1. Introduction
The outbreak of coronavirus 2019 (COVID-19) was
declared by the World Health Organization (WHO) as a global public
health emergency on January 30, 2020(1). Currently, worldwide, there have been
>249 million confirmed cases of COVID-19, and >5 million
deaths from COVID-19 reported, according to the WHO (2).
From a public health perspective, the current
pandemic has underscored that a multitude of predisposing factors
may contribute to the rapid spread of severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2), particularly among vulnerable
individuals. First, environmental pollution and chronic exposure to
chemicals, such as fossil fuel derivatives, as well as exposure to
particle matters, metals, and ultraviolet (UV)-B and ionizing
radiation have been acknowledged as risk factors for
immunodeficiency, that may contribute to the manifestation of
COVID-19(3). Second, a number of
studies have underlined that distinct cellular mechanisms may be
associated with an increased predisposition to COVID-19, including
the dysfunction of high mobility group proteins (HMGBs), which
belong to a superfamily of nuclear proteins with DNA-binding
properties that have been implicated in immunological,
pro-thrombotic and viral replicating cascades (4). Third, there is an increasing
understanding of the central role of immunological processes,
including aberrant inflammatory responses and cytokine release
during the initial stages of viral infection, as well a growing
awareness of the pivotal role of humoral and cellular responses in
the elimination or conversely, the propagation of COVID-19(5).
Of note, the COVID-19 pandemic is considered the
most severe pandemic of the 21st century with significant
repercussions not only on physical health, but on mental health as
well (6-8).
It is thus unsurprising, that the development of effective vaccines
against SARS-CoV-2 became a priority for the public health agenda
from the time of the outbreak of the pandemic. Currently, there are
several available vaccines against COVID-19, which have been proven
both safe and effective in preventing severe SARS-CoV-2 infection
or mortality from COVID-19, while to date, >50% of the world
population has received at least one dose of a COVID-19 vaccine
(9-17).
Although causal treatments for COVID-19 remain unavailable, certain
beneficial effects from vitamin supplements, probiotics and
minerals have been reported in a number of studies, although their
role is considered mostly supportive for the immune system
(10,18-20).
Multiple public health interventions have also been
implemented worldwide to decrease the transmission of
SARS-CoV-2(21). Nevertheless,
measures aiming to attenuate the viral spread, such as
self-isolation, quarantine, lockdown and movement restrictions,
have led to significant restrictions in daily activities and
routines, and along with the threat posed by the pandemic, these
measures have propagated feelings of fear, uncertainty,
stigmatization, social isolation and loneliness (22-24).
Furthermore, there have been reports of a significant increase in
alcohol consumption and a significant exacerbation of domestic
violence during the implementation of the aforementioned
restriction measures (25,26).
Thus, there is a growing concern currently regarding
the mental health sequelae of the COVID-19 pandemic (23,27,28).
In particular, accumulating evidence has been presented of relapses
in individuals with pre-existing mental health issues, who are at
risk of further deterioration, new-onset mental illness, increased
morbidity or even death, while individuals with no prior
psychiatric history are also at risk of developing psychological
issues (29,30).
Moreover, an increasing number of studies have
suggested that patients with COVID-19 may experience
neuropsychiatric manifestations, both during the acute and
post-illness stages (i.e., COVID-19 survivors) (31-38).
The severity of acute SARS-CoV-2 infection appears to be related to
subsequent psychiatric or neurological sequelae, while there may be
a tendency towards symptom improvement over time (33).
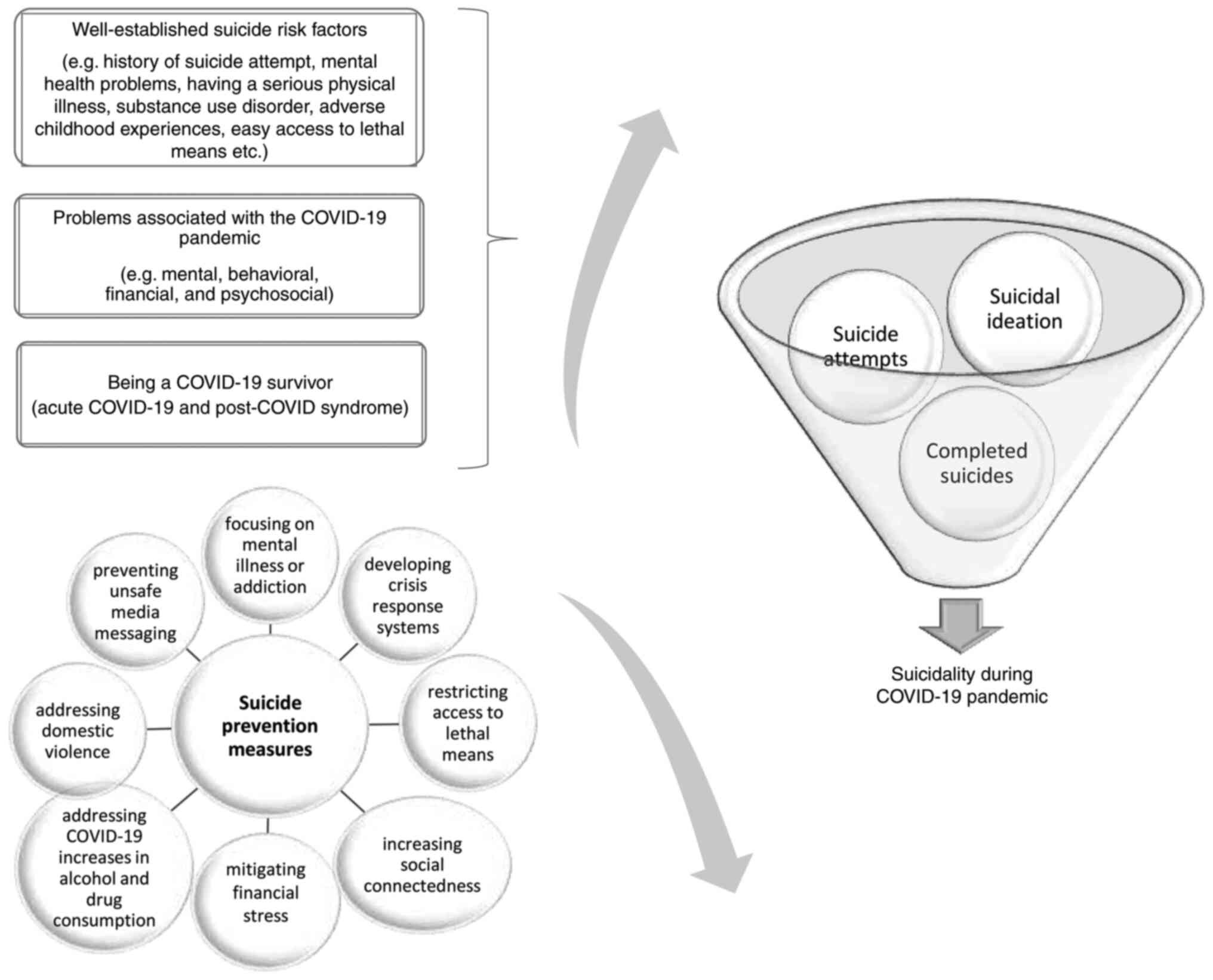
2. Suicidal behaviors in the context of the
COVID-19 pandemic
Since the outbreak of the COVID-19 pandemic, there
has been widespread concern regarding its effect on suicidality, as
COVID-19 may increase the risk of individuals developing suicidal
behaviors through its effects on a number of well-established
suicide risk factors (Fig. 1)
(39,40).
Several parameters, both at the population and
individual levels, modulate suicide risk (41). Factors that are related to an
increased number of suicides, include a history of suicide
attempts, mental health issues, experiencing social isolation,
facing financial stress or professional difficulties, criminal or
legal issues, having a serious physical illness, substance use
disorder, adverse childhood experiences, a family history of
suicide, having experienced sexual violence, barriers to health
care, stigma associated with mental illness or help-seeking, easy
access to lethal means and unsafe media portrayals of suicide
(42).
It should be noted that during previous infectious
disease outbreaks, suicide prevalence appeared to be elevated.
Specifically, suicide rates were found to have increased during the
bubonic plague, during the Spanish Flu of 1918-1919 in the United
States, during the SARS outbreak in China among the elderly, women
and lower socio-economic class, as well as during the Ebola
infection in Africa (43-46).
Mental, behavioral, financial and psychosocial
issues associated with the COVID-19 pandemic may contribute to an
increase in suicidal behaviors (39,40).
Furthermore, symptoms of psychiatric, neurological and physical
illnesses, as well as inflammatory damage to the brain among
patients with post-COVID syndrome may be associated with an
increased risk of suicidal tendencies in this population, while
COVID-19 survivors without post-COVID syndrome may also face such a
risk (47).
Suicidal ideation and suicide attempts
amidst the COVID-19 pandemic
Suicidal ideation during the COVID-19 pandemic has
been associated with loneliness, anxiety, depression, insomnia,
impaired family functioning, a history of mental health issues,
alcohol misuse, COVID-19-related stress symptoms, concerns over
COVID-19, having tested positive for COVID-19, a younger age, an
unmarried or divorced marital status, living alone, being a
military veteran, previous homelessness, financial strain, housing
instability, unemployment, a poor perceived quality of physical
health, disability and living with an individual with frail health
(48-53).
On the other hand, increased social support, resilience, positive
feelings regarding the lockdown measures and faith in a supreme
being have been identified as significant protective factors
against suicidal ideation (48,49,54).
In a previous meta-analysis of 54 studies, including
data from 308,596 individuals, that investigated suicide behaviors
during the COVID-19 pandemic, increased event rates were found when
considered against event rates from pre-pandemic studies (39). Specifically, that study
demonstrated during the COVID-19 pandemic, the combined samples'
event rate was 10.81% for suicidal ideation, 4.68% for suicide
attempts and 9.63% for self-harm, whereas when community, clinical
and frontline samples were examined separately, a trend for higher
rates was found in the clinical sample. Nevertheless, it should be
noted that the majority of the studies were cross-sectional or
retrospective chart reviews (39).
A previous longitudinal study examining the
trajectory of mental health during the first 6 weeks of lockdown
(from March 31 to May 11, 2020) in a UK adult population (n=3,077)
revealed increased rates of suicidal ideation during the initial
weeks of the pandemic-related lockdown, particularly among young
adults (55). On the other hand, a
Spanish longitudinal study aiming at examining the suicidal
ideation prevalence among 1,103 adults after the pandemic-related
lockdown measures were lifted in Spain (May 21, 2020 to June 30,
2020) compared to the pre-lockdown period (June 17, 2019 to March
14, 2020) found no differences regarding the suicidal ideation
rates (54).
As regards suicidal ideation during the pandemic, a
longitudinal study from Greece in a community sample of 811 adults,
investigated suicidal ideation rates during the first (April 7 to
May 3, 2020) as compared to the second (November 22 to December 21,
2020) pandemic-related national lockdown, and found no differences
between the two time periods; depression emerged as the only
significant prognostic factor for suicidal ideation incidence
(i.e., among individuals who experienced suicidal thoughts during
the second, but not the first lockdown) (50). Nevertheless, Veldhuis et al
(56), using a global longitudinal
convenience sample (n=1,567), surveyed both in April and September,
2020, reported a significant increase over time in suicidal
thoughts and behaviors from baseline levels [mean (M)=2.6; standard
error (SE)=0.72] to the 5-month follow-up (M=4.89; SE=0.91;
P<0.05).
In another study, temporal trends in primary
care-recorded self-harm monthly counts (from January, 2019 to May,
2021) were examined using a time series analysis of electronic
healthcare records for 2.8 million patients in the North West of
England (Greater Manchester conurbation). According to the results
of that study, an initial marked reduction in overall self-harm was
identified in April, 2020, while a sustained decrease was also
observed to the end of May, 2021. The greatest overall reductions
were observed during the first national lockdown, while longer-term
reductions were largest among males and individuals residing in the
most deprived areas; however, an increase emerged in the reports of
self-harm among adolescents (10-17 years of age) (57).
A time-trend study in Denmark using health records
from hospitals and emergency medical services (covering 46% of the
Danish population), compared the number of psychiatric in-patients,
referrals to mental health services and suicidal behavior in the
years prior to the COVID-19 pandemic to levels during the first
lockdown (March 11 to May 17, 2020), the inter-lockdown period (May
18 to December 15, 2020) and the second lockdown (December 16, 2020
to February 28, 2021). The study did not identify any significant
differences with respect to suicidal behavior or referral rates.
However, during the pandemic, the rates of psychiatric in-patients
decreased compared with the pre-pandemic levels, with the largest
decrease being recorded during the first lockdown (58).
Accordingly, a retrospective cross-sectional study
in a large, integrated, community-based health system in the USA,
on suicide-related encounters in the emergency department
demonstrated that the overall rates within 2020 did not increase,
and at times the rates decreased, in comparison to those in 2019;
however, an increase was observed in 2020 for patients with a
substance use disorders (59).
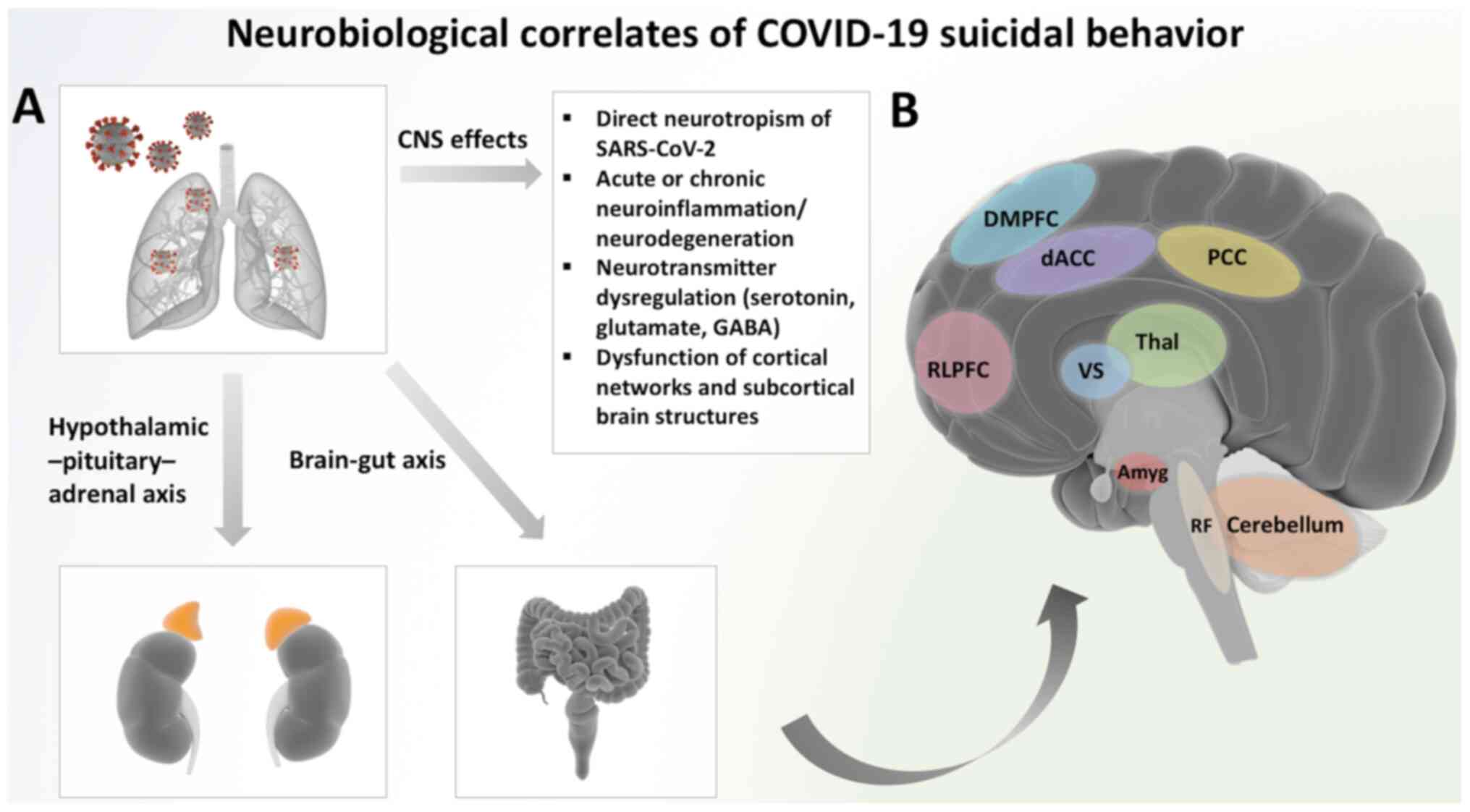
Of note, apart from the psychosocial aspects of
suicidality amidst the COVID-19 pandemic, SARS-CoV-2 infection per
se may confer an increased risk of suicidal ideation and behaviors.
Although the pathophysiological underpinnings of COVID-19
associated suicidality remain to date poorly elucidated, putative
mechanisms have been proposed that may increase suicidal
vulnerability and the overall risk of suicidal acts in infected
patients (60). Accordingly,
several mechanisms may be implicated in infection-associated brain
damage as follows: The direct neurotropic effects of SARS-CoV-2
mediated by the retrograde axonal transport of the virus from the
respiratory mucosa, hypoxic brain injury, peripheral inflammation
and monocyte-macrophage system activation that precipitate neuronal
dysfunction, and the disruption of the blood-brain barrier that
induces a prolonged state of neuroinflammation and possibly
neurodegeneration (60-64).
The SARS-CoV-2-induced cytokine ‘storm’ has been shown to play a
major role in the propagation of neuropsychiatric symptoms
associated with COVID-19, while aberrations in inflammatory
cytokines have been proposed as pathophysiological correlates of
suicidality (22,63,65,66).
In addition, neurotransmitter imbalances, including GABAergic,
glutamatergic and serotoninergic pathways, as well as widespread
neuronal network dysfunction, have been suggested to provide
neurobiological links to COVID-19 suicidality. Moreover, COVID-19
related sleep disturbances, neuroendocrine changes, including
cortisol hypersecretion and the dysregulation of the
hypothalamus-pituitary-adrenal axis, as well as the dysregulation
of the gut microbiota and the brain-gut axis may all contribute to
the emergence or exacerbation of suicidal behaviors in patients
with COVID-19 (Fig. 2) (22,67-69).
Nevertheless, SARS-CoV-2-induced neurobiological changes that
precipitate suicidality are possibly intertwined with superimposed
psychological stressors associated with COVID-19. Thus, further
research is warranted to provide neuroimaging and histopathological
data from patients with COVID-19 with suicidal tendencies or
behaviors.
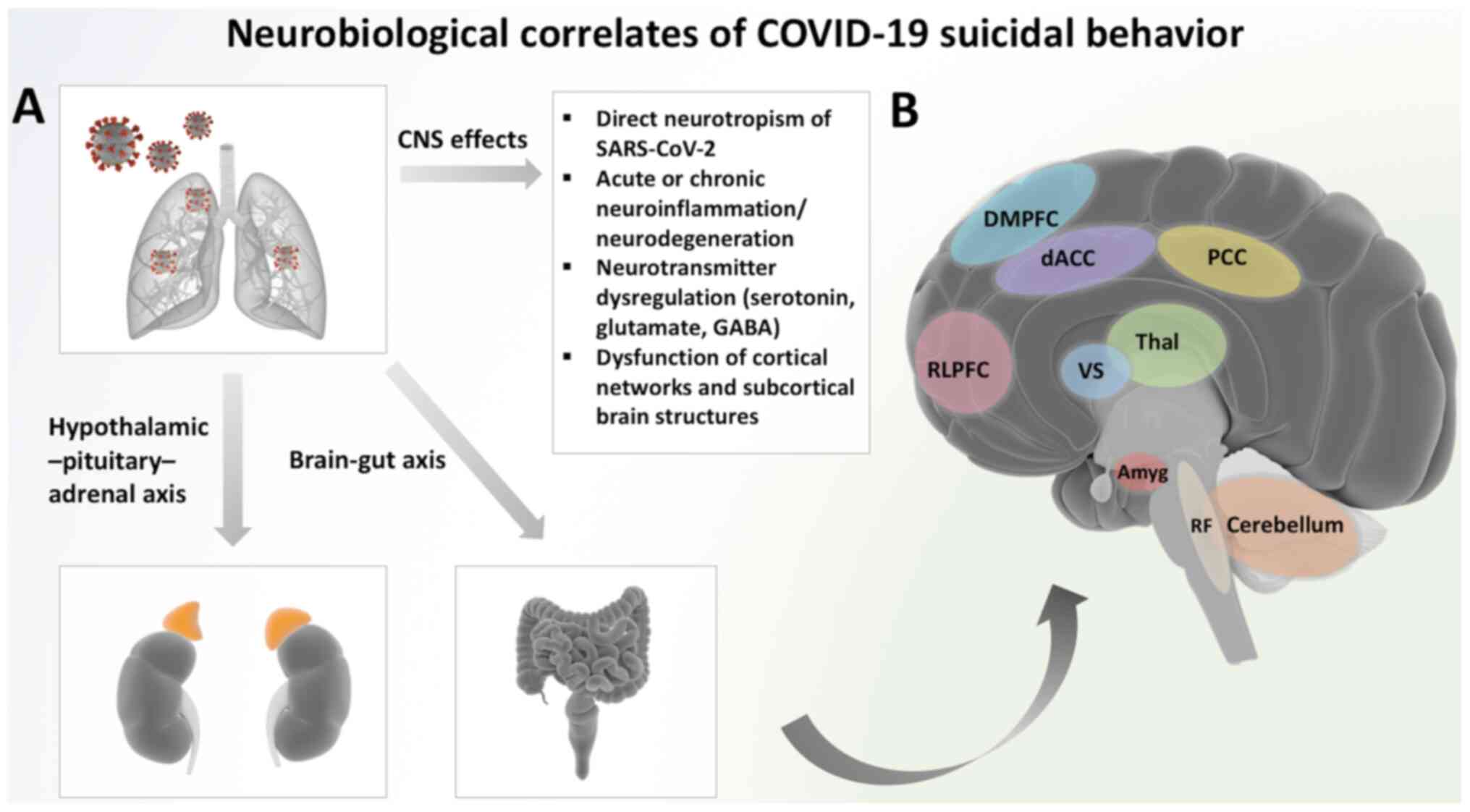 | Figure 2Neurobiological correlates of
COVID-19 suicidal behavior. (A) SARS-CoV-2 infection induces
distinctive effects in the CNS, which are mediated by the
retrograde axonal transport of the virus in the CNS in acute
COVID-19, or immune responses, including the cytokine ‘storm’, that
precipitate acute or chronic neuroinflammatory and
neurodegenerative cascades. Additionally, SARS-CoV-2 may cause the
dysregulation of neurotransmitters (i.e., serotonin, glutamate,
GABA) and the dysfunction of large cortical networks and
subcortical brain structures, which may be linked to an increased
risk of suicidality in patients with COVID-19. Further pathways
possibly involved in COVID-19-related suicidal behavior involve the
hypothalamic-pituitary adrenal axis. In COVID-19, stress responses
and cortisol hypersecretion have been shown to upregulate the
hypothalamus-pituitary-adrenal axis (adrenal glands are depicted in
orange), while further suggested mechanisms that may contribute to
emergence or exacerbation of suicidal behavior involve
dysregulation of the gut microbiota and the brain-gut axis. (B) All
the aforementioned mechanisms may induce dysfunction in several
brain regions, which have been implicated in the pathophysiology of
suicidal behavior, and are mainly located in the ventral and dorsal
prefrontal cortex, insula, mesial temporal, subcortical and
posterior regions. Notably, neuroimaging and histopathological
evidence of COVID-19-related suicidality is currently unavailable;
thus, the depicted brain regions have been linked with suicidal
behavior in previous neuroimaging studies in non-COVID-19 patients
with suicidal ideation or behavior. Further brain structures
implicated in suicidality include the DMPFC, the hippocampus and
the basal ganglia (not shown). Notably, as previously demonstrated,
autopsies of patients with COVID-19 have indicated neuronal loss
and hypoxic changes in some of the aforementioned brain regions
(64). CNS, central nervous
system; GABA, glutamate and gamma-aminobutyric acid; RLPFC,
rostrolateral prefrontal cortex; DMPFC, dorsomedial prefrontal
cortex; dACC, dorsal anterior cingulate cortex; PCC, posterior
cingulate cortex; Thal, thalamus; VS, ventral striatum; Amyg,
amygdala; RF, reticular formation. |
Completed suicides amidst the COVID-19
pandemic
From the onset of the COVID-19 pandemic, several
mental health experts have expressed concerns regarding a possible
increase in the rates of suicide and have even warned of a
‘suicide epidemic triggered by COVID-19’, a ‘dual
pandemic of suicide and COVID-19’, or a ‘suicide mortality
and COVID-19-a perfect storm’ (43,70-72).
Worldwide, cases of individuals who died through
suicide have been reported, mainly in the media, linking their
deaths to the fear of COVID-19 infection, fear of transmitting
SARS-CoV-2 to others, anxiety over COVID-19, fear of isolation due
to imposed country pandemic-related lockdown and a lack of
knowledge. Further triggers that have been identified for suicides
related to the COVID-19 pandemic are xenophobia, COVID-19-related
stigma and social boycott, financial insecurities and uncertainty
concerning the future (73,74).
In previous a review article on suicide reports, possible factors
and predictors of COVID-19-related suicide were categorized
according to ‘social isolation and distancing’, ‘worldwide lockdown
creating economic recession’, ‘stress, anxiety and pressure in
medical healthcare professionals’ and ‘social boycott and
discrimination’ (73).
Pirkis et al (75) investigated suicidal trends in the
early months of the COVID-19 pandemic (from April 1 to July 31,
2020) by using an interrupted time-series analysis of preliminary
data from 21 countries, including national data from 10 countries
and data from 25 regions across a further 11 countries.
Specifically, real-time data were acquired on suicides for
Australia, Austria, Canada, Chile, Croatia, United Kingdom
(England), Estonia, Germany, Italy, Japan, Netherlands, New
Zealand, Poland, South Korea, Spain, USA, Brazil, Ecuador, Mexico,
Peru and Russia. Their study demonstrated that suicide rates
remained unaltered or declined in the early months of the pandemic
compared with the expected levels based on the pre-pandemic period,
in high-income and upper-middle-income countries (75).
Furthermore, other studies using official data and
taking into consideration the effect of temporal trends, have also
reported no increase in suicide rates during the early months of
the pandemic. In particular, studies from Greece, Australia
(Queensland) and the USA (Massachusetts) have demonstrated
stability in suicide rates, whereas a study from Peru reported a
decline in suicides following the implementation of a
pandemic-related lockdown (76-79).
Another study from Japan demonstrated fluctuations in suicide rates
and highlighted their association with pandemic-induced employment
shocks (80).
The absence of an increase in suicide figures, at
least during the early months of the pandemic, can be connected to
a range of factors. From the beginning of the pandemic, its
profound mental health consequences were highlighted. This may have
led to governments responding rapidly in order to strengthen
existing mental health services, while developing telemedicine
services, as well as to enact fiscal support initiatives with the
aim of moderating the economic repercussions of pandemic-related
lockdowns. Furthermore, for some individuals, the stay-at-home
period may have offered them the opportunity to avoid everyday life
stresses, while the collective feeling of all individuals facing a
pandemic may have been beneficial and helped them feel connected
and supported (75,81). Nevertheless, there is evidence to
indicate that while suicide rates remain stable or decline during
times of acute crises, delayed increases may appear in the period
that follows. Indeed, a lag effect of exposure to distressing
situations on suicide rates has been previously observed for major
world events, such as World War I, World War II and other natural
disasters; therefore, a timely implementation of effective
prevention strategies is required (81-83).
There is research evidence to support this pattern
of an increase in suicides. Following an initial reduction in
Japan, where monthly suicide rates decreased by 14% early stages of
the pandemic (February to June, 2020), a subsequent increase in
these rates was observed during the second wave (July to October,
2020) by 16%, with a larger increase among females, children and
adolescents (84). In addition,
while a first report on the short-term effects of the COVID-19
pandemic on suicides, including data from Mexico City, had
suggested no increase in the respective rates following the
declaration of a national emergency, a second report, following the
initial analysis and employing an interrupted time-series analysis
indicated that the number of monthly suicides increased during the
first 8 months of the pandemic; however, most of the increase
occurred beyond June, 2020, and concerned males regardless of their
age (85).
Moreover, it is worth noting, that each suicide may
affect 5-80 individuals, including nuclear family members,
relatives, friends and acquaintances, which are known as ‘suicide
survivors’. Suicide survivors face an increased risk of prolonged
or persistent complex bereavement (with rates reaching up to 40%),
depression, anxiety and substance-abuse disorders, as well as
suicidal behaviors, while social stigma and feelings of shame may
discourage them from seeking mental health-related assistance
(74,86). The suicide of a ‘significant other’
amidst the COVID-19 pandemic is even more challenging for suicide
survivors, who are already struggling to adjust to new conditions
and are likely experiencing psychological difficulties. Feelings of
confusion, doubt, non-acceptance, hopelessness, helplessness and
stigmatization may emerge, while the fact that death and grief
rituals, that would facilitate adjustment to bereavement and a
healthy adaptation to the loss, have either been suspended or
modified due to pandemic-related regulations, rendering it even
harder for suicide survivors to mourn their loved ones and ‘say
their goodbyes’ (74,87).
Suicide prevention during the COVID-19 pandemic is a
global priority and requires addressing not only pandemic-specific
suicide risk factors, but also pre-pandemic ones. Interventions
proposed to significantly mitigate the negative impact of the
pandemic on the risk of increased suicidal behaviors include
focusing on the needs of individuals with mental illness or
addiction, increasing social connectedness, developing robust,
accessible and culturally inclusive crisis response systems,
restricting access to lethal means, addressing COVID-19-related
increases in alcohol consumption and drug overdoses, mitigating
financial stress, addressing domestic violence issues and
preventing unsafe media and entertainment messaging (Fig. 1) (40).
3. Conclusion
The present review has illustrated the impact of the
various aspects related to the COVID-19 pandemic on suicidal
behaviors, while presenting a comprehensive overview of
epidemiological data, as well as evidence on pathophysiological
mechanisms implicated in suicidal ideation and behaviors in
patients infected with SARS-CoV-2. Improving the current
understanding of risk factors that contribute to suicidality is
important as it may help mental health professionals in identifying
patients at high risk, and can eventually facilitate the
development of targeted interventions and prevention
strategies.
Despite the initial alarming predictions and
warnings regarding an ‘epidemic’ of suicides due to COVID-19, the
majority of studies presented in the present review article suggest
that difficulties and experienced distress related to the pandemic
do not inevitably translate into increased suicide-related deaths,
at least not in the short-term. However, it should be pointed out
that, even if suicide figures have remained at mostly stable
levels, they represent ‘real lives lost, real families
devastated’ (88). Moreover,
the long-term mental health effects of the COVID-19 pandemic have
yet to be unfolded and are likely to remain for a long period of
time or even appear after the actual pandemic. Thus, long-term data
are urgently required to reflect the possible long-term
repercussions or late-effects of the pandemic. The limitations of
the present review thus include the scarcity of available data on
long-term outcomes of patients who recovered from acute COVID-19,
but continue to suffer from major psychological effects of the
pandemic. Future research is urgently required to enable the
characterization of risk factors and the early identification of
predictors of suicidal behavior during the ongoing pandemic of
COVID-19.
Suicide prevention and measures in order to promote
mental health and well-being, as well as to mitigate COVID-19
psychological consequences, particularly among vulnerable groups
and populations at a higher risk, should be a priority for health
care professionals and policymakers.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
VE, MIS, NSi and MM wrote the original draft, edited
and critically revised the manuscript. GT, VZ, DAS, NSm and ER
critically revised and edited the manuscript. All authors
substantially contributed to the conception, writing and revision
of the work and have read and approved the final manuscript. Data
authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
References
|
1
|
Sohrabi C, Alsafi Z, O'Neill N, Khan M,
Kerwan A, Al-Jabir A, Iosifidis C and Agha R: World Health
Organization declares global emergency: A review of the 2019 novel
coronavirus (COVID-19). Int J Surg. 76:71–76. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
World Health Organization (WHO):
Coronavirus disease 2019 (COVID-2019): Weekly epidemiological
update, 2021. WHO, Geneva, 2021. www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
Accessed November 13, 2021.].
|
|
3
|
Tsatsakis A, Petrakis D, Nikolouzakis TK,
Docea AO, Calina D, Vinceti M, Goumenou M, Kostoff RN, Mamoulakis
C, Aschner M and Hernández AF: COVID-19, an opportunity to
reevaluate the correlation between long-term effects of
anthropogenic pollutants on viral epidemic/pandemic events and
prevalence. Food Chem Toxicol. 141(111418)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Islam M, Hossen M, Kamaz Z, Zali A, Kumar
M, Anca Oana D, Arsene A, Calina D and Sharifi-Rad J: The role of
HMGB1 in the immune response to SARS-COV-2 infection: From
pathogenesis towards a new potential therapeutic target. Farmacia.
69:621–634. 2021.
|
|
5
|
Neagu M, Calina D, Docea AO, Constantin C,
Filippini T, Vinceti M, Drakoulis N, Poulas K, Nikolouzakis TK,
Spandidos DA and Tsatsakis A: Back to basics in COVID-19: Antigens
and antibodies-Completing the puzzle. J Cell Mol Med. 25:4523–4533.
2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Leaune E, Samuel M, Oh H, Poulet E and
Brunelin J: Suicidal behaviors and ideation during emerging viral
disease outbreaks before the COVID-19 pandemic: A systematic rapid
review. Prev Med. 141(106264)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kahil K, Cheaito MA, El Hayek R, Nofal M,
El Halabi S, Kudva KG, Pereira-Sanchez V and El Hayek S: Suicide
during COVID-19 and other major international respiratory
outbreaks: A systematic review. Asian J Psychiatr.
56(102509)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zoumpourlis V, Goulielmaki M, Rizos E,
Baliou S and Spandidos DA: [Comment] The COVID-19 pandemic as a
scientific and social challenge in the 21st century. Mol Med Rep.
22:3035–3048. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Calina D, Hartung T, Docea AO, Spandidos
DA, Egorov AM, Shtilman MI, Carvalho F and Tsatsakis A: COVID-19
vaccines: Ethical framework concerning human challenge studies.
Daru. 28:807–812. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Torequl Islam M, Nasiruddin M, Khan IN,
Mishra SK, Kudrat-E-Zahan M, Alam Riaz T, Ali ES, Rahman MS,
Mubarak MS, Martorell M, et al: A perspective on emerging
therapeutic interventions for COVID-19. Front Public Health.
8(281)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Calina D, Hernández AF, Hartung T, Egorov
AM, Izotov BN, Nikolouzakis TK, Tsatsakis A, Vlachoyiannopoulos PG
and Docea AO: Challenges and scientific prospects of the newest
generation of mRNA-Based vaccines against SARS-CoV-2. Life (Basel).
11(907)2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kostoff RN, Kanduc D, Porter AL, Shoenfeld
Y, Calina D, Briggs MB, Spandidos DA and Tsatsakis A: Vaccine- and
natural infection-induced mechanisms that could modulate vaccine
safety. Toxicol Rep. 7:1448–1458. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Calina D, Docea AO, Petrakis D, Egorov AM,
Ishmukhametov AA, Gabibov AG, Shtilman MI, Kostoff R, Carvalho F,
Vinceti M, et al: Towards effective COVID-19 vaccines: Updates,
perspectives and challenges (Review). Int J Mol Med. 46:3–16.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Calina D, Sarkar C, Arsene AL, Salehi B,
Docea AO, Mondal M, Islam MT, Zali A and Sharifi-Rad J: Recent
advances, approaches and challenges in targeting pathways for
potential COVID-19 vaccines development. Immunol Res. 68:315–324.
2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hernández AF, Calina D, Poulas K, Docea AO
and Tsatsakis AM: Safety of COVID-19 vaccines administered in the
EU: Should we be concerned? Toxicol Rep. 8:871–879. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kostoff RN, Calina D, Kanduc D, Briggs MB,
Vlachoyiannopoulos P, Svistunov AA and Tsatsakis A: Why are we
vaccinating children against COVID-19? Toxicol Rep. 8:1665–1684.
2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ritchie H, Mathieu E, Rodés-Guirao L,
Appel C, Giattino C, Ortiz-Ospina E, Hasell J, Macdonald B,
Beltekian D and Roser M: Coronavirus pandemic (COVID-19) OurWorldInData.org, 2020. https://ourworldindata.org/covid-vaccinations.
Accessed November 13, 2021.].
|
|
18
|
Islam M, Salehi B, Karampelas O,
Sharifi-Rad J, Anca Oana D, Martorell M and Calina D: High skin
melanin content, vitamin D deficiency and immunity: Potential
interference for severity of COVID-19. Farmacia. 68:970–983.
2020.
|
|
19
|
Sharifi-Rad J, Rodrigues CF,
Stojanović-Radić Z, Dimitrijević M, Aleksić A, Neffe-Skocińska K,
Zielińska D, Kołożyn-Krajewska D, Salehi B, Milton Prabu S, et al:
Probiotics: Versatile bioactive components in promoting human
health. Medicina (Kaunas). 56(433)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Islam MT, Quispe C, Martorell M, Docea AO,
Salehi B, Calina D, Reiner Ž and Sharifi-Rad J: Dietary
supplements, vitamins and minerals as potential interventions
against viruses: Perspectives for COVID-19. Int J Vitam Nutr Res:
Jan 13, 2021 (Epub ahead of print).
|
|
21
|
Ayouni I, Maatoug J, Dhouib W, Zammit N,
Fredj SB, Ghammam R and Ghannem H: Effective public health measures
to mitigate the spread of COVID-19: A systematic review. BMC Public
Health. 21(1015)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Dhrisya C, Prasathkumar M, Becky R, Anisha
S, Sadhasivam S, Essa MM, Chidambaram SB, Al-Balushi B, Guillemin
GJ and Qoronfleh MW: Social and biological parameters involved in
suicide ideation during the COVID-19 pandemic: A narrative review.
Int J Tryptophan Res. 13(1178646920978243)2020.
|
|
23
|
Serafini G, Parmigiani B, Amerio A,
Aguglia A, Sher L and Amore M: The psychological impact of COVID-19
on the mental health in the general population. QJM. 113:531–537.
2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Tsamakis K, Triantafyllis AS, Tsiptsios D,
Spartalis E, Mueller C, Tsamakis C, Chaidou S, Spandidos DA, Fotis
L, Economou M, et al: COVID-19 related stress exacerbates common
physical and mental pathologies and affects treatment (Review). Exp
Ther Med. 20:159–162. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kumar A and Nayar KR: COVID 19 and its
mental health consequences. J Mental Health. 30:1–2.
2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Calina D, Hartung T, Mardare I, Mitroi M,
Poulas K, Tsatsakis A, Rogoveanu I and Docea AO: COVID-19 pandemic
and alcohol consumption: Impacts and interconnections. Toxicol Rep.
8:529–535. 2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Duan L and Zhu G: Psychological
interventions for people affected by the COVID-19 epidemic. Lancet
Psychiatry. 7:300–302. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tsamakis K, Tsiptsios D, Ouranidis A,
Mueller C, Schizas D, Terniotis C, Nikolakakis N, Tyros G,
Kympouropoulos S, Lazaris A, et al: COVID-19 and its consequences
on mental health (Review). Exp Ther Med. 21(244)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Byrne A, Barber R and Lim CH: Impact of
the COVID-19 pandemic-a mental health service perspective. Prog
Neurol Psychiatry. 25:27–33b. 2021.
|
|
30
|
Vai B, Mazza MG, Delli Colli C, Foiselle
M, Allen B, Benedetti F, Borsini A, Casanova Dias M, Tamouza R,
Leboyer M, et al: Mental disorders and risk of COVID-19-related
mortality, hospitalisation, and intensive care unit admission: A
systematic review and meta-analysis. Lancet Psychiatry. 8:797–812.
2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Dinakaran D, Manjunatha N, Naveen Kumar C
and Suresh BM: Neuropsychiatric aspects of COVID-19 pandemic: A
selective review. Asian J Psychiatr. 53(102188)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Mazza MG, De Lorenzo R, Conte C, Poletti
S, Vai B, Bollettini I, Melloni EMT, Furlan R, Ciceri F,
Rovere-Querini P, et al: Anxiety and depression in COVID-19
survivors: Role of inflammatory and clinical predictors. Brain
Behav Immun. 89:594–600. 2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Schou TM, Joca S, Wegener G and
Bay-Richter C: Psychiatric and neuropsychiatric sequelae of
COVID-19-A systematic review. Brain Behav Immun. 97:328–348.
2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kumar S, Veldhuis A and Malhotra T:
Neuropsychiatric and cognitive sequelae of COVID-19. Front
Psychology. 12(577529)2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Giannopoulou I, Galinaki S, Kollintza E,
Adamaki M, Kympouropoulos S, Alevyzakis E, Tsamakis K, Tsangaris I,
Spandidos DA, Siafakas N, et al: COVID-19 and post-traumatic stress
disorder: The perfect ‘storm’ for mental health (Review). Exp Ther
Med. 22(1162)2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Tsatsakis A, Calina D, Falzone L, Petrakis
D, Mitrut R, Siokas V, Pennisi M, Lanza G, Libra M, Doukas SG, et
al: SARS-CoV-2 pathophysiology and its clinical implications: An
integrative overview of the pharmacotherapeutic management of
COVID-19. Food Chem Toxicol. 146(111769)2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Huang C, Huang L, Wang Y, Li X, Ren L, Gu
X, Kang L, Guo L, Liu M, Zhou X, et al: 6-month consequences of
COVID-19 in patients discharged from hospital: A cohort study.
Lancet. 397:220–232. 2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Taquet M, Geddes JR, Husain M, Luciano S
and Harrison PJ: 6-month neurological and psychiatric outcomes in
236 379 survivors of COVID-19: A retrospective cohort study using
electronic health records. Lancet Psychiatry. 8:416–427.
2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Dubé JP, Smith MM, Sherry SB, Hewitt PL
and Stewart SH: Suicide behaviors during the COVID-19 pandemic: A
meta-analysis of 54 studies. Psychiatry Res.
301(113998)2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Moutier C: Suicide prevention in the
COVID-19 Era: Transforming threat into opportunity. JAMA
Psychiatry. 78:433–438. 2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Turecki G and Brent DA: Suicide and
suicidal behaviour. Lancet. 387:1227–1239. 2016.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Centers for Disease Control and Prevention
(CDC): Suicide Prevention-Risk and Protective Factors. CDC,
Atlanta, GA, 2021. www.cdc.gov/suicide/factors/index.html. Accessed
October 2, 2021.
|
|
43
|
Banerjee D, Kosagisharaf JR and
Sathyanarayana Rao TS: ‘The dual pandemic’ of suicide and COVID-19:
A biopsychosocial narrative of risks and prevention. Psychiatry
Res. 295(113577)2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Wasserman IM: The impact of epidemic, war,
prohibition and media on suicide: United States, 1910-1920. Suicide
Life Threat Behav. 22:240–254. 1992.PubMed/NCBI
|
|
45
|
Cheung YT, Chau PH and Yip PS: A revisit
on older adults suicides and Severe Acute Respiratory Syndrome
(SARS) epidemic in Hong Kong. Int J Geriatr Psychiatry.
23:1231–1238. 2008.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Bitanihirwe BK: Monitoring and managing
mental health in the wake of Ebola. Commentary. Ann Ist Super
Sanita. 52:320–322. 2016.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Sher L: Post-COVID syndrome and suicide
risk. QJM. 114:95–98. 2021.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Elbogen EB, Lanier M, Blakey SM, Wagner HR
and Tsai J: Suicidal ideation and thoughts of self-harm during the
COVID-19 pandemic: The role of COVID-19-related stress, social
isolation, and financial strain. Depress Anxiety. 38:739–748.
2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Papadopoulou A, Efstathiou V, Yotsidi V,
Pomini V, Michopoulos I, Markopoulou E, Papadopoulou M,
Tsigkaropoulou E, Kalemi G, Tournikioti K, et al: Suicidal ideation
during COVID-19 lockdown in Greece: Prevalence in the community,
risk and protective factors. Psychiatry Res.
297(113713)2021.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Efstathiou V, Michopoulos I, Yotsidi V,
Smyrnis N, Zompola C, Papadopoulou A, Pomini V, Papadopoulou M,
Tsigkaropoulou E, Tsivgoulis G, et al: Does suicidal ideation
increase during the second COVID-19 lockdown? Psychiatry Res.
301(113990)2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Antonelli-Salgado T, Monteiro GMC, Marcon
G, Roza TH, Zimerman A, Hoffmann MS, Cao B, Hauck S, Brunoni AR and
Passos IC: Loneliness, but not social distancing, is associated
with the incidence of suicidal ideation during the COVID-19
outbreak: A longitudinal study. J Affect Disord. 290:52–60.
2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Killgore WDS, Cloonan SA, Taylor EC,
Fernandez F, Grandner MA and Dailey NS: Suicidal ideation during
the COVID-19 pandemic: The role of insomnia. Psychiatry Res.
290(113134)2020.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Killgore WDS, Cloonan SA, Taylor EC and
Dailey NS: Loneliness: A signature mental health concern in the era
of COVID-19. Psychiatry Res. 290(113117)2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Ayuso-Mateos JL, Morillo D, Haro JM, Olaya
B, Lara E and Miret M: Changes in depression and suicidal ideation
under severe lockdown restrictions during the first wave of the
COVID-19 pandemic in Spain: A longitudinal study in the general
population. Epidemiol Psychiatr Sci. 30(e49)2021.PubMed/NCBI View Article : Google Scholar
|
|
55
|
O'Connor RC, Wetherall K, Cleare S,
McClelland H, Melson AJ, Niedzwiedz CL, O'Carroll RE, O'Connor DB,
Platt S, Scowcroft E, et al: Mental health and well-being during
the COVID-19 pandemic: Longitudinal analyses of adults in the UK
COVID-19 Mental Health & Wellbeing study. Br J Psychiatry: Oct
21, 2020 (Epub ahead of print).
|
|
56
|
Veldhuis CB, Nesoff ED, McKowen ALW, Rice
DR, Ghoneima H, Wootton AR, Papautsky EL, Arigo D, Goldberg S and
Anderson JC: Addressing the critical need for long-term mental
health data during the COVID-19 pandemic: Changes in mental health
from April to September 2020. Prev Med. 146(106465)2021.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Steeg S, Bojanić L, Tilston G, Williams R,
Jenkins DA, Carr MJ, Peek N, Ashcroft DM, Kapur N, Voorhees J and
Webb RT: Temporal trends in primary care-recorded self-harm during
and beyond the first year of the COVID-19 pandemic: Time series
analysis of electronic healthcare records for 2.8 million patients
in the Greater Manchester Care Record. EClinicalMedicine.
41(101175)2021.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Rømer TB, Christensen RHB, Blomberg SN,
Folke F, Christensen HC and Benros ME: Psychiatric admissions,
referrals, and suicidal behavior before and during the COVID-19
pandemic in denmark: A time-trend study. Acta Psychiatr Scand.
144:553–562. 2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Ridout KK, Alavi M, Ridout SJ, Koshy MT,
Awsare S, Harris B, Vinson DR, Weisner CM, Sterling S and Iturralde
E: Adult Suicide-Related emergency department encounters during the
COVID-19 Pandemic: A Cross-sectional study. Lancet Regional Health
Am. 4(100078)2021.
|
|
60
|
Conejero I, Nobile B, Olié E and Courtet
P: How does COVID-19 affect the neurobiology of suicide? Curr
Psychiatry Rep. 23(16)2021.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Troyer EA, Kohn JN and Hong S: Are we
facing a crashing wave of neuropsychiatric sequelae of COVID-19?
Neuropsychiatric symptoms and potential immunologic mechanisms.
Brain Behav Immun. 87:34–39. 2020.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Steiner J, Gos T, Bogerts B, Bielau H,
Drexhage HA and Bernstein HG: Possible impact of microglial cells
and the monocyte-macrophage system on suicidal behavior. CNS Neurol
Disord Drug Targets. 12:971–979. 2013.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Ngo B, Lapp SA, Siegel B, Patel V,
Hussaini L, Bora S, Philbrook B, Weinschenk K, Wright L, Anderson
EJ, et al: Cerebrospinal fluid cytokine, chemokine, and SARS-CoV-2
antibody profiles in children with neuropsychiatric symptoms
associated with COVID-19. Mult Scler Relat Disord.
55(103169)2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Solomon IH, Normandin E, Bhattacharyya S,
Mukerji SS, Keller K, Ali AS, Adams G, Hornick JL, Padera RF Jr and
Sabeti P: Neuropathological features of Covid-19. N Engl J Med.
383:989–992. 2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Brundin L, Bryleva EY and Thirtamara
Rajamani K: Role of inflammation in suicide: From mechanisms to
treatment. Neuropsychopharmacology. 42:271–283. 2017.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Schmaal L, van Harmelen AL, Chatzi V,
Lippard ETC, Toenders YJ, Averill LA, Mazure CM and Blumberg HP:
Imaging suicidal thoughts and behaviors: A comprehensive review of
2 decades of neuroimaging studies. Mol Psychiatry. 25:408–427.
2020.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Pfennig A, Kunzel HE, Kern N, Ising M,
Majer M, Fuchs B, Ernst G, Holsboer F and Binder EB:
Hypothalamus-pituitary-adrenal system regulation and suicidal
behavior in depression. Biol Psychiatry. 57:336–342.
2005.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Mello MT, Silva A, Guerreiro RC, da-Silva
FR, Esteves AM, Poyares D, Piovezan R, Treptow E, Starling M, Rosa
DS, et al: Sleep and COVID-19: Considerations about immunity,
pathophysiology, and treatment. Sleep Sci. 13:199–209.
2020.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Chen J and Vitetta L: Gut-brain axis in
the neurological comorbidity of COVID-19. Brain Commun.
3(fcab118)2021.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Reger MA, Stanley IH and Joiner TE:
Suicide mortality and coronavirus disease 2019-a perfect storm?
JAMA Psychiatry. 77:1093–1094. 2020.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Tandon R: COVID-19 and suicide: Just the
facts. Key learnings and guidance for action. Asian J Psychiatr.
60(102695)2021.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Mannix R, Lee LK and Fleegler EW:
Coronavirus disease 2019 (COVID-19) and Firearms in the United
States: Will an epidemic of suicide follow? Ann Intern Med.
173:228–229. 2020.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Thakur V and Jain A: COVID 2019-suicides:
A global psychological pandemic. Brain Behav Immun. 88:952–953.
2020.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Pinto S, Soares J, Silva A, Curral R and
Coelho R: COVID-19 suicide survivors-a hidden grieving population.
Front Psychiatry. 11(626807)2020.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Pirkis J, John A, Shin S, DelPozo-Banos M,
Arya V, Analuisa-Aguilar P, Appleby L, Arensman E, Bantjes J, Baran
A, et al: Suicide trends in the early months of the COVID-19
pandemic: An interrupted time-series analysis of preliminary data
from 21 countries. Lancet Psychiatry. 8:579–588. 2021.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Faust JS, Shah SB, Du C, Li S-X, Lin Z and
Krumholz HM: Suicide deaths during the COVID-19 Stay-at-Home
advisory in massachusetts, March to May 2020. JAMA Netw Open.
4(e2034273)2021.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Calderon-Anyosa RJC and Kaufman JS: Impact
of COVID-19 lockdown policy on homicide, suicide, and motor vehicle
deaths in Peru. Prev Med. 143(106331)2021.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Vandoros S, Theodorikakou O, Katsadoros K,
Zafeiropoulou D and Kawachi I: No evidence of increase in suicide
in Greece during the first wave of Covid-19 medRxiv: doi:
https://doi.org/10.1101/2020.11.13.20231571.
|
|
79
|
Leske S, Kõlves K, Crompton D, Arensman E
and de Leo D: Real-time suicide mortality data from police reports
in Queensland, Australia, during the COVID-19 pandemic: An
interrupted time-series analysis. Lancet Psychiatry. 8:58–63.
2021.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Ando M and Furuichi M: The impact of
COVID-19 employment shocks on suicide and poverty alleviation
programs: An early-stage investigation. medRxiv: doi: https://doi.org/10.1101/2020.11.16.20232850.
|
|
81
|
Wasserman D, Iosue M, Wuestefeld A and
Carli V: Adaptation of evidence-based suicide prevention strategies
during and after the COVID-19 pandemic. World Psychiatry.
19:294–306. 2020.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Zalsman G, Stanley B, Szanto K, Clarke DE,
Carli V and Mehlum L: Suicide in the time of COVID-19: Review and
recommendations. Arch Suicide Res. 24:477–482. 2020.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Lester D: Suicide rates before, during and
after the world wars. Eur Psychiatry. 9:262–264. 1994.
|
|
84
|
Tanaka T and Okamoto S: Increase in
suicide following an initial decline during the COVID-19 pandemic
in Japan. Nat Hum Behav. 5:229–238. 2021.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Borges G, Garcia JA, Pirkis J, Spittal MJ
and Lopez-Arellano O: Suicide after and during the COVID-19
pandemic in Mexico City. SSRN, Rochester, NY, 2021. https://ssrn.com/abstract=3879041 or http://dx.doi.org/10.2139/ssrn.3879041. Accessed
June, 30, 2021.
|
|
86
|
Berman AL: Estimating the population of
survivors of suicide: Seeking an evidence base. Suicide Life Threat
Behav. 41:110–116. 2011.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Castle J and Phillips WL: Grief rituals:
Aspects that facilitate adjustment to bereavement. J Loss Trauma.
8:41–71. 2003.
|
|
88
|
Appleby L: What has been the effect of
Covid-19 on suicide rates? BMJ. 372(n834)2021.PubMed/NCBI View Article : Google Scholar
|