas can be
present in either solitary or multiple forms (1,2) and
they usually occur in the region of the metaphysis of long bones in
immature skeletons, thus causing deformities (5). Although these lesions may present with
a characteristic radiological aspect, they can also have atypical
localizations or may become malignant, which makes imaging
diagnosis difficult (5).
Apart from malignant transformations,
osteochondromas can present with a series of complications,
including fractures in pedunculated lesions, vascular lesions such
as formation of pseudoaneurysms, neurological complications such as
peripheral nerves compression or formation of a bursa affecting the
cartilaginous surface of the lesion and results from local friction
(5,6).
The present retrospective study aimed to analyze the
association between the accuracy of medical imaging techniques and
histopathological examinations of osteochondroma in order to
determine a final diagnosis in patients with this pathology.
Materials and methods
The present retrospective study was conducted to
determine the degree of accuracy of imaging diagnostic procedures
in pediatric patients presenting with a positive histopathological
diagnosis of osteochondroma.
In this study, we initially selected 66 patients
showing radiological aspects of osteochondroma. From these 66
patients, only 56 patients with a positive histopathological
diagnosis of osteochondroma were included. Patients were aged
between 2 and 16 years, and 32 were men and 24 were females. The
clinicopathological data were obtained from the records of each
patient treated at the Craiova County Hospital Pediatric Surgery
Department between June 2014 and November 2019.
The inclusion criteria were as follows: Patients
aged 0-18 years examined in the Pediatric Surgery Department, with
the presence of at least one imaging examination and presence of a
positive histopathological examination. There were no exclusion
criteria. Conventional radiography of the involved areas in
anteroposterior and lateral projections was used and, depending on
the characteristics of each case, computerized tomography (CT)
scans and magnetic resonance imaging (MRI) examinations were
performed. In order for the final diagnosis to be confirmed,
histopathological examinations of biopsy samples were conducted.
Biological material consisted of specimens collected during core
needle biopsies performed under local anesthesia as outpatient
procedures. The samples were then transferred to the Anatomic
Pathology Department, where they underwent a fixation process using
10% buffered formalin and then processed by the classical HP
technique consisting in paraffin embedding and hematoxylin and
eosin staining. The microscope slides were analyzed under an
optical microscope.
Results
The present study included a cohort of 66 patients,
with only 56 patients meeting the criteria. Certain patient details
were taken into consideration, including age, sex, lesion
localization, lesion imaging semiotics and histopathological
aspects. From the 56 patients, 24 were male (43%) and 32 were
female (57%).
With regards to the age of the patients, this study
included individuals aged between 2 and 16 years, with a mean age
of 10 years and 10 months (10 years and 8 months for female
patients and 11 years for male patients). The median age was 10±2
years and the interquartile range was 25-75%.
Osteochondroma is a lesion that is frequently
diagnosed either in solitary or multiple forms. In the present
study, we discovered that the majority of osteochondromas diagnosed
were solitary (89%), while the multiple form was present in only
11% of the cases (Fig. 1; Table I). Although the number of patients
diagnosed with multiple osteochondroma was small, we noticed a
higher incidence among female patients in comparison with male
patients (66 and 33%, respectively).
 | Table IIncidence of osteochondroma
localization, type and form reported in patients from the present
study. |
Table I
Incidence of osteochondroma
localization, type and form reported in patients from the present
study.
| Osteochondroma
localization | Incidence, % |
|
Left
scapula | 11 |
|
Right
scapula | 6 |
|
Humerus
(left and right) | 5 |
|
Left
femur | 28 |
|
Right
femur | 11 |
|
Left
tibia | 17 |
|
Right
tibia | 11 |
|
Peroneus
(left and right) | 5 |
|
Hallux (left
and right) | 6 |
| Osteochondroma
type | |
|
Pedunculated | 72 |
|
Sessile | 28 |
| Osteochondroma
form | |
|
Solitary | 89 |
|
Multiple | 11 |
Regarding lesion localization, the study highlighted
a possible tendency of osteochondromas to occur in certain regions,
including femur (39%), tibia (28%), scapula (17%), hallux (6%),
peroneus (5%) and humerus (5%; Table
I). Furthermore, 66% of patients presented these benign lesions
on the left side of the body.
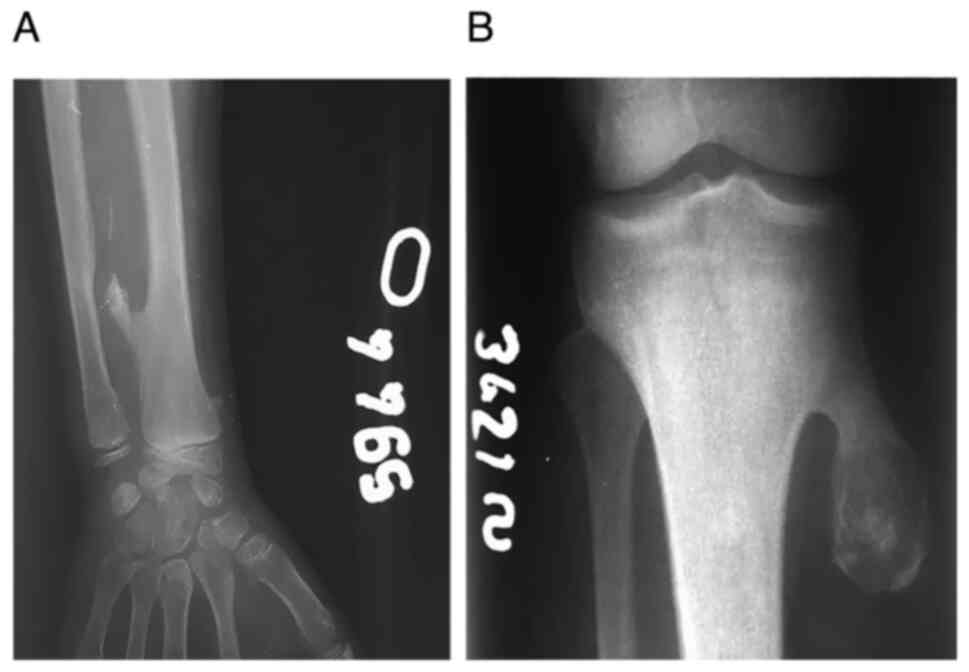
The type of osteochondroma, which could be either be
sessile or pedunculated, is another important aspect of imaging
semiotics. In this study, 28% of patients presented with sessile
osteochondroma, while the rest of the patients were diagnosed with
pedunculated type osteochondroma (Fig.
2; Table I).
It is important to emphasize that only some of the
examined patients complained of pain or local edema, while the rest
of the patients were incidentally diagnosed with osteochondroma
after some traumatic episodes. Therefore, 16 patients (28.5%)
presented with complaints such as local edema or pain. The 40
remaining patients (71.5%) were diagnosed after traumatic
incidents, some of them with fractures associated with these
lesions (Fig. 3).
Initially, the present study included 66 patients
that presented with imaging aspects of osteochondroma. From these
66 patients, only 56 had a confirmed histopathological diagnosis of
osteochondroma. It is therefore worth noticing that imaging
examinations have a 100% sensibility, although their accuracy is
84%. Thus, imaging diagnosis failed in 16% of cases. This was
mainly because in 10 patients the diagnosis of osteochondroma was
not confirmed. In these 10 patients, the differential diagnosis was
made with the supracondylar spur (in solitary forms) or with
metachondromatosis (in multiple forms).
Discussion
Osteochondroma is one of the most common benign bone
tumors. An important characteristic of this lesion is the presence
of the cartilaginous envelope, which covers the cortex and the
medullary canal of the subjacent bone. Lichtenstein and Muller's
theory suggested that the periosteum could have the potential to
form chondroblasts and osteoblasts due to a high turnover rate.
Thus, an osteochondroma may arise due to induced or spontaneous
change in periosteal cell differentiation. This theory is often
presented in literature and cited by multiple authors (7-11),
while other authors (2,12,13)
considered that these lesions might appear either spontaneously or
in relation to external factors such as irradiation, fractures or
after surgical interventions.
Regarding the sex of the patients, the results
obtained in our study were slightly different from the ones
presented by Kannan et al (14) showing a higher incidence of
osteochondromas among male patients. Furthermore, Tong et al
(15) reported that the incidence
of osteochondromas was twice higher in male patients compared with
female patients.
With regards to the age of the patients, the data
from our study were similar to those reported in previous studies.
In the present study, most patients were diagnosed between 8 and 12
years of age, which is what Kannan et al (14), de Souza and Bispo Júnior (5) and Kitsoulis et al (7) also reported.
Many authors suggested that solitary osteochondromas
occur as a consequence of an abnormal growth process causing the
herniation of a fragment of the growth plate in the periosteum
area. Consequently, the lesion will appear in the metaphysis region
either in a sessile or a pedunculated form (1). With respect to the origin of multiple
hereditary osteochondromatosis, previous studies suggested that a
mutation in the tumor suppressing genes exostosin
glycosyltransferase 1 and exostosin glycosyltransferase 2 could be
the cause of this pathology. These genes are responsible for the
synthesis of heparan sulfate proteoglycans (HSPGs), thus any
mutation would lead to a reduction in HSPGs synthesis, facilitating
therefore the occurrence of multiple hereditary osteochondromatosis
(16,17).
Regarding lesion localization, the results from the
present findings were in a slight contradiction with the results
other studies, reporting that tibia, femur and peroneus were the
main sites for osteochondroma discovery. Yet, our findings
describing a higher rate of lesion localized on the left side of
the body were similar to the results from Tong et al
(15), although this previous study
did not report such a high rate of left-side lesions.
Osteochondroma is generally an asymptomatic
pathology; however, it can lead to pain, local edema or certain
complications such as peripheral nerve compression, aneurysms,
thrombosis and fractures (7).
Previous studies described the malignant transformation of
osteochondroma into chondrosarcoma as being the most severe
complications (3,12,13,18).
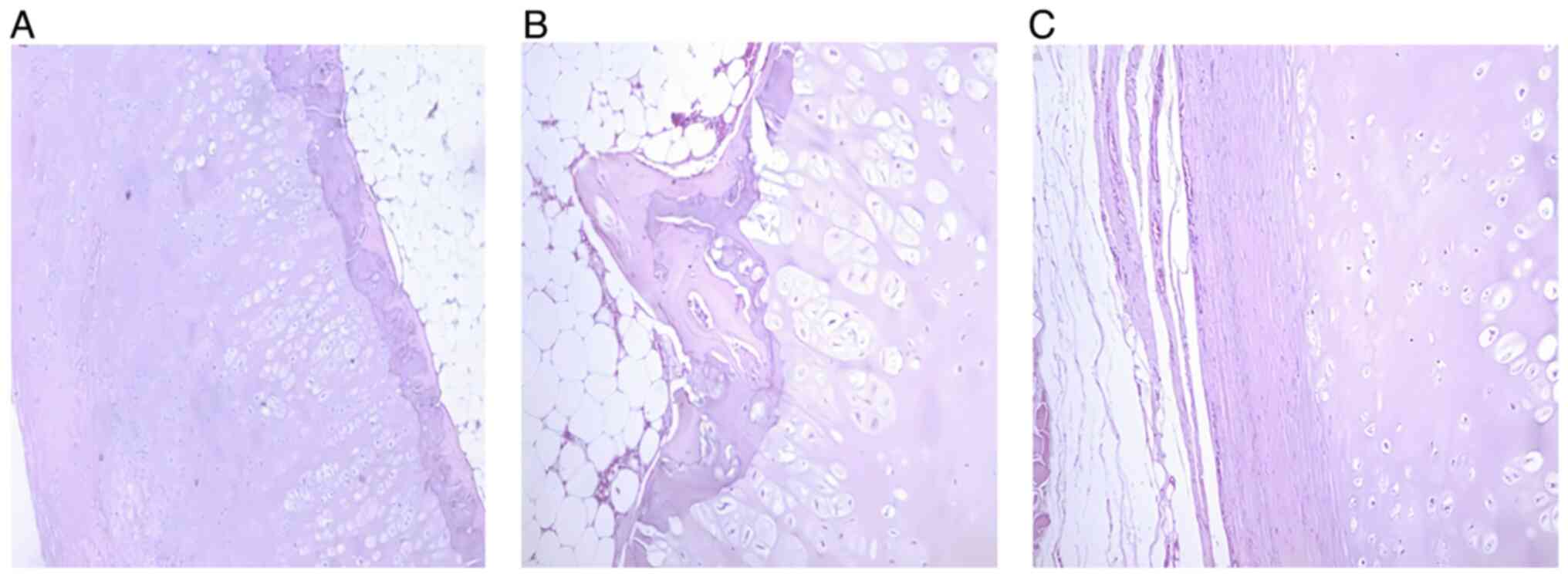
Histologically, osteochondroma lesion consist of
three layers: perichondrium, cartilage and bone. The exterior layer
is the fibrous perichondrium, which continues with the subjacent
bone periosteum (Fig. 4). The next
layer is the cartilaginous cap, which under normal circumstances
has a thickness of <20 mm that further decreases as the patient
is getting older (4). In patients
where osteochondroma is suspected, the accuracy of the final
diagnosis is superior when histopathological examinations are
conducted. Thus, the histological examination of the biopsy sample
helps confirm the diagnosis of osteochondroma by revealing specific
cells such as chondrocytes, adipocytes, osteocytes (osseous tissue
resulting from endochondral ossification) (Fig. 4A and B), cartilaginous tissue and perichondrium
presenting connective tissue with blood vessels (Fig. 4C). The transition area between bone
and cartilage cap can also be noticed, which is similar to a growth
plate with endochondral ossification into mature bone (Fig. 4B).
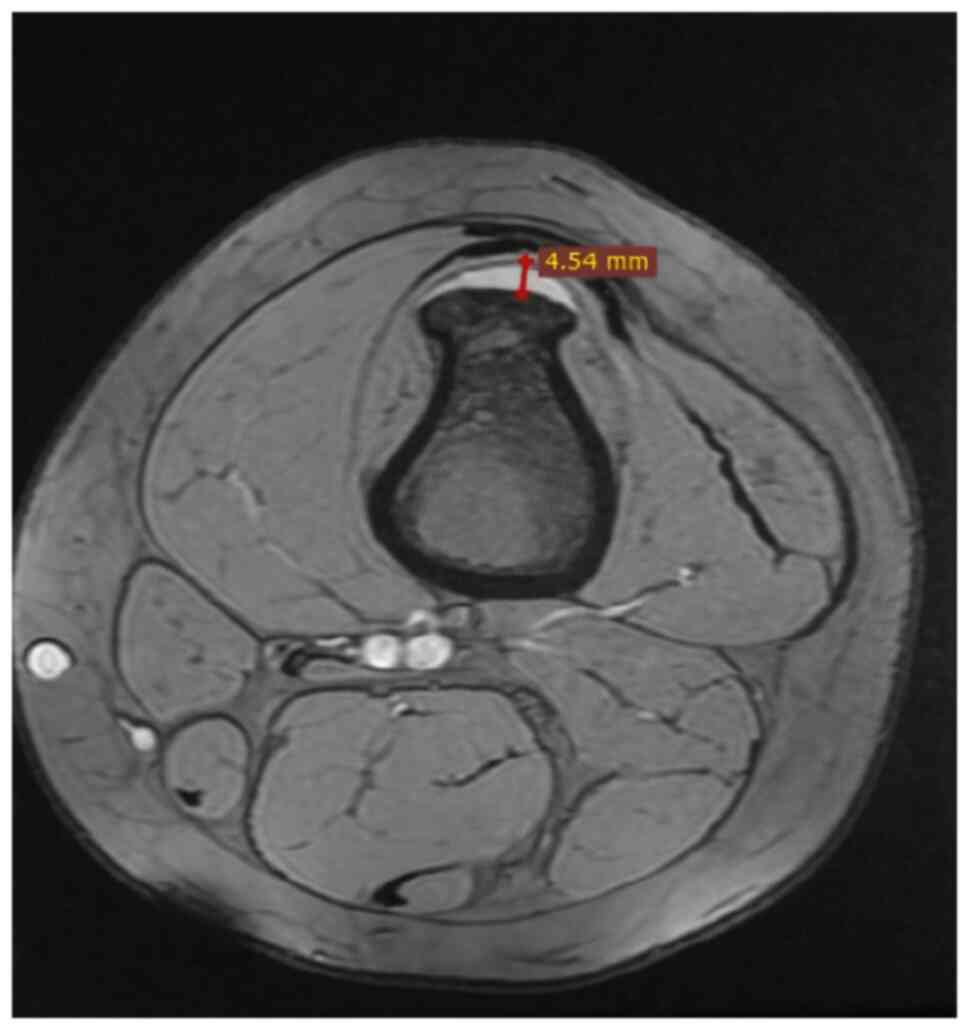
Previous studies reported that the average width of
the cartilage cap is <30 mm in pediatric patients due to the
continuity of the growth process (Fig.
5), although it was also demonstrated that this width could not
be >20 mm in normal adults because a larger width would be
associated with malignant transformation such as chondrosarcoma
(2,19,20).
Chondrocytes are essential cells during endochondral
ossification where a loss of cartilaginous architecture takes
place. Both chondrocyte atypia and necrosis are some
characteristics that could indicate secondary malignant
transformation, which, according to Tong et al (15), has a rate of ~0.6% in the simple
form and 2.9% in the multiple form.
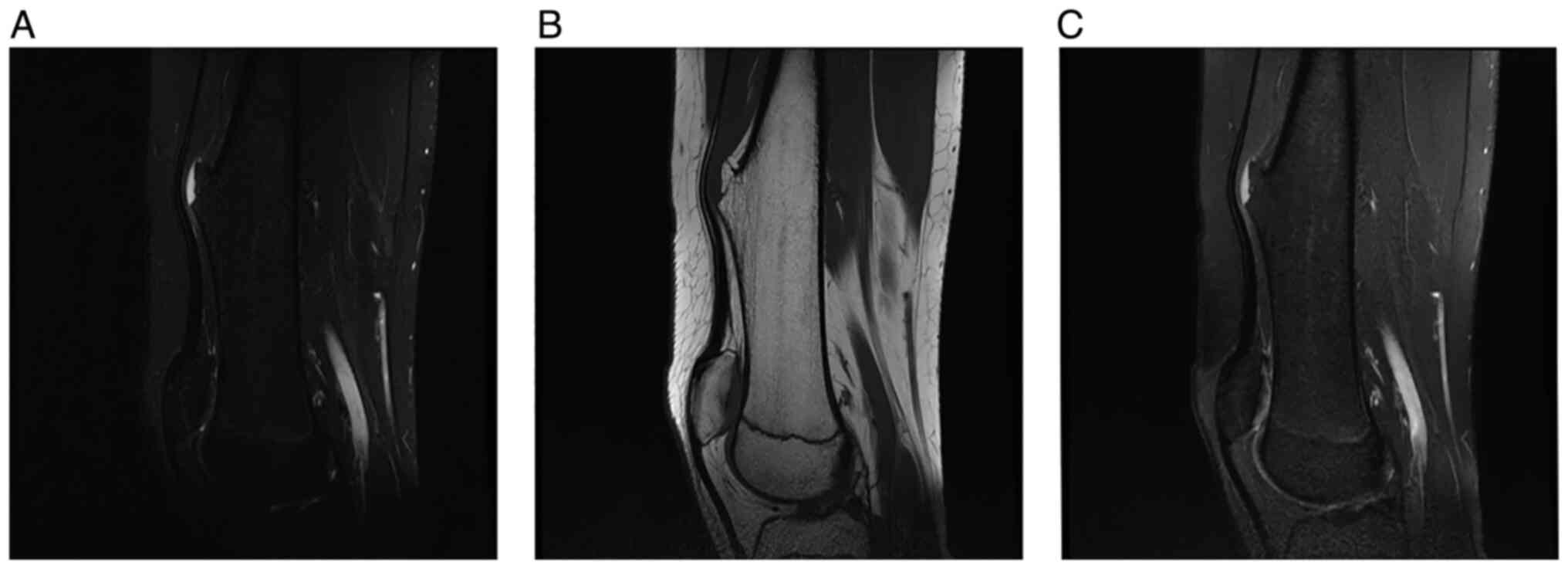
Imaging semiology is sufficient for osteochondromas
and can even be, in some cases, of pathognomonic value, especially
when the irregular calcifications inside the lesion and the cortex
of the lesion in direct contact with the main cortical bone are
clearly visible (4). In the case of
CT scans and MRI examinations, radiologists can also appreciate the
continuity of the medullary bone around the lesion (Fig. 6). Furthermore, these examinations
can help evaluating the thickness of the cartilaginous cap, and a
thickness of >20 mm could suggest a malignant transformation
(5).
MRI examination is the only available imaging method
that does not cause radiation and can very accurately reveal
numerous areas such as soft tissue, bone marrow, cartilage, muscle,
ligaments and tendons that are adjacent to the lesion. In addition,
MRI helps the clinician evaluating more accurately the cartilage
overlying the lesion (Fig. 7)
(5,21).
In summary, osteochondromas are generally
asymptomatic some lesions that are often diagnosed incidentally
following a trauma. Thus, it is very difficult to determine the
exact incidence of this pathology. Although the risk of malignant
transformation of these lesions is low, clinicians should not
forget that one of these risk factors is irradiation, which means
that adopting the right imaging examination protocols during
patient follow-up is crucial. As a result, MRI examinations are
more appropriate in pediatric patients for the following benefits:
Lack of ionizing radiation, multiplanar reformation capabilities
and excellent resolution. Subsequently, it is preferable that the
imaging protocols would be coordinated by the radiologist in order
to ensure the lowest radiation possible. Furthermore, every
clinician should consider that the accuracy of diagnosis is higher
every time histopathological examinations are conducted. Although
the precision of imaging examinations is high, the final diagnosis
is higher following histopathological analysis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
IB, MP, DA and SB conceived and designed the study.
IB, CS and MRM acquired the data. IB, MP, DA and LRS assessed the
authenticity of the data, analyzed and validated the results. IB
and MP were responsible for the preparation of the original draft.
Final manuscript editing was performed by IB and DA. MJT reviewed
the literature data and revised the article critically for
important intellectual content, gave the final approval of the
version to be published and supervised the manuscript publication.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the University of
Medicine and Pharmacy of Craiova, Committee of Ethics and Academic
and Scientific Deontology.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Caro-Domínguez P and Navarro OM: Bone
tumors of the pediatric foot: Imaging appearances. Pediatr Radiol.
47:739–749. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Murphey MD, Choi JJ, Kransdorf MJ,
Flemming DJ and Gannon FH: Imaging of osteochondroma: Variants and
complications with radiologic-pathologic correlation.
Radiographics. 20:1407–1434. 2000.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Whitehouse, RW: Computed tomography of
bone tumours (Chapter 2). In: Kindblom LG, Davies AM, Sundaram M
and James SLJ (eds): Imaging of Bone Tumors and Tumor-Like Lesions:
Techniques and Applications. Springer-Verlag, Berlin, Heidelberg,
2009.
|
|
4
|
Fletcher CDM, Unni KK and Mertens F (eds):
Pathology and Genetics of Tumours of Soft Tissue and Bone.
IARCPress, Lyon, pp234-236, 2002.
|
|
5
|
de Souza AM and Bispo Júnior RZ:
Osteochondroma: Ignore or investigate? Rev Bras Ortop. 49:555–564.
2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Dorfman HD and Czerniak B: Osteochondroma.
Bone tumors. Mosby, St. Louis, MO, pp331-346, 1998.
|
|
7
|
Kitsoulis P, Galani V, Stefanaki K,
Paraskevas G, Karatzias G, Agnantis NJ and Bai M: Osteochondromas:
Review of the clinical, radiological and pathological features. In
Vivo. 22:633–646. 2008.PubMed/NCBI
|
|
8
|
Preda SA, Nechita F, Comanescu MC,
Albulescu DM, Tuculina MJ, Docea AD, Burada E, Vasile RC and Mitroi
M: Evaluation of bone turnover and DXA markers in premature ovarian
failure. Rev Chim. 6 (Bucharest):2054–2057. 2019.
|
|
9
|
Preda SA, Albulescu DM, Mitroi MR, Popescu
M, Nechita F, Camen A and Cotoi IA: Craniofacial morphology aspects
in children with isolated growth hormone deficiency-a cephalometric
study. Rom J Morphol Embryol. 60:653–658. 2019.PubMed/NCBI
|
|
10
|
Kumar PS, Rao DS, Manepalli S, Damera A
and Killada JK: Osteochondroma involving the ramus of the mandible:
An unusual location. Case Rep Dent. 2020(8603027)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Dandriyal R, Giri KY, Pant S, Alam S and
Joshi A: Giant osteochondroma of the coronoid process. J Maxillofac
Oral Surg. 14 (Suppl 1):S412–S416. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Douis H and Saifuddin A: The imaging of
cartilaginous bone tumours. I. Benign lesions. Skeletal Radiol.
41:1195–1212. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Garcia RA, Inwards CY and Unni KK: Benign
bone tumors-recent developments. Semin Diagn Pathol. 28:73–85.
2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kannan P, Suresh MJ and Anandan H:
Radiology-pathological correlation of primary benign bone tumors: A
retrospective study. Int J Sci Stud. 5:215–222. 2017.
|
|
15
|
Tong K, Liua H, Wang X, Zhong Z, Cao S,
Zhong C, Yang Y and Wang G: Osteochondroma: Review of 431 patients
from one medical institution in South China. J Bone Oncol. 8:23–29.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Wuyts W and Van Hul W: Molecular basis of
multiple exostoses: Mutations in the EXT1 and EXT2 genes. Hum
Mutat. 15:220–227. 2000.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Yang C, Zhang R, Lin H and Wang H:
Insights into the molecular regulatory network of pathomechanisms
in osteochondroma. J Cell Biochem. 120:16362–16369. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ahmed AR, Tan TS, Unni KK, Collins MS,
Wenger DE and Sim FH: Secondary chondrosarcoma in osteochondroma:
Report of 107 patients. Clin Orthop Relat Res. 411:193–206.
2003.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Motamedi K and Seeger LL: Benign bone
tumors. Radiol Clin North Am. 49:1115–1134, v.2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lin PP, Moussallem CD and Deavers MT:
Secondary chondrosarcoma. J Am Acad Orthop Surg. 18:608–615.
2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gemescu IN, Thierfelder KM, Rehnitz C and
Weber MA: Imaging features of bone tumors: Conventional radiographs
and MR imaging correlation. Magn Reson Imaging Clin N Am.
27:753–767. 2019.PubMed/NCBI View Article : Google Scholar
|