Introduction
Despite the development of novel implants based on
biomechanical principles, the mechanical complications of
osteosynthesis exhibit high rates of 1-32% (1-8).
In order to optimize the surgical treatment and the implant used,
biomechanical testing remains the gold standard. There is a
multitude of biomechanical studies on the osteosynthesis of
proximal femoral fractures, performed on both cadaveric and
composite bone, in different loading modes, with heterogeneous
results (1-7,9,10).
Although cadaveric bone has long been considered a ‘gold standard’
for biomechanical testing (3,11),
composite bone is an increasingly used alternative (9).
Knowing the area of contact of the hip joint and the
distribution of pressure during daily activities is important in
predicting the mechanism of mechanical complications after
osteosynthesis, providing biomechanical reasons for preoperative
planning and postoperative rehabilitation (12). While walking, the pressure on the
femoral head is not constant or evenly distributed. Yoshida et
al (12) stated that during
walking, the peak pressure is located on the side roof of the
acetabulum. During standing and sitting and while bending the
knees, the peak pressures are located at the edge of the posterior
horn (12). When climbing the
stairs, the maximum pressure is found on the side roof, and this is
higher than that when going down the stairs (12). Most studies (2-6,9,10)
perform the loading directly on the femoral head or through a metal
piece that concentrates the force on a limited area of the head,
thus not respecting the hip joint contact area (2,9,10). The
present study was performed to generate loading/unloading cups
similar to the human acetabulum with similar biomechanical
properties compared with the hip cartilage using additive
technology in order to simulate the in vivo conditions while
walking.
Materials and methods
Materials
After a comparative analysis of the materials
compatible with the Stratasys FORTUS 250 mc machine, acrylonitrile
butadiene styrene M30 (ABS-M30), a synthetic material with similar
mechanical properties compared with the cartilage at the level of
the adult hip (Table I), was
selected (13). The characteristics
of the ABS-M30 material were taken from the datasheet published by
Stratasys, Ltd. The characteristics of the hip cartilage were taken
from data reported in the literature (1). Acrylonitrile butadiene styrene (ABS)
is a thermoplastic polymer of fossil source obtained through the
polymerization of styrene and butadiene in the presence of
acrylonitrile, which allows the manufacturing of models using
additive manufacturing technology (14,15).
 | Table ICharacteristics of the ABS and ASA
material vs. hip cartilage (1,2). |
Table I
Characteristics of the ABS and ASA
material vs. hip cartilage (1,2).
| | Material |
|---|
| Characteristics | ABS-P400 | ASA | ABS-M30 | Hip cartilage |
|---|
| Tensile strength,
MPa | 22 | 32.8 | 36 | 80 |
| Tensile modulus,
MPa | 1,627 | 1,450-2,800 | 2,400 | 2,210 |
To simulate the articular cartilage at the level of
the femoral head and condyles and to achieve a uniform distribution
of the compression forces, the loading was carried out using two
3D-printed parts made on a Stratasys FORTUS 250 mc computer
numerical control (CNC) machine (Stratasys, Ltd.) using ABS-M30
(Stratasys, Ltd.).
Methods
For biomechanical testing, forces between 208 and
1,400 N with frequencies between 0.2 and 1 Hz were used to simulate
the normal gait of a 70 kg adult in vivo. The contact
surface of the femoral head with the loading cup was 27.7
cm2. At maximum load (1,400 N), the force to be
supported was 51.85 N/cm2, which was lower than the
tension modulus of the ABS-M30 material (2.4x105 N/cm²),
allowing its elastic deformation.
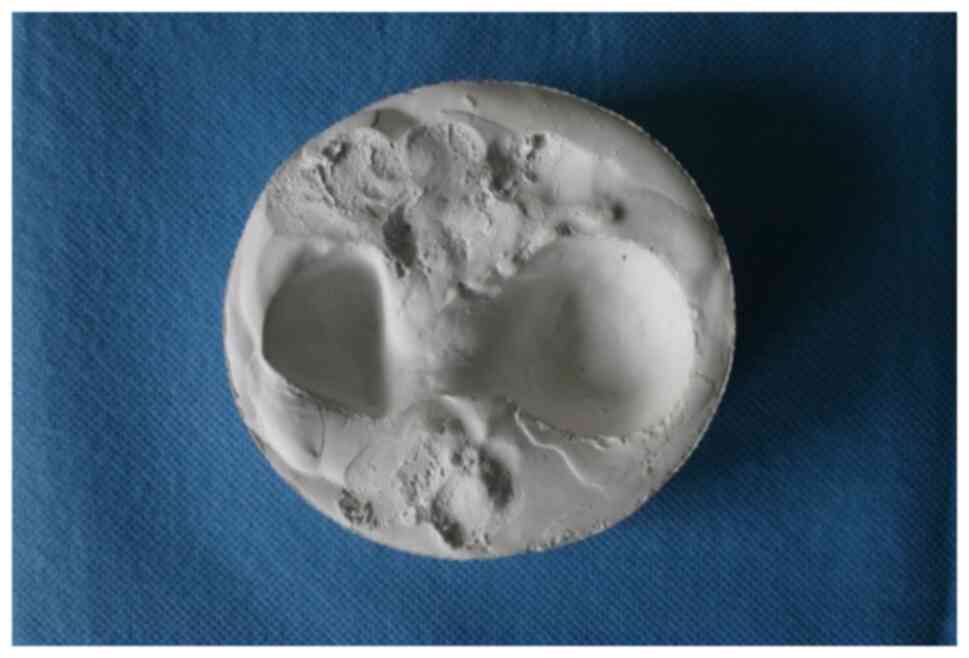
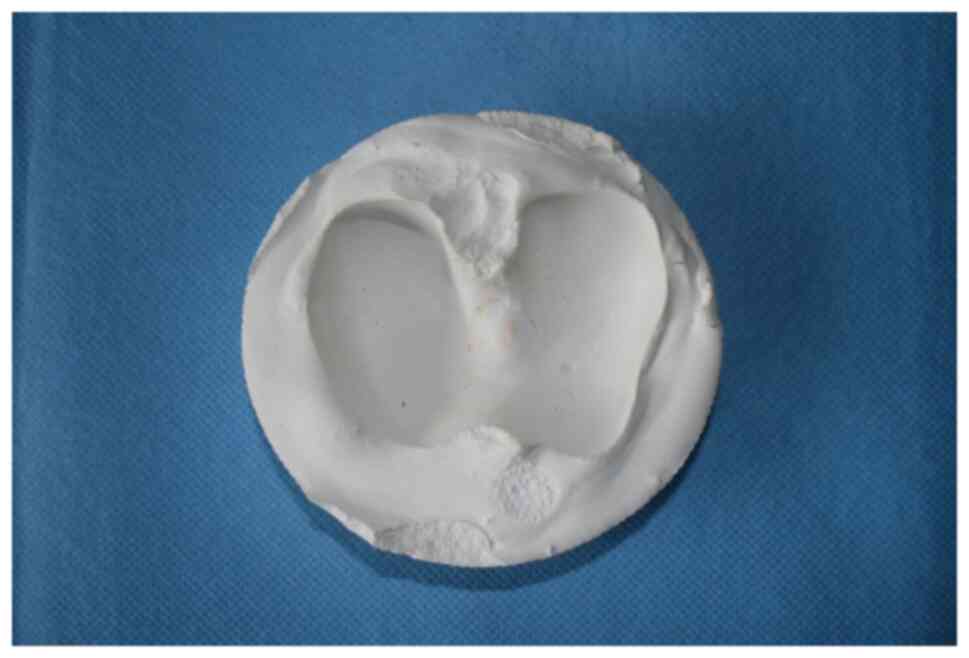
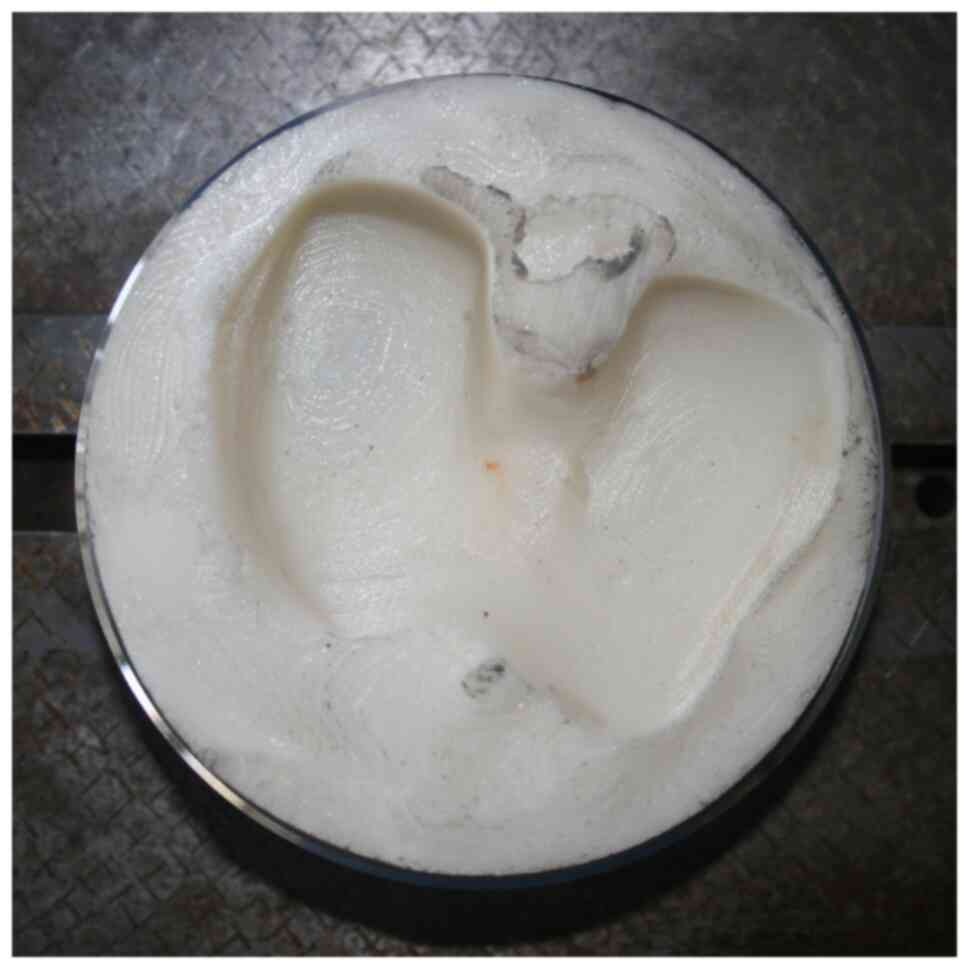
The loading/unloading cups were made through the
impression of a Sawbones® (Pacific Research
Laboratories, Inc.) femur model in casting gypsum (Figs. 1 and 2), which had been vacuum mixed for
degasification. After the impression was performed and the casts
were dried, the casts were painted for scanning using 3D Scan Spray
(Helling GmbH).
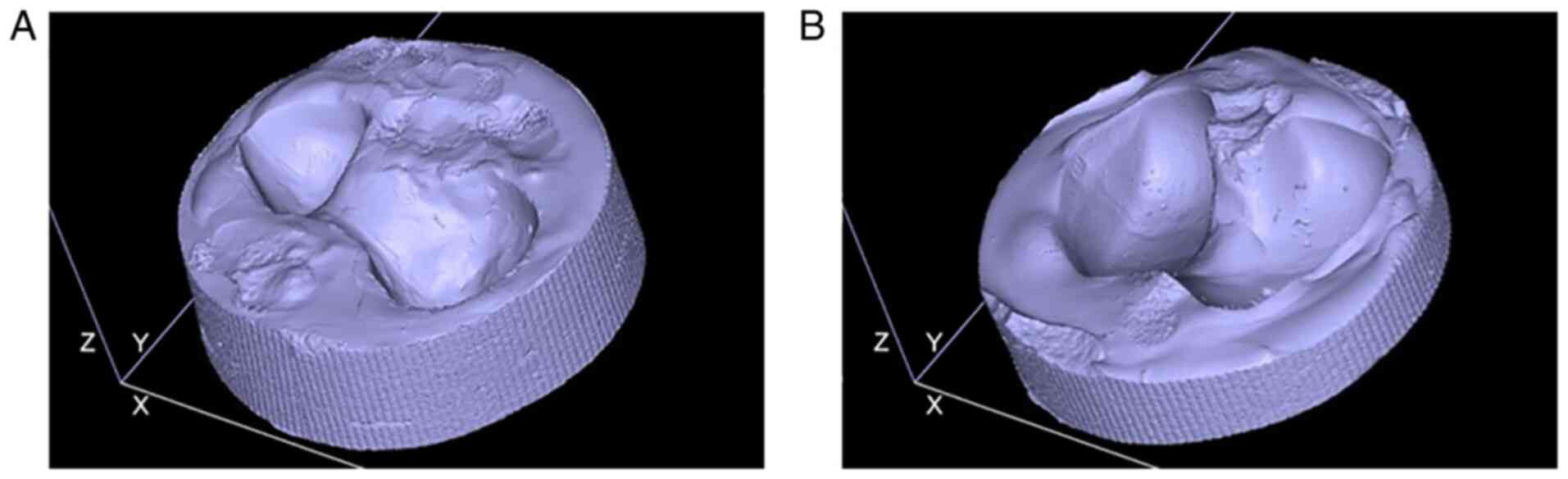
These casts were then scanned using a 3D scanner,
Creaform HandySCAN3D 300 (Ametek, Inc.) (Fig. 3), with a volumetric accuracy of 0.02
mm, obtaining 3D digital models in STL format using the Creaform
VXelements 1 software (https://www.creaform3d.com/en/metrology-solutions/3d-applications-software-platforms/vxmodel-scan-cad-software-module;
Fig. 4).
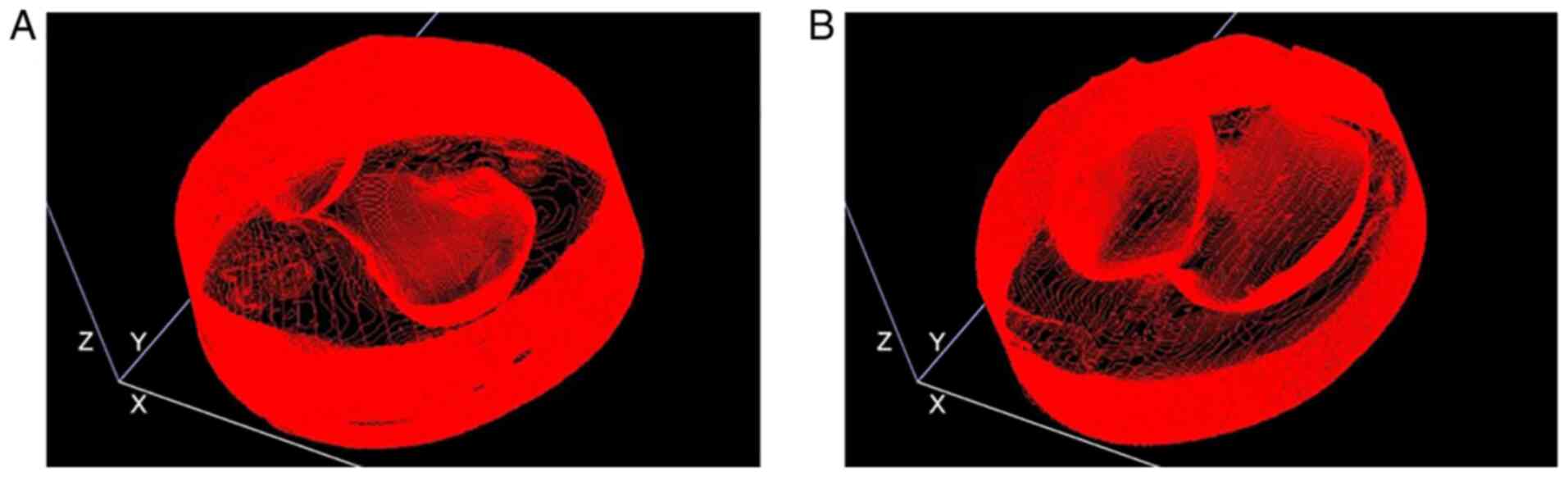
3D digital models in STL format were processed using
Insight software (v15.9; Stratasys, Ltd.; Figs. 4 and 5).
Results
Fig. 6, Fig. 7 and Fig.
8 show models obtained after processing, with the CNC
trajectories of the 3D printing head, in a thermally controlled
atmosphere. The distance between the printed layers was 0.127
mm.
The loading/unloading cups designed in this manner
simulated the acetabular cavity and the tibial plateaus
anatomically and could represent a good technical solution in order
to optimize the distribution of the loading/unloading forces in the
context of biomechanical experiments
Discussion
Most studies have attempted the loading directly on
the femoral head, thus failing to respect the in vivo model
(2,9,10).
Therefore, these studies (2-6,9,10)
have opted for loading the femoral head using a metallic plate that
shows limited contact with the femoral head. Other authors have
used a cadaveric hemipelvis, which was prepared to be tested
(7). In a biomechanical study on a
cadaveric femur (1), the femoral
head was loaded using a methyl polymethacrylate cup. Unlike the
aforementioned studies (2-6,9,10),
which attempted to load the femoral head by means of a rigid part
with limited contact, Kane et al (8) understood the necessity of a uniform
distribution of the mechanical stress at the level of the femoral
head and used a urethane polymer (Smooth-Cast1 Urethane Series 300;
Smooth-On, Inc.) to manufacture the loading cup. Although it
ensures a uniform distribution of mechanical tension in the femoral
head, the urethane polymer has properties similar to those of
natural rubber and fails to transmit forces naturally (https://us.misumi-ec.com/maker/misumi/mech/product/ur/detail/detail.html).
The ABS material was used by Reddy et al
(16) to design models of human
bones using additive manufacturing technology. They used CT to scan
various models of dry human bones and converted the resulting files
into the STL format, which was used to reconstruct the digital
model required for the 3D printing (16). Unlike Reddy et al (16), the present study used laser scanning
to create the 3D model, which is a faster and less costly
method.
It is well-known that, at the level of the femoral
head, the articular cartilage exhibits a phenomenon of progressive
degeneration following the loss of elasticity of the collagen fiber
network (17). Research conducted
by Kempson (17) and confirmed by
Silver et al (18) has
demonstrated that, at the level of the femoral head, the
superficial layer of the cartilage exhibits a decrease in pressure
resistance from 150 MPa at the age of 7 years to 80 MPa at the age
of 90 years and from 60 MPa at the age of 7 years to 10 MPa at the
age of 85 years. In a subsequent study, Silver et al
(13) identified an elastic module
of the articular cartilage at the level of the femoral head with
values of 7.0 GPa at parallel stress and 2.21 GPa at perpendicular
stress. In the present study, the ABS-M30 material used to design
the loading cup exhibited an elasticity module of 2.4 GPa, which
resembles the mechanical properties of adult hip cartilage.
3D printing is currently widely used in orthopedic
practice, particularly for pre-surgery planning in arthroplasties
and traumatology. Tack et al (14), in a systematic literature review
published in 2016, which analyzed the utility of 3D printing in
medical practice, identified 227 articles whose authors used
additive manufacturing technology in the current practice. Tack
et al (14) identified the
advantages of this technique: reduction of surgical time,
improvement of outcome and decrease of intra-surgery irradiation
time. In the field of research of orthopedics, notable progress has
been made regarding the mathematic modelling of the haversian
structure of the bone in view of designing experimental models
using additive manufacturing technology (15). Nevertheless, the authors of the
present study admit that there are important limitations related to
the printing material. Biomechanical studies simulating human
cartilage using additive manufacturing technology were not
identified in the literature. The selected material exhibits
similar tensile strength and tensile modulus compared with the
cartilage at the level of the adult human hip, thus mimicking the
mechanical properties of adult hip cartilage.
In conclusion, manufacturing the loading cups from
the ABS-M30 material using the method proposed in the present study
allowed the realistic reproduction of the anatomy and the
distribution of the forces at the level of the hip in in
vitro biomechanical studies simulating walking.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
EC and TSG conceived the study. EC, TSG, PDS and BP
developed the methodology. OA, AF and PDS performed formal
analysis. AF, NF and MGP performed data curation. TSG and NF wrote
the initial draft of the manuscript. EC and PDS confirm the
authenticity of all the raw data. OA, BP EC and PDS revised the
manuscript in light of the literature findings. All authors
provided resources. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wang J, Ma JX, Jia HB, Chen Y, Yang Y and
Ma XL: Biomechanical evaluation of four methods for internal
fixation of comminuted subtrochanteric fractures. Medicine
(Baltimore). 95(e3382)2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Schaefer TK, Spross C, Stoffel KK and
Yates PJ: Biomechanical properties of a posterior fully threaded
positioning screw for cannulated screw fixation of displaced neck
of femur fractures. Injury. 46:2130–2133. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Röderer G, Moll S, Gebhard F, Claes L and
Krischak G: Side plate fixation vs. intramedullary nailing in an
unstable medial femoral neck fracture model: A comparative
biomechanical study. Clin Biomech (Bristol, Avon). 26:141–146.
2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Windolf M, Braunstein V, Dutoit C and
Schwieger K: Is a helical shaped implant a superior alternative to
the Dynamic Hip Screw for unstable femoral neck fractures? A
biomechanical investigation. Clin Biomech (Bristol, Avon).
24:59–64. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Strauss E, Frank J, Lee J, Kummer FJ and
Tejwani N: Helical blade versus sliding hip screw for treatment of
unstable intertrochanteric hip fractures: A biomechanical
evaluation. Injury. 37:984–989. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Rosenblum SF, Zuckerman JD, Kummer FJ and
Tam BS: A biomechanical evaluation of the Gamma nail. J Bone Joint
Surg Br. 74:352–357. 1992.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Santoni BG, Nayak AN, Cooper SA, Smithson
IR, Cox JL, Marberry ST and Sanders RW: Comparison of femoral head
rotation and varus collapse between a single lag screw and
integrated dual screw intertrochanteric hip fracture fixation
device using a cadaveric hemi-pelvis biomechanical model. J Orthop
Trauma. 30:164–169. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kane P, Vopat B, Heard W, Thakur N, Paller
D, Koruprolu S and Born C: Is tip apex distance as important as we
think? A biomechanical study examining optimal lag screw placement.
Clin Orthop Relat Res. 472:2492–2498. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Basso T, Klaksvik J and Foss OA:
Statistical consequences of using bone mineral density to pair
cadaver femurs in comparative ex vivo hip fracture studies. Bone
Joint Res. 3:317–320. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Basso T, Klaksvik J, Syversen U and Foss
OA: A biomechanical comparison of composite femurs and cadaver
femurs used in experiments on operated hip fractures. J Biomech.
47:3898–3902. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Deneka DA, Simonian PT, Stankewich CJ,
Eckert D, Chapman JR and Tencer AF: Biomechanical comparison of
internal fixation techniques for the treatment of unstable
basicervical femoral neck fractures. J Orthop Trauma. 11:337–343.
1997.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yoshida H, Faust A, Wilckens J, Kitagawa
M, Fetto J and Chao EY: Three-dimensional dynamic hip contact area
and pressure distribution during activities of daily living. J
Biomech. 39:1996–2004. 2006.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Silver FH, Bradica G and Tria A: Elastic
energy storage in human articular cartilage: Estimation of the
elastic modulus for type II collagen and changes associated with
osteoarthritis. Matrix Biol. 21:129–137. 2002.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tack P, Victor J, Gemmel P and Annemans L:
3D-printing techniques in a medical setting: A systematic
literature review. Biomed Eng Online. 15(115)2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Robles-Linares JA, Ramírez-Cedillo E,
Siller HR, Rodríguez CA and Martínez-López JI: Parametric modeling
of biomimetic cortical bone microstructure for additive
manufacturing. Materials (Basel). 12(913)2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Reddy MV, Eachempati K, Gurava Reddy AV
and Mugalur A: Error analysis: How precise is fused deposition
modeling in fabrication of bone models in comparison to the parent
bones? Indian J Orthop. 52:196–201. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kempson GE: Age-related changes in the
tensile properties of human articular cartilage: A comparative
study between the femoral head of the hip joint and the talus of
the ankle joint. Biochim Biophys Acta. 1075:223–230.
1991.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Silver FH, Bradica G and Tria A:
Relationship among biomechanical, biochemical, and cellular changes
associated with osteoarthritis. Crit Rev Biomed Eng. 29:373–391.
2001.PubMed/NCBI View Article : Google Scholar
|