Introduction
Bicondylar tibial plateau fractures are common
injuries of the lower limb, leading to the destabilization of both
the medial and lateral condyles (1-3).
This type of fracture accounts for up to 39% of all tibial plateau
fractures (4). The bicondylar
fracture occurs as a result of significant trauma involving a
high-energy mechanism in which the varus or valgus is combined with
axial loading (3).
The C1.1 (AO-41) fracture, from the AO/OTA
classification, is a complex variation of bicondylar fractures
where the fracture line is described as having an inverted ‘Y’
trajectory (5). In the case of a
bicondylar fracture, the reduction and fixation techniques usually
involve an open reduction and an internal fixation using a plate
and screws that can be applied laterally, medially, or combined
(4). Dual plating is considered the
most stable type of fixation for bicondylar tibial plateau
fractures. However, the surgical approach for dual plating is
complex, involving two incisions and soft-tissue manipulation.
Moreover, for this type of fracture, soft-tissue complications are
an important concern associated with dual plating (4). Plates with polyaxial stability (PAS)
offer the possibility to adapt the position of the screws to the
fracture trajectory. Due to this, appropriate fixation and
stabilization can be achieved through a single plate with lateral
fixation (6).
However, each case of bicondylar fracture must be
analyzed in the context of specific clinical features, considering
the trajectory of the fracture and the affected soft tissues. This
is necessary because no single method can guarantee optimal results
for the full range of possible clinical cases (4). The selection of an inappropriate
treatment for the bicondylar fracture can lead to a reduction in
the range of motion of the joint and joint instability. There are,
of course, several other issues that contribute to poor results in
the treatment of bicondylar plateau fractures. The advanced age of
>50 years of a patient has been associated with poor
postoperative results (7-9).
Smoking, the existence of an open fracture, and compartment
syndrome can increase the risk of infection (10,11).
In assessing the outcome of a fracture at the knee joint, the
Rasmussen and Iowa scores are the only tools specifically designed
for this (12,13). However, these tools have not been
validated with a rigorous methodology to assess the results of
patients with bicondylar tibial plateau fractures (4).
The finite element analysis (FEA) method is
particularly advantageous as it allows for the virtual
reconstruction of the anatomical and physiological conditions of
this type of fracture. Bone shape and fracture trajectory, as well
as biomechanical conditions, such as the force generated by muscle
deformation, which in turn is transmitted through tendons to the
bone, can be simulated (14).
It is quite difficult to make an experimental
device, in vitro, that respects the anatomical and
physiological conditions as can be done in FEA. This method has
been widely used in trauma research in orthopedics, to determine
whether there are stress concentrators in the implants or
osteosynthesis used, that would lead to their deformation or
rupture, but also to analyze the effect of these devices on the
bone tissue (14-16).
For the C1.1 type bicondylar fracture (AO-41), the scientific
literature presents a lack of FEA studies to distinguish between
different simulated scenarios and to analyze the results
obtained.
The aim of the present study was to analyze three
methods of reduction, single medial, single lateral and dual
plating, for the treatment of the bicondylar tibial plateau
fracture, C1.1 (AO-41), using FEA to determine the stress and
strains at the level of the reduced and stabilized fracture.
Materials and methods
Knee model
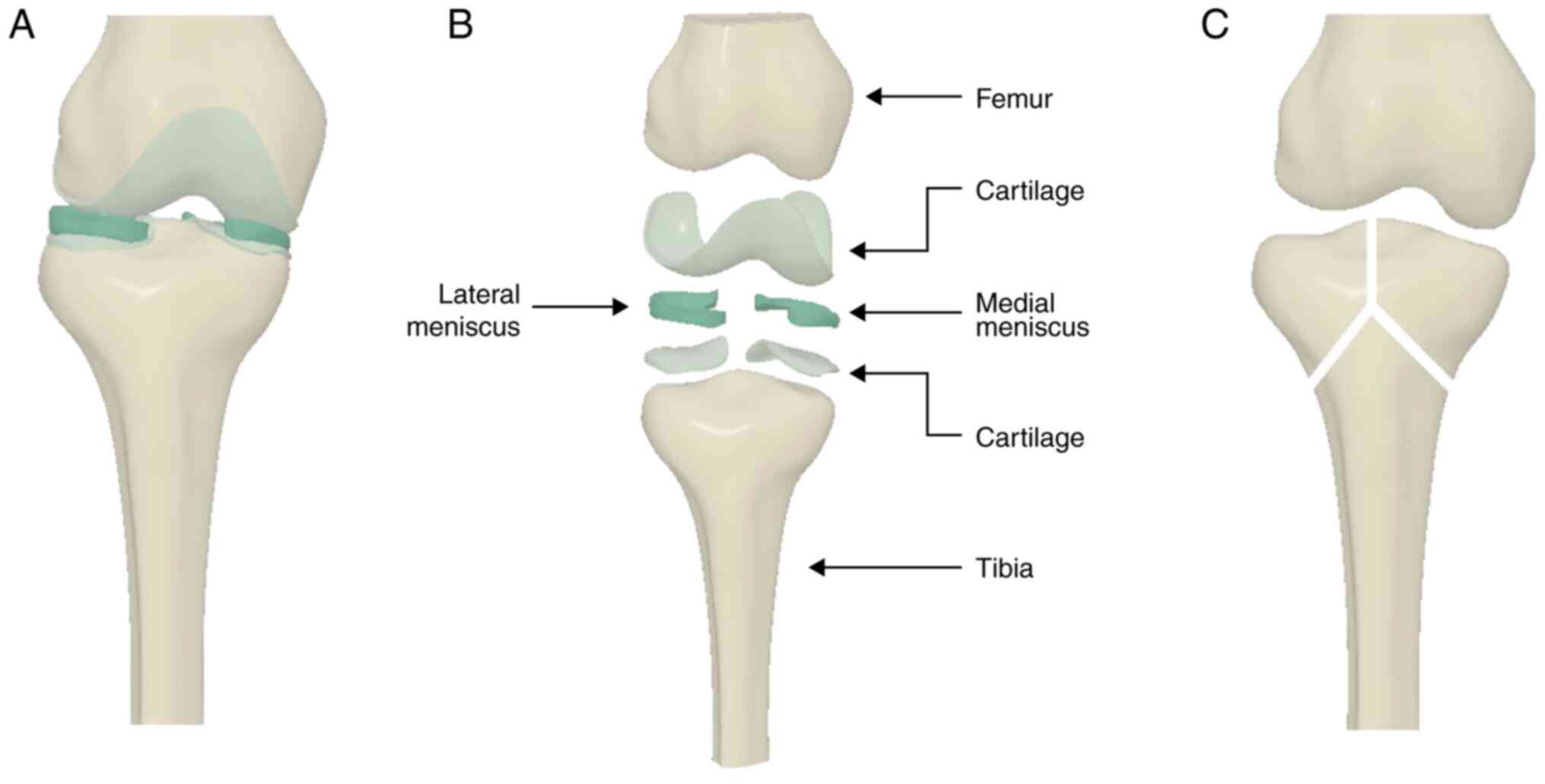
For this study, a 3D model of the knee was obtained
using CT images in Slicer3D (http://www.slicer.org) and 3D modeling with further
processing was carried out using Autodesk ReCap Photo version 2019
and Autodesk Fusion360 (Autodesk, Inc.). Following the bone
reconstruction, the menisci and cartilage tissue were modeled in
Autodesk Fusion360 (Autodesk, Inc.) (Fig. 1).
Method selection and load
simulation
A simple metaphyseal fracture, type C1.1 (AO-41),
according to the AO/OTA classification, was modeled, with an
inverted ‘Y’ trajectory. For this type of fracture, three methods
of fracture reduction were selected, single medial, single lateral
and dual plating. Proximal polyaxial tibial plates and screws of 3
mm diameter, with no threads were modeled and placed accordingly
for the three methods of reduction. To ensure contact areas between
the plate and tibia, very small volumes of material were cut from
the plates, following the contour of the contact surfaces. These
volumes were very small and negligible in terms of plate thickness,
having only the role of providing small contact areas. The
positioning of the plates and screws on the fractured 3D model is
presented in Fig. 2.
Load simulation was performed in the Simulation
Mechanical 2017 software (Autodesk, Inc.). Materials assigned to
all parts were considered materials with linear isotropic and
elastic mechanical properties and were characterized by Young's
modulus and the Poisson's ratio, the values of which are presented
in Table I (17-19).
 | Table IMaterial properties. |
Table I
Material properties.
| Material
(Refs.) | Young's Modulus
(MPa) | Poisson's
ratio |
|---|
| Cortical bone
(17) | 17,000 | 0.33 |
| Trabecular bone
(17) | 5,000 | 0.33 |
| Cartilage (18) | 5 | 0.46 |
| Menisci (18) | 59 | 0.49 |
| Titanium (19) | 110,000 | 0.3 |
Determining the magnitude of the
forces
To obtain the appropriate magnitude of the forces
applied, the peak value in the maximal weight acceptance phase that
occurs during a slow walking gait cycle was considered. In a
complete gait cycle, the reaction force has two peaks occurring at
weight acceptance and push-off, as well as a minimum value in
mid-stance. The first peak was considered for the calculation of
the applied forces. The approximation of the position, as a
percentage of the gait cycle, of this first peak was produced based
on the data reported by Arnold and his collaborators (20). Thus, the first peak of the ground
reaction force occurs at 16% of the gait cycle at a walking speed
of 1 m/sec.
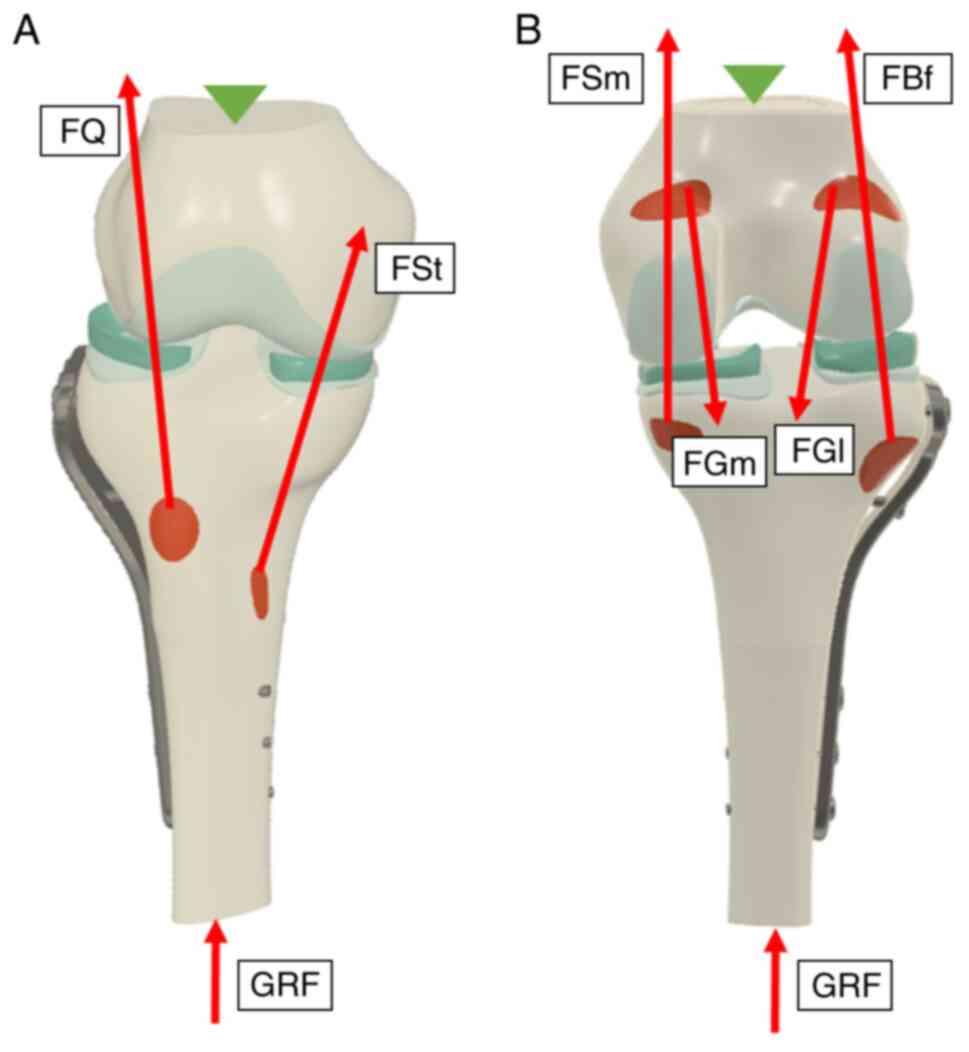
The forces were calculated for an individual with a
body mass of 70 kg. The applied loads were represented by the
forces of the quadriceps muscle (FQ), semitendinosus
(FSt) and semimembranosus (FSm), medial and
lateral gastrocnemius (FGm, FGl), biceps
femoris (FBf), as well as the ground reaction force
(GRF), as revealed in Fig. 3.
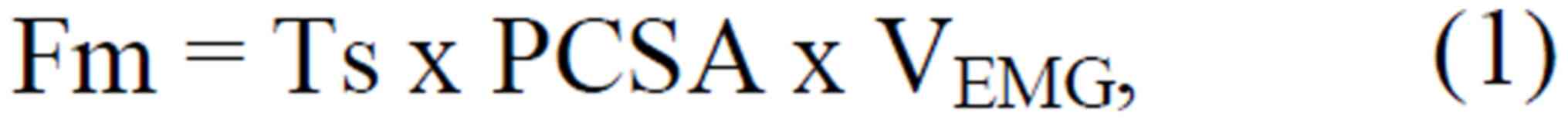
The magnitude of these forces was calculated using
the formula:
where Fm is muscle force, Ts is specific tension,
PCSA is physiological cross-sectional area, and VEMG is
normalized value of muscle activity during maximal weight
acceptance.
For the specific tension of the muscle, an average
value of 22.5 N/cm2 was used, and the physiological
cross-sectional area, specific to each muscle, was selected from
available data from the literature (21,22).
The normalized value of the muscle activity, during maximal weight
acceptance, was approximated from the data reported by Arnold and
his collaborators (20).
The directions of the muscle forces were established
according to data from the literature (22-26).
In the frontal plane, an angle of 3˚ between the mechanical and the
vertical axis was considered. In the simulation interface, the
directions of the forces were set to the vertical axis. In the
frontal plane, FQ was oriented in the direction of the Q
angle (14˚), calculated to the vertical axis, FBf 11.8˚
medial, FSm 7˚ lateral, FSt 5.1˚ lateral,
FGl 4.8˚ lateral, and FGm 5.3˚ medial to the
mechanical axis of the tibia (23-27).
For the sagittal plane, the knee was considered to
be in extension, and the anatomical axis of the tibia, which
corresponded to the mechanical axis, was vertical. In the sagittal
plane, FQ, FGl, and FGm were
considered parallel to the tibial axis and FBf 7.3˚
anterior to the tibial axis, FSm oriented at 16.1˚ and
FSt at 19.6˚ posterior to the tibial axis (24-26).
Regarding the direction of the GRF, the step size
was extremely small postoperatively. Thus, GRF acted normally on
the tibial surface, the angle between the tibia and the reaction
force being negligible. The magnitude of the GRF was approximated
based on data reported by Arnold and his collaborators, at maximum
weight acceptance (20). Table II reveals the rounded values of the
muscular forces as well as the GRF. The fibula bone was not
included in this study. However, the contact area between the
fibula and the tibia was considered as the area of application of
the force developed by the biceps femoris muscle, which has its
insertion in the fibula. Constraints were applied to the diaphyseal
surface of the femur, completely restricting the movement of this
surface. The type of contact selected between the simulation
elements was bonded. A descriptive image of the forces and
constraints applied to the 3D model is shown in Fig. 3.
 | Table IIRounded values of applied forces
(N). |
Table II
Rounded values of applied forces
(N).
| FQ | FSm | FSt | FBf | FGl | FGm | GRF |
|---|
| 213 | 50 | 13 | 42 | 24 | 62 | 720 |
Results
Analysis of maximum principal stress
and strain values
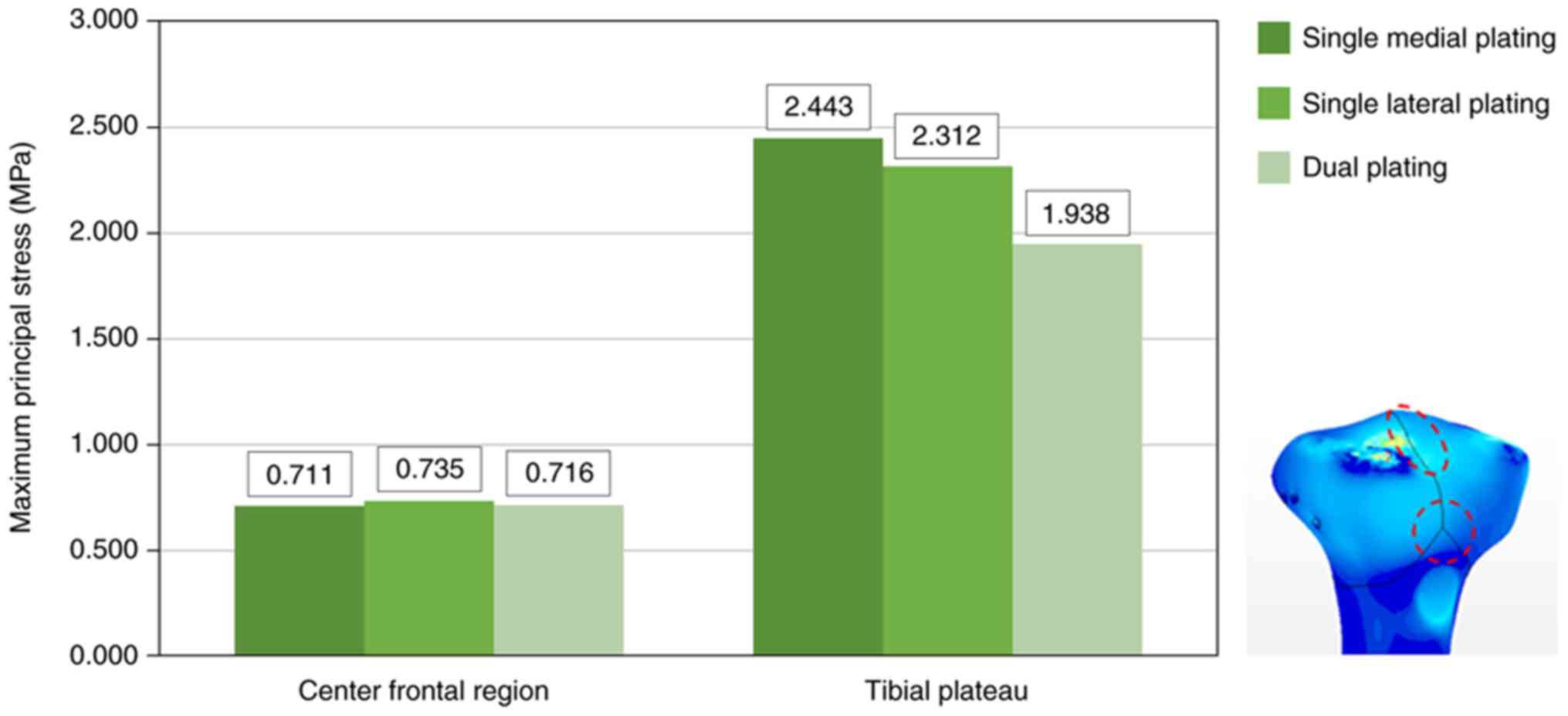
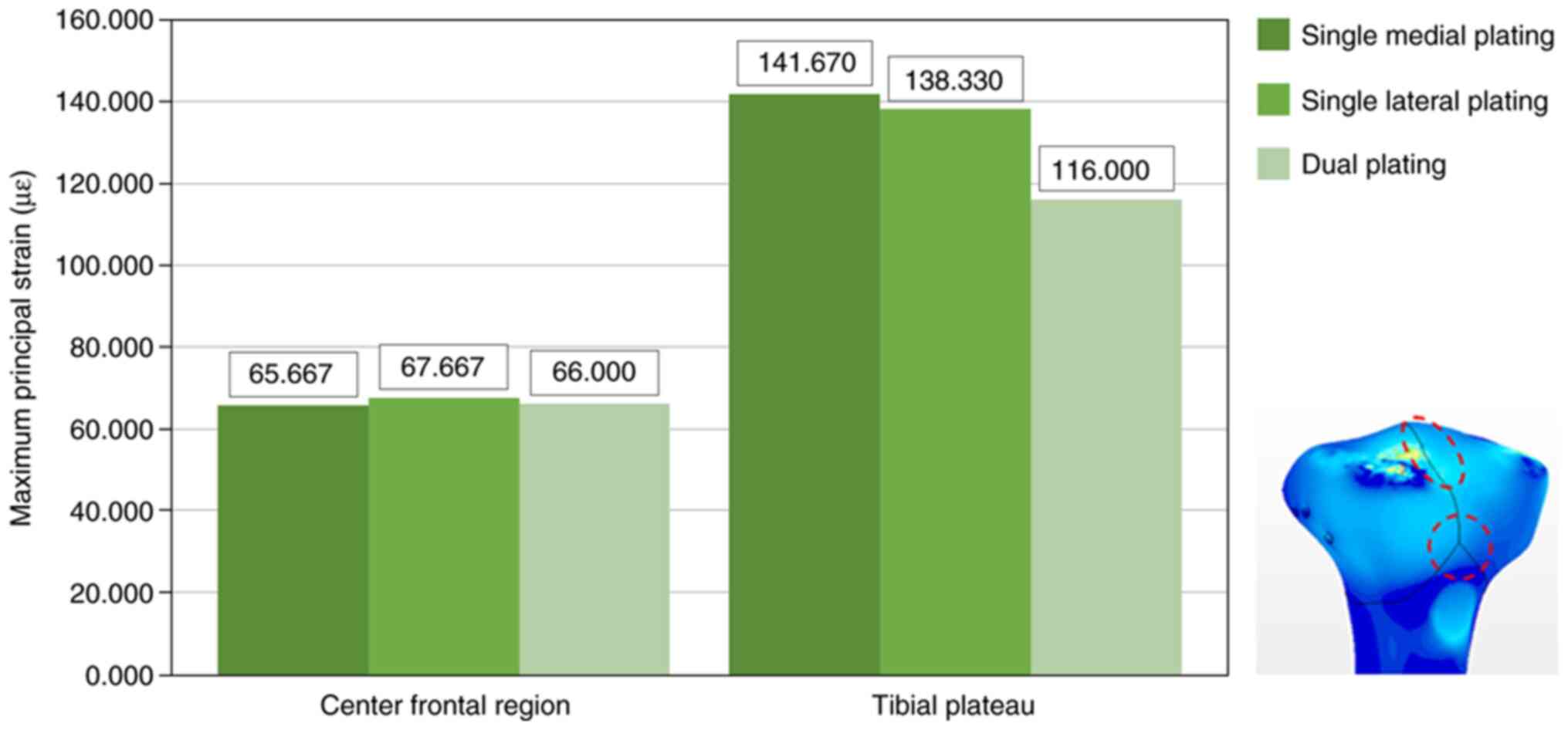
In this study, the values of maximum principal
stress and strain were analyzed (Figs.
4 and 5). Values were recorded
at the cortical level near the fracture lines, in two areas, the
central frontal area (where the fracture lines split) and the
tibial plateau area. To eliminate artifacts represented by high
local values, an average of 3 values recorded in the vicinity of
the area of interest was made. The highest stress and strain values
were recorded near the fracture lines, in the tibial plateau area.
Dual plating led to a decrease of stress and strain values in this
region. In the center frontal area, values were similar between the
three methods of reduction analyzed.
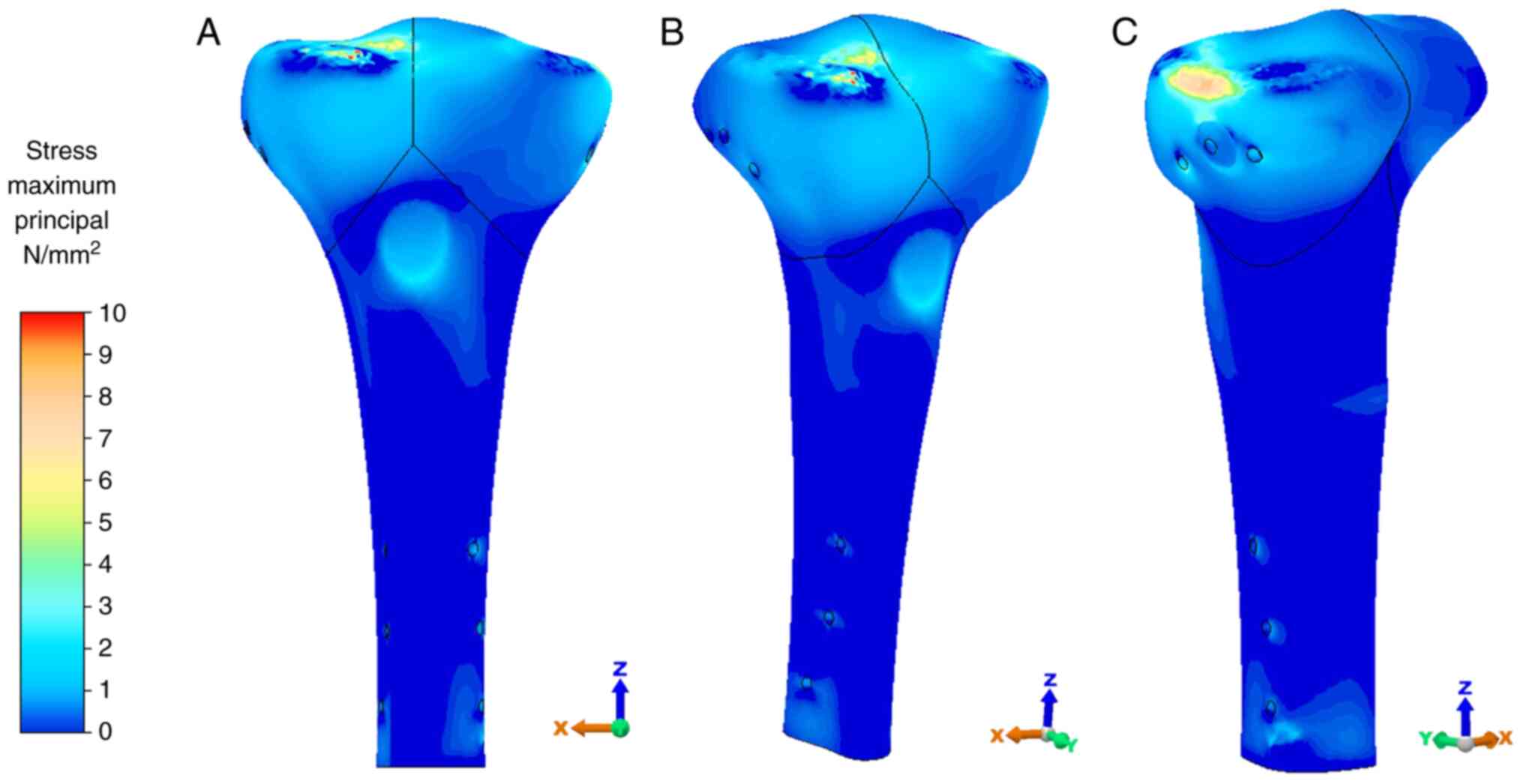
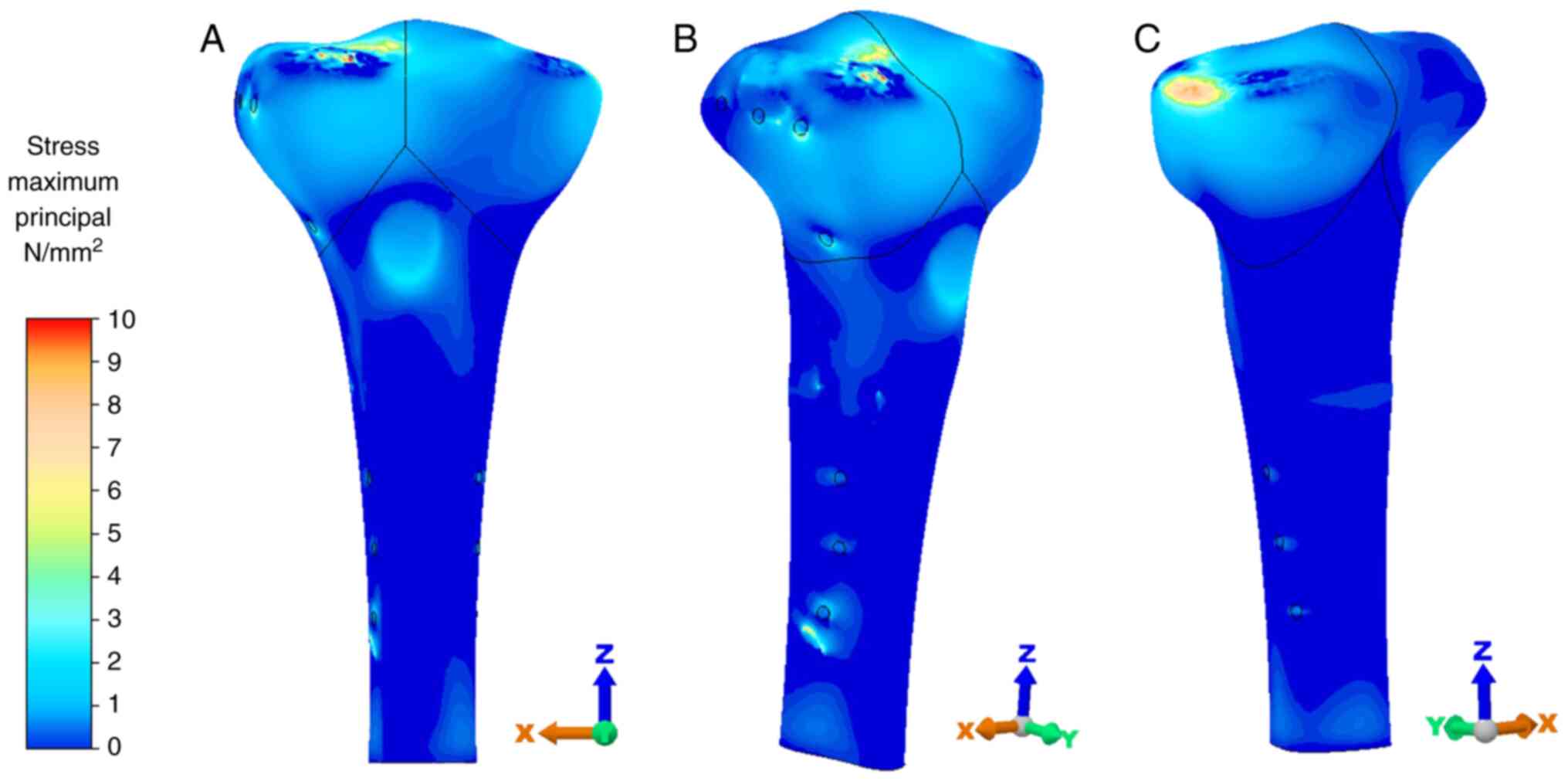
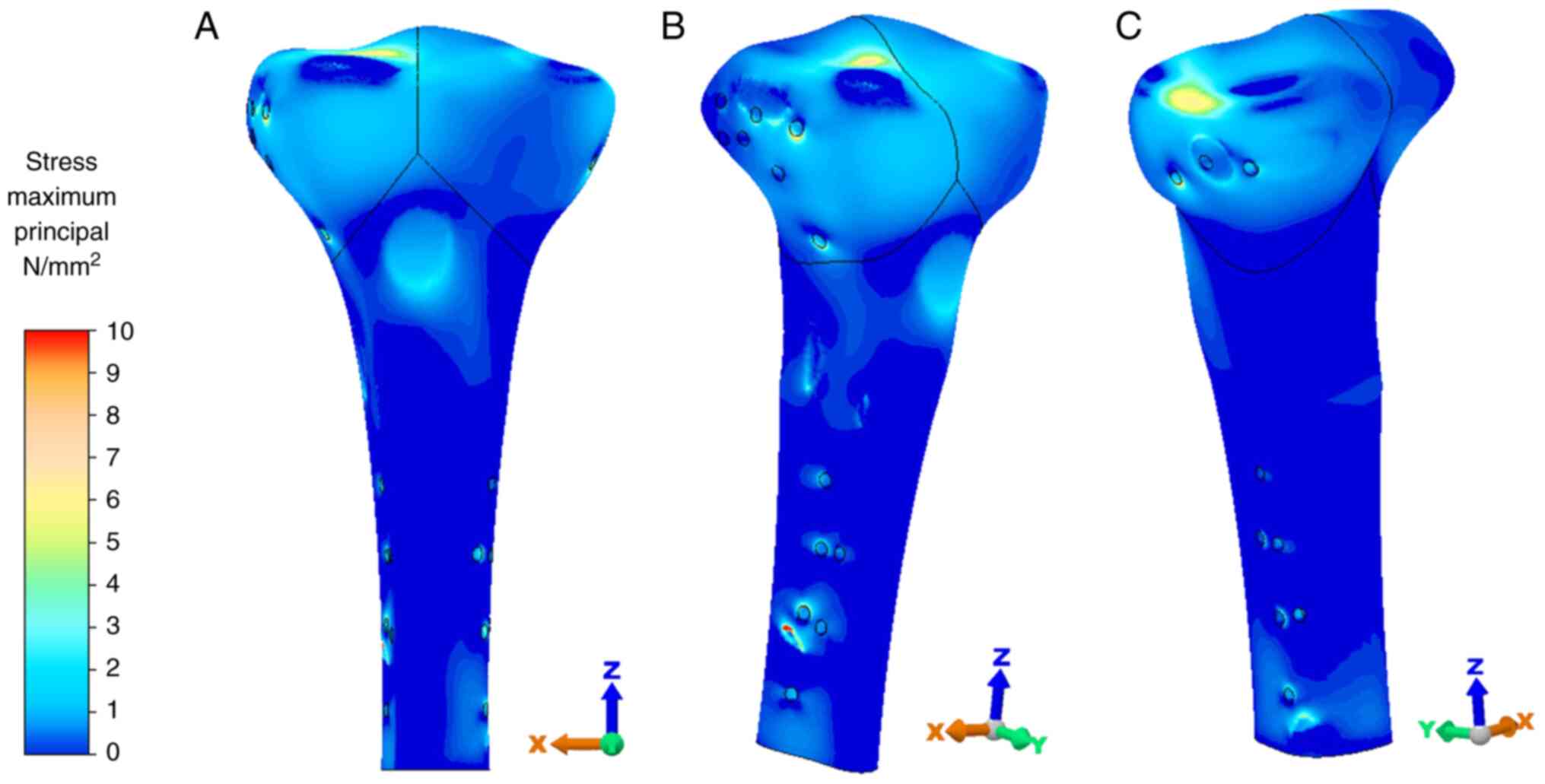
Stress distribution
The distribution of the stress values at the level
of the tibia was also analyzed. For an optimal view of the stress
distribution, the color legend was changed to highlight the areas
of stress concentration. Thus, the upper-stress limit for this
stress distribution was selected as 10 MPa. This value does not
represent the maximum stress obtained but is only a value selected
for a stronger exposure of the high-stress concentration areas. The
stress concentration areas were located in the region of the
fracture, predominantly in the area of the tibial plateau, as is
evident in Fig. 6, Fig. 7 and Fig.
8. Small areas of stress concentration were evident in regions
where the forces were applied and the plates came in direct contact
with the bone. These areas appear in all three cases due to the
same loading applied.
Discussion
The aim of the present study was to analyze the
complex reduction and fixation of the tibial plateau C1.1 (AO-41)
type fracture, considering three methods of reduction, single
medial, single lateral and dual, by using proximal polyaxial plates
and screws. The results revealed that both stress and strain
increased in the region of the tibial plateau. The stresses and
strains increased due to the forces applied but also the fixture of
the plates. The bone discontinuity caused by the fracture path
caused a large amount of stress on the plate when loading was
applied, which was then transmitted to the bone tissue near the
screws and further along to the fracture lines.
Strain values can be analyzed in relation to the
physiological intervals defined by Frost through the mechanostat
theory (28). The theory defines
the mechanism of adaptation of the bone tissue to the action of a
mechanical stimulus that is maintained in a specific area by the
variation of bone mass (29,30).
In other words, the action of a mechanical stimulus leads to a
remodeling of the bone tissue, for the bone to respond favorably to
the applied loads. The response of bone tissue can be quantified by
analyzing the values of the strain generated (28,31).
There are four intervals of bone strain, <1,000 µɛ (absence of
an applied load, potential for tissue atrophy), 1,000-1,500 µɛ
(tissue homeostasis), 1,500-3,000 µɛ (physiological load that
promotes bone remodeling), and >3,000 µɛ (overload associated
with fractures and bone resorption) (28,31).
The values of strain obtained in both areas were
found in the minimum strain range. Although it is considered that
in the present study the strain was not enough to achieve bone
remodeling, it is noteworthy that the simulation was performed
taking into account forces applied during a smaller walking speed.
However, the average speed for normal walking is reported at
approximately 1.33 m/sec, while slow walking speed is approximately
0.66 m/sec (32). By decreasing the
walking speed, the muscle forces also decrease, resulting in lower
values of stress and strain. At lower speeds, acceleration is also
smaller. The same acceleration can be transposed to the system of
forces in the human body, i.e., the lower the acceleration, the
lower the forces exerted by the muscles, and thus, the stress
transmitted to the bone tissue becomes smaller. In addition, the
variation of the GRF in a complete walking cycle may change and in
the context of a fracture, the variation can also extend to the
walking phases. As the speed of movement or the angle of the GRF
changes by increasing the step size, the load on the tibia may
increase accordingly.
The variation obtained shows that dual plating leads
to smaller stress and strain values near the fracture lines in the
tibial plateau area. Dual plating is considered to be the most
stable type of fixation for bicondylar tibial plateau fractures;
however, the surgical approach involved is complex and soft-tissue
complications are an important concern associated with dual plating
(4). In the present study, values
obtained for single lateral plating were close in range.
Considering the complexity of the surgical approach for dual
plating, single lateral plating may be a solution for good
reduction with fewer surgical risks and complications.
Moreover, plates with PAS provide the means to adapt
the position of the screws to the fracture trajectory. Thus,
appropriate fixation and stabilization can be achieved through a
single plate with lateral fixation (6).
We observed that the stress concentration areas are
located in the fracture area, more specifically in the tibial
plateau region, in the vicinity of the fracture line. The location
of the stress concentration areas may derive from the loading
generated by the muscular forces and also the type of contact
between the surfaces. The type of contact between the elements is a
limitation of FEA studies as it is difficult to characterize the
contact between the fracture fragments, postoperatively.
For this type of fracture, there is a lack of FEA
studies to help distinguish between different simulated scenarios
and to analyze the results obtained. As aforementioned, the
existing studies describe only from a clinical point of view, the
impact of different methods of reduction and osteosynthesis of
simple metaphyseal fracture of the tibial plateau.
The FEA study by Samsami et al addresses the
bicondylar tibial plateau fracture; however, the fracture
trajectory is extremely different from that of the present study
(33). Additionally, the loading
mode differs, forces of 350 N and 250 N were applied to the tibial
plateau region in that study (33).
Being a type of fracture characterized by increased
heterogeneity from patient to patient, it also has a high risk of
complications of treatment (34).
Among the reported complications, there are associated lesions of
the menisci and cruciate ligaments, vascular or nerve lesions,
vicious consolidation, knee stiffness, and osteoarthritis (4). The heterogeneity of the fracture is
also highlighted by the variety of technical solutions for
reduction and stabilization. Normal means are open reduction and
internal fixation in the bicondylar fractures of the tibial plateau
(4,35).
In the context of a lack of FEA studies addressing
the C1.1 fracture type (AO-41) and the limitations of the FEA
method, the results obtained in the present study need to be
analyzed together with several aspects. The materials assigned to
the 3D models were considered elastic linear. The values of the
muscle PCSA used to calculate the force were obtained from
cadaveric specimens and may be smaller than in vivo measured
values in patients (22).
Furthermore, the normalized EMG activity values were taken from a
gait cycle of 1 m/sec speed. Although smaller than the average
walking speed, slow walking speed is approximately 0.66 m/sec
(32). A smaller walking speed may
lead to smaller applied forces and thus to decreased stress and
strain. Nevertheless, studies are required to determine the
variation of muscle forces in a slow walking cycle, in the context
of a reduced and stabilized bicondylar tibial plateau fracture.
Concurrently, it is necessary to determine the variation of the GRF
that occurs during a postoperative slow walking cycle, to obtain
appropriate reference values. It is imperative that such studies be
conducted on postoperative patients for the accuracy of data.
Considering the limitations of this study, the
results of the present study have shown that dual plating leads to
smaller stress and strain values near the fracture lines in the
tibial plateau area. However, values obtained for single lateral
plating were close in range. Considering the complexity of the
surgical approach for dual plating, single lateral plating may be a
solution for good reduction with fewer surgical risks and
complications. Plates with polyaxial stability allow for adaptation
of the position of the screws to the fracture trajectory. This
provides the means for appropriate fixation and stabilization
through a single plate with lateral fixation.
The values of strain obtained in both areas are
found in the minimum strain range. Although in the present study,
it is considered that the bone is not loaded enough to achieve bone
remodeling or homeostasis, it is notable that the stresses
transmitted by the plates and screws should not cause associated
trauma but should only stabilize and reduce the fracture to promote
healing.
The present study can be further developed to
explore forces that occur in other moments of a slow walking cycle
to describe the complete loading of the fractured tibia. However,
studies are required to determine the variation of muscle forces
that occur in a slow walking cycle, in the context of a reduced and
stabilized bicondylar fracture at the tibial plateau.
Further studies on the C1.1 fracture (AO-41) are
required to analyze the complex issue of reducing and stabilizing
such a fracture and to characterize the postoperative state while
providing predictable parameters for an optimal result.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data analyzed during this study are included in
this published article.
Authors' contributions
NF, FM and SABM conceived the study. NF, FM, SABM
and PDS developed and designed the methodology. NF, FM, SABM, PDS,
LS and BP performed formal data analysis. NF, FM, SABM, LS and BP
performed curation and interpretation of data. All authors provided
resources. All authors worked on the original draft and editing of
the manuscript. NF, FM and SABM confirm the authenticity of all the
raw data. All authors have read and agreed to the published version
of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Urruela AM, Davidovitch R, Karia R,
Khurana S and Egol KA: Results following operative treatment of
tibial plateau fractures. J Knee Surg. 26:161–165. 2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Rademakers MV, Kerkhoffs GM, Sierevelt IN,
Raaymakers EL and Marti RK: Operative treatment of 109 tibial
plateau fractures: Five- to 27-year follow-up results. J Orthop
Trauma. 21:5–10. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Markhardt BK, Gross JM and Monu JUV:
Schatzker classification of tibial plateau fractures: Use of CT and
MR imaging improves assessment. Radiographics. 29:585–597.
2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lee AK, Cooper SA and Collinge C:
Bicondylar tibial plateau fractures: A critical analysis review.
JBJS Rev. 6(e4)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Meinberg EG, Agel J, Roberts CS, Karam MD
and Kellam JF: Fracture and dislocation classification
compendium-2018. J Orthop Trauma. 32 (Suppl 1):S1–S170.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sîrbu PD, Friedl W, Carata E, Petreus T,
Poroch V, Botez P and Stratulat S: Are the plates with polyaxial
stability (pas) the ideal treatment in complex periarticualar
fractures? Bul Inst Polit Iaşi Tomul LVII (LXI) Fasc. 4:212–19.
2011.
|
|
7
|
Barei DP, Nork SE, Mills WJ, Coles CP,
Henley MB and Benirschke SK: Functional outcomes of severe
bicondylar tibial plateau fractures treated with dual incisions and
medial and lateral plates. J Bone Joint Surg Am. 88:1713–1721.
2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ali AM, Burton M, Hashmi M and Saleh M:
Treatment of displaced bicondylar tibial plateau fractures
(OTA-41C2&3) in patients older than 60 years of age. J Orthop
Trauma. 17:346–352. 2003.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Schwartsman R, Brinker MR, Beaver R and
Cox DD: Patient self-assessment of tibial plateau fractures in 40
older adults. Am J Orthop (Belle Mead NJ). 27:512–519.
1998.PubMed/NCBI
|
|
10
|
Morris BJ, Unger RZ, Archer KR, Mathis SL,
Perdue AM and Obremskey WT: Risk factors of infection after ORIF of
bicondylar tibial plateau fractures. J Orthop Trauma. 27:e196–e200.
2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Colman M, Wright A, Gruen G, Siska P, Pape
HC and Tarkin I: Prolonged operative time increases infection rate
in tibial plateau fractures. Injury. 44:249–252. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Rasmussen PS: Tibial condylar fractures.
Impairment of knee joint stability as an indication for surgical
treatment. J Bone Joint Surg Am. 55:1331–1350. 1973.PubMed/NCBI
|
|
13
|
Merchant TC and Dietz FR: Long-term
follow-up after fractures of the tibial and fibular shafts. J Bone
Joint Surg Am. 71:599–606. 1989.PubMed/NCBI
|
|
14
|
van den Munckhof S and Zadpoor AA: How
accurately can we predict the fracture load of the proximal femur
using finite element models? Clin Biomech (Bristol, Avon).
29:373–380. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Vulovic A, Šušteršič T and Filipovic N:
Finite element analysis of femoral implant under static load. 2017
IEEE 17th International Conference on Bioinformatics and
Bioengineering (BIBE), pp.559-562, 2017. doi:
10.1109/BIBE.2017.00012.
|
|
16
|
Carrera I, Gelber PE, Chary G,
Gonzalez-Ballester MA, Monllau JC and Noailly J: Fixation of a
split fracture of the lateral tibial plateau with a locking screw
plate instead of cannulated screws would allow early weight
bearing: A computational exploration. Int Orthop. 40:2163–2169.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Luo CA, Hua SY, Lin SC, Chen CM and Tseng
CS: Stress and stability comparison between different systems for
high tibial osteotomies. BMC Musculoskelet Disord.
14(110)2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Peña E, Calvo B, Martínez MA, Palanca D
and Doblaré M: Finite element analysis of the effect of meniscal
tears and meniscectomies on human knee biomechanics. Clin Biomech
(Bristol, Avon). 20:498–507. 2005.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Diffo Kaze A, Maas S, Kedziora S, Belsey
J, Haupert A, Wolf C, Hoffmann A and Pape D: Numerical comparative
study of five currently used implants for high tibial osteotomy:
Realistic loading including muscle forces versus simplified
experimental loading. J Exp Orthop. 5(28)2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Arnold EM, Hamner SR, Seth A, Millard M
and Delp SL: How muscle fiber lengths and velocities affect muscle
force generation as humans walk and run at different speeds. J Exp
Biol. 216:2150–2160. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Enoka RM (ed): Neuromechanics of human
movement. Human Kinetics. 4th edition. Champaign, IL, p 370,
2008.
|
|
22
|
Ward SR, Eng CM, Smallwood LH and Lieber
RL: Are current measurements of lower extremity muscle architecture
accurate? Clin Orthop Relat Res. 467:1074–1082. 2009.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Adouni M and Shirazi-Adl A: Evaluation of
knee joint muscle forces and tissue stresses-strains during gait in
severe OA versus normal subjects. J Orthop Res. 32:69–78.
2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Mesfar W and Shirazi-Adl A: Biomechanics
of the knee joint in flexion under various quadriceps forces. Knee.
12:424–434. 2005.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mesfar W and Shirazi-Adl A: Knee joint
mechanics under quadriceps-hamstrings muscle forces are influenced
by tibial restraint. Clin Biomech (Bristol, Avon). 21:841–848.
2006.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Aalbersberg S, Kingma I, Ronsky JL, Frayne
R and van Dieen JH: Orientation of tendons in vivo with active and
passive knee muscles. J Biomech. 38:1780–1788. 2005.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Hillman SK: In: Essentials of Interactive
Functional Anatomy Cdr Edition. Primal Pictures (ed). London, UK,
2003.
|
|
28
|
Frost HM: Bone ‘mass’ and the
‘mechanostat’: A proposal. Anat Rec. 219:1–9. 1987.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Huiskes R, Weinans H, Grootenboer HJ,
Dalstra M, Fudala B and Slooff TJ: Adaptive bone-remodeling theory
applied to prosthetic-design analysis. J Biomech. 20:1135–1150.
1987.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Mullender MG and Huiskes R: Proposal for
the regulatory mechanism of Wolff's law. J Orthop Res. 13:503–512.
1995.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Frost HM: A 2003 update of bone physiology
and Wolf's law for clinicians. Angle Orthod. 74:3–15.
2004.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Perry J and Bumfield JM: Gait analysis:
Normal and pathological function. Slack, Thorofare NJ, pp432-454,
1992.
|
|
33
|
Samsami S, Herrmann S, Pätzold R, Winkler
M and Augat P: Finite element analysis of Bi-condylar Tibial
Plateau fractures to assess the effect of coronal splits. Med Eng
Phys. 84:84–95. 2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kumar G, Peterson N and Narayan B:
Bicondylar tibial fractures: Internal or external fixation? Indian
J Orthop. 45:116–124. 2011.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Johnson EE, Timon S and Osuji C: Surgical
technique: Tscherne-Johnson extensile approach for tibial plateau
fractures. Clin Orthop Relat Res. 471:2760–2767. 2013.PubMed/NCBI View Article : Google Scholar
|