Introduction
The potential application of paraclinical methods
for investigating the temporomandibular joint (TMJ) has been a
subject of constant controversy due to the absence of definitive
criteria and the lack of consensus regarding usage. The mechanism
underlying mandibular movements is highly complex and it is
mandatory that novel examination methods are developed to further
the understanding in the function of this joint. Apart from
clinical evaluation and medical imaging, graphical recordings of
mandibular movements obtained using computerized axiography can
make a significant contribution to the functional evaluation of the
TMJ (1). Compared with medical
imaging, which provides a structural analysis of the TMJ,
axiography consists of making functional recordings of condylar
movements (2). Initially
implemented as a mechanical measurement method, axiography is also
called condylography and is currently being applied on digital
platforms (3).
Computerized axiography reveals information on the
opening, closing, lateral and protrusive movements (2,3), where
its graphical output can be analyzed in the horizontal as well as
the sagittal planes (4). This
method also enables the quantitative and qualitative analysis of
pathways in both the orbiting and pivoting condyle in terms of
symmetry, speed during articular movements and aspect of the
condylar pathway (5). In addition
to information on the optimal or suboptimal TMJ performance,
computerized axiography provides data required to program the
semi-adjustable articulator, which includes Bennett angle values
and the sagittal condylar inclination (6). This characteristic of computerized
axiography have proven useful in the dental treatment industry,
including prosthetic, orthodontic and orthognathic surgery, all of
which requires the faithful replication of musculo-articular
dynamics data of the dento-maxillary system (7).
The aim of the present study was to determine the
accuracy of using computerized axiography for diagnosing TMJ
displacements, using MRI as the reference standard. In addition,
another objective of the present study was to calculate the mean
values of the Bennett angle and sagittal condylar inclination and
determine their variations according to the pathology of each case
examined.
Patients and methods
Patients
In total, 33 (66 TMJs) with signs and symptoms of
TMJ disc displacement according to the Research Diagnostic Criteria
for Temporomandibular Disorders (RDC/TMD) (8) were enrolled in this prospective study
performed over 6 months (between May and October 2017). Of the 33
patients enrolled in the present study, there were five males and
28 females. The age of the patients ranged from 14 to 65, with a
mean ± SD age of 28.4±11.3 years. On the same day, each patient
underwent clinical examination and computerized axiography, which
was performed by a single clinician (DT). MRI was performed 1-7
days after clinical examination. The clinical examination and
computerized axiography were performed at ‘Stomestet’ Dental Clinic
(Cluj-Napoca, Romania), whereas MRI was performed at ‘Skyra Vision’
Imaging Center (Cluj-Napoca, Romania). Only patients with the
following clinical TMJ disorders were included in the study: Disc
displacement with reduction (DDwR) and disc displacement without
reduction (DDwoR). The following signs were necessary for DDwR
diagnosis: i) Joint noise reported by patient; ii) click detection
during opening/closing cycles; and iii) click detection during
lateral and protrusive movements. For DDwoR diagnosis, the
following signs were considered: i) Unassisted opening <35 mm
and assisted opening <4 mm more than the unassisted opening; ii)
contralateral movements <7 mm and/or uncorrected deviation to
the ipsilateral side on opening; and iii) absence of clicking noise
(8).
Patients with contraindication to MRI, including
claustrophobia, cardiac pacemakers or ferromagnetic metals
carriers, those who were unable to undergo computerized axiography
due to muscular instability or inability to correctly perform
mandibular movements, in addition to patients with masticatory
muscles disorders, were excluded.
The research protocol in the present study was
analyzed and approved by the Ethics Committee of the University of
Medicine and Pharmacy ‘Iuliu Hatieganu’ Cluj-Napoca (approval no.
403/02.07.2015). Written informed consent was obtained from each
participant or guardian/parent of the participant enrolled in the
study.
Clinical examination
Clinical examination was performed by a single oral
surgeon (DT). Diagnosis was made based on the patient's history and
physical examination. The clinician investigated the masticatory
and cervical muscles and both TMJs. Dental occlusion was also
analyzed, both static and dynamic. The diagnostic decision tree was
elaborated according to the RDC/TMD (8).
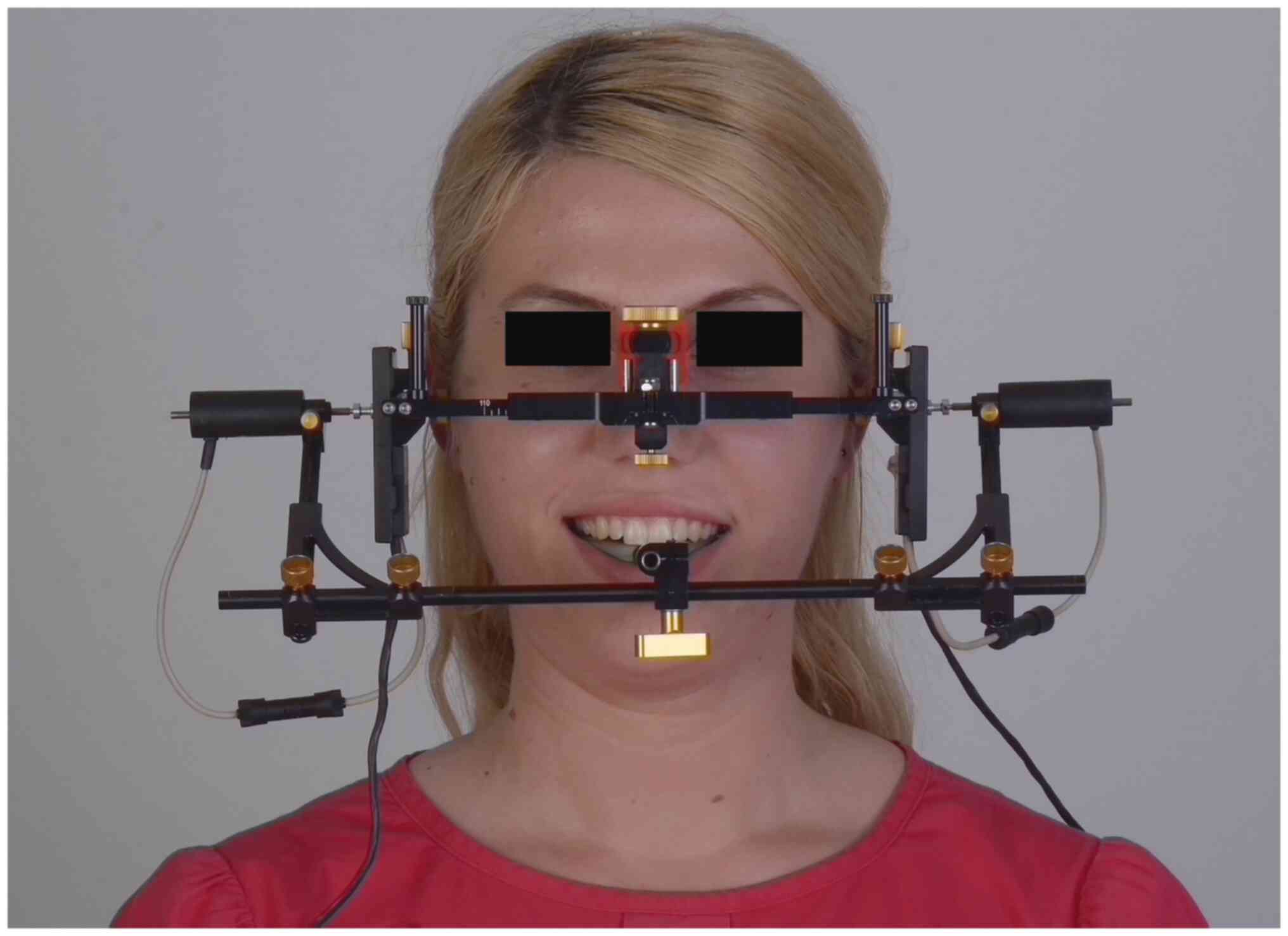
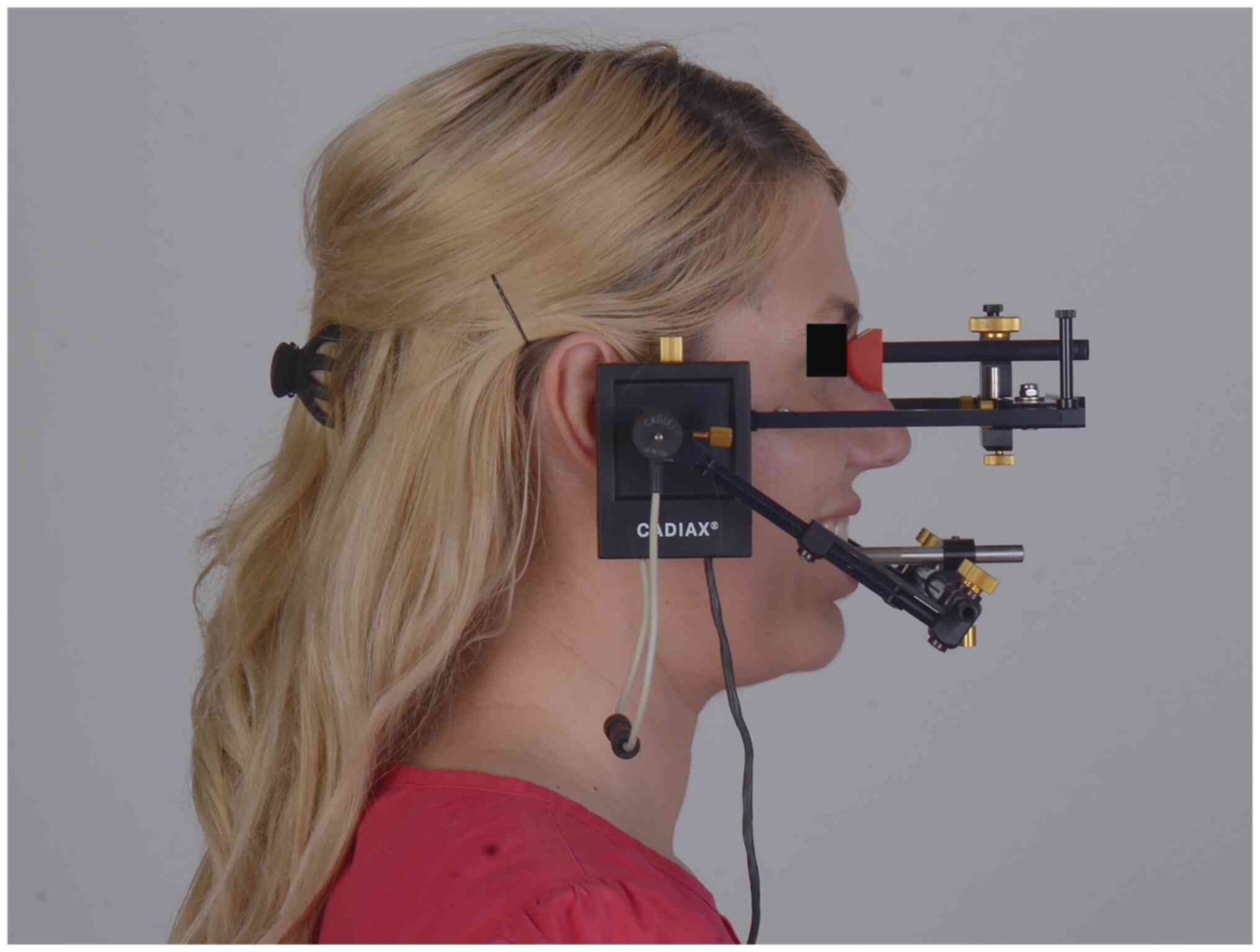
Computerized axiography
Computerized axiography and clinical examination
were performed on the same day by the same specialist. Axiography
was performed using the Cadiax Compact® II device (GAMMA
Medizinisch-wissenschaftliche Fortbildungs GmbH). Prior to
examination, each patient was informed about the movements required
during the examination. The Cadiax Compact® II device
consists of the following elements: A face bow; a mandibular bow; a
bite fork; two stilettos; two recording sensors; a central unit;
and a computer with the required software (Figs. 1 and 2; Cadiax Compact 2 Version 2.9.2; GAMMA
Medizinisch-wissenschaftliche Fortbildungs GmbHJ) (5).
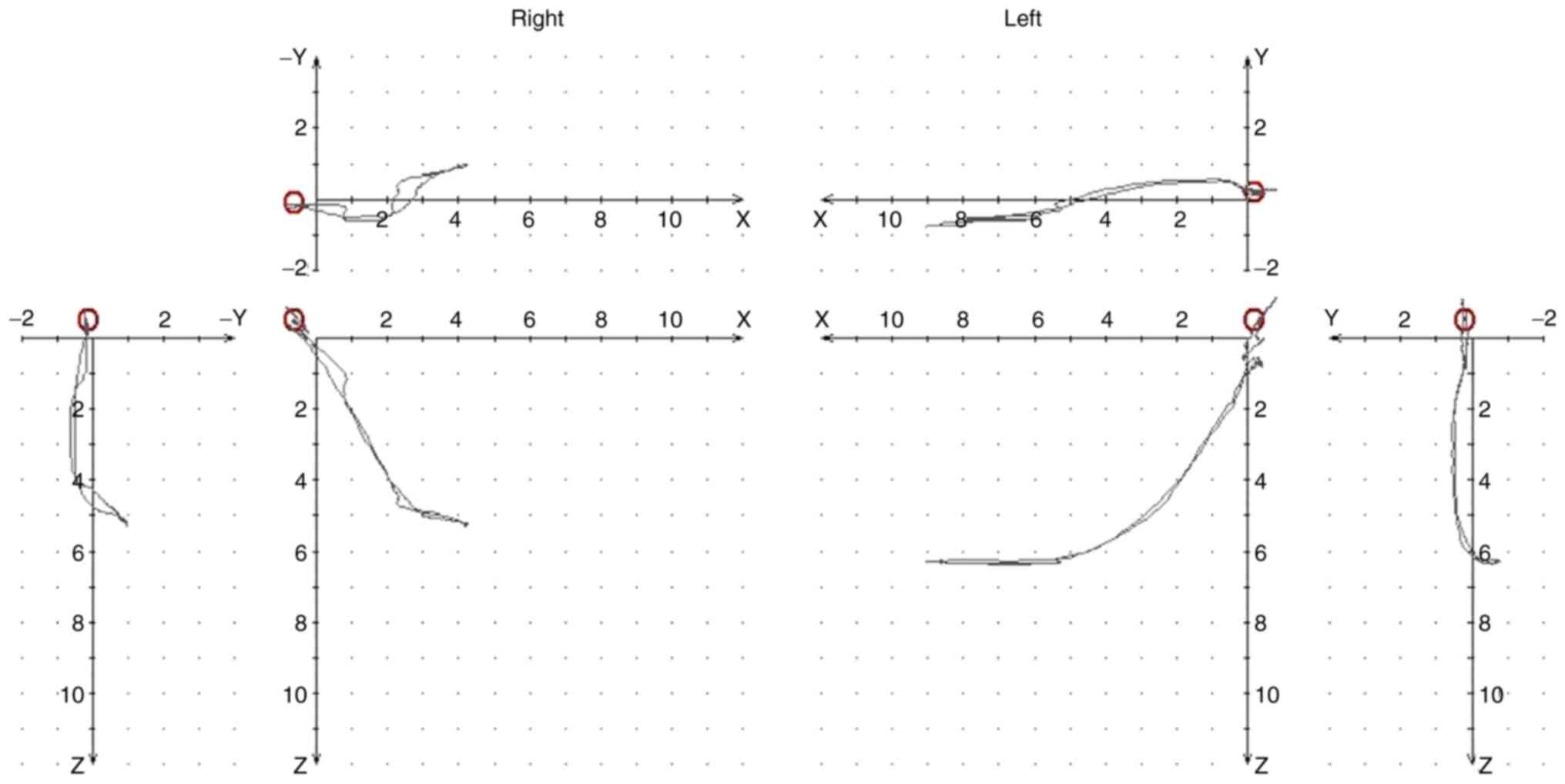
Recording mandibular movements
The reference position, which is the starting point
for all the movements, was always recorded first. This is followed
by maximum protrusion measurements, right laterotrusion
measurements, left laterotrusion measurements and maximum opening,
in that order. The recording is immediately displayed on the
computer screen, where the measurement procedure would be repeated
if the quality of the recording is of poor quality (due to patient
incoordination). The mandible would start moving from the reference
position, reaching maximum amplitude before returning to the
reference position. In total, two recordings were saved and stored
for each type of movement. The device allows for the superposition
of curves, which enables the verification of the reproducibility of
joint movements (9).
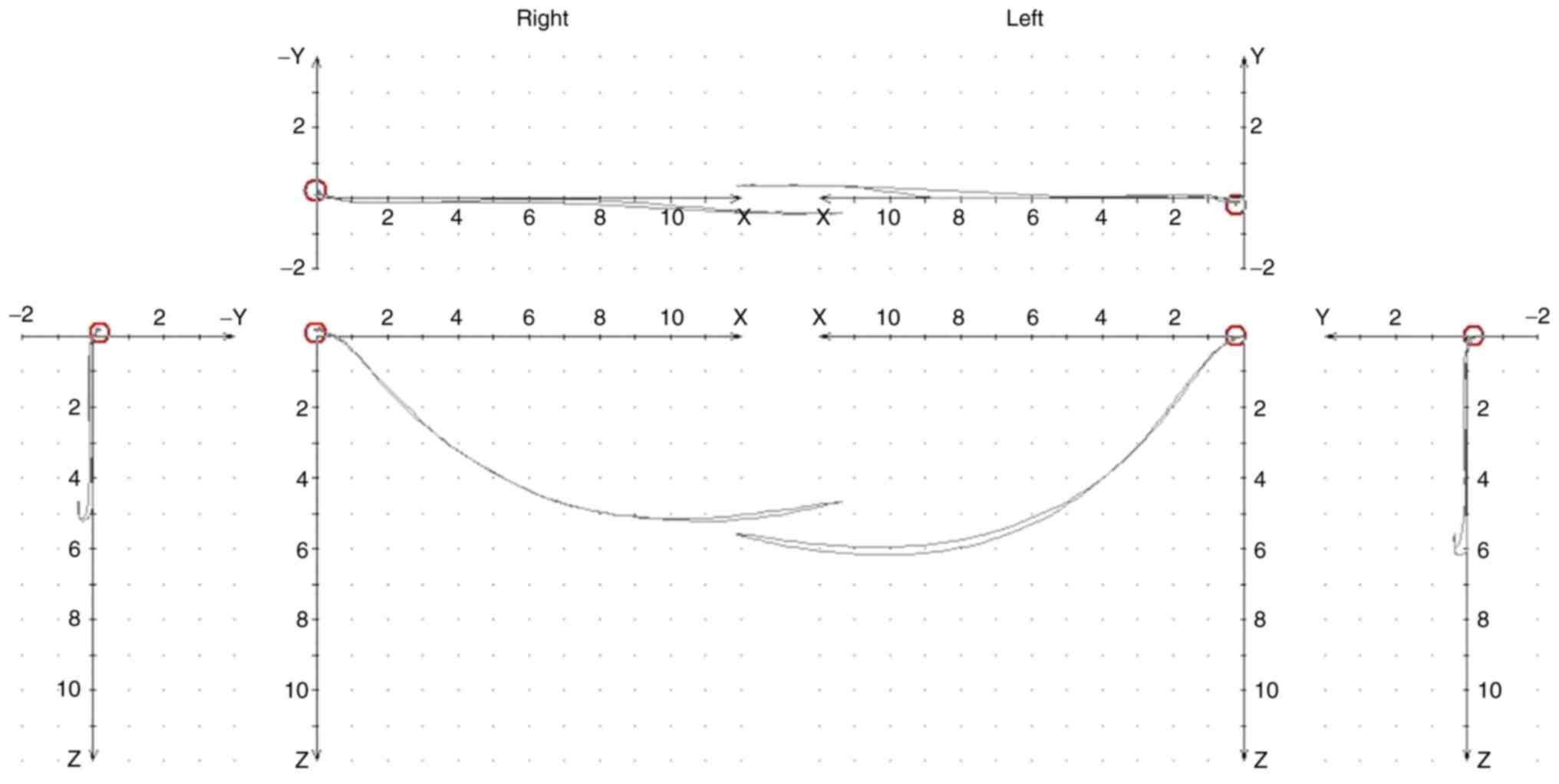
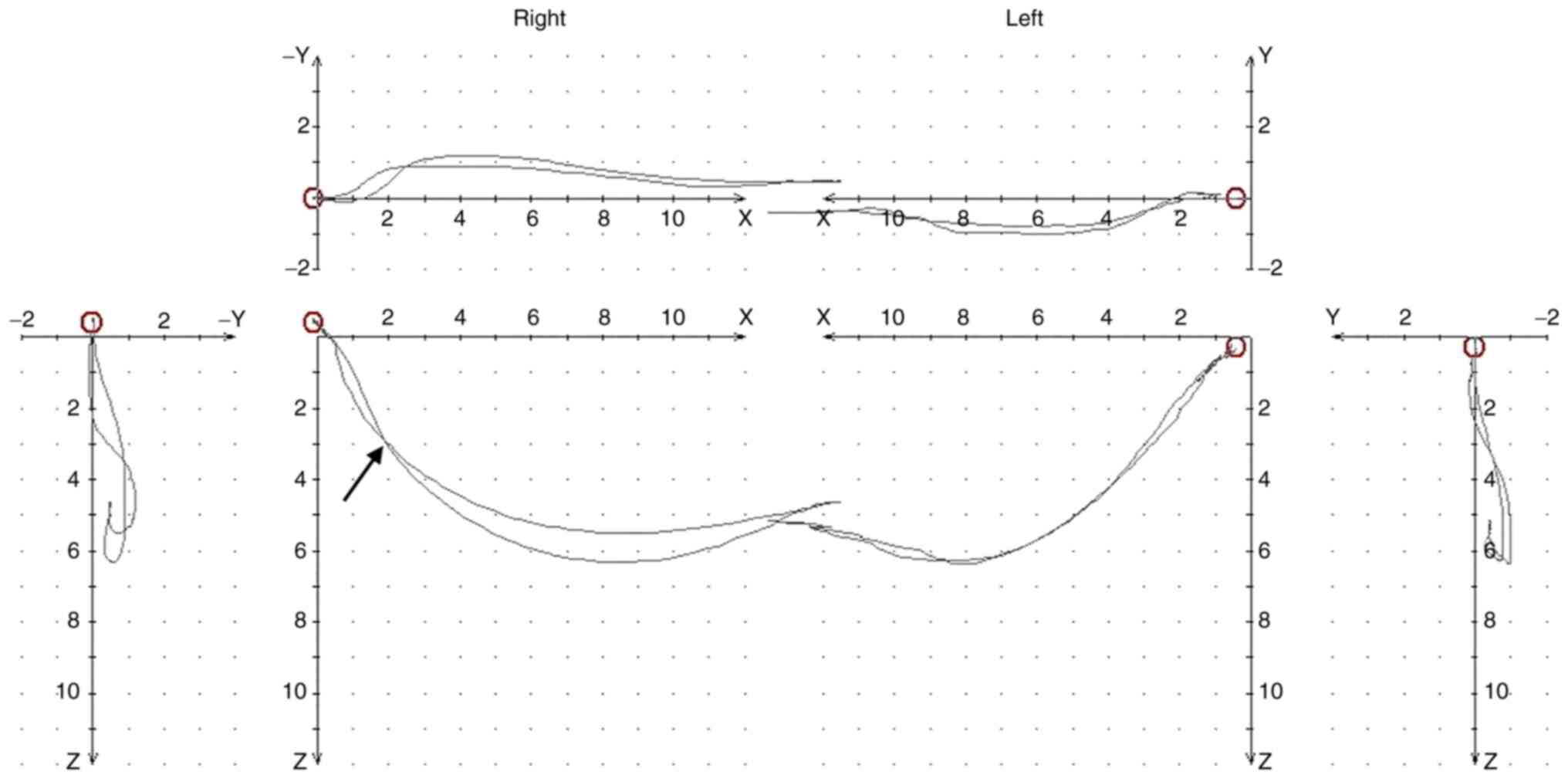
Diagnosis was made in accordance with the graphic
records, which were interpreted as follows: i) Normal TMJ was
defined as clear, regular, superimposed curves, with ≥14 mm
quantity for opening, 9 mm for maximum propulsion and laterotrusion
(Fig. 3); ii) TMJ with DDwR was
defined as observations that the advancement and return pathways to
the reference position do not overlap, but movement is not limited
from a quantitative point of view (Fig.
4); and iii) TMJ with DDwoR was defined as significant
quantitative limitation, with straight, linear pathways (Fig. 5). In addition, Bennett angle values
and the condylar sagittal inclination were also measured using
computerized axiography.
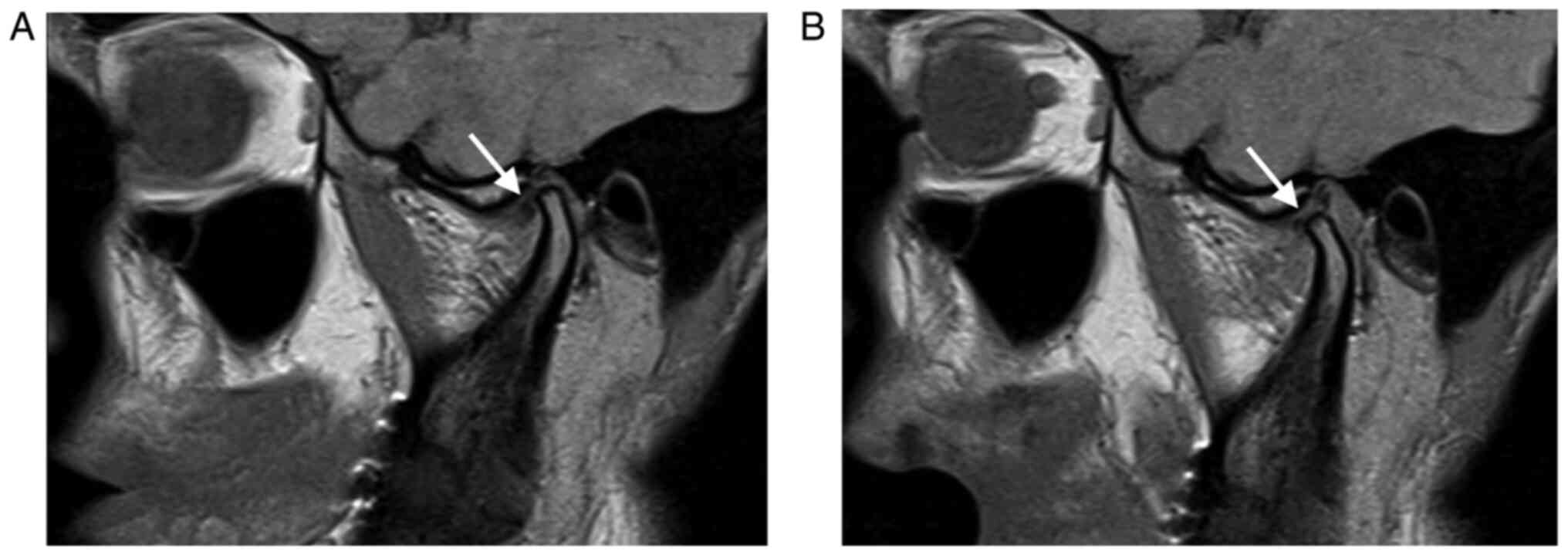
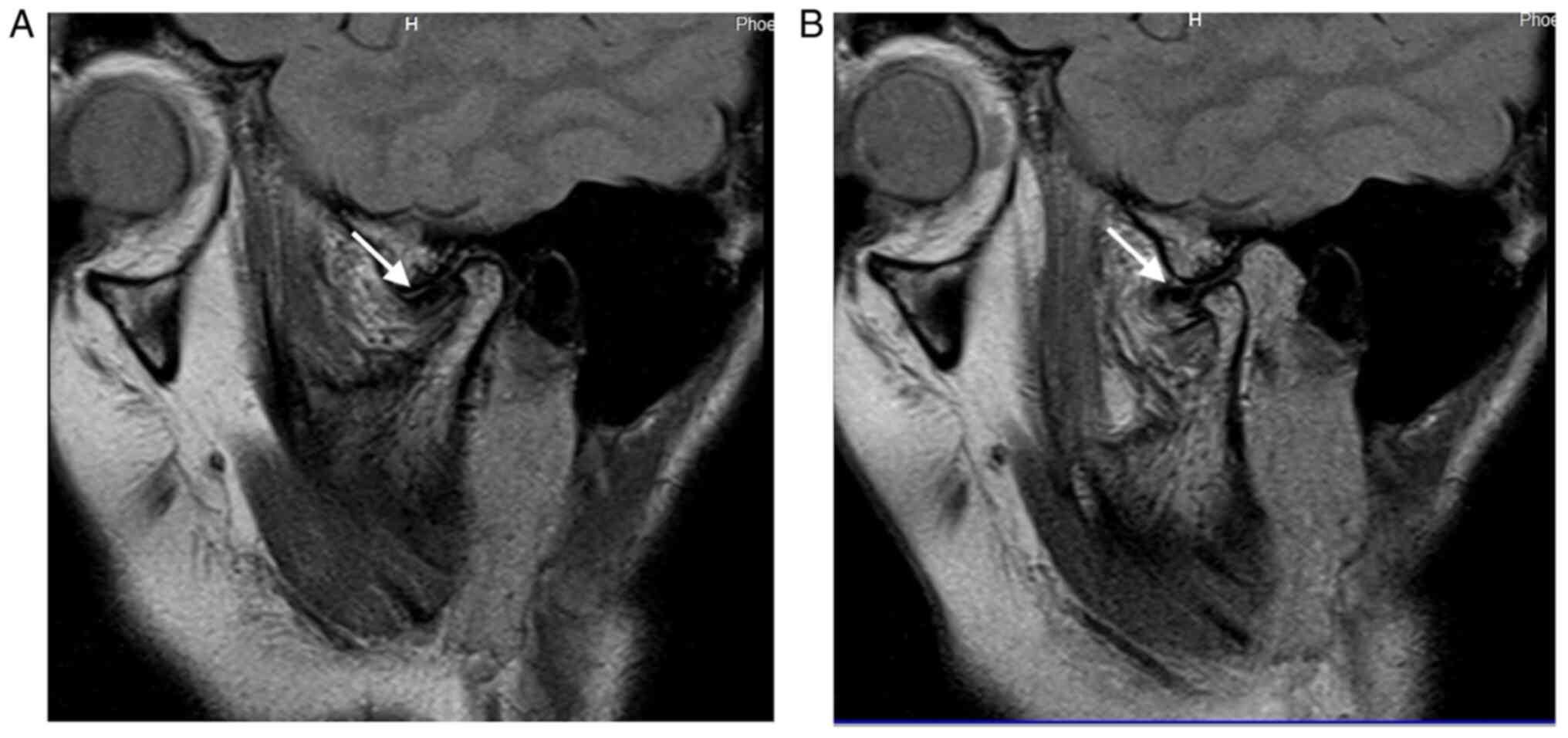
MRI examination
All MRI examinations were performed using a 1.5-T
MRI equipment (Siemens Avanto; Siemens Healthineers). MRI
assessment was performed by a radiologist (NB) blinded to both the
clinical and axiographic findings. Bilateral MR imaging of the TMJs
was performed using the same protocol. The data were collected on a
205/256 matrix, with a field of view of 120 mm and a flip angle of
150 degrees. Oblique-sagittal and coronal images were obtained of
both closed- and opened-mouth positions, perpendicular and parallel
to the long axis of the condyle. The MRI protocol included
T2-weighted and proton density sequences, with the thickness of
slices at 3 mm.
Disc displacement was considered to be present if
the posterior margin of the posterior band was situated anteriorly
to the vertical orientation of the condyle (the ‘12 o'clock line’)
(10). The MRI examination was
performed within 1-7 days following clinical examination and
computerized axiography. The results were interpreted by a single
specialist in maxillofacial imaging (NB; Figs. 6 and 7).
Statistical analysis
The characteristics of diagnostic tests
(computerized axiography being the index test, whilst MRI being the
standard test), namely sensitivity, specificity, positive and
negative predictive values, accuracy, Youden index and the 95%
confidence intervals (CI), were all computed. Exact binomial
confidence limits were calculated for the sensitivity, specificity,
positive and negative predictive values. Positive and negative
likelihood ratios were also assessed. All analyses were performed
using the R environment for statistical computing and graphics,
version 3.2.3(11).
Results
Comparison of the three
techniques
Clinical examination revealed 23 (34.85%) TMJs with
DDwR, 18 (27.27%) TMJs with DDwoR and 25 (37.88%) healthy TMJs.
Computerized axiography detected 22 (33.33%) TMJs with DDwR, 21
(31.82%) TMJs with DDwoR and 23 (34.85%) healthy TMJs. MRI
identified 30 (45.45%) TMJs with DDwR, 17 (25.76%) TMJs with DDwoR
and 19 (28.79%) healthy TMJs. In total, clinical examination
revealed 41/66 (62.12%) TMJs with disc displacements, whereas
computerized axiography showed 43/66 (65.15%). MRI indicated 47/66
(71.21%) TMJs with disc displacements (Table I). The number of disc displacements
diagnosed clinically and that diagnosed using computerized
axiography are comparable (41 vs. 43%; Table I). MRI, being the gold standard for
disc visualization, revealed the real number of disc displacements,
which was 47.
 | Table IThe results of the clinical
examination, computerized axiography and MRI. |
Table I
The results of the clinical
examination, computerized axiography and MRI.
| Examination | Total % of disc
displacements | Total % of normal
temporomandibular joints |
|---|
| Clinical
examination | 62.12 | 37.88 |
| Computerized
axiography | 65.15 | 34.85 |
| MRI | 71.21 | 28.79 |
Statistical indicators of computerized axiography,
including the sensitivity, specificity, diagnostic accuracy, Youden
index, positive predictive value, negative predictive value,
positive likelihood ratio and negative likelihood ratio were
assessed, using MRI as a reference standard (Table II). The sensitivity and specificity
of computerized axiography for detection of TMJ disc displacements
were 85.11 and 94.74%, respectively. The Youden index was also
found to be high (0.8), showing a viable diagnostic accuracy for
computerized axiography.
 | Table IIComputerized axiography findings
compared with MRI findings. |
Table II
Computerized axiography findings
compared with MRI findings.
| Statistical
parameter | Disc
displacement | 95% confidence
interval |
|---|
| Sensitivity, % | 85.11 | 71.69-93.8 |
| Specificity, % | 94.74 | 73.97-99.87 |
| PPV, % | 97.56 | 87.14-99.94 |
| NPV, % | 72 | 50.61-87.93 |
| LR+ | 16.17 | 2.39-109.36 |
| LR- | 0.16 | 0.08-0.31 |
| Diagnostic accuracy,
% | 87.88 | 77.51-94.62 |
| Youden index | 0.8 | 0.46-0.94 |
| Number necessary for
diagnosis | 1.25 | 1.07-2.19 |
The values of the Bennett angle and of the sagittal
condylar inclination were also calculated. The sagittal condylar
inclination had a mean ± SD of 42.08±8.02 (95% CI, 40.1-44.05),
with values ranging from 20 to 60. The Bennett angle variable
(transversal condylar guidance) had a median (IQR) of 9 (7-13)
with values ranging from 5 to 30 (95% CI, 7.5-11).
Discussion
The patient's clinical history and the observation
of articular noises, such as clicking, are typically used to
diagnose DDwR clinically (12).
However, clicking may be the result of other causes, not only disc
displacement (13). For instance,
articular ligaments may produce such noises, where a clicking sound
may occur during the rotational movement of the collateral lateral
ligament due to its fragility (13). Synovial noises, which occurs
especially when chewing solid food, are also described as having
the characteristics of clicking sounds. In addition, condylar
surface irregularities may be the cause of articular noises during
the rotational movement occurring in the lower compartment of the
joint, between the condylar surface and the articular disc
(12,14). Such cases are difficult to diagnose
clinically, rendering the axiographic investigation of the TMJ
potentially beneficial for obtaining additional important data for
accurate clinical diagnosis.
The high statistical values of specificity and
sensitivity obtained in the present study suggest computerized
axiography to be an important screening method for confirming or
exclude disc displacement. The resulting Youden index also
exhibited diagnostic value for the use of computerized axiography.
However, incipient DDwR cannot be diagnosed using axiography due to
the thickness of the bite fork applied on the lower arch. The
presence of the fork slightly increases the vertical dimension of
occlusion, where if the displacement is mild, the disc would adjust
itself to the new vertical dimension so that it appears as ‘normal’
in the reference position according to the axiograph recording. The
present study reported six such false negative cases. In this
situation, accurate diagnosis was required using MRI
examination.
Previous studies performed by Ahangari et al
(15) and Torabi et al
(16) substantiated the accuracy of
the Cadiax Compact® II device recordings, in terms of
both the resulting graphical output and values used for programming
the semi-adjustable articulator. In particular, the semi-adjustable
articulator program were compared to the wax records used for
programming the articulator.
Controversies remain regarding the application of
electronic devices for diagnosing TMJ disorders. Electronic methods
include axiography, electromyography and Doppler ultrasound for
recording articular noises (17). A
number of previous accounts (18-20)
asserted that using devices for recording mandibular dynamics serve
no diagnostic value. Cooper and Rabuzzi (21) reported that any movements recorded
by axiography are slower in patients with TMD compared with those
in healthy individuals (<300 mm/sec). By contrast, Feine et
al (22) found that slower
speeds, even bellow the aforementioned value, can also be recorded
in healthy individuals. In addition, Romanelli et al
(23) proposed that axiography is
an accurate method for diagnosing disc displacements in the TMJ.
Due to insufficient clinical data being available in this field, in
a 2018 review Constantinides et al (24) concluded that computerized axiography
is not a useful tool for detecting internal TMJ disturbances. In a
previous study of Manfredini et al (25), which evaluated the diagnostic value
of axiography in disc displacements and joint effusion, reached the
same conclusion. Indeed, controversial opinions and findings have
been reported on the potential diagnostic value of axiography. The
values obtained for sensitivity and specificity are summarized in
Table III. All previous studies
(26-30)
presented in Table III indicate a
very good specificity for computerized axiography, which is in
agreement with the results from the present study. Axiography
appeared to be a highly specific form of TMJ examination. In terms
of sensitivity, it appears to be lower (between 56 and 86%). As
also found in the present study and mentioned by Ozawa and Tanne
(28), the false negative results
are likely to be due to the application of the bite fork, which
could change the condylar starting position and is an important
factor in cases with incipient TMJ disc displacements. In the
present study, only six such cases were reported and the
sensitivity for the overall diagnosis of disc displacements was
85.11%. In addition, the diagnostic sensitivity obtained in the
studies mentioned in Table III
could be dependent on the multiple systems of classification used
for TMJ disc displacements (in terms of clinical and MRI
classification). The classification system differs from one study
to another and could affect the values of statistical
indicators.
 | Table IIIResults of the main studies that
previously evaluated the sensitivity and specificity of axiography
compared with MRI results. |
Table III
Results of the main studies that
previously evaluated the sensitivity and specificity of axiography
compared with MRI results.
| Author | Year | Sensitivity, % | Specificity, % | (Refs.) |
|---|
| Parlet et
al | 1993 | 64 | 100 | (26) |
| Rammelsberg et
al | 1996 | 86 | 90 | (27) |
| Ozawa and
Tanne | 1997 | 40 | 94 | (28) |
| Bracco et
al | 1997 | 56 | 96 | (29) |
| Kobs et
al | 2004 | 80 | 90 | (30) |
Piancino et al (31) previously analyzed the association
between computerized axiography and MRI data, which yielded a very
low kappa index of 13%. They then concluded that MRI and
computerized axiography are two completely different types of
examination methods that should instead be used in conjunction with
one another (31). The same
conclusion has also been reached by Piehslinger et al
(32), who obtained a concordance
of only 45% between MRI and computerized axiography.
In the present study, a mean value of the sagittal
condylar inclination of 42 degrees was found, whereas the Bennett
angle was 9 degrees. However, these values obtained were
heterogeneous, rendering correlation analysis between these two
parameters and the TMJ pathological parameters impossible. However,
a significant difference between a normal TMJ on one side and a
displaced TMJ on the other side for the same subject, regarding the
Bennett angle and the sagittal condylar inclination, was found.
Computerized axiography can also be used as a tool
for monitoring treatment progression by analyzing the graphic
outputs at different times, as suggested by a previous study
performed by Piancino et al (33). However, similar types of data can be
obtained by clinical examination of the muscles and TMJ (17).
A number of studies (30,34)
emphasized the importance of associating clinical examination
parameters with computerized axiography, suggesting that axiography
should be used as an extension of clinical examination as part of
the clinical analysis. As a result, axiography can increase the
diagnostic value to contribute to the differential diagnosis of
intra-articular pathology (32,34).
The present study proposes that computerized axiography, when used
as an additional diagnostic strategy, should be incorporated into
the clinical examination procedure. However, a limitation of the
present study is that the sample size is small and that the
calculation of intra- and inter-examiner agreement was not
performed.
To conclude, computerized axiography is a simple and
fast method that is capable of reproducing the functional movement
of the TMJ, which offers the opportunity to perform comparative
analyzes of the two joints. In addition, it can also be used for
the periodic evaluation of treatment progression of TMJ pathology.
MRI and computerized axiography can produce different types of data
regarding the TMJ status. Whilst MRI can yield important structural
data, axiography can reveal data on TMJ function.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Author's contributions
DT and SB confirm the authenticity of all the raw
data. DT: clinical investigation, conceptualization and analysis of
the results. NB: MRI interpretation and MRI image acquisition. DL:
methodology design of the study and statistical analysis. IAT:
visualization and validation. SB: interpretation of data, study
design. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The research protocol was analyzed and approved by
the Ethics Committee of the University of Medicine and Pharmacy
‘Iuliu Hatieganu’ Cluj-Napoca (approval no. 403/02.07.2015).
Patient consent for publication
Written informed consent was obtained from each
participant enrolled in the study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Botos AM, Mesaros AS and Zimbran AI: The
contribution of computerized axiography to the functional
evaluation of the temporomandibular joint: A case report. Clujul
Med. 89:438–442. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Slavicek R: Clinical and instrumental
functional analysis for diagnosis and treatment planning. Part 5.
Axiography. J Clin Orthod. 22:656–667. 1988.PubMed/NCBI
|
|
3
|
Kraljević S, Pandurić J, Badel T and
Dulcić N: Registration and measurement of opening and closing jaw
movements and rotational mandibular capacity by using the method of
electronic axiography. Coll Antropol. 27 (Suppl 2):S51–S59.
2003.PubMed/NCBI
|
|
4
|
Mantout B, Giradeau A, Perez C, Re JP and
Orthlieb JD: Technical validation of a computerized condylographic
system. J Stomat Occ Med. 1:45–60. 2008.
|
|
5
|
Buduru S, Blahuc S, Ciumasu A, Kui A,
Ciobanu C, Almasan O, Manziuc M and Negucioiu M: Temporomandibular
dysfunction diagnosis by means of computerized axiography. Med
Pharm Rep. 93:416–421. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Celar A and Tamaki K: Accuracy of
recording horizontal condylar inclination and bennett angle with
the cadiax compact. J Oral Rehabil. 29:1076–1081. 2002.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Schierz O, Klinger N, Schon G and
Reissmann DR: The reliability of computerized condylar path angle
assessment. Int J Comput Dent. 17:35–51. 2014.PubMed/NCBI(In English, German).
|
|
8
|
Schiffman E, Ohrbach R, Truelove E, Look
J, Anderson G, Goulet JP, List T, Svensson P, Gonzalez Y, Lobbezoo
F, et al: International RDC/TMD consortium network, international
association for dental research; orofacial pain special interest
group, international association for the study of pain. Diagnostic
criteria for temporomandibular disorders (DC/TMD) for clinical and
research applications: Recommendations of the international RDC/TMD
consortium network and orofacial pain special interest group. J
Oral Facial Pain Headache. 28:6–27. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Madhavan S, Dhanraj M and Jain AR: Methods
of recording mandibular movements-A review. Drug Invention Today.
10:1254–1259. 2018.
|
|
10
|
Tasaki MM and Westesson PL:
Temporomandibular joint: Diagnostic accuracy with sagittal and
coronal MR imaging. Radiology. 186:723–729. 1993.PubMed/NCBI View Article : Google Scholar
|
|
11
|
R Core Team R: A Language and Environment
for Statistical Computing R Foundation for Statistical Computing:
2020. http://www.r-project.org/index.html (accessed on 21st
of October 2017).
|
|
12
|
Okeson JP: Joint intracapsular disorders:
Diagnostic and nonsurgical management considerations. Dent Clin
North Am. 51:85–103. 2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Slavicek R: Diagnostics (Chapter 4). In:
The Masticatory Organ: Functions and Dysfunctions. Gamma
Medizinisch-Wissenschaftliche Fortbildungs-Gmbh, Klosterneuburg,
pp398-409, 2006.
|
|
14
|
Bag AK, Gaddikeri S, Singhal A, Hardin S,
Tran BD, Medina JA and Curé JK: Imaging of the temporomandibular
joint: An update. World J Radiol. 6:567–582. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ahangari AH, Torabi K, Pour SR and Ghodsi
S: Evaluation of the Cadiax Compact® II accuracy in
recording preadjusted condylar inclinations on fully adjustable
articulator. J Contemp Dent Pract. 13:504–508. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Torabi K, Pour SR, Ahangari AH and Ghodsi
S: A clinical comparative study of cadiax compact II and intraoral
records using wax and addition silicone. Int J Prosthodont.
27:541–543. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Manfredini D: Etiology. Instrumental
approach, Part. II. In: Current Concepts on Temporomandibular
Disorders. Quintessence Publishing Co. Ltd., London, pp223-235,
2010.
|
|
18
|
Widmer CG, Lund JP and Feine JS:
Evaluation of diagnostic tests for TMD. J Calif Dent Assoc.
18:53–60. 1990.PubMed/NCBI
|
|
19
|
Theusner J, Plesh O, Curtis DA and Hutton
JE: Axiographic tracings of temporomandibular joint movements. J
Prosthet Dent. 69:209–215. 1993.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Greene CS: Can technology enhance TM
disorder diagnosis? J Calif Dent Assoc. 18:25–33. 1990.PubMed/NCBI
|
|
21
|
Cooper BC and Rabuzzi DD: Myofacial pain
dysfunction syndrome: A clinical study of asymptomatic patients.
Laryngoscope. 94:68–75. 1984.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Feine JS, Hutchins MO and Lund JP: An
evaluation of the criteria used to diagnose mandibular dysfunction
with the mandibular kinesiograph. J Prosthet Dent. 60:374–380.
1988.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Romanelli GG, Harper R, Mock D, Pharoah MJ
and Tenenbaum HC: Evaluation of the temporomandibular joint
internal derangement. J Orofac Pain. 7:254–262. 1993.PubMed/NCBI
|
|
24
|
Costantinides F, Parisi S, Tonni I, Bodin
C, Vettori E, Perinetti G and Lenarda RD: Reliability of
kinesiography vs magnetic resonance in internal derangement of TMJ
diagnosis: A systematic review of the literature. Cranio. 38:58–65.
2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Manfredini D, Favero L, Federzoni E,
Cocilovo F and Guarda-Nardini L: Kinesiographic recordings of jaw
movements are not accurate to detect magnetic resonance-diagnosed
temporomandibular joint (TMJ) effusion and disk displacement:
Findings from a validation study. Oral Surg Oral Med Oral Pathol
Oral Radiol. 114:457–463. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Parlett K, Paesani D, Tallents RH and
Hatala MA: Temporomandibular joint axiography and MRI findings: A
comparative study. J Prosthet Dent. 70:521–531. 1993.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Rammelsberg P, Pospiech P, May HC and
Gernet W: Evaluation of diagnostic criteria from computerized
axiograhy to detect internal derangements of the TMJ. Cranio.
14:286–295. 1996.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Ozawa S and Tanne K: Diagnostic accuracy
of sagittal condylar movement patterns for identifying internal
derangement of the temporomandibular joint. J Orofac Pain.
11:222–231. 1997.PubMed/NCBI
|
|
29
|
Bracco P, Dergibus A, Piscetta R and
Giaretta GA: TMJ clicking: A comparison of clinical examination,
sonography and axiography. Cranio. 15:121–126. 1997.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kobs G, Bernhardt O and Meyer G: Accuracy
of computerized axiography controlled by MRI in detecting internal
derangements of the TMJ. Stom Baltic Dent Maxillofac J. 6:7–10.
2004.
|
|
31
|
Piancino MG, Cirillo S, Frongia G, Cena F,
Bracco AA and Bracco P: Axiography and MRI in the diagnosis of
temporomandibular joint pathology. J Stomat Occ Med. 2:50–51.
2009.
|
|
32
|
Piehslinger E, Schimmerl S, Celar A,
Crowley C and Imhof H: Comparison of magnetic resonance tomography
with computerized axiography in diagnosis of temporomandibular
joint disorders. Int J Oral Maxillofac Surg. 24:13–19.
1995.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Piancino MG, Loberi L, Frongia G,
Reverdito M, Slavicek R and Bracco P: Computerized axiography in
TMD patients before and after therapy with ‘function generating
bite’. J Oral Rehabil. 35:88–94. 2008.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Giraudeau A, Cheynet F, Mantout B, Dejou
J, Sarrat P and Orthlieb J: Diagnostic of intracapsular derangement
of TMJ: comparison of clinical examination and condylography with
MRI. Stomatologie. 104:154–167. 2007.
|