Introduction
Among all patients with acute coronary syndrome
(ACS), ~50% suffer from atherosclerosis involving multiple vessels
or the entire coronary tree (1).
Compared with single-vessel disease, ST-elevation myocardial
infarction (STEMI) with multivessel disease is associated with a
worse prognosis (2). The results of
the Abciximab Intracoronary versus intravenously Drug Application
in STEMI demonstrated that although multivessel coronary artery
disease (CAD) is not associated with reduced success of
reperfusion, multivessel disease is associated with a high risk of
adverse clinical outcomes (2).
Treatment strategies for STEMI and multivessel disease remain
controversial, including percutaneous coronary intervention (PCI)
for the culprit vessel or non-culprit vessels, as well as the
time-point (3). A useful tool is
required for evaluating the condition and predicting the prognosis
to aid clinical judgment. The Synergy Between Percutaneous Coronary
Intervention with Taxus and Cardiac Surgery (SYNTAX) scoring system
is the most widely used tool to determine the extent and severity
of CAD. The SYNTAX score is positively correlated with all-cause
mortality of patients with CAD after PCI (4). However, the SYNTAX scoring system is
complex and there is currently limited data on the effectiveness of
SYNTAX score in predicting the prognosis of STEMI patients with
multivessel disease.
The fibrinogen-to-albumin ratio (FAR) is the ratio
between serum fibrinogen levels and serum albumin. Being part of
the inflammatory reaction and processes associated with thrombosis,
fibrinogen is a biomarker for the risk of stroke and MI (5). At the same time, hypoalbuminemia is
also associated with severe MI and heart failure (6). The FAR is a valuable biomarker in the
prediction of the prognosis of multiple tumors, including
esophageal squamous cell carcinoma (7), non-small cell lung cancer (8), colorectal cancer (9) and gallbladder cancer (10). A previous study proved that the FAR
is significantly associated with the SYNTAX score and could predict
the severity of CAD in patients with STEMI (11). Hence, it was hypothesized in the
present study that the FAR may be linked to the long-term prognosis
of patients with STEMI and multivessel disease.
Materials and methods
Study population
The patients were recruited from the emergency
department to participate in the present prospective observational
cohort study. All patients included were required to fulfill the
following criteria: i) Age ≥18 years; ii) diagnosis with STEMI and
multiple vessel disease based on coronary angiography; iii) the
patient received revascularization treatment of PCI; iv) the
patient remained alive during the hospital stay; v) the patient and
their family provided written informed consent to participate in
the study. The exclusion criteria were as follows: i) Patients who
were diagnosed with Non-ST elevation myocardial infarction or
unstable angina; ii) patients who were in a coma or unconscious;
iii) patients with cancers, severe infections, serious organ
dysfunction or other serious diseases; iv) patients and families
who were not able to cooperate with the follow-up process.
The 2011 ESC Guidelines for the Management of Acute
Myocardial Infarction in Patients Presenting With ST-segment
Elevation were followed in the present study (12), according to which STEMI was defined
as electrocardiographic ST-segment elevation >2 mm in 2 or more
contiguous chest leads or ≥1 mm in 2 or more limb leads or new
onset of left bundle-branch block, together with chest pain or
other typical symptoms and elevated troponin levels >99th
percentile (13).
A total of 562 patients (Table I) with STEMI and multiple vessel
disease meeting the criteria were recruited for the present study
from July 2012 to September 2013 at Xianyang Central Hospital
(Xianyang, China). Written informed consent was acquired from the
patients and their family. The Medical Ethics Committee of Xianyang
Central Hospital (Xianyang, China) approved the present study (no.
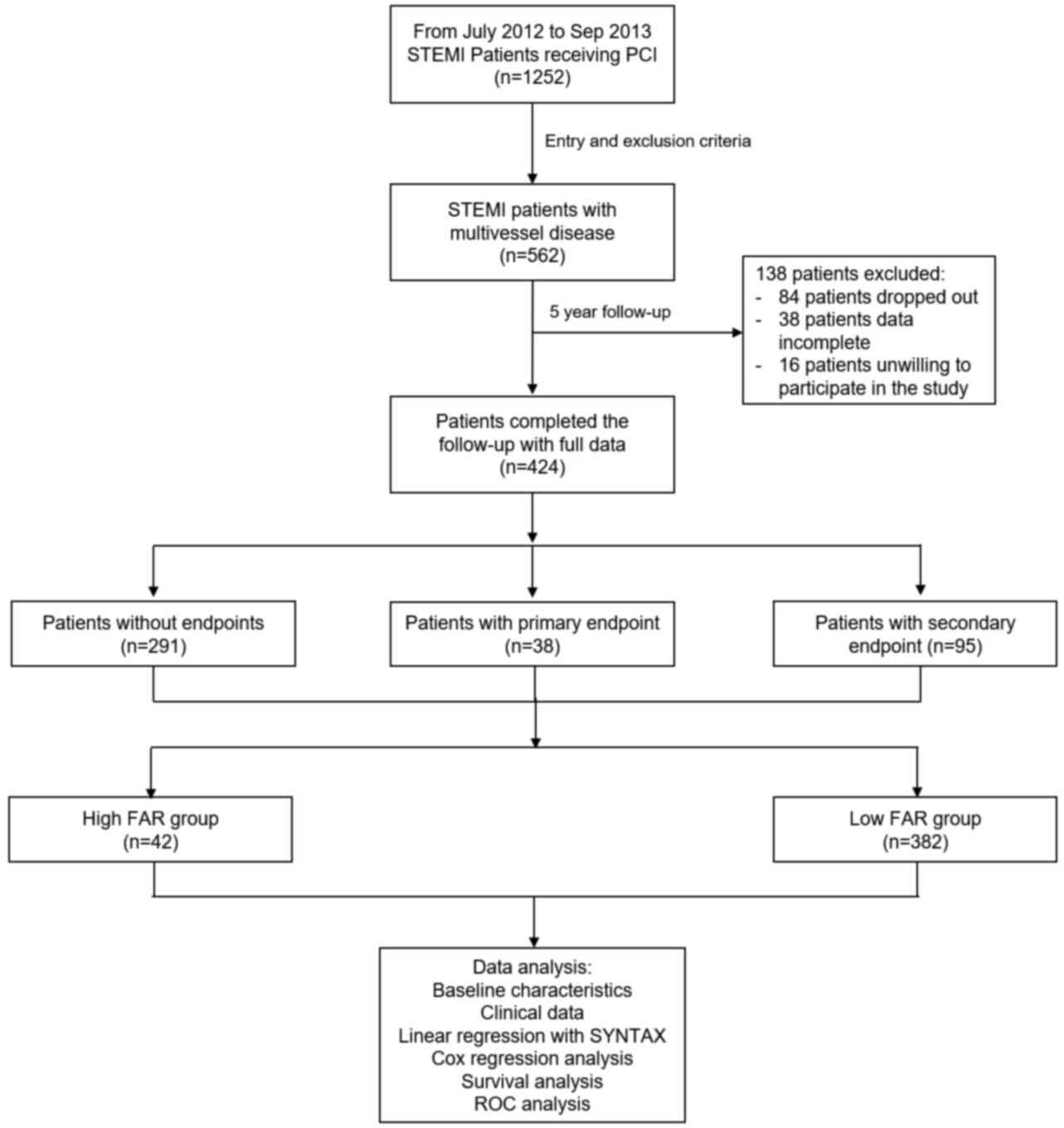
20120535). The study design is presented in the flowchart in
Fig. 1.
 | Table IDemographic characteristics and
clinical data of the patients enrolled stratified by the
endpoints. |
Table I
Demographic characteristics and
clinical data of the patients enrolled stratified by the
endpoints.
| Variables | Patients without
endpoints (n=291) | Patients with primary
endpoint (n=38) | Patients with
secondary endpoint (n=95) | P-valuea |
|---|
| Demographics | | | | |
|
Age
(years) | 61.5±15.8 |
71.5±10.3b |
64.0±12.7b,c | <0.001 |
|
Male
sex | 181 (62.2) | 23 (60.5) | 57 (60.0) | 0.921 |
|
BMI
(kg/m2) | 24.6±3.2 | 25.1±2.7 | 24.1±3.3 | 0.234 |
|
Smoking | 108 (37.1) | 8 (21.1) | 36 (37.8) | 0.136 |
| LVEF | 49.6±10.0 | 45.6±11.7 | 50.4±9.9 | 0.065 |
| Comorbidities | | | | |
|
Heart
failure | 79 (27.1) | 19
(50.0)b | 16
(16.8)c | <0.001 |
|
Hypertension | 68 (23.4) | 16
(42.1)b | 29 (30.5) | 0.031 |
|
Diabetes
mellitus | 46 (15.8) | 5 (13.2) | 15 (15.8) | 0.912 |
|
Chronic
kidney disease | 13 (4.5) | 4 (10.5) | 3 (3.2) | 0.182 |
|
Chronic lung
disease | 34 (11.7) | 3 (7.9) | 8 (8.4) | 0.569 |
|
Cerebrovascular
disease | 17 (5.8) | 1 (2.6) | 9 (9.5) | 0.278 |
|
Tumor | 8 (2.7) | 1 (2.6) | 3 (3.2) | 0.976 |
| Laboratory tests on
admission | | | | |
|
Peak cTnT
(ng/dl) | 4.80 (2.90,
6.39) | 5.43 (3.18,
6.90) | 4.46 (2.93,
6.17) | 0.403 |
|
Peak CK-MB
(ng/dl) | 552.1 (419.8,
668) | 493.7 (379.7,
676.6) | 593.6 (420.3,
717.2) | 0.183 |
|
Creatinine
(µmol/l) | 103.1 (76.2,
131.4) | 112.5 (72.8,
136.0) | 94.0 (70.6,
122.5) | 0.190 |
|
NT-proBNP
(ng/l) | 71.1 (27.3,
123.1) | 91.3 (55.7,
168.4) | 74.2 (35.9,
123.2) | 0.073 |
|
hsCRP
(mg/l) | 21.5 (12.9,
30.2) | 27.1 (21.6,
36.0)b | 24.0 (15.3,
32.3) | 0.008 |
|
ALT
(U/l) | 14 (6, 23) | 17 (9, 24) | 16 (8, 23) | 0.289 |
|
AST
(U/l) | 20 (11, 29) | 24 (10.5,
31.3) | 21 (11, 30) | 0.636 |
|
Fibrinogen
(µg/ml) | 278 (216, 336) | 417 (277,
492)b | 280 (217,
349)c | <0.001 |
|
Albumin
(g/dl) | 3.37 (3.11,
3.69) | 3.14 (2.73,
3.38)b | 3.32 (3.09,
3.56)c | <0.001 |
| SYNTAX score | 20 (16, 23) | 24 (20,
30)b | 19 (16,
22)c | <0.001 |
| FAR | 81.2 (63.4,
99.5) | 136.6 (98.3,
156.3)b | 84.0 (67.3,
106.0)c | <0.001 |
In-hospital treatment
Coronary angiography and interventional therapy were
routinely performed. The ‘infarct-related artery only’ strategy for
PCT was adopted in the present study (14). Successful PCI was defined as
coronary angiography indicating residual lumen stenosis of <10%
and a blood flow classification of Thrombolysis in MI grade
3(15). In patients with emergency
PCI, 300 mg aspirin was administered as soon as possible prior to
surgery, and furthermore, oral clopidogrel 300-600 mg or ticagrelor
180 mg was administered orally. Patients were given oral aspirin
100 mg/day and clopidogrel 75 mg/day (or ticagrelor 90 mg twice
daily) for at least 1 year according to the 2011 ESC Guidelines for
the Management of Acute Myocardial Infarction in Patients
Presenting With ST-segment Elevation (12).
Data collection
Clinical data were collected from the electronic
medical record database of Xianyang Central Hospital. The FAR was
calculated from serum fibrinogen and albumin concentrations on
admission. Plasma fibrinogen levels were detected by the
coagulation method using STA CompactMax automatic coagulation
analyzer (Diagnostica Stago Ltd.) and high-sensitivity c-reactive
protein (hs-CRP) was detected by immunoturbidimetry using an AU5400
automatic biochemical analyzer (Olympus Corporation). Albumin
levels and myocardial injury markers, including cardiac troponin T
(cTnT) as well as creatinine kinase (CK)-MB, creatinine,
NT-proB-type natriuretic peptide (NT-proBNP), alanine
aminotransferase (ALT) and aspartate aminotransferase (AST) were
also tested using the Abbott Architect C16000 autoanalyzer (Abbott
Laboratories) on admission.
Clinical endpoints
The primary endpoint was defined as all-cause
mortality during follow-up and the secondary endpoint was a
composite of major adverse cardiac events (MACE), including
myocardial infarction (MI), stroke, unscheduled revascularization
and rehospitalization due to heart failure.
Follow-up
All patients enrolled were followed up by telephone
or visits to the original clinics where they were enrolled every
year for a total of 5 years. The parameters determined during
follow-up included survival status, recent readmission and other
complications. The data of cases with self-dropout or missed
contact were considered as censored data.
Statistical analysis
SPSS version 19.0 (IBM Corp) was used for
statistical analysis in the present study. The variables were first
subjected to a normality of distribution test (Kolmogorov-Smirnov
test). Continuous variables following a normal distribution were
expressed as the mean ± standard deviation and categorical
variables were presented as proportions, while continuous variables
that did not fit a normal distribution were described as the median
and interquartile range. Comparison of continuous variables between
different groups was performed using one-way analysis of variance
and Tukey's multiple-comparisons test of independent samples. The
Kruskal-Wallis test and Dunn's multiple-comparisons test were
adopted for comparison of different groups for non-normal
distributed variables of independent samples. A χ2 test
was performed for comparisons of categorical variables. Linear
regression analysis was used to examine the correlation between the
SYNTAX score and the FAR.
A receiver operating characteristic (ROC) curve
analysis was also performed to determine the best cut-off value of
the FAR in predicting all-cause death, based on which all patients
were divided into a high FAR group and a low FAR group. The Cox
proportional hazards model was adopted as the regression method to
determine hazard ratios (HR) compare the relative hazard between
the high FAR group and the low FAR group. Univariate analysis
between covariates and endpoints was performed and covariates with
P<0.10 were entered into the multivariate analysis. The survival
status was compared between the two groups via Kaplan-Meier
survival curves and log-rank tests. P<0.05 was considered to
indicate statistical significance.
Results
Demographics and baseline
characteristics
A total of 562 patients were enrolled in the current
study, with an average age of (68.3±20.3 years), a male/female
ratio of 64.9% (365/562). Among the 562 patients, =424 patients
completed the 5-year follow-up. During this period, 38 cases of
all-cause death occurred, while secondary endpoints were observed
in 95 patients, including 41 cases of recurrent MI, 31 cases of
unscheduled revascularization, 13 cases of rehospitalization due to
heart failure and 10 cases of stroke. The remaining 291 patients
did not reach any endpoint.
The demographics and baseline data of patients
without endpoints, patients with the primary endpoints and patients
with secondary endpoints we compared in Table I. The three groups had similar data
in terms of sex ratio, body mass index and smoking status (all
P>0.05). However, the patients with primary endpoints were
significantly older than those in the other two groups
(P<0.001). Furthermore, they had a significantly higher
proportion of heart failure (P<0.001) and hypertension (P=0.031)
than other two groups, but the three groups had no disparity in
diabetes mellitus, chronic kidney disease, chronic lung disease,
cerebrovascular disease and tumors (All P>0.05). As for
laboratory test results on admission, no significant difference was
identified among the three groups in peak cTnT, peak CK-MB,
creatinine, NT-proBNP, ALT and AST (all P>0.05), while patients
with primary or secondary endpoints had significantly higher hs-CRP
(P<0.001) and fibrinogen (P<0.001) and lower albumin
(P<0.001).
Lesions and treatment
The coronary artery lesions and treatments were
compared between the different groups (Table II). As for the angiographic
findings, a great disparity between patients with and those without
endpoints was apparent. The patients with the primary endpoint had
a higher number of diseased arteries and this group had a higher
proportion of patients with 3-vessel disease, left main CAD and
chronic total occlusion (all P<0.01). As a consequence, there
was also a significant difference in the number of stents used in
PCI among the three groups (P<0.001). However, no significant
difference was observed in culprit artery type, use of DES and
medication at discharge (all P>0.05).
 | Table IILesions and treatment of the patients
enrolled stratified by the endpoints. |
Table II
Lesions and treatment of the patients
enrolled stratified by the endpoints.
| Item | Patients without
endpoints (n=291) | Patients with
primary endpoint (n=38) | Patients with
secondary endpoint (n=95) |
P-valuea |
|---|
| Angiographic
findings | | | | |
|
Number of
diseased arteries | 2.3±0.5 |
2.7±0.4b |
2.2±0.3c | <0.001 |
|
≥3-vessel
disease | 104 (35.7) | 25
(65.8)b | 45 (47.4) | 0.001 |
|
LMCA
disease | 10 (3.4) | 6
(15.8)b | 5
(5.3)c | 0.005 |
|
Chronic
total occlusion | 20 (6.9) | 10
(26.3)b | 11 (11.6) | 0.001 |
| Culprit artery | | | | 0.552 |
|
Left
anterior descending artery | 124 (42.6) | 18 (47.4) | 33 (34.7) | |
|
Circumflex
artery | 51 (17.5) | 8 (21.1) | 21 (22.1) | |
|
Right
coronary artery | 114 (39.2) | 11 (28.9) | 40 (42.1) | |
|
Left main
coronary artery | 2 (0.7) | 1 (2.6) | 1 (1.1) | |
| PCI | | | | |
|
Number of
stents | 2.1±0.6 |
2.5±0.5b |
2.4±0.3b | <0.001 |
|
Use of
DES | 80 (27.5) | 15 (39.5) | 28 (29.5) | 0.308 |
| Medication at
discharge | | | | |
|
Aspirin | 289 (99.3) | 38 (100.0) | 94 (98.9) | 0.805 |
|
Clopidogrel | 256 (88.0) | 33 (86.8) | 80 (84.2) | 0.638 |
|
Ticagrelor | 35 (12.0) | 5 (13.2) | 15 (15.8) | 0.638 |
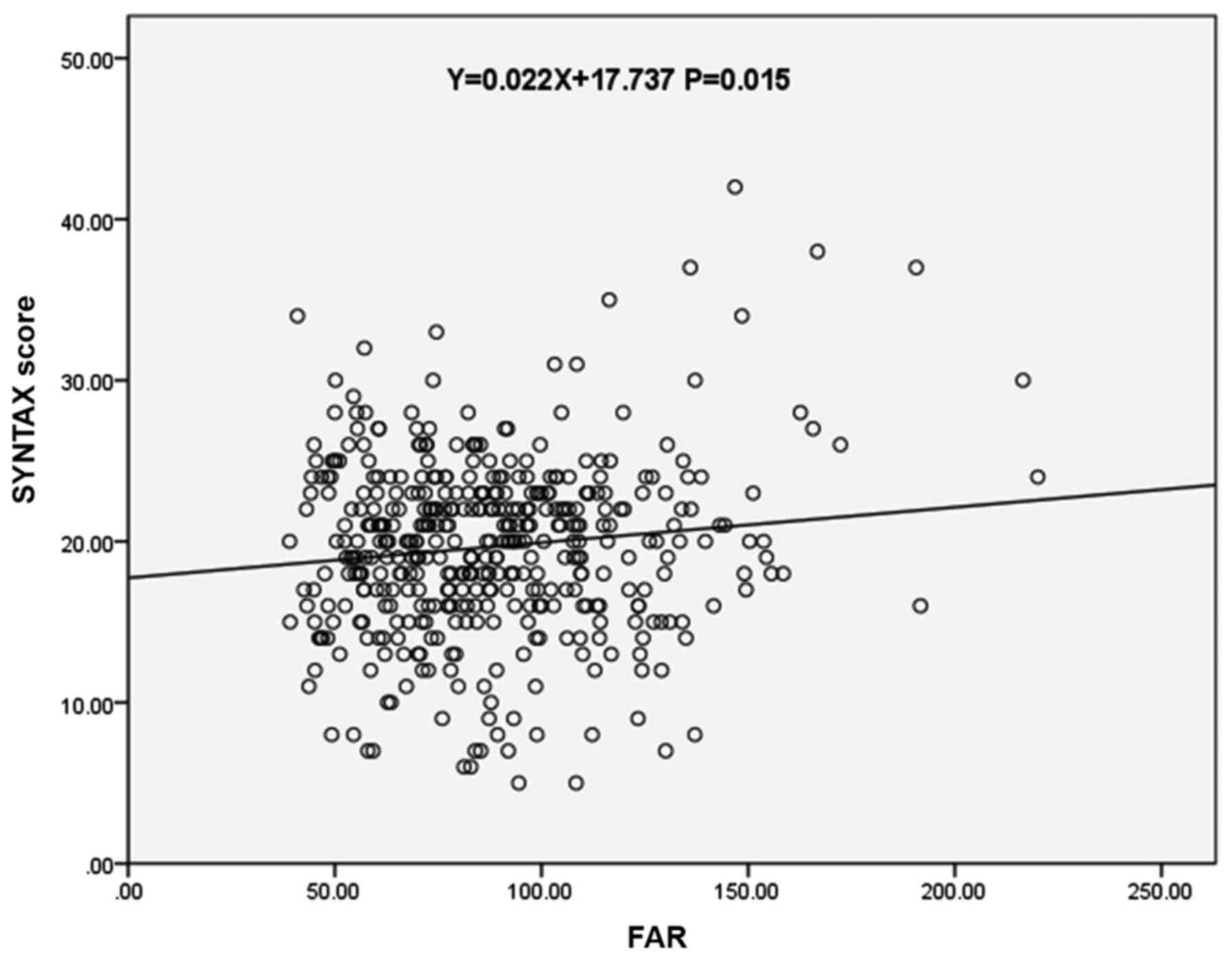
Correlation between SYNTAX score and
the FAR
The association between the SYNTAX score and FAR in
patients with STEMI and multiple vessel disease was also validated.
As presented in Table I, patients
with primary outcomes had a significantly higher SYNTAX score and
FAR than the other two groups (P<0.001). The correlation between
the SYNTAX and the FAR was then examined by linear regression
analysis, which demonstrated that the SYNTAX score had a linear
correlation with the FAR (r, 0.118; y, 0.022x+17.737; P=0.015;
Fig. 2).
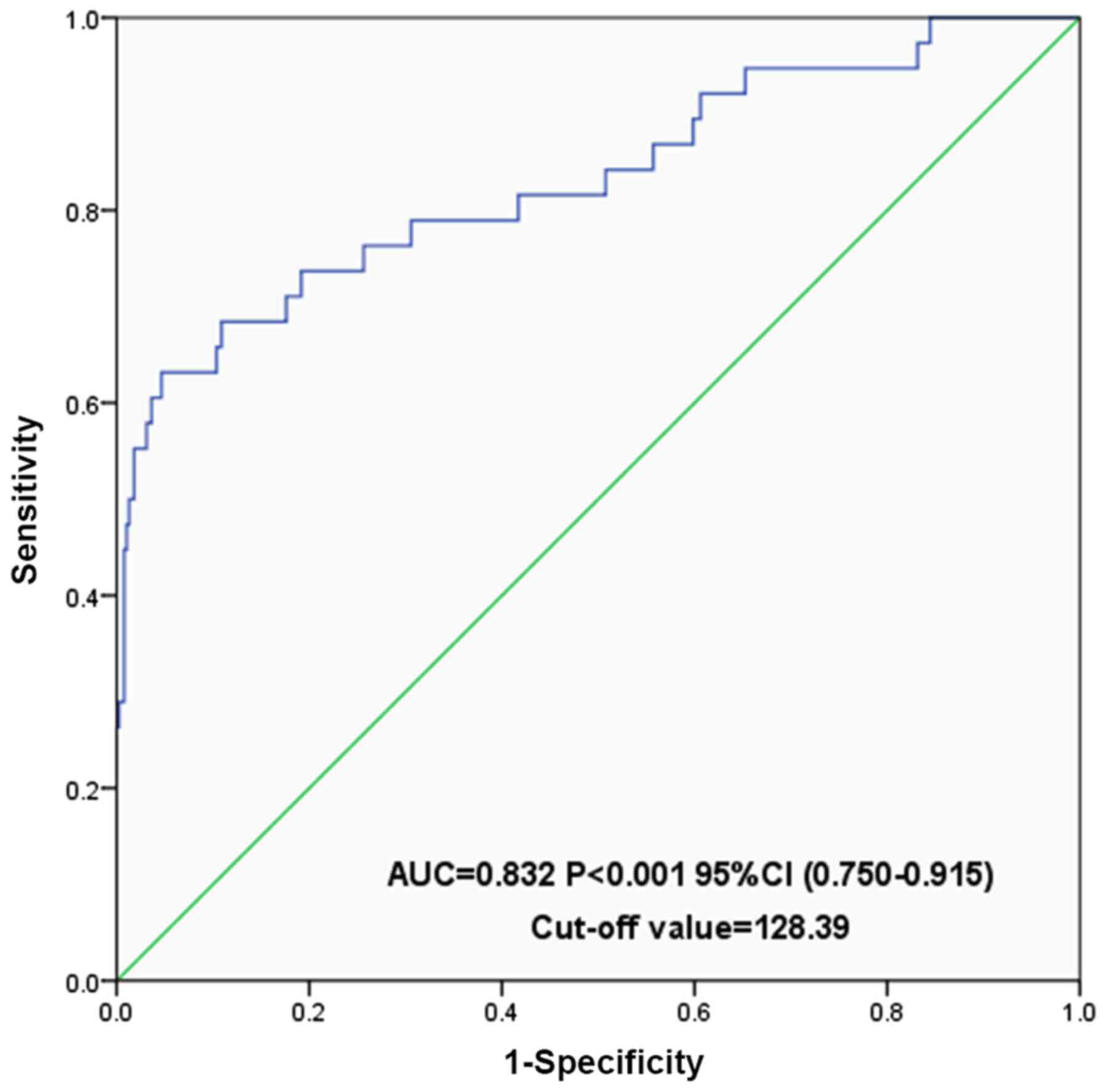
ROC curve analysis
A ROC curve analysis was performed to determine the
value of the FAR in the prediction of the long-term outcomes of
patients with STEMI and multivessel disease (Fig. 3). It was demonstrated that FAR is
significant in predicting all-cause death with an AUC of 0.832 (95%
CI for the AUC, 0.750-0.915; P<0.001) at the ideal cut-off value
of the FAR determined at 128.4. The sensitivity was 63.2% and the
specificity was 95.3%.
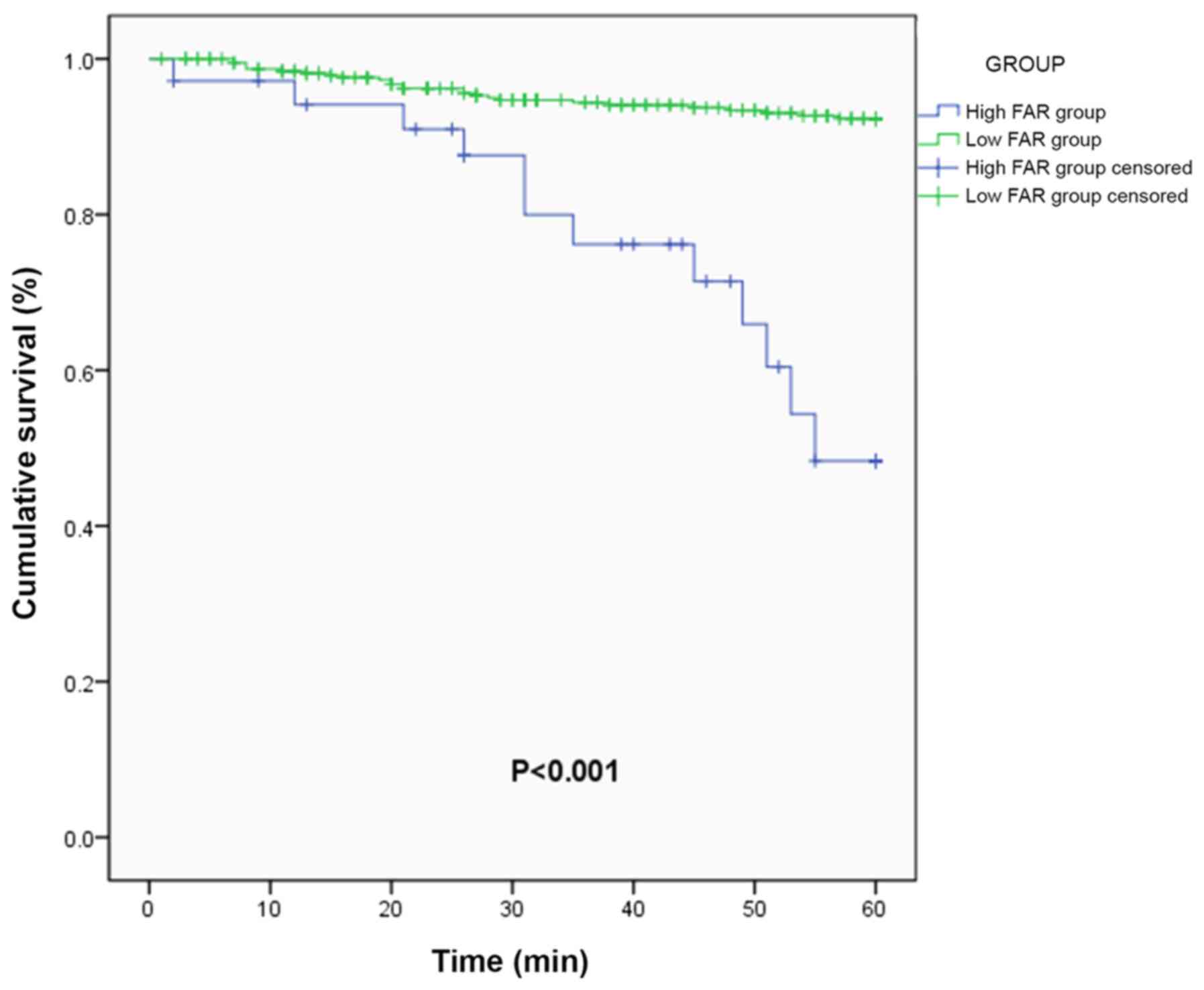
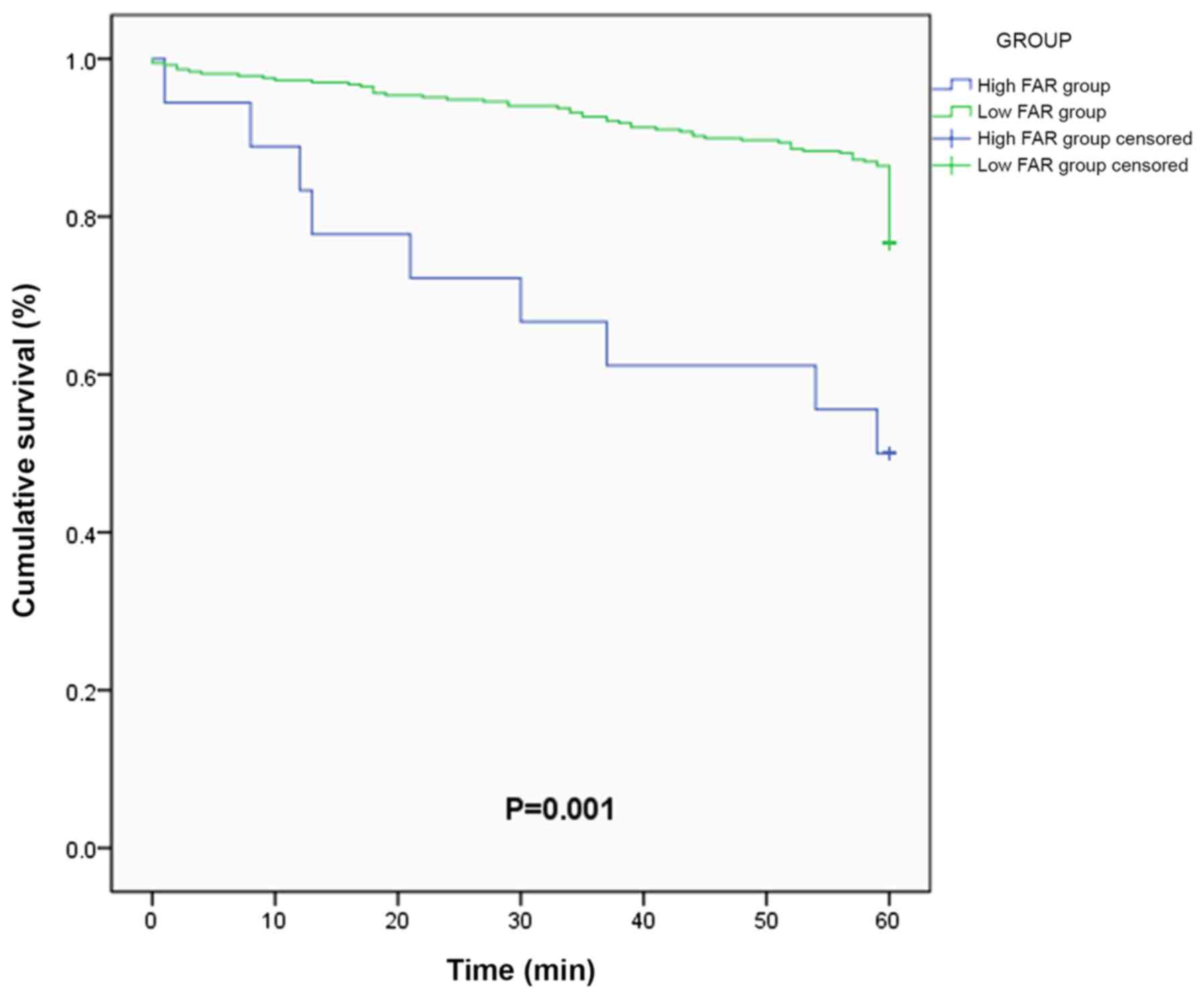
Primary endpoint
Using the cut-off value of 128.4, the patients were
divided into the high FAR group (n=42) and the low FAR group
(n=382), and the long-term survival was compared using Kaplan-Meier
curves. The results indicated that the two groups had significantly
different survival curves. Compared with the low FAR group, the
high FAR group had an unfavorable survival curve and a
significantly lower survival rate (P<0.001; Fig. 4). Univariate Cox regression found
that FAR was associated with worse prognosis (HR, 1.031; 95% CI,
1.023-1.040; P<0.001). Multivariate Cox regression analysis
demonstrated that the FAR was an independent risk factor for the
all-cause death (HR, 1.029; 95% CI, 1.020-1.037; P<0.001;
Table III), adjusted by age,
heart failure, hs-CRP, and hypertension.
 | Table IIIMultivariate Cox regression analysis
of factors influencing the primary endpoint. |
Table III
Multivariate Cox regression analysis
of factors influencing the primary endpoint.
| Risk factor | B | SE | Wald | P-value | HR | 95% CI |
|---|
| Agea | 0.043 | 0.013 | 10.669 | 0.001 | 1.044 | 1.017-1.071 |
| Heart
failureb | 0.708 | 0.326 | 4.723 | 0.030 | 2.030 | 1.072-3.843 |
| hs-CRPa | 0.030 | 0.017 | 3.090 | 0.079 | 1.031 | 0.997-1.066 |
|
Hypertensionb | 0.907 | 0.339 | 7.146 | 0.008 | 2.477 | 1.274-4.816 |
| FARa | 0.029 | 0.004 | 45.612 | <0.001 | 1.029 | 1.020-1.037 |
Secondary endpoints
The secondary endpoints were also compared between
the high FAR and the low FAR groups, which were MACE including the
recurrent MI, stroke, unscheduled revascularization and
rehospitalization due to heart failure (Fig. 5). The high FAR group had a
significantly higher incidence of secondary endpoints (P=0.001).
The multivariate Cox regression analysis demonstrated that the FAR
was an independent risk factor for total MACE (HR, 1.48; 95% CI,
2.62-4.63; P=0.001), even adjusted by age, heart failure,
hypertension and hs-CRP in multivariate analysis (Table IV). Subgroup analysis for
individual MACE indicated that only MI was significantly associated
with the FAR (HR, 1.62; 95% CI, 3.49-7.52; P<0.001), while the
other three endpoints were not (all P>0.05).
 | Table IVCox regression analysis of secondary
endpoints for the high FAR group vs. low FAR group. |
Table IV
Cox regression analysis of secondary
endpoints for the high FAR group vs. low FAR group.
| | Unadjusted |
Adjusteda |
|---|
| Factor | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Secondary
endpoint | | | | |
|
Myocardial
infarction | 1.79
(3.75-7.87) | <0.001 | 1.62
(3.49-7.52) | 0.001 |
|
Stroke | 0.21
(1.67-13.18) | 0.628 | 0.23
(1.95-16.34) | 0.537 |
|
Emergent
revascularization | 0.71
(2.03-5.82) | 0.186 | 0.81
(2.4-7.15) | 0.115 |
|
Readmission
due to heart failure | 0.15
(1.14-8.77) | 0.901 | 0.13
(1.05-8.41) | 0.961 |
| Total secondary
end-points | 1.48
(2.56-4.45) | 0.001 | 1.48
(2.62-4.63) | 0.001 |
Discussion
Abundant pieces of evidence have linked the FAR with
the severity and prognosis of CAD and demonstrated its value in
risk stratification and prediction of the prognosis of STEMI
(10,16-18).
The present study not only investigated the association between the
FAR and the SYNTAX score but explored the importance of the FAR in
predicting the long-term outcomes for the patients with STEMI and
multivessel disease. It was revealed that the FAR exhibited a
linear correlation with the SYNTAX score, indicating its potential
in assessing the severity. The observational cohort study proved
that the FAR had potential value in predicting long-term outcomes.
Of note, Cox regression analysis indicated no significant
association between the FAR and stroke, unscheduled
revascularization or rehospitalization for heart failure.
For patients with STEMI and multivessel disease, the
prognosis remains unsatisfying. It was reported that patients with
STEMI and multivessel CAD had poorer long-term mortality and a
higher incidence of MACE (19).
Different treatment strategies have been developed with
controversies regarding their usefulness continuing. Previous
observational and small randomized controlled trials have
demonstrated conflicting results regarding the optimal treatment
strategy (20). Specifically,
complete vs. culprit-only revascularization has been compared. A
review summarized current evidence on the different treatment
options and concluded that the optimal revascularization strategy
remains uncertain, while interventional cardiologists should
determine the optimal reperfusion strategy based on concrete
factors, including clinical characteristics, disease severity and
complexity of lesions (1). A
simple, cost-effective and sufficient risk assessment approach is
required to predict the prognosis and direct the clinical
strategy.
The SYNTAX scoring system is ubiquitously applied
worldwide to assess the severity of CAD. Certain studies have also
explored its value in prognosis prediction. Braga et al
(4) reported on a retrospective
cohort study on 535 patients with STEMI undergoing primary-PCI, who
were divided into three groups according to their residual SYNTAX
score (rSS): Complete revascularization (rSS=0; n=198), reasonable
incomplete revascularization (0<rSS<8; n=238) and incomplete
revascularization (rSS≥8; n=99). The study suggested that rSS was
positively correlated with in-hospital mortality and MACE (4). In the present study, the association
between the SYNTAX score and FAR was analyzed, indicating a linear
correlation between them. Compared with the SYNTAX score, the FAR
has the advantages of simplicity, efficiency and sufficiency. A
higher fibrinogen and lower albumin concentration are associated
with worse outcomes for patients with CAD (21,22).
As the combination of fibrinogen and albumin as a ratio, the FAR is
more sensitive and accurate as a stratification marker for CAD.
Cetin et al (16)
investigated the predictive value of the FAR in ACS, which
demonstrated that FAR may be used for the prediction of MACE in
patients with ACS who have undergone PCI. Another study indicated
that the baseline FAR was independently and significantly
associated with angiographic no-reflow and short-term mortality in
patients with ACS (18). Different
from previous studies, the present study focused on long-term
outcomes of patients with STEMI and multivessel disease using a
prospective cohort design. The present and previous studies have
indicated that the FAR is a biomarker reflecting the systemic
inflammation level and associated with the severity of CAD.
However, it should be emphasized that the FAR is a valuable
biomarker in the prognosis prediction of multiple tumors, including
esophageal squamous cell carcinoma, non-small cell lung cancer,
colorectal cancer and gallbladder cancer. As a result, there is a
possibility that the association between the FAR and the prognosis
of patients with STEMI may be falsely positive, which requires
further validation.
Several limitations of the present study must be
noted. First, only one PCI strategy was selected in the present
study, which limited the sample size and brought about certain
bias. Furthermore, the long-term prognosis was affected by the
compliance of patients, which was not recorded or considered in the
present study. Finally, a comparison between the FAR and other
markers, including hs-CRP, albumin and fibrinogen alone, may be
helpful.
In conclusion, the FAR was correlated with long-term
mortality and the incidence of MACE in patients with STEMI and
multivessel disease, which may indicate the potential of the FAR to
serve as a biomarker.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GL and GXC designed and led the current study. MLL,
HG, WNF and CMF collected and analyzed the patient data. GL and HG
wrote the manuscript and WNF revised it. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Medical Ethics
Committee of Xianyang Central Hospital (Xianyang, China). The
patients provided written informed consent regarding the use of
their data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Vogel B, Mehta SR and Mehran R:
Reperfusion strategies in acute myocardial infarction and
multivessel disease. Nat Rev Cardiol. 14:665–678. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
de Waha S, Eitel I, Desch S, Fuernau G,
Pöss J, Schuler G and Thiele H: Impact of multivessel coronary
artery disease on reperfusion success in patients with ST-elevation
myocardial infarction: A substudy of the AIDA STEMI trial. Eur
Heart J Acute Cardiovas Care. 6:592–600. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bates ER, Tamis-Holland JE, Bittl JA,
O'Gara PT and Levine GN: PCI strategies in patients with ST-segment
elevation myocardial infarction and multivessel coronary artery
disease. J Am Coll Cardiol. 68:1066–1081. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Braga CG, Cid-Alvarez AB, Dieguez AR,
Alarez BA, Otero DL, Sánchez RO, Pena XS, Salvado VG, Trillo-Nouche
R and González-Juanatey JR: Prognostic impact of residual SYNTAX
score in patients with ST-elevation myocardial infarction and
multivessel disease: Analysis of an 8-year all-comers registry. Int
J Cardiol. 243:21–26. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wilhelmsen L, Svardsudd K, Korsan-Bengtsen
K, Larsson B, Welin L and Tibblin G: Fibrinogen as a risk factor
for stroke and myocardial infarction. N Engl J Med. 311:501–505.
1984.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Nelson JJ, Liao D, Sharrett AR, Folsom AR,
Chambless LE, Shahar E, Szklo M, Eckfeldt J and Heiss G: Serum
albumin level as a predictor of incident coronary heart disease:
The atherosclerosis risk in communities (ARIC) study. Am J
Epidemiol. 151:468–477. 2000.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kijima T, Arigami T, Uchikado Y, Uenosono
Y, Kita Y, Owaki T, Mori S, Kurahara H, Kijima Y and Okumura H:
Combined fibrinogen and neutrophil-lymphocyte ratio as a prognostic
marker of advanced esophageal squamous cell carcinoma. Cancer Med.
108:193–199. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Li SQ, Jiang YH, Lin J, Zhang J, Sun F,
Gao QF, Zhang L, Chen QG, Wang XZ and Ying HQ:
Albumin-to-fibrinogen ratio as a promising biomarker to predict
clinical outcome of non-small cell lung cancer individuals. Cancer
Med. 7:1221–1231. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sun F, Tan YA, Gao QF, Li SQ, Zhang J,
Chen QG, Jiang YH, Zhang L, Ying HQ and Wang XZ: Circulating
fibrinogen to pre-albumin ratio is a promising biomarker for
diagnosis of colorectal cancer. J Clin Lab Anal.
33(e22635)2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Xu WY, Zhang HH, Xiong JP, Yang XB, Bai Y,
Lin JZ, Long JY, Zheng YC, Zhao HT and Sang XT: Prognostic
significance of the fibrinogen-to-albumin ratio in gallbladder
cancer patients. World J Gastroenterol. 24:3281–3292.
2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Karahan O, Acet H, Ertas F, Tezcan O,
Çalişkan A, Demir M, Kaya AF, Demirtaş S, Çevik MU and Yavuz C: The
relationship between fibrinogen to albumin ratio and severity of
coronary artery disease in patients with STEMI. Am J Emerg Med.
34:1037–1042. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Task Force on the management of ST-segment
elevation acute myocardial infarction of the European Society of
Cardiology (ESC). Steg PG, James SK, Atar D, Badano LP,
Blömstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq
G, et al: ESC Guidelines for the management of acute myocardial
infarction in patients presenting with ST-segment elevation. Eur
Heart J. 33:2569–2619. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ibanez B, James S, Agewall S, Antunes MJ,
Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA,
Halvorsen S, et al: 2017 ESC Guidelines for the management of acute
myocardial infarction in patients presenting with ST-segment
elevation: The task force for the management of acute myocardial
infarction in patients presenting with ST-segment elevation of the
European Society of Cardiology (ESC). Eur Heart J. 39:119–177.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lee JM, Rhee TM, Kim HK, Hwang D, Lee SH,
Choi KH, Kim J, Park TK, Yang JH, Song YB, et al: Comparison of
long-term clinical outcome between multivessel percutaneous
coronary intervention versus infarct-related artery-only
revascularization for patients with St-segment-elevation myocardial
infarction with cardiogenic shock. J Am Heart Assoc.
8(e013870)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bohula EA, Morrow DA, Giugliano RP,
Blazing MA, He P, Park JG, Murphy SA, White JA, Kesaniemi YA,
Pedersen TR, et al: Atherothrombotic risk stratification and
ezetimibe for secondary prevention. J Am Coll Cardiol. 69:911–921.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cetin M, Erdoğan T, Kırış T, Özer S,
Yılmaz AS, Durak H, Aykan AÇ and Şatıroğlu Ö: Predictive value of
fibrinogen-to-albumin ratio in acute coronary syndrome. Herz: Aug
6, 2019 (Epub ahead of print).
|
|
17
|
Kayapinar O, Ozde C and Kaya A:
Relationship between the reciprocal change in inflammation-related
biomarkers (fibrinogen-to-albumin and hsCRP-to-albumin ratios) and
the presence and severity of coronary slow flow. Clin Appl Thromb
Hemost. 25(1076029619835383)2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Zhao Y, Yang J, Ji Y, Wang S, Wang T, Wang
F and Tang J: Usefulness of fibrinogen-to-albumin ratio to predict
no-reflow and short-term prognosis in patients with ST-segment
elevation myocardial infarction undergoing primary percutaneous
coronary intervention. Heart Vessels. 34:1600–1607. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tarantini G, D'Amico G, Brener SJ,
Tellaroli P, Basile M, Schiavo A, Mojoli M, Fraccaro C, Marchese A,
Musumeci G and Stone GW: Survival after varying revascularization
strategies in patients with ST-segment elevation myocardial
infarction and multivessel coronary artery disease: A pairwise and
network meta-analysis. JACC Cardiovas Interv. 9:1765–1776.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Di Pasquale G, Filippini E, Pavesi PC,
Tortorici G, Casella G and Sangiorgio P: Complete versus
culprit-only revascularization in ST-elevation myocardial
infarction and multivessel disease. Int Emerg Med. 11:499–506.
2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
O'Donoghue ML, Morrow DA, Cannon CP,
Jarolim P, Desai NR, Sherwood MW, Murphy SA, Gerszten RE and
Sabatine MS: Multimarker risk stratification in patients with acute
myocardial infarction. J Am Heart Assoc. 5(pii:
e002586)2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Sanchez PL, Morinigo JL, Pabon P, Martin
F, Piedra I, Palacios IF and Martin-Luengo C: Prognostic relations
between inflammatory markers and mortality in diabetic patients
with non-ST elevation acute coronary syndrome. Heart. 90:264–269.
2004.PubMed/NCBI View Article : Google Scholar
|