Introduction
The asthma prevalence in elite athletes is higher
compared with that in the general population (1), and a number of the children practicing
various types of sports are diagnosed with asthma or have
asthma-like symptoms (2,3). The electrochemical detection of the
fraction of exhaled nitric oxide (FeNO) may be a valuable marker of
bronchial inflammation, as during airway inflammation associated
with asthma, higher than normal levels of NO are released from
bronchial epithelial cells. Thus, FeNO may be a tool to detect
undiagnosed cases of asthma or to predict asthma exacerbation in
various types of sports (4-6).
Bronchial asthma is one of the life-threatening conditions in
sports, so an accurate diagnosis and a good monitoring system are
compulsory to avoid severe exacerbation (7).
FeNO electrochemical detection is widely used in
clinical practice, as devices for detection are relatively small
and portable. Most of the devices commonly used do not need
maintenance or calibration (4,8,9).
The detection of exhaled nitric oxide is considered
a promising tool in pneumology, but its role in the diagnosis and
management of asthma cases is still under debate (10). Other medical specialties are
interested in evaluating inflammation using FeNO measurements, but
research is scarce, and the results are often conflicting (11,12).
Exercise-induced bronchoconstriction and the
pathological entities related to it are a great concern for sports
medicine, with pediatric cases being even more frequent than adult
cases (6,13,14).
The present study performed research in children enrolled in
various types of sports in Craiova (a major city from Dolj county,
in Romania), to evaluate the degree of bronchial inflammation vs.
type of sport and personal history of asthma or allergy.
Patients and methods
Study cohort
Between January and December 2018, children
practicing football, track and field, and indoor sports (fencing,
judo, handball, basketball and volleyball), who were admitted as
outpatients for routine health checks to the Department of
Pediatrics of Filantropia Municipal Hospital Craiova (Craiova,
Romania) were enrolled in a prospective study. The study included
children aged >6 years (mean age, 11.7 years) who were enrolled
in the Department of Sports Medicine as athletes mainly practicing
one of the aforementioned sports and who had the ability to perform
the technical maneuvers (spirometry and FeNO measurements)
required. The exclusion criteria were acute febrile illness and/or
acute respiratory illness, pulmonary chronic diseases (other than
asthma) and cardiovascular chronic diseases. The smokers, the
subjects who performed intense physical exercise or those who
ingested foods rich in dietary nitrate during the same day were
also rejected.
Patient assessment
The bronchial inflammation of the patients was
assessed using the Niox Vero exhaled nitric oxide analyzer
(Aerocrine AB) based on the general accepted guidelines (6), and the results were compared taking
into account the personal history of asthma, the type of sport and
the spirometry results. FeNO results >35 parts per billion (ppb)
suggested high bronchial inflammation. The spirometry evaluation
was considered abnormal (suggesting asthma) if the peak expiratory
flow (PEF) and the forced expiratory volume per one second (FEV1)
were <80% of the predicted values, and the FEV1/FVC ratio was
<85%. The bronchodilator test was considered positive if a 12%
or 200 ml increase was noted in either FEV1 or forced vital
capacity (FVC), respectively.
Statistical analysis
Demographic and clinical data were initially
regrouped using Microsoft Excel (Microsoft Corporation). This
program was used to describe the findings in terms of percentages
and group definitions. The statistical analysis was performed using
SPSS version 20 (IBM Corp.). Group comparisons were performed using
the non-parametric Mann-Whitney U or Kruskal-Wallis H test,
followed by Dunn's procedure and Bonferroni adjustment, where
appropriate, with P<0.05 considered to indicate a statistically
significant difference.
Results
Study group demographics
The 404 patients included in the present study
originated mostly from urban areas. Overall, 59.65% (241 cases)
were boys, as the main sport in the Craiova region is football and
boys are prevalent in this field (Table
I).
 | Table IDemographic data. |
Table I
Demographic data.
| | Indoor sports |
|---|
| Type of sport | Football | Track and field | Fencing | Judo | Handball | Basketball | Volleyball |
|---|
| Sex, n | | | | | | | |
|
Male | 125 | 33 | 16 | 18 | 12 | 21 | 16 |
|
Female | 10 | 24 | 14 | 7 | 42 | 34 | 32 |
| Mean age (standard
deviation), years | 9.24 (1.69) | 11.75 (2.04) | 12.39 (2.55) | 11.11 (1.95) | 12.09 (1.66) | 10.28 (2.19) | 9.11 (1.87) |
| Locality, n | | | | | | | |
|
Urban | 102 | 38 | 21 | 19 | 39 | 35 | 29 |
|
Rural | 33 | 19 | 9 | 6 | 15 | 20 | 19 |
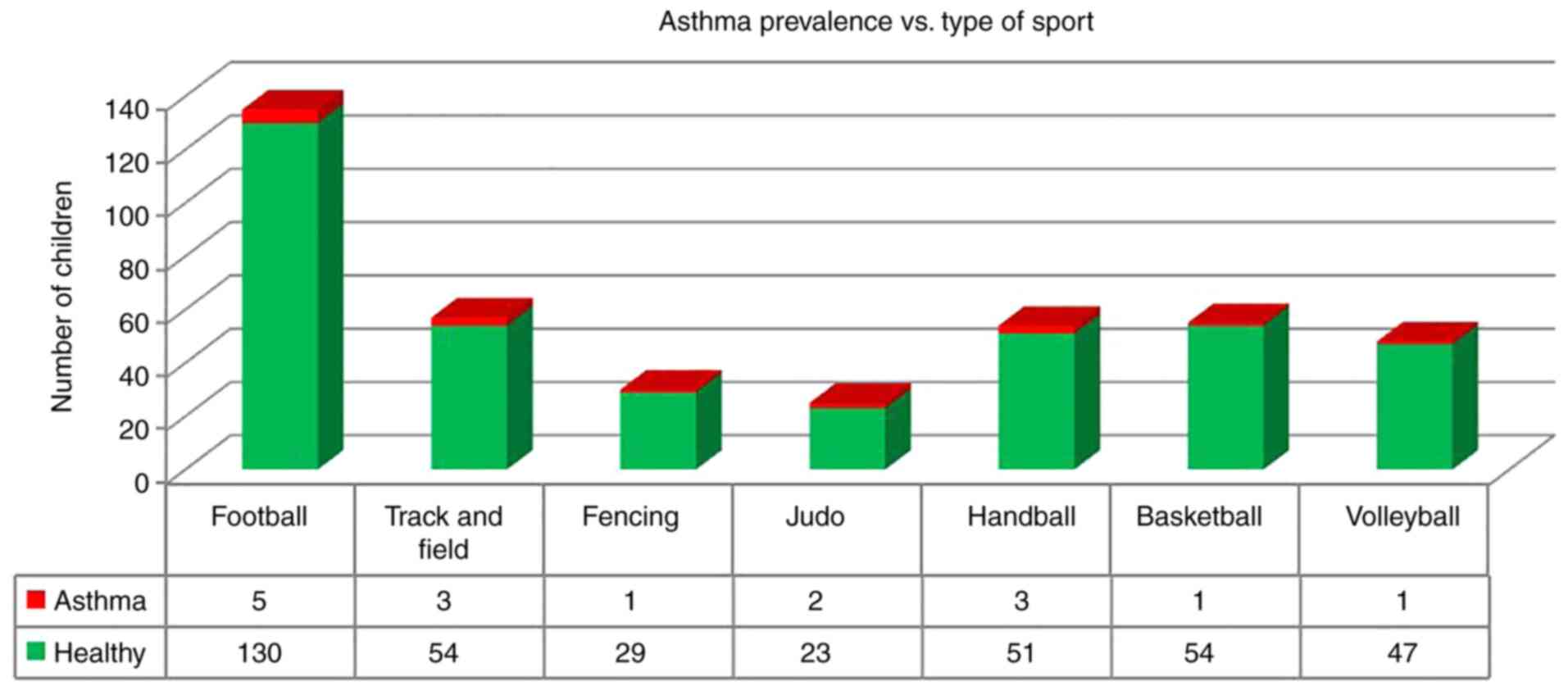
The asthma prevalence in the study group was 3.96%
(16 children; Fig. 1). Asthmatic
patients were diagnosed with the mild form of the disease and the
physical exercise was not a trigger for asthma exacerbation.
Pulmonary function testing
After anamnesis and clinical examination, FeNO
measurements followed by pulmonary function testing (spirometry:
Pre- and post-bronchodilator).
In terms of spirometric evaluation, 33 children
showed signs suggesting asthma (PEF and FEV1/FVC baseline levels
<80% of predicted values and/or reversibility after use of a
bronchodilatator via Ventolin inhaler). Only 10 of these cases were
previously diagnosed as asthma.
The biochemical detection of exhaled nitric oxide
(FeNO) was performed before the spirometry and the results are
based on molecular proportion as ppb. The patients already
diagnosed with asthma had slightly elevated FeNO levels compared
with the rest of the study group. The Mann-Whitney U test was
performed to determine if there were any differences in FeNO values
between children with asthma and children without asthma.
Distribution values for these groups were not similar, as assessed
by visual inspection. FeNO values for the asthma group (mean rank,
178.78) and non-asthma group (mean rank, 202.48) were not
statistically significantly different (U=2724.5; z=-0.80; P=0.407;
Table II).
 | Table IIFeNO level distribution, according to
various groupings. |
Table II
FeNO level distribution, according to
various groupings.
| FeNO levels, ppb | Average | Standard
deviation | P-value |
|---|
| Diagnosis | | | 0.407a |
|
Asthma
group | | | |
|
Female | 29.80 | 40.99 | |
|
Male | 27.90 | 37.17 | |
|
No asthma
diagnosis | | | |
|
Female | 27.86 | 25.83 | |
|
Male | 23.42 | 22.34 | |
| Location of
sport | | |
<0.0005a,b |
|
Indoors | | | |
|
Female | 29.29 | 26.03 | |
|
Male | 30.29 | 24.86 | |
|
Outdoors | | | |
|
Female | 23.56 | 26.71 | |
|
Male | 19.79 | 21.22 | |
| Diagnosis | | | 0.142c |
|
Asthma
diagnosis, positive spirometry | 29.10 | 39.23 | |
|
Asthma
diagnosis, negative spirometry | 27.5 | 35.56 | |
|
No asthma
diagnosis, positive spirometry | 38.13 | 33.71 | |
|
No asthma
diagnosis, negative spirometry | 24.41 | 22.96 | |
The majority of the patients came from urban areas
(mostly Craiova), as in our previous studies (15-17).
There was no statistical difference with regard to living area or
sex in the patient cohort. A total of 4 patients (3 already
diagnosed with asthma) had very high levels of exhaled nitric oxide
(>100 ppb).
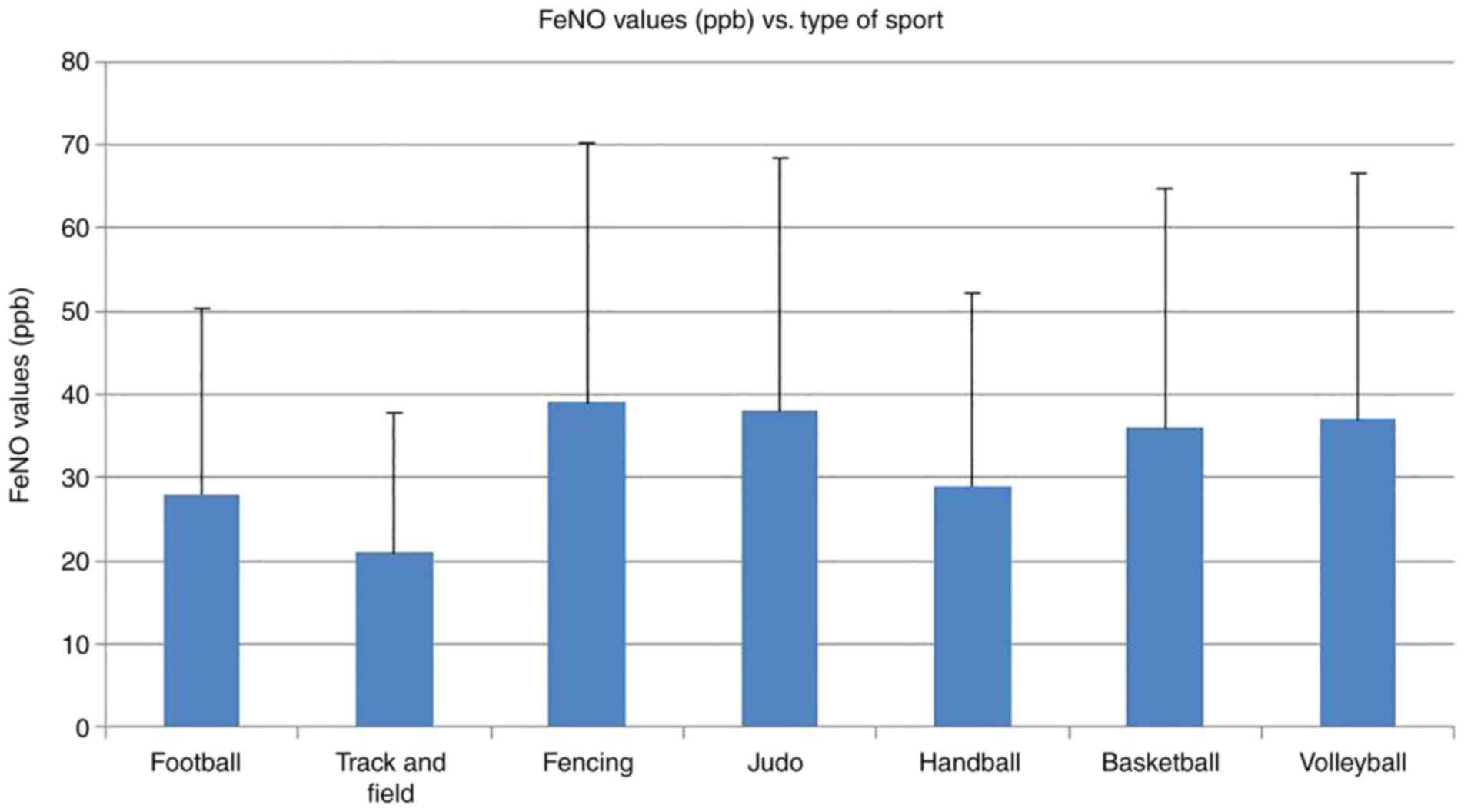
The next step was to evaluate the FeNO values in
various types of sports. The average and standard deviation
measurements are presented in Fig.
2. The average values ranged from 21 ppb for track and field
athletes to 38 ppb for fencing. It was noted that the children
practicing football and track and field had slightly decreased FeNO
levels, but the number of patients was too small to obtain
statistical significance among groups. The outdoor (football, and
track and field) and indoor (fencing, judo, handball, basketball
and volleyball) sports were then compared. Children enrolled in
indoor sports showed elevated levels of exhaled nitric oxide; thus,
it can be concluded that they have a higher level of bronchial
inflammation compared with those children who participate in
outdoor sports. The Mann-Whitney U test was also performed to
determine if there were any differences in FeNO values between
children playing indoor sports and those playing outdoor sports.
Distributions of FeNO values for these groups were similar, as
assessed by visual inspection. Median FeNO level was statistically
significantly higher for indoor sports (median value, 19) than for
outdoor sports (median value, 12) (U=26811.5; z=5.516; P<0.0005;
Table II).
The next stage of the study compared the children at
risk from asthma (the 23 cases without a diagnosis but with
positive spirometry results) with the asthma group and with the
children without a history or spirometry suggesting asthma.
Unexpectedly, the children at risk of asthma had
even higher values of FeNO compared with the asthma group. FeNO
levels had similar distributions for all groups, as assessed by
visual inspection of a boxplot chart. The Kruskal-Wallis H test was
performed to determine if there were differences in FeNO values
between the four groups of participants (asthma group with either
positive or negative spirometry, and the no asthma group with
either positive or negative spirometry). Median FeNO levels were
not statistically significantly different between groups
[χ2(3), 5.446; P=0.142;
Table II].
Discussion
Assessing airway inflammation using FeNO is a
relatively new way of monitoring, as it has only become widely
available in the last two decades. Some medical specialties seem to
be interested in this tool (rheumatology, dermatology, Ear, Nose
and Throat, and psychiatry), but the main research is based on
pneumology. The list of available pathologies is still open, as the
inflammation is related to a wide range of diseases (18-22).
Monitoring the inflammation in various sports may be a valuable
tool in diagnosing a wide range of diseases and to predict the
imminence of exacerbation (i.e. asthma attack) (23-26).
The asthma prevalence in the present study seemed
low, but a number of the patients were undiagnosed, as asthma is
still an underdiagnosed condition in Romania, both in children and
adults. The results of the spirometry testing combined with FeNO
measurements showed that a number of so called ‘healthy’ children
had an asthmatic profile.
In the present study, children practicing 7 types of
sports were enrolled and asthma cases were reported in all of them.
The popularity of football, especially in the Craiova region, is so
high that 33.4% of the cases were of young footballers. The FeNO
measurements, stratified by type of sport, showed decreased levels
in football, and track and field, followed by handball.
When the outdoor sports (football, and track and
field) and indoor sports (fencing, judo, handball, basketball and
volleyball) were compared, the FeNO levels were found to be
significantly higher in the children practicing indoor sports, thus
we hypothesize that bronchial inflammation is greater in these
athletes. Although the asthma cases were not more frequent in this
subgroup, the risk of having a bronchospasm may be higher, and
these children may be at risk of respiratory failure during an
intense effort. The precise cause of these higher levels is
unknown, but it can be theorized that the environment is to blame,
as a number of these children are practicing sports in old
buildings, with intense humidity and molds.
Unfortunately, the data gathered until now for
asthma has placed the FeNO measurement as a secondary tool in the
diagnosis and management of asthma, as the research recorded has
had conflicting results (10,27,28).
However, the technique is widely available, easy to perform and
non-invasive, so the interest in clinical settings remains
high.
In conclusion, using a portable electrochemical
analyzer to evaluate children at risk of an asthma attack,
especially athletes, may be an opportunity to prevent exacerbation
of the condition, which may be life threatening. Encouraging
children to practice sports is one of the cornerstones of pediatric
education, but the advantages and the dangers of this activity must
be balanced. The electrochemical evaluation of bronchial
inflammation is an accessible tool that can help medical staff to
identify children at risk of developing a bronchospasm during
intense physical activity.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RD, FD and ADG conceptualized the study, prepared
the initial draft and shared first authorship. CD, DS and MAD
acquired the raw data, and also performed the literature data
collection. RD and DS confirm the authenticity of all the raw data.
LS, NM and MI analyzed and interpreted the patient data. NM and DS
also provided essential critical revisions. All authors have read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
Informed consent was obtained from parents or legal
guardians for all children. Prior approval for the study was
obtained from the Ethics Committee of the University of Medicine
and Pharmacy of Craiova (Craiova, Romania). The Filantropia
Municipal Hospital, the Infectious Disease Hospital and the
Clinical Emergency County Hospital are all part of the Clinical
Departments of the University of Medicine and Pharmacy of
Craiova.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Carlsen KH, Anderson SD, Bjermer L, Bonini
S, Brusasco V, Canonica W, Cummiskey J, Delgado L, Del Giacco SR,
Drobnic F, et al: Exercise-induced asthma, respiratory and allergic
disorders in elite athletes: Epidemiology, mechanisms and
diagnosis: Part I of the report from the Joint Task Force of the
European Respiratory Society (ERS) and the European academy of
allergy and clinical immunology (EAACI) in cooperation with GA2LEN.
Allergy. 63:387–403. 2008.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Norqvist J, Eriksson L, Söderström L,
Lindberg A and Stenfors N: Self-reported physician-diagnosed asthma
among Swedish adolescent, adult and former elite endurance
athletes. J Asthma. 52:1046–1053. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Selge C, Thomas S, Nowak D, Radon K and
Wolfarth B: Asthma prevalence in German Olympic athletes: A
comparison of winter and summer sport disciplines. Respir Med.
118:15–21. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Maniscalco M, Vitale C, Vatrella A, Molino
A, Bianco A and Mazzarella G: Fractional exhaled nitric
oxide-measuring devices: Technology update. Med Devices (Auckl).
9:151–160. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
American Thoracic Society and European
Respiratory Society. ATS/ERS recommendations for standardized
procedures for the online and offline measurement of exhaled lower
respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir
Crit Care Med. 171:912–930. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Dweik RA, Boggs PB, Erzurum SC, Irvin CG,
Leigh MW, Lundberg JO, Olin AC, Plummer AL and Taylor DR: American
Thoracic Society Committee on Interpretation of Exhaled Nitric
Oxide Levels (FENO) for Clinical Applications. An official ATS
clinical practice guideline: Interpretation of exhaled nitric oxide
levels (FENO) for clinical applications. Am J Respir Crit Care Med.
184:602–615. 2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Gonzalez A, Mares AV and Espinoza DR:
Common pulmonary conditions in sport. Clin Sports Med. 38:563–575.
2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Harnan SE, Tappenden P, Essat M, Gomersall
T, Minton J, Wong R, Pavord I, Everard M and Lawson R: Measurement
of exhaled nitric oxide concentration in asthma: A systematic
review and economic evaluation of NIOX MINO, NIOX VERO and
NObreath. Health Technol Assess. 19:1–330. 2015.PubMed/NCBI View
Article : Google Scholar
|
|
9
|
Olaguibel JM, Parra A, Alvarez MJ, Quirce
S and Lopez R: Measurements of fractional exhaled nitric oxide with
2 portable electrochemical sensors: A comparative study. J Investig
Allergol Clin Immunol. 21:322–333. 2011.PubMed/NCBI
|
|
10
|
Global Initiative for Asthma. Global
Strategy for Asthma Management and Prevention, 2019. Available
from: https://ginasthma.org.
|
|
11
|
Torretta S, Drago L, Marchisio P,
Cappadona M, Rinaldi V, Nazzari E and Pignataro L: Recurrences in
chronic tonsillitis substained by tonsillar biofilm-producing
bacteria in children. Relationship with the grade of tonsillar
hyperplasy. Int J Pediatr Otorhinolaryngol. 77:200–204.
2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Oswieximska J, Ziora K, Ziora D, Machura
E, Smerdzinski S, Pis-Spychala M, Kasperski J, Zamlynski J and
Kasperska-Zajac A: Elevated levels of exhaled nitric oxide in
patients with anorexia nervosa. Eur Child Adolesc Psychiatry.
23:845–850. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Caillaud D, Horo K, Baiz N, Banerjee S,
Charpin D, Lavaud F, de Blay F, Raherison C and Annesi-Maesano I:
Exercise-induced bronchospasm related to different phenotypes of
rhinitis without asthma in primary schoolchildren: The French Six
Cities Study. Clin Exp Allergy. 44:858–866. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kuti BP, Kuti DK, Omole KO, Mohammed LO,
Ologun BG and Oso BI: Prevalence and factors associated with
exercise-induced bronchospasm among rural school children in Ilesa,
Nigeria. Niger Postgrad Med J. 24:107–113. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Diaconu R, Stanescu L, Diaconu C and
Niculescu C: Exhaled nitric oxide in pediatric athletes admitted to
a sports medicine department. Eur Respir J. 46 (Suppl
59)(PA3648)2015.
|
|
16
|
Diaconu R, Stanescu L, Diaconu C and Calin
G: Exhaled nitric oxide and the therapeutic regimens in childhood
asthma. Eur Respir J. 42 (Suppl 57)(P1119)2013.
|
|
17
|
Diaconu R, Diaconu C and Dumitra G:
(Craiova, Sadova Romania). Exhaled nitric oxide and serum IgE in
children admitted to a pediatric department. Eur Respir J. 40:
(Suppl 56)(P4577)2012.
|
|
18
|
Dop D, Gheonea C, Stanescu GL, Morosanu
AE, Diaconu R, Niculescu CE, Ognean ML and Niculescu D: Aspiration
pneumonia in an infant with neurological sequelae-case report. Rom
J Morphol Embryol. 56:1191–1194. 2015.PubMed/NCBI
|
|
19
|
Stanescu GL, Plesea IE, Diaconu R, Gheonea
C, Sabetay C, Tistea D and Niculescu EC: Meckel's diverticulum in
children, clinical and pathological aspects. Rom J Morphol Embryol.
55 (3 Suppl):S1167–S1170. 2014.PubMed/NCBI
|
|
20
|
Diaconu R, Oprea B, Vasilescu MM,
Niculescu EC, Ciobanu MO, Diaconu C, Gheonea C and Stanescu GL:
Inflamed molluscum contagiosum in a 6-year-old boy: A case report.
Rom J Morphol Embryol. 56 (2 Suppl):S843–S845. 2015.PubMed/NCBI
|
|
21
|
Zaharie MN, Carstea D, Streba CT, Mitrut
P, Glodeanu AD, Carstea AP, Zaharie SI, Dascalu IT, Tuculina MJ,
Bunget AM, et al: Renal dysfunction-a possible marker of severity
of heart failure. Rev Chim. 69:1435–1440. 2018.
|
|
22
|
Carstea D, Streba LA, Glodeanu AD, Carstea
AP, Vancu M and Ninulescu AM: The accuracy of combined physical
examination and ultrasonography for the detection of abdominal
aorta aneurysm. Rom J Morphol Embryol. 49:569–572. 2008.PubMed/NCBI
|
|
23
|
Feitosa LA, Dornelas de Andrade A, Reinaux
CM and Britto MC: Diagnostic accuracy of exhaled nitric oxide in
exercise-induced bronchospasm: Systematic review. Rev Port Pneumol.
18:198–204. 2012.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Scollo M, Zanconato S, Ongaro R, Zaramella
C, Zacchello F and Baraldi E: Exhaled nitric oxide and
exercise-induced bronchoconstriction in asthmatic children. Am J
Respir Crit Care Med. 161:1047–1050. 2000.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Caspersen C, Stang J, Thorsen E and
Stensrud T: Exhaled nitric oxide concentration upon acute exposure
to moderate altitude. Scand J Med Sci Sports. 23:e102–e107.
2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Stang J, Braten V, Caspersen C, Thorsen E
and Stensrud T: Exhaled nitric oxide after high-intensity exercise
at 2800 m altitude. Clin Physiol Funct Imaging. 35:338–343.
2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Petsky HL, Kew KM, Turner C and Chang AB:
Exhaled nitric oxide levels to guide treatment for adults with
asthma. Cochrane Database Syst Rev. 9(CD011440)2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Petsky HL, Kew KM and Chang AB: Exhaled
nitric oxide levels to guide treatment for children with asthma.
Cochrane Database Syst Rev. 11(CD011439)2016.PubMed/NCBI View Article : Google Scholar
|