Introduction
Neuroendocrine tumors (NETs) are most commonly found
in the gastrointestinal tract. Previous epidemiological studies
have shown that the small intestine, rectum, and appendix are the
sites most at risk of developing NETs (1,2).
Appendiceal NET accounts for ~19% of all NETs and is the most
common type of appendiceal cancer. Even so, appendiceal NET is a
relatively rare disease in terms of prevalence, especially in
children (3). Due to the lack of
specific and standardized clinical guidelines, laboratory or
imaging profiles for diagnosis on presentation, it remains
exceptionally difficult to diagnose appendiceal NET preoperatively.
As a result, it can be easily misdiagnosed as acute or chronic
appendicitis. Therefore, such individuals would typically need a
second operation, which is performed based on the size of the
tumor. The present study reports an unusual case of acute
appendicitis in an adolescent individual caused by appendiceal NET.
The aim of the present case report is to provide guidance and
assistance for the early diagnosis and treatment of appendiceal NET
in children.
Case report
A 13-year-old female adolescent individual with pain
in the lower right abdomen for 3 days was first admitted to
Shanghai Children's Hospital (Shanghai, China). She initially
complained of pain in the lower right abdomen but without fever or
diarrhea 3 days before admission. However, she vomited once 1 day
before admission. No similar type of abdominal pain was experienced
by the patient in the past. Physical examination revealed a fixed
area of tenderness in the lower right abdomen without rebound
tenderness. No obvious masses could be found in the abdominal area
and the bowel sound was normal. Laboratory examination revealed her
inflammatory markers to be elevated. Specifically, the white blood
cell count was 8.49x109 cells/l and C reactive protein
(CRP) count was 15 mg/l. The blood biochemical parameters of liver
function, renal function and electrolytes were normal. In addition,
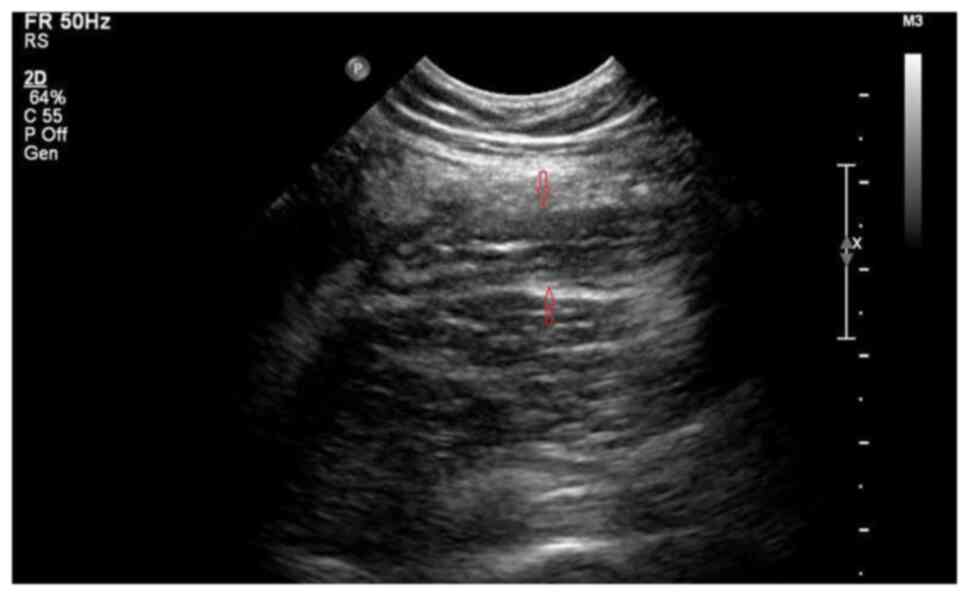
abdominal ultrasound revealed that the diameter of the appendix was
9 mm, suggesting an acutely inflamed appendix (Fig. 1). From the computerized tomography
(CT) scan images it could be observed that the appendix was
thickened with exudation, where there was a small quantity of fluid
within the pelvic cavity (Fig.
2).
After preoperative preparation, the patient
underwent surgery. During the operation, the appendix was found to
be located in the pelvic area with notable swelling in the head and
body. No obvious perforations were observed and the root of the
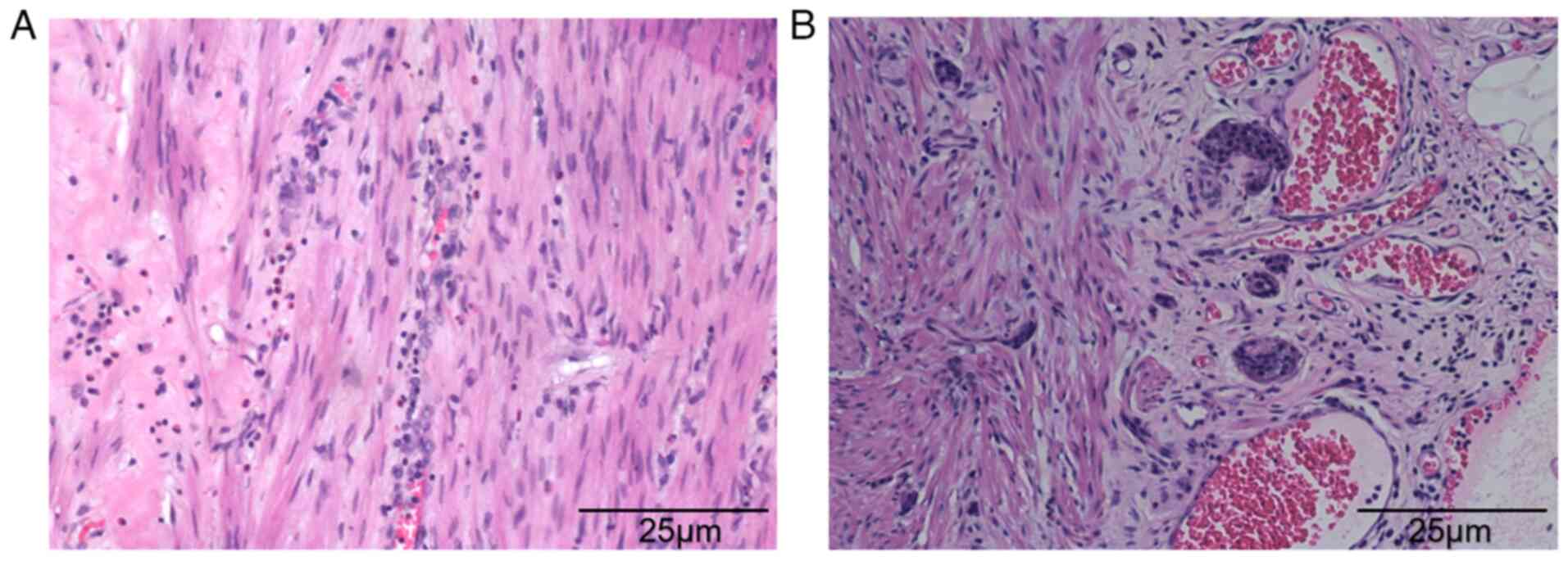
appendix was otherwise healthy. Pathological examination found that
a appendiceal NET was located at the tip of the appendix, the
diameter of which was 7 mm. Acute purulent appendicitis was also
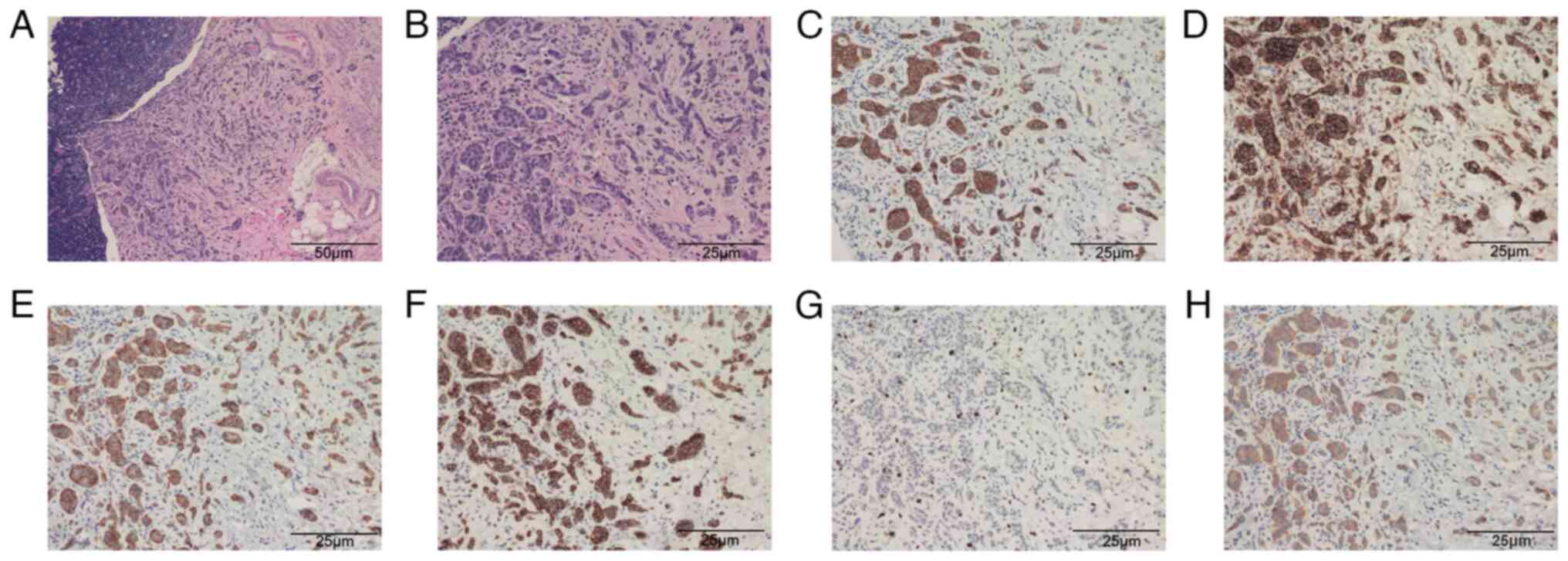
detected (Fig. 3). The diagnosis
of appendiceal NET was confirmed by the positive immunostaining of
tumor markers, such as synaptophysin (Syn)+, Ki-67,
chromogranin A (CgA)+, cytokeratin (CK)+,
CD56+, cytokeratin (CAM) 5.2+ (Fig. 4).
No further treatment was administered. The patient
recovered in 4 days after surgery and was discharged without
complications. No tumor recurrence and metastasis were found 2
years after the operation. Abdominal enhanced CT and enteroscopy
examinations yielded normal unremarkable results.
Discussion
Appendiceal neuroendocrine tumor (NET) is a
relatively uncommon and low-grade malignancy that has a detection
rate of 0.3 to 0.9% in all patients and only 0.08% in pediatric
patients following appendectomy (4,5). It
typically originates from subepithelial neuroendocrine cells
located in the intrinsic mucosa (6,7),
where its predilection site appears to be the tip of the appendix,
followed by the body and root of the same organ (8). According to the Ki-67 proliferation
index and the mitotic rate, which are considered to be predictors
of metastasis and recurrence, the WHO in 2010 classified
appendiceal NET into G1 [Ki-67 <2% and mitotic rate <2/10
high-power field (HPF)] and G2 [Ki-67 is 3-20% and mitotic rate is
2-20 HPF] (9). A number of studies
have previously shown that the clinical progression of G1- and
G2-stage appendiceal NET is relatively stable, with only limited
cases showing invasiveness (10).
The present case was diagnosed to be in the G1 phase.
Acute appendicitis, related to obstruction of the
appendix lumen by fecalith, lymphoid hyperplasia or tumors, is a
common surgical indication. Due to the low incidence of appendiceal
NET in children and the lack of specific clinical presentations,
the preoperative diagnosis of this disease is highly difficult. At
present it must be confirmed by pathological examination after
appendicitis appendectomy or other surgical interventions in the
abdominal cavity. Previous studies have revealed that patients with
appendiceal NET have older onset age and lower white blood cell
count compared with those with appendicitis (11). However, since these two differences
are not quantifiable, they can be easily ignored by clinicians. In
the case of the patient reported above, the tumor was located at
the tip of the appendix, where the clinical presentation was
similar to that of acute appendicitis.
The majority of appendiceal NET exhibit the
biological characteristics of benign tumors, such that metastasis
has almost never been observed in children (2). Therefore the primary choice of
treatment is surgery, where the scope of surgical resection is
determined according to the size, location and metastatic status of
the tumor. It is important to note that the size of the tumor is
the most reliable index for predicting invasion and therefore the
most important factor for determining the type of surgical method.
Furthermore, it is generally considered that tumors located in the
tip and middle of the appendix with a diameter of <1 cm will
more likely present biological characteristics of benign tumors
that will not undergo metastasis, but appendectomy is required.
However, ileocecal resection is advisable for tumors located in the
root of the appendix with diameters <1 cm, especially for
younger patients. By contrast, tumors with diameters >2 cm
frequently presents with biological characteristics of malignant
tumors, where the occurrence of distant metastasis is 20-85%. It is
generally considered at present that radical resection of the right
colon should been performed, although Ciarrocchi et al
(12) previously proposed that
tumor size should not be considered an absolute indication for
right hemicolectomy. For tumors with diameters of 1-2 cm, the
optimal surgical method remains controversial (13-15).
Furthermore, for tumors located in the tip or body of the appendix
that do not infiltrate into the serous membrane or lymph node,
appendectomy can be performed simply without complications
(16).
It remains to be a challenge to make an accurate
clinical diagnosis of appendiceal NET according to the currently
known atypical clinical presentations. While some patients can be
admitted to the hospital with symptoms such as lower right
abdominal mass and gastrointestinal bleeding, other patients can
appear with NET syndrome such as intermittent flush, purple face,
diarrhea, asthma attacks and shock (12). NET syndrome frequently indicates
that the tumor has already progressed to advanced stages.
Therefore, appendix swelling, fester, bezoar, necrosis or
perforation should not be the only parameter examined following
appendix resection. In addition, it should also be examined if
there is a yellow or white hard round mass in patients suspected
with appendicitis. Appendiceal NET should never be ruled out and a
biopsy must be conducted in time to avoid injuries caused by
secondary surgery in patients. In addition, laboratory examinations
of parameters, including serum serotonin, tryptophan and
5-hydroxyindoleacetic acid should be evaluated in patients
discovered with appendiceal NET accidentally after appendectomy.
Various forms of imaging examination such as chest X-ray,
ultrasonic and abdominal CT (17)
should also be performed to exclude metastases.
Appendiceal NET is a low-grade malignancy, with a
relatively optimistic clinical prognosis on account of the low
rates of distant metastasis, slow growth characteristics and long
natural course of the disease (18). Tumor size, proliferation rate,
infiltration of the appendiceal wall and status of the surgical
margins are indicators of prognosis (19).
In conclusion, appendiceal NET is rare in children
and there is a lack of specific clinical presentation. The majority
of patients present with symptoms similar to those of acute or
chronic appendicitis, rendering it easily misdiagnosed. Therefore,
clinicians should deepen their understanding of appendiceal NET,
which should be considered, particularly during surgical
procedures. The present report intends to highlight that
appendiceal NET should not be overlooked as an unusual cause of
acute appendicitis especially in children, to avoid the necessity
of a second operation.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TG conceived the study and wrote the initial draft
of the paper. TG also contributed to care of the patient and
literature review. WX contributed to the study, performed
additional analyses and produced the final draft of the paper. WX
and TG confirm the authenticity of all the raw data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The procedure mentioned in the present report has
been approved by the Ethics Committee of Shanghai Children's
Hospital (approval no. 2018R055).
Patient consent for publication
Written informed consent of this case report was
obtained from the legal guardian of the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Alexandraki KI, Kaltsas GA,
Grozinsky-Glasberg S, Chatzellis E and Grossman AB: Appendiceal
neuroendocrine neoplasms: Diagnosis and management. Endocr Relat
Cancer. 23:R27–R41. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Moris D, Tsilimigras DI, Vagios S,
Ntanasis-Stathopoulos I, Karachaliou GS, Papalampros A, Alexandrou
A, Blazer DG III and Felekouras E: Neuroendocrine neoplasms of the
appendix: A review of the literature. Anticancer Res. 38:601–611.
2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Emmanouil H, Paraskevi P, Vasiliki SF,
Fragandrea L and Koliouskas DE: Carcinoid tumors of the appendix in
children: Experience from a tertiary centre in northern Greece. J
Pediatr Gastroenterol Nutr. 51:622–625. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Allan B, Davis J, Perez E, Lew J and Sola
J: Malignant neuroendocrine tumors: Incidence and outcomes in
pediatric patients. Eur J Pediatr Surg. 23:394–399. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Shapiro R, Eldar S, Sadot E, Papa MZ and
Zippel DB: Appendiceal carcinoid at a large tertiary center:
Pathologic findings and long-term follow-up evaluation. Am J Surg.
201:805–808. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Meeks MW, Grace S, Chen Y, Petterchak J,
Bolesta E, Zhou Y and Lai JP: Synchronous quadruple primary
neoplasms: Colon adenocarcinoma, collision tumor of neuroendocrine
tumor and Schwann cell hamartoma and sessile serrated adenoma of
the appendix. Anticancer Res. 36:4307–4311. 2016.PubMed/NCBI
|
|
7
|
Wu H, Chintagumpala M, Hicks J, Nuchtern
JG, Okcu MF and Venkatramani R: Neuroendocrine tumor of the
appendix in children. J Pediatr Hematol Oncol. 39:97–102.
2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kim JY and Hong SM: Recent updates on
neuroendocrine tumors from the gastrointestinal and
pancreatobiliary tracts. Arch Pathol Lab Med. 140:437–448.
2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yamaguchi T, Fujimori T, Tomita S,
Ichikawa K, Mitomi H, Ohno K, Shida Y and Kato H: Clinical
validation of the gastrointestinal NET grading system.Ki67 index
criteria of the WHO 2010 classification is appropriate to predict
metastasis or recurrence. Diagn Pathol. 8(65)2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mullen JT and Savarese DM: Carcinoid
tumors of the appendix: A population-based study. J Surg Oncol.
104:41–44. 2011.
|
|
11
|
Van Gompel JJ, Stoddard E and Chen H:
Incidental carcinoid tumors of the appendix: Do they affect
presentation or prognosis? Int Surg. 92:331–334. 2007.PubMed/NCBI
|
|
12
|
Ciarrocchi A, Pietroletti R, Carlei F,
Necozione S and Amicucci G: Propensity adjusted appraisal of the
surgical strategy for appendiceal carcinoids. Tech Coloproctol.
19:35–41. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lambert G, Lardy H, Martelli H, Orbach D,
Gauthier F and Guérin F: Surgical management of neuroendocrine
tumors of the appendix in children and adolescents: A retrospective
French multicenter study of 114 cases. Pediatr Blood Cancer.
63:598–603. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ciarrocchi A, Rindi G and Pietroletti R:
Diagnosis and treatment of primary tumors of the appendix: A
critical review. J Gastrointest Cancer. 52:471–475. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lobeck IN, Jeste N, Geller J, Pressey J
and von Allmen D: Surgical management and surveillance of pediatric
appendiceal carcinoid tumor. J Pediatr Surg. 52:925–927.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
National Comprehensive Cancer Network
Guidelines for patients neuroendocrine tumors (version1 .2018).
Available from: https://www.nccn.org/patients/guidelines/content/PDF/neuroendocrine-patient.pdf.
|
|
17
|
Ciarrocchi A, Pietroletti R, Carlei F and
Amicucci G: Clinical significance of metastatic lymph nodes in the
gut of patients with pure and mixed primary appendiceal carcinoids.
Dis Colon Rectum. 59:508–512. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Deschamps L and Couvelard A: Endocrine
tumors of the appendix: A pathologic review. Arch Pathol Lab Med.
134:871–875. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Prommegger R, Obrist P, Ensinger C,
Profanter C, Mittermair R and Hager J: Retrospective evaluation of
carcinoid tumors of the appendix in children. World J Surg.
26:1489–1492. 2002.PubMed/NCBI View Article : Google Scholar
|