1. Introduction
Dementia represents a major neurocognitive disorder
caused by brain disease or injury and is characterized by
impairments in executive function, learning and memory, attention,
language, perceptual-motor function, and/or social cognition, among
other psychiatric, mood, and behavioural disturbances (1).
Unfortunately, the onset of this disease may be very
subtle, and patients frequently present unspecific symptoms that
can be easily confused with chronic fatigue syndrome, depression,
insomnia, anaemia, infections, side effects of medication, natural
aging, nutrient imbalances, or vitamin and hormone deficiencies.
For this reason, dementia is commonly misdiagnosed or overlooked in
the earlier stages (1-5).
Since the average life expectancy has increased,
dementia rates are rapidly growing in all continents (1). Epidemiologic studies revealed that ~6%
of the population over 65 years is diagnosed with dementia
(1-5),
and 46.8 million people live with dementia worldwide. Furthermore,
the total number of patients with dementia is estimated to double
every 20 years. There is no curative treatment for the disease, and
the burden on society is significant (5).
The main nursing interventions for patients with
advanced dementia include periodic change of position to avoid the
appearance of pressure ulcers, active and passive mobilization,
massage, passive feeding, skin hygiene, bed and body linen, bedding
with flea and urinary catheter management. In the situation where
these patients are immobilized in beds, it is necessary to prevent
falls by properly arranging the space in the bed to eliminate
safety risks. These procedures are used as an attempt to overcome
complications of advanced dementia such as metabolic disorders
related to nutritional deficiency, depression, self-injury and
impaired self-image. Patients with advanced stages of dementia
frequently require professional 24-h supervision for their personal
safety, basic needs, and the administration of medication (1-5).
Autonomous robotic assistive technology may represent an affordable
and practical solution to this global problem.
For this reason, the purpose of this study was to
perform a comparative analysis of traditional nursing techniques
and autonomous robotic applications used on patients with advanced
stages of dementia.
PubMed, Cochrane Library, EMBASE, and WILEY
databases were searched for relevant articles regarding nursing
techniques used in patients with advanced dementia, starting with
traditional techniques and ending with artificial intelligence
(AI)-based systems and autonomous robots. The search terms
included: (advanced dementia OR severe dementia) AND (AI OR robotic
OR robots OR neural networks OR deep learning OR automated
procedures OR autonomous application).
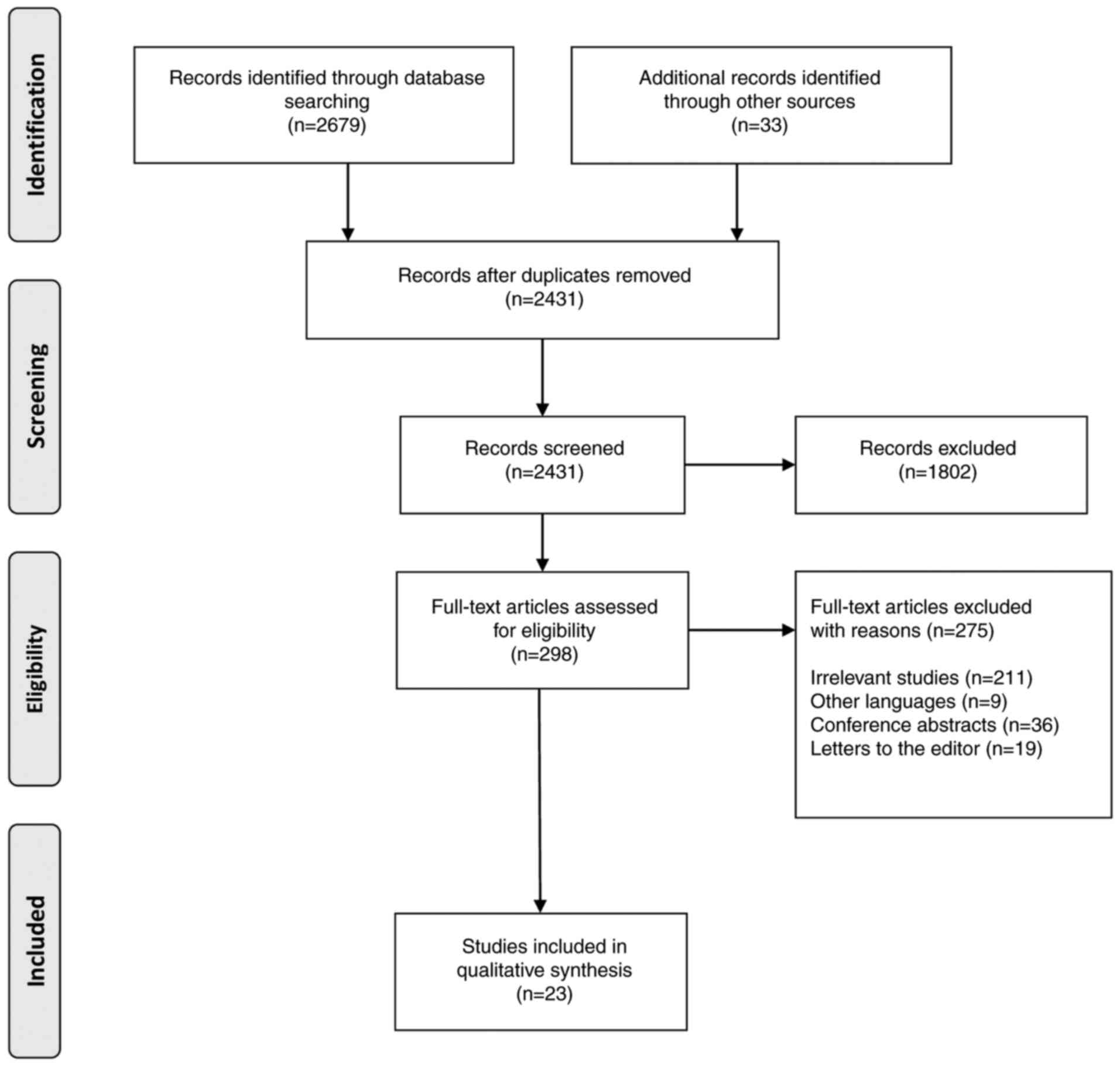
Exclusion criteria were: conference presentations,
letters to the editor, studies written in languages other than
English, case reports, pediatric studies, abstracts, and editorials
(Fig. 1). A total of 2 independent
authors (LD and SLP) reviewed eligibility titles, abstracts, and
full text of eligible articles. Data extraction was conducted
independently by both reviewers. Fig.
1 demonstrates the search strategy using the PRISMA flow
diagram.
Discrepancies related to the results of the quality
assessment evaluation between the two investigators were resolved
through discussion. Results of the methodological quality
assessment did not have any effect on the eligibility of the
studies in our systematic review.
Our search identified a total of 2,679 articles.
Following use of human filters, the search identified 298 articles.
Following application of all filters (human filters, while
excluding conference abstracts and conference papers), 112 studies
remained. Finally, a total of 23 articles were included in this
systematic review: 8 studies analyzing traditional nursing
techniques and 15 studies analyzing autonomous robotic
applications.
2. Traditional nursing techniques for
patients with advanced dementia
The articles that were selected mention the
importance of traditional nursing techniques in different aspects
of the multifaceted health problem that is dementia (Table I).
 | Table ITraditional nursing techniques for
advanced dementia patients. |
Table I
Traditional nursing techniques for
advanced dementia patients.
| Author (Refs.) | Year | Evidence type | Method | Treatment | Outcome |
|---|
| Husebo et al
(6) | 2011 | Cluster randomized
controlled trial | Patients with
stepwise pain treatment protocol vs. control group (patients with
usual management) | Eight weeks of three
times a day pain medication according to a 4-step protocol with a
2-week follow-up | Efficient pain
management significantly reduces agitation |
| Sampson et al
(7) | 2009 | Systematic
review | Inclusion of
observational studies in the absence of randomized controlled
trials | - | Insufficient
evidence on the benefits of tube feeding; requirement for further
studies |
| Skovdahl et
al (8) | 2007 | Study | Data was analyzed
with qualitative content analysis | Tactile stimulation
in five patients with moderate-to-severe dementia and a tendency
towards aggression or restlessness | Positive feelings
and relaxation |
| Ridder et al
(9) | 2013 | Exploratory
randomized controlled trial | Music therapy vs.
standard care | Six weeks of two
times per week individual music therapy sessions | Decrease in
agitation and improvement in quality of life |
| Murphy et al
(10) | 2016 | Systematic
review | Only two studies
concerning palliative care were considered; meta-analysis of the
data was not possible | - | Insufficient
evidence for evaluating the influence |
| Aasmul et al
(11) | 2016 | Cluster randomized
controlled trial | Caregivers for
patients in the intervention group vs. caregivers for patients in
the control group | Individual pain
treatment for 8 weeks, followed by a 4-week wash-out period | Decrease of staff
distress in the intervention group |
|
Birkenhäger-Gillesse et al
(12) | 2018 | Randomized
controlled study | Dyads (patient and
caregiver) included either in the intervention group or in the
control group; data collected at baseline, 3 months, and 6
months | ‘More at Home with
Dementia’ training program for 5 days | Focus on the
quality of life of the caregiver at three months and
neuropsychiatric symptoms of the patient |
| Sanchez-Valdeon
et al (13) | 2019 | Study | Quasi-experimental;
pre-post case series design; data collection at start, following 6
months and following 12 months | 12 months of weekly
30-min long individual canine-assisted therapy | Significant
benefits for quality of life |
An extensive trial conducted by Husebo et al
(6) evaluated the effects of a
4-step pain management protocol on agitation, aggression, pain,
activities of daily life, and cognition in patients suffering from
moderate to severe dementia and clinically significant behavioural
changes. All patients were residents of one of the 60 single
independent nursing home units included in the trial. The outcome
was evaluated using multiple measuring tools: Cohen-Mansfield
agitation inventory, neuropsychiatric inventory (nursing home
version), mobilisation-observation-behaviour-intensity-dementia-2
pain scale, activities of daily life, and Mini-Mental State
Examination (MMSE). The active intervention proved to be of great
benefit in addition to the non-specific effect, and the authors
suggested that well-coordinated pain management could be used
extensively for the assistance of agitated residents of nursing
homes suffering from dementia.
Following performance of a systematic review of
enteral tube feeding in patients with advanced dementia, Sampson
et al (7) concluded that the
benefits are not supported by sufficient evidence despite numerous
patients receiving this intervention. Concurrently, it appeared
that the side effects of this procedure lacked adequate study.
A team led by Skovdahl et al (8) studied the effect of tactile
stimulation in five residents from a nursing home who suffered from
behavioural and psychiatric symptoms of dementia. The caregivers
were instructed on performing tactile stimulation and applied this
technique at least once a week. Each session was documented using a
form designed specifically for this purpose. The entire
documentation containing 60 pages was then analyzed using
qualitative content analysis. The sessions designed to continue for
28 weeks with a mean duration of 45 min had a positive and relaxing
influence, however, the use of such therapies should be respectful
towards the preferences of patients.
The effect of music therapy was studied by Ridder
et al (9) in an exploratory
randomized controlled trial that compared the standard care group
of patients with the groups receiving music therapy twice a week,
for six weeks in a row. Music therapy demonstrated a positive
effect on the quality of life and reduced agitation
disruptiveness.
Murphy et al (10) analyzed the effects of palliative
care interventions in patients with advanced dementia, but their
systematic review identified only two completed studies that
matched their criteria. These studies assessed different outcomes,
making it impossible to draw any conclusion other than an
imperative need for high-quality research on this subject.
Taking care of residents diagnosed with dementia may
also take its toll on the nursing home staff. Aasmul et al
(11) concluded that individual
pain management in such patients would indirectly reduce staff
distress with lasting effects. The research methodology included
subjects from 60 nursing home units, where the primary caregivers
had direct contact with the patient (highly agitated patients with
advanced dementia) for at least four weeks.
Training programs for caregivers in medical settings
could delay the admission of the patient to a nursing home, prove
cost-efficient, and lessen the burden for the caregivers. This is
what the researchers coordinated by Birkenhäger-Gillesse et
al (12) are currently trying
to demonstrate with a randomized controlled study protocol designed
to examine the effects of a 5-day training program (‘More at Home
with Dementia’) in an intervention group.
The effect of canine-assisted therapy on the quality
of life of patients diagnosed with Alzheimer's type dementia was
evaluated in a quasi-experimental study by Sanchez-Valdeon et
al (13). The authors used
specifically trained dogs in therapy sessions lasting 30 min and
repeated once a week for 12 months. All the subjects experienced a
positive influence on the quality of life [outcome assessed using
the Quality of Life in Late-Stage Dementia (QUALID) scale]. The
fact that the study included only a small number of participants
prevents the extrapolation of the results.
3. Autonomous Robotic Applications for
patients with advanced dementia
Our search for studies concerning autonomous robotic
applications used for patients with advanced dementia identified 15
studies (Table II).
 | Table IIAutonomous robotic applications for
patients with advanced dementia. |
Table II
Autonomous robotic applications for
patients with advanced dementia.
| Author (Refs.) | Year | Evidence type | Method | Treatment | Outcome |
|---|
| Demange et
al (14) | 2019 | Study | Qualitative (five
focus groups) and quantitative (questionnaire survey) approach | PARO®
robot | Framework for the
use of the PARO® robot in the management of acute pain
in persons with dementia |
| Valentí et
al (15) | 2015 | Study | Robot (NAO), pet
robot (PARO) or real animal (dog) nursing home: one of the three
parallel therapeutic arms CONTROL, PARO and NAO (Phase 1) and
CONTROL, PARO, and DOG (Phase 2); day care center, all patients NAO
(Phase 1) PARO (Phase 2). | 3 months of 2
days/week therapy sessions | Phase 1:
improvement in the NPI irritability and the NPI total score; Phase
2: no differences at follow-up |
| Abraha et al
(16) | 2020 | Review | Three trials
including 144 patients | Simulated presence
therapy | No firm
conclusion |
| Moyle et al
(17) | 2015 | Cluster-randomized
controlled trial | Three treatment
groups: PARO®, Plush-Toy (non-robotic PARO®)
or usual care | 10 weeks of 3
non-facilitated 15-min sessions with PARO or PlushToy each | Results yet to be
published |
| Astell et al
(18) | 2019 | Study | Summarizes key
areas of technology development; identifies future directions and
implications | - | Urges an immediate
policy, funding, and practice change, for better risk reduction,
prevention, and early detection |
| Atee et al
(19) | 2018 | 2-week
observational study | Electronic Pain
Assessment Tool | - | Good reliability
properties, and appropriate to use in residents with advanced
dementia |
| Hall et al
(20) | 2017 | Embedded
multiple-case study | 36 semi-structured
interviews with staff, relatives, and residents; 175 h of
observation; resident care record review | - | Use of monitoring
technologies encouraged if perceived as safety enhancing |
| Bossen et al
(21) | 2015 | Review | Evaluation of
online and internet-based technology use in monitoring and
support | - | Positive impact of
telemedicine and smart technologies on helping caregivers and
reducing costs |
| Bharucha et
al (22) | 2009 | Review | Review of
intelligent cognitive devices, physiologic and environmental
sensors, and advanced integrated sensor networks | - | Computational and
ethical challenges with the development of intelligent assistive
devices |
| Beuscher et
al (23) | 2017 | Study | Use of socially
assistive robots (NAO humanoid robot) | - | The need for
further studies on the role of socially assistive robots |
| Koutentakis et
al (24) | 2020 | Review | Evaluation of
socially assistive robots | - | A socially
assistive robot could perform almost all the functions desired of
Alzheimer's disease-related dementia patients and their
caregivers |
| Pirhonen et
al (25) | 2020 | Study | Impact of social
robots and communicating technology | - | Social robots could
alleviate emotional and social loneliness in assisted living
(ethical concerns) |
| Majumder et
al (26) | 2017 | Review | Evaluation of data
on smart home-based remote healthcare technologies | - | Useful
comprehensive information is provided by smart homes |
| Dang et al
(27) | 2017 | Study | Intelligent
interactive care system based on a multimodal deep neural
network | - | Accurate algorithm
for recognition |
| Cipriani and
Fiorino (28) | 2020 | Study | Summary of the
events that occurred in Italy during the beginning of the SARS-CoV2
pandemic, with the focus on older age groups | - | Dementia as one of
the most frequent comorbidities in deceased patients with COVID19;
discrimination based on personal characteristics (such as age or
disability) was inadmissible |
In the study performed by Demange et al
(14), it was demonstrated that the
PARO® robot (Intelligent System Co.) was helpful in
supporting the treatment of acute pain in 12 patients with
dementia. The PARO® robot is a pet robot in the shape of
a baby harp seal designed for psychological care in geriatric
patients. It was previously successfully used to accompany the
treatment of certain behavioural disorders, reducing loneliness,
stress levels and improving communication and/or social behaviours
in elderly patients with dementia. A total of 92% of the patients
revealed a positive attitude toward the PARO robot, regardless of
the type of painful situation (14).
Valentí et al (15) conducted a study in an elderly
population group with dementia, comparing the effect of a humanoid
robot (NAO), a pet robot (PARO), and a dog on behavioural changes,
reduction of apathy, and improvement of quality of life. The study
was conducted in a nursing home on 101 patients (Phase 1) who
interacted either with the humanoid robot, with the pet robot, or
received conventional therapy. In Phase 2 of the study, 110
patients interacted either with a dog, with the PARO robot, or
received conventional therapy. In the day-care centre, 20 patients
were included in Phase 1 and 17 patients in Phase 2. Concerning the
patients from the nursing home, the authors revealed that in those
from Phase 1, patients in the robot groups exhibited an improvement
in apathy; patients in the NAO group exhibited a decline in
cognition as assessed by the MMSE scores. The robot groups
exhibited no significant changes between them. For patients
included in Phase 2, the QUALID scale scores were increased in the
PARO group. In the day-care centre, patients from Phase 1 revealed
an improvement in the Neuropsychiatric Inventory-Questionnaire
(NPI) irritability and total score (15). Patients from Phase 2 demonstrated no
differences at follow-up (15).
Simulated presence therapy is a type of intervention
used in patients with dementia that uses audio or video recordings
of family members that are played to the person with dementia. Its
potential role in improving behavioural and psychological symptoms
and quality of life in people with dementia was recently assessed
by a Cochrane systematic review conducted by Abraha et al
(16). Three trials including 144
patients were considered eligible for the study. In these studies,
simulated presence therapy was compared with usual care,
personalized music, a ‘placebo’ audiotape containing the voice of a
person, and one-to-one social interaction performed by trained
research assistants. Within each trial, the effect of simulated
presence therapy (SPT) on behaviour, compared with usual care, was
mixed and depended on the measure used. The quality of the studies
included in this systematic review was extremely low, given the
very low number of patients included and the inherent risk of bias.
Therefore, no firm conclusions concerning the efficacy of simulated
presence therapy for treating behavioural and psychological
symptoms and improving the quality of life of people with dementia
could be drawn (16).
Moyle et al (17) proposed to evaluate the effect of the
PARO® robot, a Plush-toy or usual care on apathy,
agitated behaviours, loneliness, and depression in 380 patients
with dementia aged 60 years or more. The secondary outcomes of this
trial included sleep duration, step count, changes in psychotropic
medication use, change in treatment costs, and staff and family
perceptions of the PARO robot or Plush-Toy. To date, the results of
this study have yet to be published.
In their study, Astell et al (18) summarized the existing data in the
literature up to 2019, on the impact of technology development on
the management of dementia and identified future directions and
implications. The authors focused on specific areas related to the
evaluation and treatment of patients with dementia, namely:
Diagnosis, assessment and monitoring, maintenance of function of
patients with dementia, leisure and activities of these patients,
caregiving and management, and future directions. They concluded
that despite the rapid pace of innovations in the field of
technology, urgent change was required in services and policies.
Existing technology can collect prospective data, model risk, and
provide supportive monitoring for patients with dementia.
Atee et al (19) conducted a 2-week observational study
on a population of 10 patients with moderate to severe dementia and
examined the inter-rater reliability of the electronic Pain
Assessment Tool (ePAT) among evaluators when assessing pain.
Secondary outcomes included the assessment of the relationship
between total instrument scores and facial scores, as determined by
the automated facial expression analysis. They found excellent
agreement on overall total scores [coefficient of concordance 0.92
(95% CI: 0.85-0.96)] at rest, but only moderate (κ=0.59) on
categorical scores upon movement. Based on these results, the
authors concluded that the ePAT demonstrated favorable reliability
properties, supporting its use in patients with advanced dementia
(19).
Hall et al (20) conducted a study assessing enablers
and obstacles in implementing monitoring technologies in care
homes. The study included 24 staff members, nine residents, and
nine relatives. They revealed that the most important reason for
using monitoring technologies was to improve safety and increase
freedom of residents, despite concerns related to ethical aspects
(e.g., resident privacy). Setbacks were mostly related to the
difficult cooperation of residents and the insufficient involvement
of the staff in understanding the technologies. Other drawbacks
included the frequently generated alarms that placed a burden upon
staff and the lack of positive perception of some technologies by
the staff members as useful complements to standard care.
Collectively, the authors concluded that if the technology is
perceived as enhancing the safety of residents, it may be accepted
by the residential home staff, allowing residents to benefit from
its advantages (20).
In their review article, Bossen et al
(21) assessed the current role of
smart technologies in supporting family caregivers of patients with
dementia. Following the brief summary of the costs and the negative
outcomes of caregiving, the authors presented the positive role of
telemedicine and e-health, internet-based technology, and the
support of caregivers through technology. The current roles of the
monitoring systems were described. Potential challenges to their
adoption were also discussed. Future directions and cutting-edge
technologies were briefly mentioned as well. The authors concluded
that telemedicine and smart technologies have an important
potential in helping caregivers of patients with dementia and
reducing healthcare costs (21).
Bharucha et al (22) assessed the existing evidence up to
2009 in several databases (computer science, engineering, and
medical) that assessed the role of intelligent cognitive devices,
physiologic and environmental sensors, and advanced integrated
sensor networks in facilitating the healthcare for patients with
dementia. The search strategy of authors identified a total of 58
technologies (both basic and advanced) with potential applications
to dementia care. However, no clinical trial had been conducted up
to the date of the publication of the review of the authors, that
provided evidence-based arguments supporting the use of these
technologies in the healthcare of patients with dementia. The
authors identified 11 cognitive orthotics, 15 environmental
sensors, 10 physiological sensors, and 22 advanced integrated
sensor systems, with six studies assessing the development of
memory aids. The authors concluded that intelligent assistive
devices existent at that time could be applied in helping patients
with dementia, despite remaining computational and ethical
challenges.
Beuscher et al (23) evaluated the potential role of
socially assistive robots in providing efficient and safe
healthcare. Of the 19 participants included in this study, 11 had a
one-to-one interaction with the NAO robot (a medium-sized humanoid
robot of 58 cm and 4.3 kg). Overall, the robot was well accepted,
with participants rating it as easy to understand (68%), having a
pleasant voice (74%), capable of hearing and understanding its
speech (79%), capable of keeping them interested (95%), and having
a pleasant appearance (86%). However, only 63% rated the
interaction with the robot as comfortable. The authors concluded
that although socially assistive robots have an important potential
in assisting health care providers in caring for older adults in
physical, cognitive, and social activities, future studies were
still required to precisely indicate their role in the care of
elderly patients (23).
Koutentakis et al (24) conducted a review of the currently
existing literature up to 2020 on socially assistive robots and
their potential benefit in alleviating care for patients with
Alzheimer's disease and Alzheimer's disease-related dementia. The
authors presented the existing evidence of the efficacy of socially
assistive robots, the acceptance, needs, and preference, and the
emotion recognition and the response of these robots. They
subsequently described the design and electronics of such robots,
with the software used and their features. The authors concluded
that due to the increasing life expectancy, a higher number of
individuals will require care and support during their advanced
period of life, particularly those with dementia. Socially
assistive robots could be of invaluable help in the future
(24).
Pirhonen et al (25) conducted a study on the impact of
social robots and communicating technology in decreasing social and
emotional loneliness in elderly residents. Assessed aspects were
those included in the analytical frame built on Robert Weiss'
division of relational functions: Social integration, attachment,
reassurance of worth, opportunity for nurturance, guidance in
stressful situations, and sense of reliable alliance. The authors
identified that social robots can positively influence both social
and emotional loneliness in this population. However, ethical
concerns related to lack of human contact and deception still need
to be considered before using social robots when caring for the
elderly (25).
Majumder et al (26) analyzed the existing data on smart
home-based remote healthcare technologies in their comprehensive
review. They discussed the role of several wearable Wireless Body
Area Network (WBAN), implantable WBAN, and remote health monitoring
WBAN, with the emphasis on remote health monitoring. The effect of
the Internet on healthcare and Internet-connected homes was
discussed. Smart monitoring systems for the elderly and people with
disabilities were presented and analyzed. Prototypes for smart
homes for elderly healthcare were subsequently presented, and
commercial solutions were offered. The authors concluded that smart
homes could provide useful comprehensive information about the
overall health status of the elderly through continuous
monitoring.
Dang et al (27) described in their study, an
intelligent interactive care system based on a multimode deep
neural network, addressing the interaction with patients with
dementia. Information on motion and mental features was acquired
using depth images and electroencephalograms. The authors proposed
an algorithm that simplified the process of recognition and
achieved a high accuracy and recognition rate, of >90%, for both
shuffled and continuous datasets.
Cipriani and Fiorino (28) described the outburst of the COVID-19
pandemic in Italy in early 2020. They presented the reported
mortality rate of 12.2%, which was even higher in elderly patients
aged 80 to 89 years old which was 31%. One of the most common
comorbidities (11.9%) of deceased patients with COVID-19 was
dementia. Ethical aspects related to the admittance of patients
with severe COVID-19 to the Intensive Care Unit, such as an age
limit or the presence of dementia, were mentioned. An important
question was raised concerning the criteria of providing
non-palliative care to patients in need, in an overwhelmed medical
system, and who should be left to succumb to this disease (26). The authors expressed their direct
discontent about triage of patients based on characteristics such
as age and disability (28).
The continuously growing number of individuals with
dementia poses a major challenge for global public health (29). The integration of robotics into
dementia care offers new possibilities for improving the lives of
patients and easing the burden on caregivers and healthcare
services (24,30).
Generally, there are favorable benefits from
robot-assisted activities to warrant further research in this field
(24,31-33).
However, the benefits these robots may provide are determined by
the individual characteristics of the patient, particularly the
degree of cognitive impairment and the presence or lack of prior
technology experience. All the studies concerning autonomous
AI-based applications included in this systematic review revealed
that the method is feasible for clinical practice.
Our study has several strengths. First, to the best
of our knowledge, this is the first systematic review to perform a
comparative analysis between traditional nursing techniques and
autonomous robotic applications used on patients with advanced
stages of dementia. Second, the subject of this systematic review
is of major relevance due to the increasing number of patients with
dementia, the economic burden, and the lack of qualified personnel.
Third, the COVID-19 pandemic and the risk of infection with the
COVID-19 virus, both for the patients, relatives, and medical
personnel, render autonomous AI-based applications for the care of
patients with dementia a feasible cost-efficient solution (34).
This review has several limitations. The first
limitation is the insufficient number of patients with dementia
used for training of the AI-based applications. Second, was the
lack of studies with a comparative analysis of distinct
technologies, and thereby, the inability to find clear evidence
concerning the best AI-based application for patients with
dementia.
The implementation of these technical possibilities
following the diagnosis of dementia and their permanent adaptation
to the stages of disease evolution will permit training of patients
in the management of their suffering.
4. Conclusions
Significant evidence was revealed, demonstrating
that autonomous robotic applications used for patients with
advanced stages of dementia are a feasible, cost-efficient solution
and represent a benefit for the patients and the healthcare
system.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Data sharing is not applicable to this article, as
no datasets were generated or analyzed during the current
study.
Authors' contributions
LD suggested the methodology and searched the
literature. SLP contributed to the writing of the manuscript and
searched the literature. MB contributed to the writing of section
on the traditional nursing techniques. LM contributed to the
writing of section on the autonomous robotic applications. AI
analyzed the results and revised the manuscript. AI and SLP confirm
the authenticity of all the raw data. LCP contributed to the
writing of manuscript. LPD revised the manuscript. MFS revised the
manuscript and contributed to the writing of the manuscript. DLD
analyzed the results. All authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gale SA, Acar D and Daffner KR: Dementia.
Am J Med. 131:1161–1169. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Prince M, Bryce R, Albanese E, Wimo A,
Ribeiro W and Ferri CP: The global prevalence of dementia: A
systematic review and metaanalysis. Alzheimers Dement. 9:63–75.e2.
2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lopez OL and Kuller LH: Epidemiology of
aging and associated cognitive disorders: Prevalence and incidence
of Alzheimer's disease and other dementias. Handb Clin Neurol.
167:139–148. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wolters FJ and Ikram MA: Epidemiology of
dementia: The Burden on society, the challenges for research.
Methods Mol Biol. 1750:3–14. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Cooper C, Tandy AR, Balamurali TB and
Livingston G: A systematic review and meta-analysis of ethnic
differences in use of dementia treatment, care, and research. Am J
Geriatr Psychiatry. 18:193–203. 2010.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Husebo BS, Ballard C, Sandvik R, Nilsen OB
and Aarsland D: Efficacy of treating pain to reduce behavioural
disturbances in residents of nursing homes with dementia: Cluster
randomised clinical trial. BMJ. 343(d4065)2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sampson EL, Candy B and Jones L: Enteral
tube feeding for older people with advanced dementia. Cochrane
Database Syst Rev: Apr 15, 2009 (Epub ahead of print). doi:
10.1002/14651858.CD007209.pub2.
|
|
8
|
Skovdahl K, Sörlie V and Kihlgren M:
Tactile stimulation associated with nursing care to individuals
with dementia showing aggressive or restless tendencies: An
intervention study in dementia care. Int J Older People Nurs.
2:162–170. 2007.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ridder HM, Stige B, Qvale LG and Gold C:
Individual music therapy for agitation in dementia: An exploratory
randomized controlled trial. Aging Ment Health. 17:667–678.
2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Murphy E, Froggatt K, Connolly S, O'Shea
E, Sampson EL, Casey D and Devane D: Palliative care interventions
in advanced dementia. Cochrane Database Syst Rev.
12(CD011513)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Aasmul I, Husebo BS and Flo E: Staff
distress improves by treating pain in nursing home patients with
dementia: Results from a cluster-randomized controlled trial. J
Pain Symptom Manage. 52:795–805. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Birkenhäger-Gillesse EG, Kollen BJ,
Zuidema SU and Achterberg WP: The ‘more at home with dementia’
program: A randomized controlled study protocol to determine how
caregiver training affects the well-being of patients and
caregivers. BMC Geriatr. 18(252)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sánchez-Valdeón L, Fernández-Martínez E,
Loma-Ramos S, López-Alonso AI, Bayón Darkistade E and Ladera V:
Canine-Assisted therapy and quality of life in people with
Alzheimer-type dementia: Pilot study. Front Psychol.
10(1332)2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Demange M, Pino M, Kerherve H, Rigaud AS
and Cantegreil-Kallen I: Management of acute pain in dementia: A
feasibility study of a robot-assisted intervention. J Pain Res.
12:1833–1846. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Valentí Soler M, Agüera-Ortiz L, Olazarán
Rodríguez J, Mendoza Rebolledo C, Pérez Muñoz A, Rodríguez Pérez I,
Osa Ruiz E, Barrios Sánchez A, Herrero Cano V, Carrasco Chillón L,
et al: Social robots in advanced dementia. Front Aging Neurosci.
7(133)2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Abraha I, Rimland JM, Lozano-Montoya I,
Dell'Aquila G, Velez-Diaz-Pallares M, Trotta FM, Cruz-Jentoft AJ
and Cherubini A: Simulated presence therapy for dementia. Cochrane
Database Syst Rev. 4(CD011882)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Moyle W, Beattie E, Draper B, Shum D,
Thalib L, Jones C, O'Dwyer S and Mervin C: Effect of an interactive
therapeutic robotic animal on engagement, mood states, agitation
and psychotropic drug use in people with dementia: A
cluster-randomised controlled trial protocol. BMJ Open.
5(e009097)2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Astell AJ, Bouranis N, Hoey J, Lindauer A,
Mihailidis A, Nugent C and Robillard JM: Technology and Dementia
Professional Interest Area. Technology and dementia: The future is
now. Dement Geriatr Cogn Disord. 47:131–139. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Atee M, Hoti K, Parsons R and Hughes JD: A
novel pain assessment tool incorporating automated facial analysis:
Interrater reliability in advanced dementia. Clin Interv Aging.
13:1245–1258. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Hall A, Wilson CB, Stanmore E and Todd C:
Implementing monitoring technologies in care homes for people with
dementia: A qualitative exploration using Normalization process
theory. Int J Nurs Stud. 72:60–70. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Bossen AL, Kim H, Williams KN, Steinhoff
AE and Strieker M: Emerging roles for telemedicine and smart
technologies in dementia care. Smart Homecare Technol Telehealth.
3:49–57. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Bharucha AJ, Anand V, Forlizzi J, Dew MA,
Reynolds CF III, Stevens S and Wactlar H: Intelligent assistive
technology applications to dementia care: Current capabilities,
limitations, and future challenges. Am J Geriatr Psychiatry.
17:88–104. 2009.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Beuscher LM, Fan J, Sarkar N, Dietrich MS,
Newhouse PA, Miller KF and Mion LC: Socially assistive robots:
Measuring older adults' perceptions. J Gerontol Nurs. 43:35–43.
2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Koutentakis D, Pilozzi A and Huang X:
Designing socially assistive robots for Alzheimer's disease and
related dementia patients and their caregivers: Where we are and
where we are headed. Healthcare (Basel). 8(73)2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Pirhonen J, Tiilikainen E, Pekkarinen S,
Lemivaara M and Melkas H: Can robots tackle late-life loneliness?
Scanning of future opportunities and challenges in assisted living
facilities. Futures. 124(102640)2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Majumder S, Aghayi E, Noferesti M,
Memarzadeh-Tehran H, Mondal T, Pang Z and Deen MJ: Smart homes for
elderly healthcare-recent advances and research challenges. Sensors
(Basel). 17(2496)2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Dang X, Kang B, Liu X and Cui G: An
interactive care system based on a depth image and EEG for aged
patients with dementia. J Healthc Eng. 2017(4128183)2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Cipriani G and Fiorino MD: Access to care
for dementia patients suffering from COVID-19. Am J Geriatr
Psychiatry. 28:796–797. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ienca M, Jotterand F, Vică C and Elger B:
Social and assistive robotics in dementia care: Ethical
recommendations for research and practice. Int J of Soc Robotics.
8:565–573. 2016.
|
|
30
|
Cheng ST: Dementia caregiver burden: A
research update and critical analysis. Curr Psychiatry Rep.
19(64)2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Hung L, Liu C, Woldum E, Au-Yeung A,
Berndt A, Wallsworth C, Horne N, Gregorio M, Mann J and Chaudhury
H: The benefits of and barriers to using a social robot PARO in
care settings: A scoping review. BMC Geriatr.
19(232)2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Martin F, Aguero C, Canas JM, Abella G,
Benitez R, Rivero S, Valenti M and Martinez-Martin P: Robots in
therapy for dementia patients. J Physical Agents. 7:49–56.
2017.
|
|
33
|
Papadopoulos I, Koulouglioti C, Lazzarino
R and Ali S: Enablers and barriers to the implementation of
socially assistive humanoid robots in health and social care: A
systematic review. BMJ Open. 10(e033096)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Lima MR, Wairagkar M, Natarajan N,
Vaitheswaran S and Vaidyanathan R: Robotic telemedicine for mental
health: A multimodal approach to improve human-robot engagement.
Front Robot AI. 8(618866)2021.PubMed/NCBI View Article : Google Scholar
|