Introduction
Finite element analysis can be used to calculate the
tensile stress on a polyethylene tibial insert and von Mises
stress. Polyethylene (PE) wear leads to a process known as
‘particle disease’ a factor of failure of the procedure. Total knee
arthroplasty (TKA) has become a routine intervention for treating
late stage osteoarthritis worldwide. Its success, in terms of
function and survivorship, costs, days of hospitalization, depends
on several factors, including component alignment and ligament
balance (1). The ideal conditions
for success of TKA are still a matter of debate in the literature.
On the one hand, most researchers agree that, for better
survivorship, the overall alignment should be neutral or slightly
valgus and the tibial component must be positioned at a right angle
to the tibial mechanical axis (2,3). On
the other hand, there are studies which have demonstrated no
difference in terms of survival between groups of neutrally aligned
and other then neutrally aligned knees after TKA (4). These authors argue that the mechanical
axis goal of 0±3˚ is not enough to predict the durability of modern
TKA implants (4). Furthermore, an
additional issue of TKA is post-surgery patient satisfaction.
Studies report that patient satisfaction ranges between 75 and 92%,
even in the case of knees with neutral alignment of components. For
example, a systematic review of studies on post-TKA patient
satisfaction published between 2000 and 2012 showed only 85%
satisfaction (5). The new concept
of kinematic knee alignment arose as a response to the issues
discussed above. Kinematic knee alignment aims to improve the
functionality of the patient knee and to control pain, with minimal
surgical involvement, centered on ligament balance (6). Despite the widespread view that
neutral alignment is a condition for TKA success, kinematic knee
alignment does not always ensure neutral overall alignment and
tibial alignment. These findings highlight the combined importance
of both alignment and ligament balance for TKA outcomes. In some
cases, especially in severe varus knees, standard bone cuts and
safety ligament releases may not be enough for balancing the TKA.
In such cases, secondary asymmetric tibial resection may be
necessary to achieve balance, although overall alignment may not
remain neutral. Good knowledge of contact pressures and pressure
areas in TKA is the key to success for the knee implant. It has
been shown that higher contact stress on the tibial bearing
component is associated with more severe damage in the tibial
components (6). The present study
assessed the validity of a finite element analysis for predicting
behavior over time of a cemented knee implant used in TKA, for
different mechanical loads, and the correlation with clinical
outcomes of this procedure.
Patients and methods
Our study took place between 2008 and 2015. A total
of 80 TKAs were performed on 70 patients. The patients were split
in two groups. Whereas in group 1 of 50 TKAs, secondary asymmetric
tibial recut was not necessary, group 2 of 30 TKAs, needed
secondary asymmetric tibial recut for balancing. Out of the 70
patients, the sex ratio was 45:25 in favor of women. At the moment
of TKA, the mean age of the patients was 65.5. The mean body mass
index (BMI) was 24.9 kg/m2. Group 1 consists of 25
female and 18 male patients; mean age 62.5 years, mean BMI 26
kg/m2. Regarding group 2, it included 27 patients, of
which 20 were female and 7 men. Participants in group 2 had a mean
age of 61.4 years and a mean BMI of 23.2 kg/m2. All
surgical procedures were performed by the same senior surgeon. For
all cases, the same type of posterior-stabilized cemented knee
prosthesis (Zimmer-Nexgen) was utilized. All osteophytes were
removed. Next, medial ligament release was performed, using a
subperiosteal osteotome. For the patients in group 1, these actions
alone led to a balanced knee, thus we did not need further
procedures. For the patients in group 2, a further asymmetrical
tibial coronal recut was needed, because of the tightness in
flexion and extension of the medial compartment. The surgeon
removed an extra slice of bone, 2-mm thickness, from the medial
tibial plateau. After this artifice, the knee became balanced, with
equal extension and flexion gaps. Recovery began immediately after
surgery, with alternating placement of the knee in the flexion and
extension positions. Postoperative control was conducted at 6
weeks, 3 months, 6 months, and 1 year periods, and then, once
yearly. The mean follow-up period for the patients was 5 years (±3
years). The range of motion, stability to varus-valgus stress and
Knee Society Score (KSS) (7) were
noted for all patients, preoperatively and during each
postoperative visit. Standing standard AP and a lateral view X-ray
exam of the knee was conducted preoperatively and postoperatively.
We also conducted computational simulations using finite element
analysis of two situations: i) The ideal prosthetic component
positioning, corresponding to group 1 of patients, and ii) the 3˚,
5˚ and 8˚ of varus tibial malposition, but with a balanced knee,
corresponding to patients in group 2. Malposition in varus for the
tibial component results from extensive surgical removal from the
medial part and little removal from the lateral part of the tibial
plateau. The in vivo kinematics tests for the knee, have
been achieved using SIMI Motion (SIMI Reality Motion Systems GmbH),
a performance system for image acquisition and image analysis. The
image acquisition was achieved with two video cameras, high speed,
in two planes at a 90˚angle. The metal implants were made of cobalt
chromium molybdenum alloy (CoCrMo). The femoral component
wasentirely made of CoCrMo alloy. The tibial component consisted of
two parts. One was made of CoCrMo alloy, and the other of PE. The
elastic modulus of the material (polyethylene) was established at
1,016 MPa, and the Poisson constant considered 0.46. The modulus of
elasticity was obtained by the ratio between stress per area unit
and the consecutive deformation.
Statistical analysis
SPSS software 20 (IBM Corp.) was used for
statistical analysis. P<0.05 was assigned to indicate
statistical significance. The results are expressed as the value of
the standard deviation ± the arithmetic mean for continuous
quantitative variables. Quantitative variables were expressed as
proportions. The independent t-test was performed to determine
statistical significance. We considered the results to be
statistically significant if the P-values concerning the two groups
were <0.05, with a 95% confidence interval.
Results
We found no statistically significant differences
between the group 1 and 2 regarding demographic characteristics:
Age, sex, height and weight. In addition, we noted no differences
in terms of postoperative evolution of KSS, frontal laxity and
range of motion (Table I).
 | Table IPostoperative outcomes. |
Table I
Postoperative outcomes.
| | Group 1
(P<0.001) | Group 2
(P<0.001) |
|---|
| Score | Preoperative | Postoperative | Preoperative | Postoperative |
|---|
| Knee society
score | 25.15±12.1 | 96.3±5.6 | 20.45±10.1 | 92.15±12.1 |
| Range of motion | 76.4±24.3˚ | 110.3±9.7˚ | 70.5±20.8˚ | 100.4±20.3˚ |
| Frontal laxity | 8.81±2.8˚ | 1.34±1.2˚ | 10.5±4.8˚ | 1.7±1.4˚ |
However, we did observe a statistically significant
difference between the groups, regarding the positioning of the
tibial component. The mean angle between the tibial component and
the tibial mechanical axis was 1±3.5˚ of varus for group 1, and
respectively 3±3.5˚ of varus for group 2 (P<0.001). We did not
need any revision for any of the operated knees at the final
follow-up period. The mean follow-up interval was 6 years. The
results of the finite element analysis are summarized in Table II.
 | Table IIFinite element analysis. |
Table II
Finite element analysis.
| Alignment | Maximum contact
pressure (megapascal) | Mean contact
pressure-medial condyle (megapascal) | Mean contact
pressure-lateral condyle (megapascal) |
|---|
| Mechanical | 10.90 | 6.00 | 6.00 |
| 3˚ of varus | 12.10 | 6.26 | 5.00 |
| 5˚ of varus | 16.30 | 14.00 | 7.00 |
| 8˚ of varus | 18.30 | 16.00 | 9.00 |
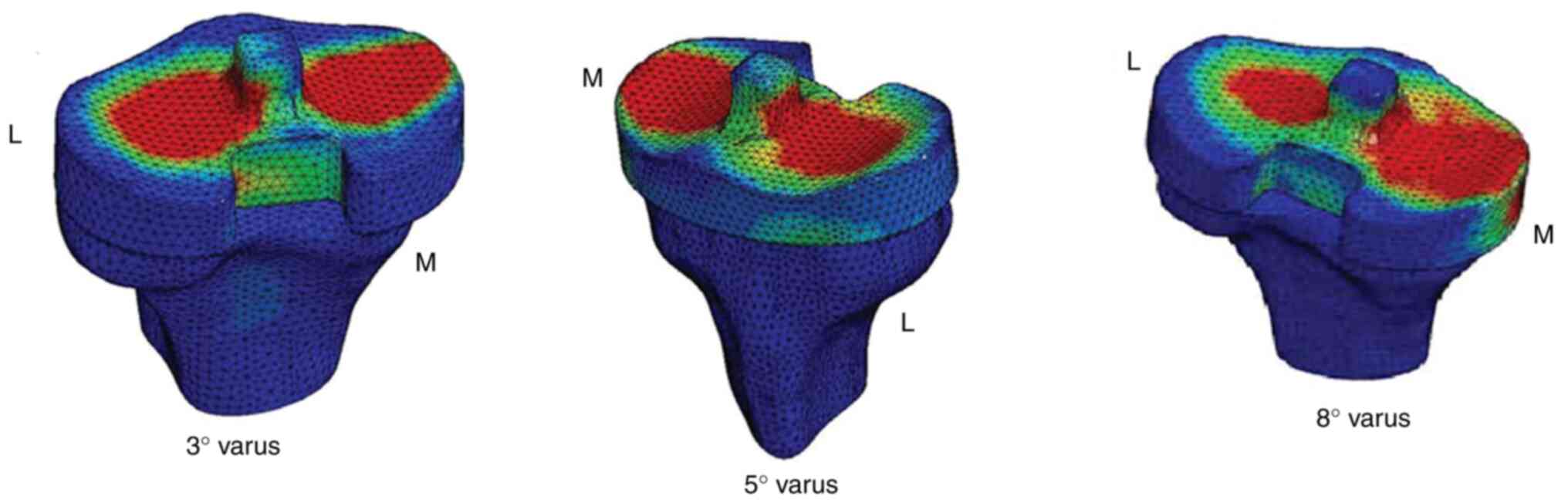
We also measured the stress around the tibial post
for 3˚, 5˚ and 8˚ of tibial varus malalignment (Fig. 1).
For 3˚, the maximum contact pressure (13.7 MPa) was
around the base of the tibial post, especially on the lateral side.
Towards the tip of the post there was a decrease in pressure: 5.4
MPa on the lateral side (L) and 4 MPa on the medial (M) side. For
5˚, the maximum contact pressure increased to 17.5 MPa around the
post base. At the top of the post, the contact pressure was 8 MPa
placed on the lateral part and 3.5 MPa on the medial part. For 8˚,
the maximum contact pressure increased to 22.5 MPa around the post
base. At the top of the post, the contact pressure was 6.5 MPa on
the medial side of the tibial plateau and 14.1 MPa on the lateral
side.
Discussion
If the contact pressure areas are known, it is
possible to provide the potential wear of polyethylene (PE). The
higher the contact pressure on the tibial component, the more
severe the damage to the implant may be, due to particle disease
(6). Polyethylene is a polymer
which contains CH2-chains (8,9). For
orthopedic implants, a type of this polymer is used, ultra-high
molecular weight (UHMWPE). The elastic modulus of PE diminishes
with tension. PE is a viscous-elastic implant, having the potential
of plastic deformation in addition to wear. Beside wear, creep and
plastic deformation may occur in PE fatigue. Long polymer chains of
PE can slide over each other, resulting in creeping (10). Creep is responsible for
delaminating, but decreases over time (10). The wear of PE results in particle
debris between 0.2 to 10 µm which results in phagocytosis by
macrophages. The macrophages activate other mediators responsible
for osteolysis such as tumor necrosis factor (TNF) α, interleukin
(IL)-1, and IL-6, or act like osteoclasts with direct bone
resorption (10). A proper position
of the implant is crucial for prosthetic joint load distribution,
wear and survival of the prosthesis (6). The best placement of the prosthetic
knee implant components remains uncertain. The disagreement among
orthopedic surgeons is magnified by the important number of
patients displeased with TKA. Most surgeons have concluded that a
good alignment provides the best chances for survivorship of TKA
(6). Mechanical best alignment
represents the condition in which both angles between the femoral
cut and the mechanical axis of the femur, respectively, between the
tibial cut and the mechanical axis of the tibia have 90˚ (11). However, some authors show that a
femoral component placed in a 7˚ valgus position, with the tibial
plateau perpendicular to the long axis of the tibia, ensures an
equal distribution of forces between the medial and the lateral
sides and in consequence, assuring the best chances for
survivorship (12). Howell et
al considers that kinematic knee alignment is provided by
aligning the transverse femoral component axis with the primary
transverse axis in the femur about which the tibia makes movement
of flexion and extension. The authors also consider, regarding the
tibial component, that the longitudinal tibia axis should make a
90˚ angle with the transverse femoral axis, about which flexion and
extension of the tibia take place (13). For this purpose, the femoral cut
should be made 1˚-2˚ more valgus, while the tibial cut should be
made 1˚-2˚ varus, compared to the mechanically aligned TKA
(14). Surgeons who support this
approach claim that the restoration of mechanical alignment becomes
improper in patients with constitutional alignment in varus or
valgus and could cause increased tension in the collateral
ligaments (15). They also argue
that patients whose previous alignment is restored, may have better
clinical and functional status than patients whose alignment is set
to neutral (16). Irrespective of
the operatory technique for TKA, an important problem for surgeons
is represented by technical details. For example, instrument errors
are of great consequence in this respect. For the femoral distal
cut, precision depends on the intramedullar rod engaging the
isthmus of the medullar canal for realign the anatomical axis. The
precision of placement is influenced by the rod length and
thickness, the diameter of the medullar canal, and by the placement
of the entry hole for the intramedullar guides (13,14).
Therefore, surgeons aiming for mechanical alignment must be aware
that instruments and the location of the entry holes could lead to
large errors. The goal of our TKAs in both groups was to obtain
mechanical alignment. With regard to tibial component alignment, we
observed a significant difference between the two groups. In group
1, there was a neutral alignment (1±3.5˚), while in group 2 it was
in principle in the varus position (3±3.5˚). The vast majority of
patients in group 2 constituted extreme situations, because of
additional asymmetric tibial varus cut. The finite element analysis
showed that in a 3˚ varus inclination of the interline, but with a
balanced knee, the maximum contact pressure measured at the surface
of tibial plateau increased by 11% compared to the value of
mechanical alignment. At 8˚ of inclination the maximum contact
stress intensified by 68%, even for a balanced knee. For 3˚ of
varus the distribution of forces was uniform on both tibial
condyles, and the mean medial contact stress was 1.26 MPa higher
than the lateral contact stress. At 8˚ of varus, we observed a
medial displacement of the contact patch, and the mean medial
contact stress was 7 MPa higher than lateral stress. There are very
few studies regarding post-cam stress of posterior-stabilized knee
prosthesis. Pulosky et al investigated tibial post wear of
certain types of knee prosthesis and found increased wear of the
posterior part of the tibial post (17). Huang et al found a maximum
von Mises contact stress of 21.2 MPa at 60˚ flexion and 27.6 MPa at
150˚ flexion (18). Koh et
al researched post-cam design via finite element analysis to
study the most normal-like knee mechanics (19). Amyand's hernia was a curious
association in one case (20). Our
study showed that for 3˚ of varus inclination of the articular
interline the maximum contact pressure was localized around the
base of the tibial post, especially on the lateral side (13.7 MPa).
As the inclination increased, the stress increased, also at the top
of the post, thus leading to shearing and bending forces around the
lateral and the medial aspect of the surface. These forces added to
those from the posterior component of the post during flexion and
contributed to tibial post wear.
In conclusion, polyethylene has a special abrasive
resistance, shows low friction forces, high impact resistance, good
chemical resistance and high energy absorption in contact with
CoCrMo alloy. Still these advantages are also dependent on multiple
factors such as surgical technique or implant positioning. The
study findings support our technique for balancing severe varus
knee and demonstrated that a computational model can be a useful
tool for predicting clinical outcomes. If more than 3˚ of varus in
the tibia in the coronal plane, more stress will be sent in the
post-cam and on the surface of the implant. Still further studies
are necessary to completely evaluate the loadings, regarding
complex 3D motion of the prosthetic knee and not only by
varus-valgus stress.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
NG, GS and HO had major contributions in the
conception of the study and writing the manuscript. BS, MCTD and NB
analyzed and interpreted the patient data and searched the
literature for similar work and articles and contributed to writing
the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was conducted according to the World
Medical Association Declaration of Helsinki, using a protocol
approved by the local Bioethics Committee from Elias Emergency
Clinical Hospital (Bucharest, Romania). All patients previously
signed an informed written consent concerning hospitalization,
treatment and possible future publication of data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare no conflict or competing
interests.
References
|
1
|
Savlovschi C, Serban D, Andreescu Cv,
Dascalu Am and Pantu H: Economic analysis of medical management
applied for left colostomy. Chirurgia (Bucur). 108:666–669.
2013.PubMed/NCBI
|
|
2
|
Fang DM, Ritter MA and Davis KE: Coronal
alignment in total knee arthroplasty: Just how important is it? J
Arthroplasty. 24:39–43. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Berend ME, Ritter MA, Meding JB, Faris PM,
Keating EM, Redelman R, Faris GW and Davis KE: Tibial component
failure mechanisms in total knee arthroplasty. Clin Orthop Relat
Res. 428:26–34. 2004.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Parratte S, Pagnano MW, Trousdale RT and
Berry DJ: Effect of postoperative mechanical axis alignment on the
fifteen-year survival of modern, cemented total knee replacements.
J Bone Joint Surg Am. 92:2143–2149. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Schulze A and Scharf HP: Satisfaction
after total knee arthroplasty: Comparison of 1990-1999 with
2000-2012. Orthopade. 42:858–865. 2013.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
6
|
Dossett HG, Swartz GJ, Estrada NA, Lefevre
GW and Kwasman BG: Kinematically versus mechanically aligned total
knee arthroplasty. Orthopedics. 35:e160–e169. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Insall JN, Dorr LD, Scott RD and Scott WN:
Rationale of the knee society clinical rating system. Clin Orthop
Relat Res. 248:13–14. 1989.PubMed/NCBI
|
|
8
|
Socea B, Socea LI, Bratu OG, Mastalier B,
Dimitriu M, Carap A and Constantin VD: Recurrence rates and mesh
shrinkage after polypropylene vs. Polyester mesh hernia repair in
complicated hernias. Revista de Materiale Plastice. 55:79–81.
2018.
|
|
9
|
Socea B, Carâp A, Bratu OG, Diaconu CC,
Dimitriu M, Socea LI, Bobic S and Constantin VD: The role of the
composite and biologic meshes in the trocar site hernia repair
following laparoscopic surgery. Revista de Materiale Plastice.
55:146–148. 2018.
|
|
10
|
Bitar D and Parvizi J: Biological response
to prosthetic debris. World J Orthop. 6:172–189. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Insall JN, Binazzi R, Soudry M and
Mestriner LA: Total knee arthroplasty. Clin Orthop Relat Res.
192:13–22. 1985.PubMed/NCBI
|
|
12
|
Hsu RW, Himeno S, Coventry MB and Chao EY:
Normal axial alignment of the lower extremity and load-bearing
distribution at the knee. Clin Orthop Relat Res. 255:215–227.
1990.PubMed/NCBI
|
|
13
|
Howell SM, Roth JD and Hull ML: Kinematic
alignment in total knee arthroplasty. Definition, history,
principle, surgical technique, and results of an alignment option
for TKA. Arthropaedia. 1:44–53. 2014.
|
|
14
|
Howell SM and Hull ML: Kinematic alignment
in total knee arthroplasty. In: Insall & Scott Surgery of the
Knee. Scott N (ed). 5th edition. Chapter 121. Elsevier-Churchill
Livingstone, Philadelphia, pp1255-1268, 2012.
|
|
15
|
Gu Y, Roth JD, Howell SM and Hull ML: How
frequently do four methods for mechanically aligning a total knee
arthroplasty cause collateral ligament imbalance and change
alignment from normal in white patients? J Bone Joint Surg Am.
96(e101)2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Vanlommel L, Vanlommel J, Claes S and
Bellemans J: Slight undercorrection following total knee
arthroplasty results in superior clinical outcomes in varus knees.
Knee Surg Sports Traumatol Arthrosc. 21:2325–2330. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Puloski SK, McCalden RW, MacDonald SJ,
Rorabeck CH and Bourne RB: Tibial post wear in posterior stabilized
total knee arthroplasty: An unrecognized source of polyethylene
debris. J Bone Joint Surg Am. 83:390–397. 2001.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Huang CH, Liau JJ, Cheng CK and Huang CH:
Influence of post-cam design on stresses on posterior-stabilized
tibial posts. Clin Orthop Relat Res. 450:150–156. 2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Koh YG, Son J, Kwon OR, Kwon SK and Kang
KT: Effect of post-cam design for normal knee joint kinematic,
ligament, and quadriceps force in patient-specific
posterior-stabilized total kneearthroplasty by using finite element
analysis. Biomed Res Int. 2018(2438980)2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Savlovschi C, Brănescu C, Serban D, Tudor
C, Găvan C, Shanabli A, Comandaşu M, Vasilescu L, Borcan R,
Dumitrescu D, et al: Hernia Amyand-caz clinic [Amyand's hernia-a
clinical case]. Chirurgia (Bucur). 105:409–414. 2010.PubMed/NCBI
|