Introduction
Radioresistance has important role in local
recurrence and distant metastases of head and neck cancer (HNC).
Radiation-induced cytokines in the tumor and its microenvironment
collectively contribute to the tumor response to radiation
(1-3).
CD47 is expressed on the surface of human cancer cells including
head and neck cancer and has been implicated in various
pathophysiologic processes including tumor cell apoptosis,
survival, proliferation, migration, adhesion, and metastasis.
Cancer cells expressing CD47, which evade the innate immune system
initiates a signaling cascade to inhibit macrophage phagocytosis
(4-6).
Previously, CD47 has been regarded as an attractive
radio-therapeutic target because blocking CD47 signal can increase
to radiation response with protection of normal tissues (7). Furthermore, CD47 is frequently
overexpressed in HNC and radiation causes a decrease of CD47
expression in a dose-dependent manner (3). However, the mechanism of CD47
overexpression has not been elucidated in radioresistant HNC.
The RNA-binding protein, Tristetraprolin (TTP), is
encoded by the ZFG36 gene and is one of the most well-characterized
AU-rich element (ARE)-binding proteins within the 3'UTR. It
enhances decay of ARE-containing transcripts and plays an important
role in various processes including cellular differentiation,
proliferation, tumorigenesis, and immunity (8-12).
Because of its ability to bind and target ARE-containing mRNAs for
rapid degradation, numerous studies have shown that TTP exhibits as
tumor-suppressor. Thus, loss of TTP expression or function is
closely associated with tumor progression or poor outcome in
malignant tumors (13,14). It was known that some
tumor-associated genes with ARE sequences can be subject to
TTP-mediated mRNA degradation. The data indicate that target mRNAs
of TTP are mainly oncogenes in tumorigenesis (12).
Previously, it was reported that a regulatory
pathway for the IL-23, IL-27, and IL-33 cytokines by TTP could be
important role in regulation of antitumor immunity (15-17).
However, there are no convincing reports that identify the
molecular mechanism for the regulation of CD47 by TTP in cancer
cells exhibiting radioresistance. In the present study, we
demonstrate that decreased TTP expression induced sustained CD47
overexpression and prevented phagocytosis in radioresistant HNC
cells. Thus, TTP transfection can enhance phagocytosis through its
derogation activity by directly binding to CD47 AREs within the
CD47 3'UTR in radioresistant HNC cells. Based on our previous study
in which DNMT1 was overexpressed in radioresistant HNC (18), we found that DNMT1 regulated TTP
expression by DNA methylation, epigenetically.
Materials and methods
Cell culture
We used HN31 cells provided by Dr Jeffrey N. Myers
(University of Texas, MD Anderson Cancer Center). The HNC were
cultured in Dulbecco's modified Eagle's medium (Invitrogen; Thermo
Fisher Scientific, Inc.) with 10% fetal bovine serum (Invitrogen)
and 100 µg/ml of penicillin/streptomycin and incubated at 37˚C and
5% CO2. HNC cells were cultured to ~50% confluence in
vented 75 cm2 culture flasks. An isogenic model of
successively irradiated HN31R cells was established as our
protocols designed to investigate radioresistance (19).
In vitro phagocytosis assay
Macrophages (1x105) were seeded into
glass bottom cell culture dishes (NEST Biotechnology, 801002). HN31
or HN31R cells were labeled with CFDA SE according to the
manufacturer's protocol. Before the adding 2x105 of CFDA
SE-labeled tumor cells, macrophages were incubated in serum-free
medium for 2 h. Macrophages were repeatedly washed and subsequently
images were captured using a confocal microscope. The phagocytic
index was estimated as the number of phagocytosed CFSE+ cells per
100 macrophages.
Quantitative real-time PCR (qRT-PCR)
analysis for RNA kinetics
For RNA kinetic analysis, actinomycin D was used and
CD47 mRNA expression assessed by quantitative PCR. Total RNA was
isolated with the PureLink™ RNA Mini Kit (Thermo Fisher Scientific,
Inc.) and cDNA synthesized with a first-strand cDNA synthesis kit
by reverse transcription-PCR (iNtRON Biotechnology). We used
SYBR®-Green master mix (Applied Biosystems; Thermo
Fisher Scientific, Inc.) for qRT-PCR using a PRISM®-7500
sequence detection system (Applied Biosystems; Thermo Fisher
Scientific, Inc.). All reactions were performed in triplicate in
96-well plates and the mean values used to estimate mRNA
expression. The primer sequences were as follows: CD47 forward,
5'-TATCCTCGCTGTGGTTGGACTG-3' and reverse,
5'-TAGTCCAAGTAATTGTGCTAGAGC-3'; TTP forward,
5'-CGCTACAAGACTGAGCTAT-3' and reverse, 5'-GAGGTAGAACTTGTGACAGA-3';
GAPDH forward, 5'-ACATCAAGAAGGTGGTGAAG-3' and reverse,
5'-CTGTTGCTGTAGCCAAATTC-3'.
Transfection of TTP
TTP overexpressing HN31R cells were generated using
the pcDNA6/V5 vector (Invitrogen; Thermo Fisher Scientific, Inc.).
We cloned the full-length human cDNA of TTP using RT-PCR from the
RNA of HN31 cells with forward primer
5'-CCGTGAATTCATGGATCTGACTGCCAT-3' and reverse primer
5'-CACTCTCGAGCTCAGAAACAGAGATGC-3' The product was subcloned into
the pcDNA6/V5 vector. Approximately 1.5x107 cells were
electroporated using 20 µg of pcDNA6/V5-TTP at 500 V, 975 lF using
a Gene Pulser electroporator II (Bio-Rad). After transfection,
transfected HN31R/pcDNA6/V5-TTP cells with human TTP were selected
with 10 µg of Blasticidin/ml (Invitrogen; Thermo Fisher Scientific,
Inc.) at 3 days after transfection. Stable TTP overexpression was
tested by western blots using anti-human TTP polyclonal antibody
(ab33058; Abcam). A control cell line, HN31R/pcDNA6/V5, was made by
transfection with the pcDNA6/V5 vector.
RNA interference
HN31 cells were pated into 6-well plates
(3x105 cells per ml) 24 h before transfection. HN31
cells was transfected with 45 nM of TTP-siRNA (sc-36760; Santa Cruz
Biotechnology, Inc.), 50 nM of CD47 siRNA (h) (sc-35006), 30 nM of
EphA3 siRNA (sc-39934; Santa Cruz Biotechnology, Inc.) or control
siRNA-A (sc-37007; Santa Cruz Biotechnology, Inc.) with
Lipofectamine™ RNAiMAX (Invitrogen; Thermo Fisher
Scientific, Inc.). The cells were grown for 24 h before western
blotting analysis. TTP expression was evaluated at 3, 7 days and
every experiment.
Dual-luciferase assay
Analysis of human CD47 3'UTR revealed the presence
of thirteen AREs (http://rna.tbi.univie.ac.at/AREsite2/welcome). A
various deletion mutant of the CD47 3'-UTR were PCR-amplified from
the cDNA of HN31R cells by PCR using the following primer sets:
CD47 Frag-ARE-1-7, CCGCTCGAGACGTGATTGTTAGTT and
ATTTGCGGCCGCCTGATTTAAAGAGA; CD47 Frag-ARE-8-13,
CCGCTCGAGCAAATTCCATCACAT and ATTTGCGGCCGCACAATCATTTCTCC; CD47
Frag-ARE-10-13, CCGCTCGAGGCTTAGTTCTATTAG and
ATTTGCGGCCGCACAATCATTTCTCC; CD47 Frag-ARE-8-13(No9 mut AUUUA-AGCA),
GACTCTTCCATTCAGTTTTAGCATTGTGTGTTCTCACAGTGACAC and
GTGTCACTGTGAGAACACACAATGCTAAAACTGAATGGAAGAGTC.
The PCR products were inserted into the
XhoI/NotI sites a psiCHECK2 Renilla/firefly
Dual-Luciferase expression vector (Promega). Luciferase assays,
HN31R cells were co-transfected with thepsiCHECK-CD47 3'-UTR
constructs and pcDNA6/V5-TTP with the TurboFect™. Transfected cells
were collected at 24 h for RNA extraction and at 48 h for
measurement of luciferase activity using Wallac Victor 1420
multilabel counter (EG&G Wallac). Firefly luciferase activity
of psiCHECK2/CD47 3'UTR was normalized to Renilla luciferase for
each sample and Luciferase assays represent at least three
independent experiments.
Electrophoretic mobility shift assay
(EMSA)
The biotinylated RNA probes for wild-type
(wtCD47-EMSA,
5'-UUGACUCUUCCAUUCAGUUUUAUUUAUUGUGUGUUCUCACAGUGACACCAUU-3') and
mutant (mutCD47-EMSA,
5'UUGACUCUUCCAUUCAGUUUUAGCAUUGUGUGUUCUCACAGUGACACCAUU-3') were
synthesized by BIONEER Co. (Daejeon, Korea). RNA EMSA was performed
with Lightshift® Chemoluminescent EMSA Kit (Pierce) as
previously described protocols (20).
Western blot analysis
Total protein was extracted with RIPA buffer (Thermo
Fisher Scientific, Inc.). Protein concentrations were calculated
using the Bradford assay kit (Bio-Rad Laboratories). Equal amounts
of protein were separated by SDS-PAGE and transferred to
nitrocellulose membranes (Amershan International). Membranes were
incubated with primary antibodies to Tristetraprolin (ab33058;
Abcam), CD47 (ab175388; Abcam), DNMT1 (#5032; Cell Signaling
Technology), EphA3 (sc-920; Cell Signaling Technology), phospho-AKT
Ser473 (#4060; Cell Signaling Technology) and β-actin (sc-47778;
Sigma-Aldrich; Merck KGaA). Membranes were then incubated with
secondary antibodies (anti-mouse or anti-rabbit IgG HRP conjugate;
Bethyl Laboratories), and specific binding was detected with a
SuperSignal West Pico Trial kit (Thermo Fisher Scientific, Inc.)
according to the manufacturer's instructions (Cayman Chemical).
Western blotting analysis was performed at least three times, and
representative figures are presented. The expression of the protein
was quantified as compared to the beta-actin in the Western
blot.
Methylation-specific PCR (MSP) for
TTP
Genomic DNA (1 µg) was denatured with sodium
bisulfite using the EpiTect Bisulfite kit (Qiagen). This treatment
resulted in the conversion of unmethylated cytosine to thymine, but
methylated cytosine remained not changed. Primer sequences of TTP
were as follows: (5'-to-3'): TTP, ATTGGGTAGGTGTTT thymidine's
TATTTGT (unmethylated sense), TAGTTTAGGGTTAGTTAGGTTGCGT (methylated
sense), TAACCCTAAACTAATTCCCTTCCA (unmethylated antisense),
AAATATCGACCGAAAATAAAAACG (methylated antisense). And PCR
amplification was conducted with primers that specifically amplify
methylated or unmethylated DNA using an EpiTect MSP kit (Qiagen).
PCR was performed as following thermal conditions: 1 cycle of 95˚C
for 5 min and 35 cycle of 94˚C for 45 sec, 56˚C (Unmethylation) or
57.5˚C (Methylation) for 30 sec, and 72˚C for 30 sec, and then one
cycle of 72˚C for 10 min. Each amplified product was loaded onto 2%
agarose gels, visualized using ethidium bromide, and images were
captured.
Statistical analysis
For statistical comparisons, P-values were
determined using unpaired Student's t-test or one-way ANOVA.
P<0.05 was considered to indicate a statistically significant
difference.
Results
CD47 expression and phagocytosis is
correlated with TTP expression in radioresistant HNC cell line
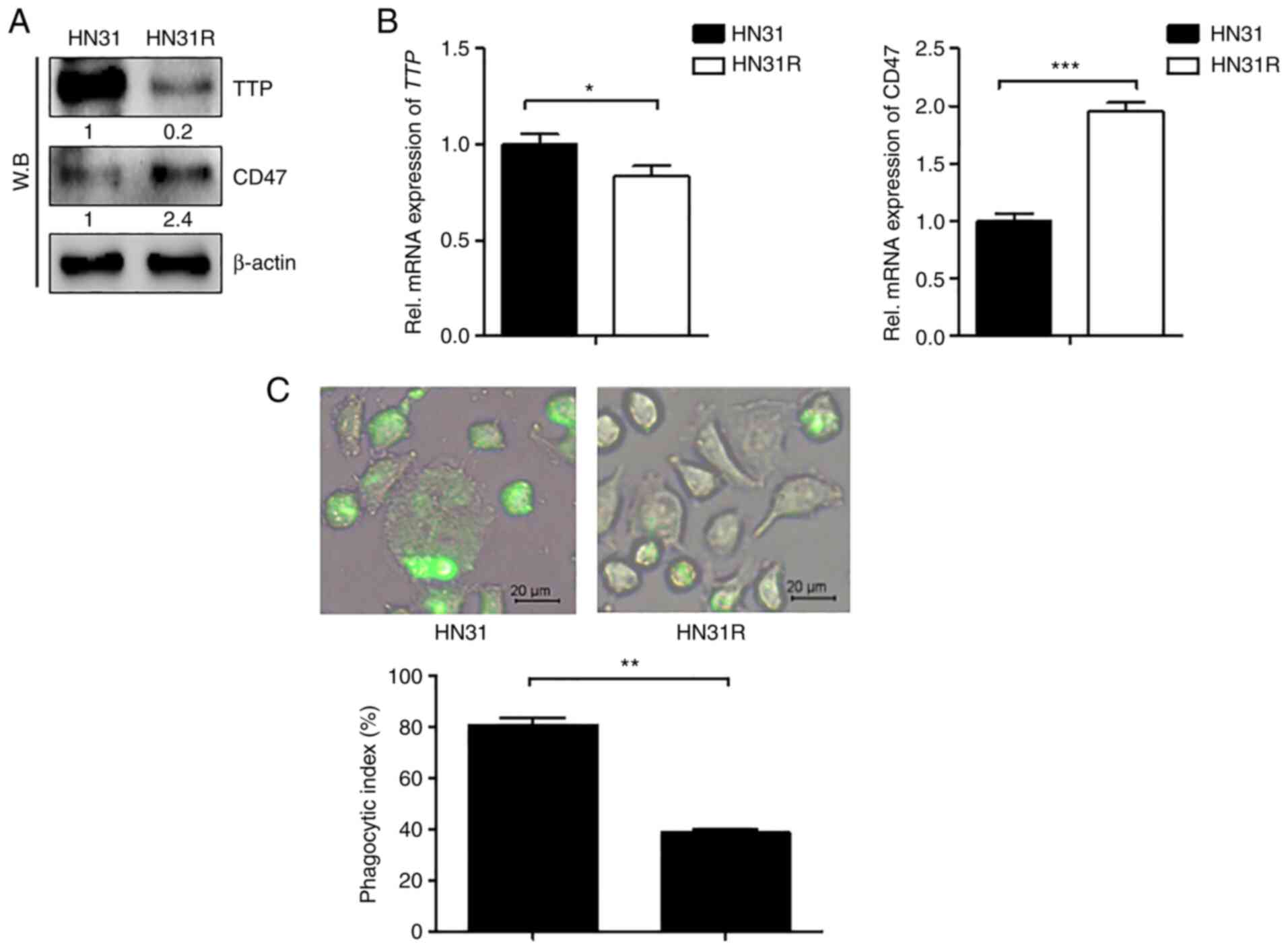
TTP and CD47 expression levels were first examined
by RT-PCR and western blot analysis in HN31 and HN31R cells. TTP
levels were high in HN31 cells, but low in the radioresistant HN31R
cell line. In contrast, CD47 levels were low in HN31 cells compared
with that in the HN31R cell line (Fig.
1A and 1B). We next determined
whether CD47 phagocytosis is mediated by CD47 expression in HN31
and HN31R cells. In HN31R with CD47 overexpression, phagocytosis
was inhibited compared with that in the HN31 cell line (Fig. 1C).
TTP decreases expression of CD47 mRNA
and increases phagocytosis in radioresistant HNC cell line
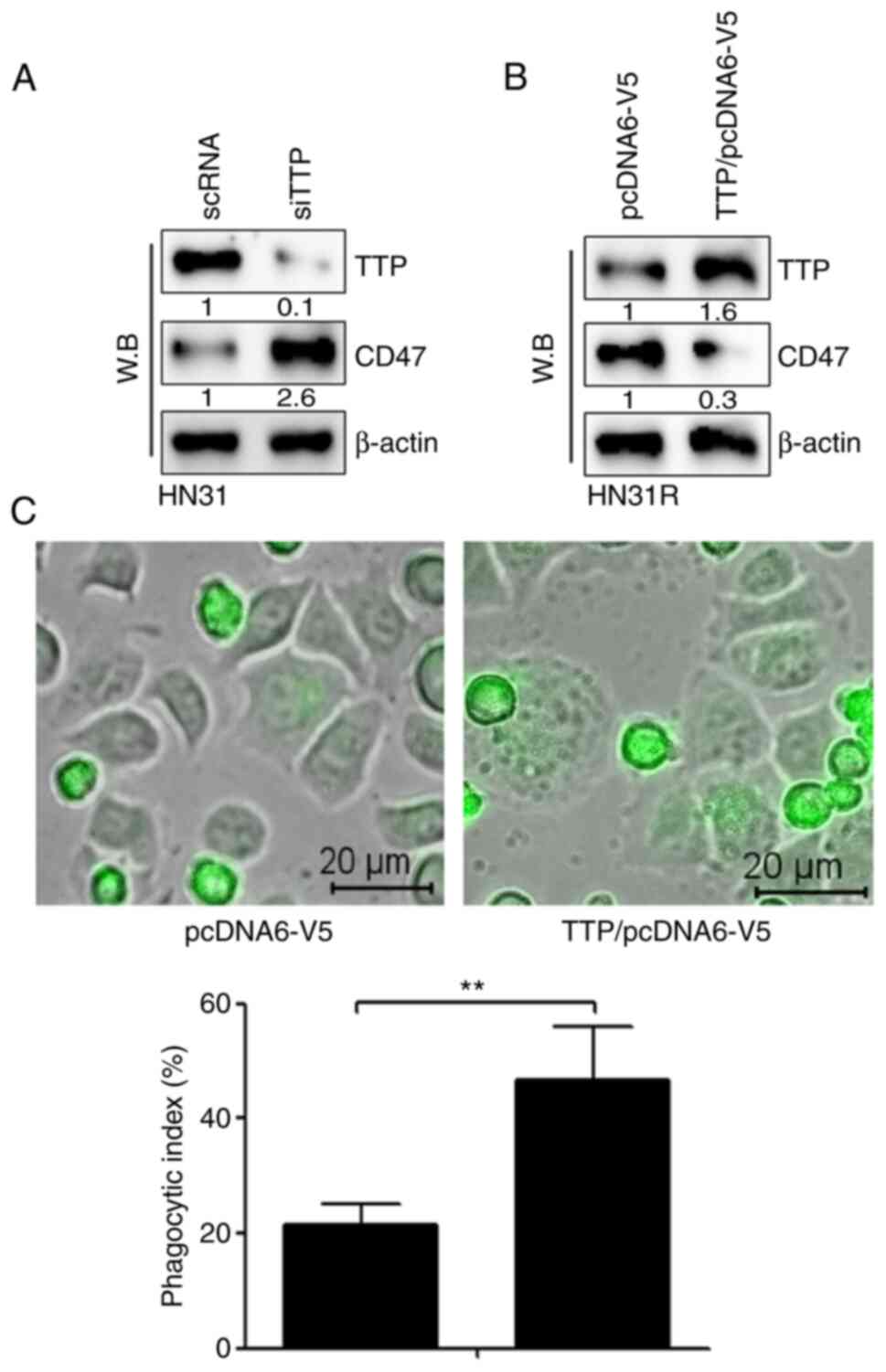
We investigated whether silencing or overexpression
of TTP regulates CD47 expression in HN31 and HN31R cells. TTP
silencing by siRNA increased the levels of CD47 protein in HN31
cells (Fig. 2A). When TTP was
expressed in HN31R cells by transfection of TTP significantly
inhibited the level of CD47 protein (Fig. 2B). To identify the effect on
phagocytosis, a phagocytosis assay was performed following TTP
overexpression in HN31R cells. The results indicated that the CD47
suppression-mediated phagocytosis index increased significantly
after TTP overexpression (Fig.
2C).
TTP interacts to ARE 9 in the 3'UTR of
CD47 mRNA and increases CD47 mRNA degradation
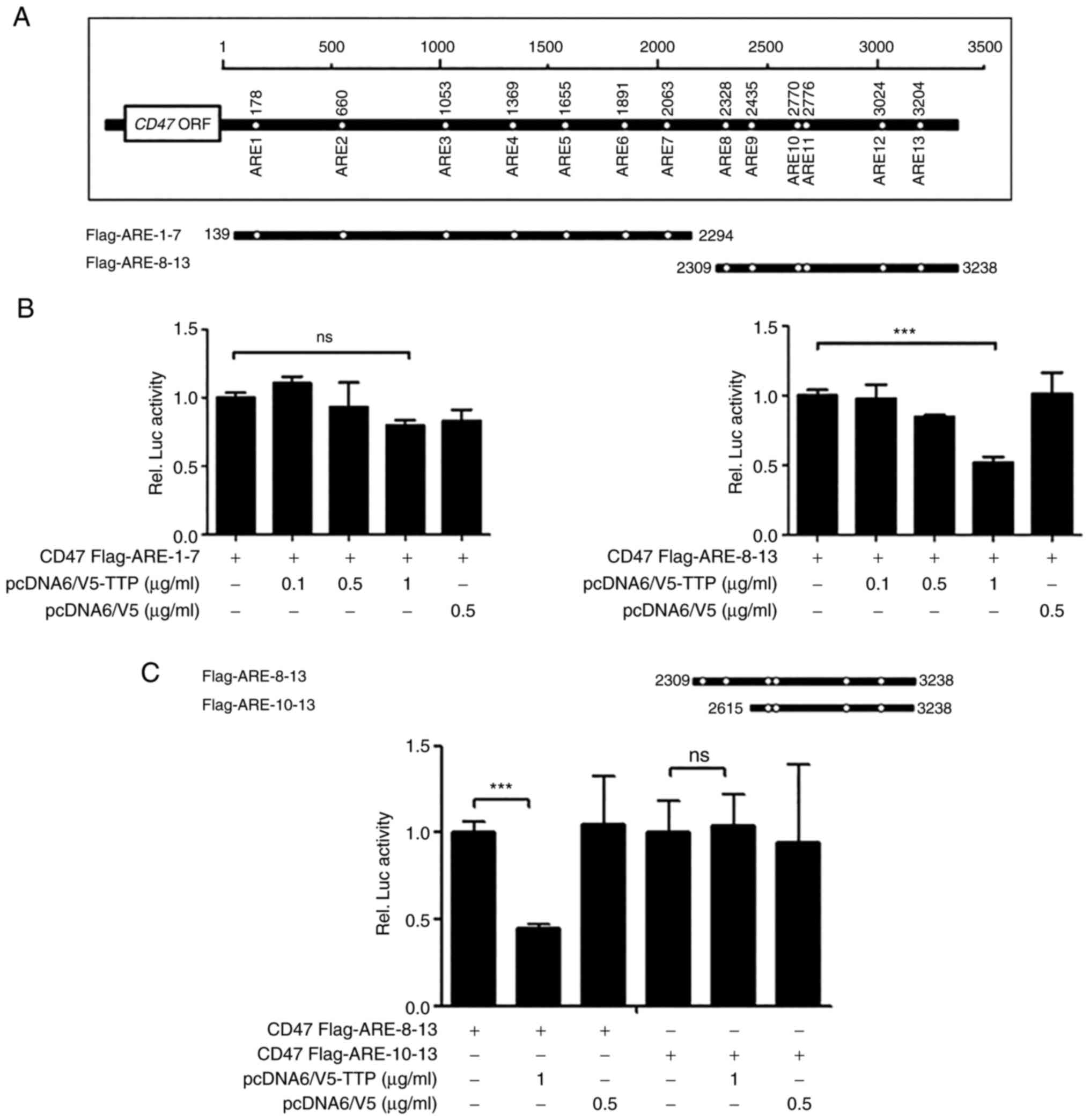
Human CD47 3'UTR has the presence of thirteen AREs
(Fig. 3A). To investigate whether
suppression of CD47 expression by TTP was mediated through
interaction in the 3'UTR of CD47 mRNA, luciferase reporter gene
linked to the full-length CD47 3'UTR divided into two constructs
(Flag AREs 1-7 and Flag AREs 8-13) in the psiCHECK2 plasmid was
used. Next, we investigated which AREs within the CD47 3'UTR were
necessary for TTP activity. A luciferase reporter gene linked to
oligonucleotides containing Flag AREs 1-7 and AREs 8-13 within the
CD47 3'UTR were prepared using the psiCHECK2 plasmid. Whereas the
luciferase activity of Flag AREs 1-7 was not changed by TTP
expression, that of Flag AREs 8-13 was significantly inhibited
(Fig. 3B). We then subdivided Flag
AREs 8-13 further to prepare a Flag AREs 10-13 construct and
measured luciferase activity of CD47 by TTP. Because the luciferase
activity of Flag AREs 10-13 was not affected by TTP expression, we
concluded that TTP binds to ARE 8-9 in the CD47 mRNA 3'UTR
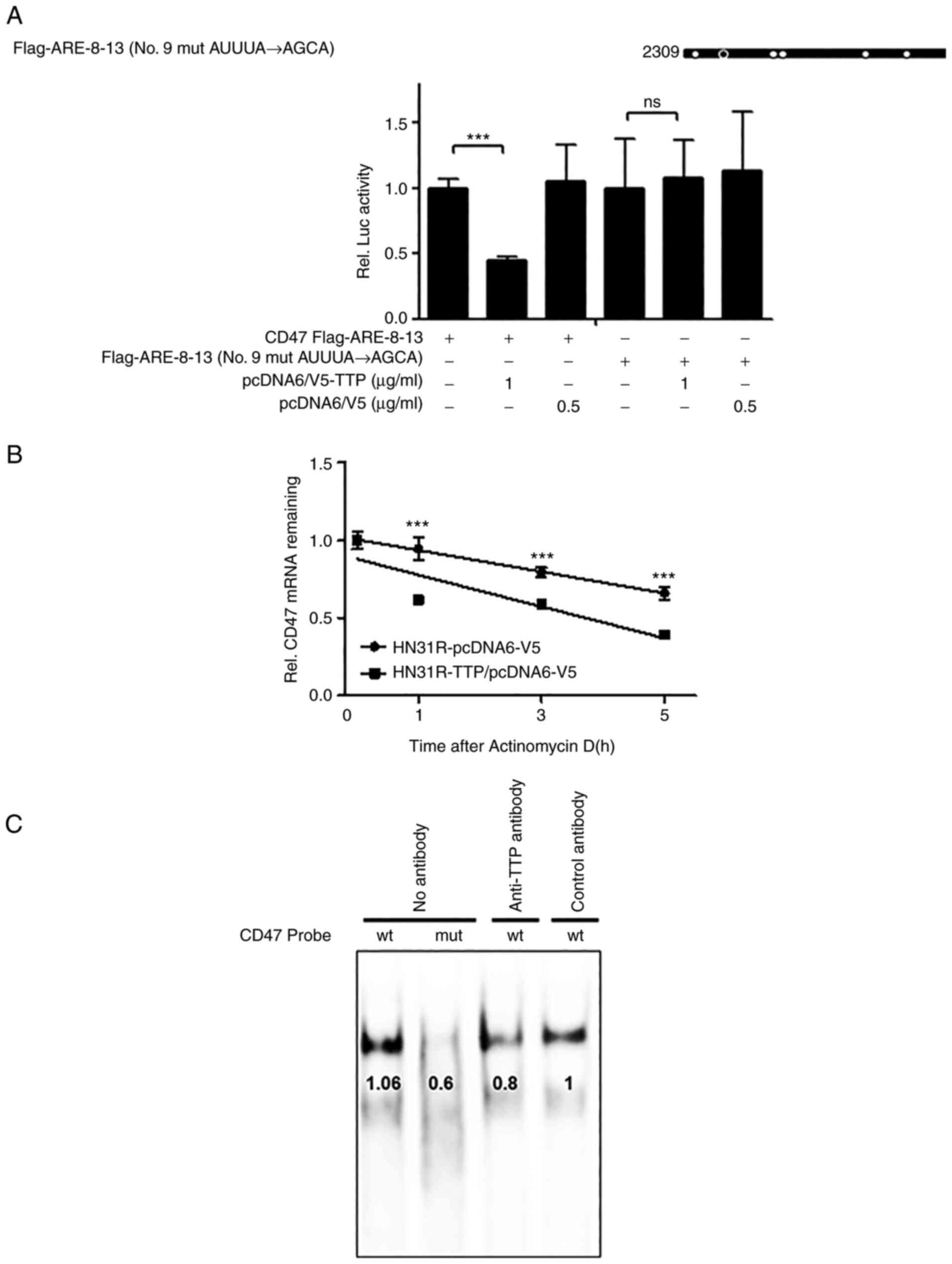
(Fig. 3C). Because AREs 8-9 was
closely located in CD47, AREs 8-13 with single mutation in the ARE
9 motif (AUUUA→AGCA) were used to confirm whether ARE 9 was
responsible for the TTP binding (Fig.
4A). A single ARE 9 mutant in CD47 was prevented the TTP
inhibitory effect compared with the full ARE 8-13 construct.
Although these results were determined using overexpressed TTP
protein ectopically, the significance of CD47 ARE 9 for TTP binding
was demonstrated. Then, to investigate if suppression of CD47 by
TTP resulted from CD47 mRNA stability, the half-life of the mRNA
was estimated by qRT-PCR. After the transfection with pcDNA6/V5-TTP
(HN31R/TTP) or the pcDNA6/V5 control vector (HN31R/pcDNA), the
half-life of TTP overexpressing CD47/TTP cells was significantly
shorter compared with control HN31R/pcDNA cells in actinomycin D
treatment (Fig. 4B). To confirm
the association between endogenous TTP and ARE in the CD47 3'UTR,
RNA EMSA was performed with a biotinylated RNA probe containing a
wild-type or mutant ARE9 of CD47. Cytoplasmic extracts which
prepared from TTP transfection HN31R cells were incubated with the
biotinylated RNA. When the wild-type CD47 ARE 9 probe was mixed
with the cytoplasmic extracts of TTP transfection HN31R cells, we
found a dominant probe-protein complex (Fig. 4C). However, the mutant CD47 ARE 9
probe s could not make the probe-protein complex. When the reaction
mixture was preincubated with anti-TTP antibody, the formation of
the CD47 ARE 9 probe-protein complex was reduced but not with the
control. These results indicate that TTP can combine at the 9th ARE
of CD47 and enhances decay of CD47 mRNA.
Sustained TTP suppression and CD47
activation is maintained through DNA methylation in radioresistant
HNC cell lines
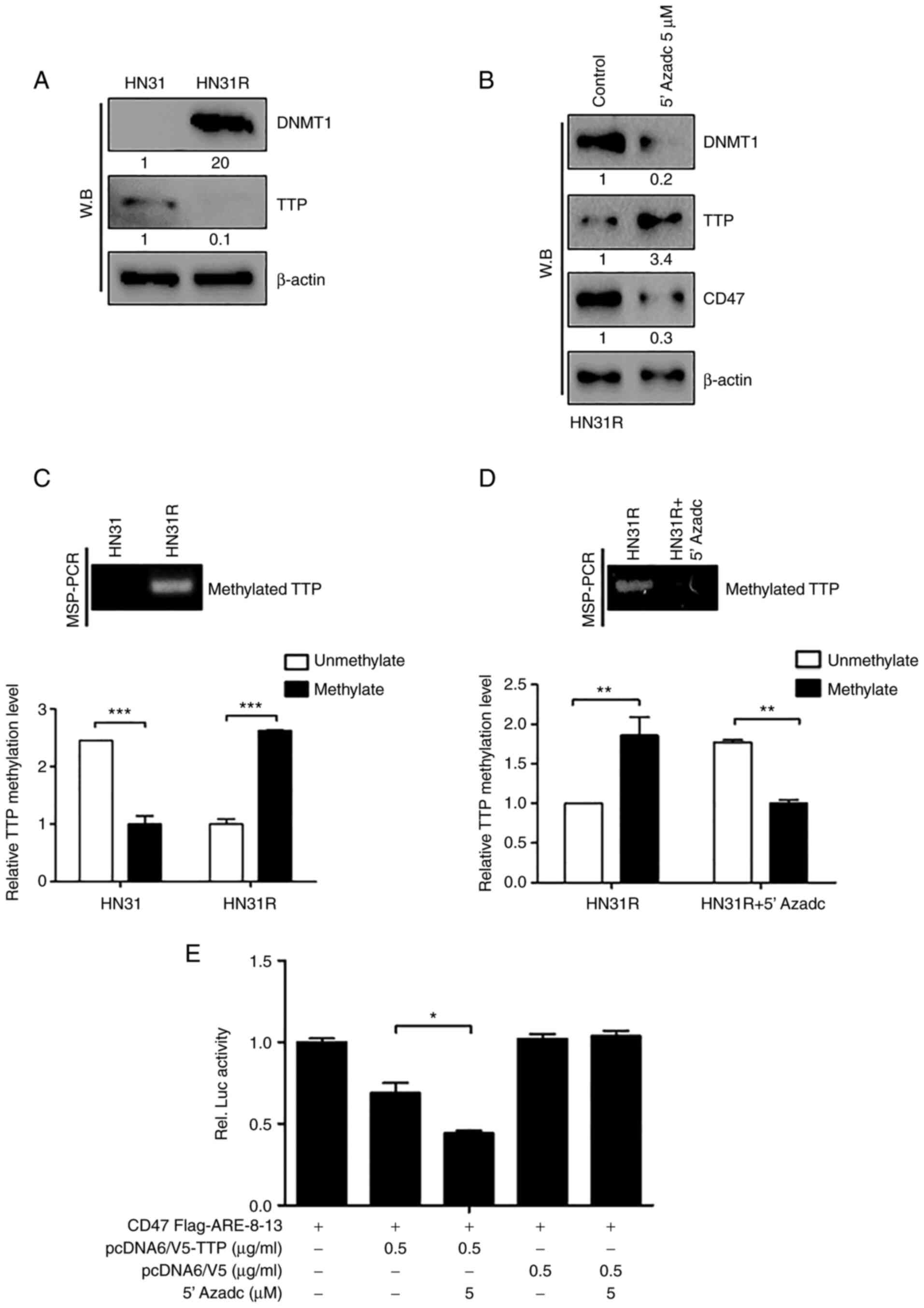
Based on our previous study in which DNMT1 (DNA
methyltransferase) was found to be overexpressed in radioresistant
HNC (10), we examined the
regulation of TTP by DNA methylation in radioresistant HNC cells.
DNMT1 expression was increased significantly in HN31R cells
compared with parent HN31 cells (Fig.
5A). To determine the DNA methylation of TTP by DNMT1 in HN31R
cells, 2 successive days with 5 µM 5-AZAdC (DNA demethylating
agent) was treated to HN31R cells and the protein level of TTP and
CD47 protein was checked in HN3R cells using Western blotting. When
DNMT1 protein in whole-cell lysates was reduced, TTP expression was
increased significantly with decreased CD47 expression at the
protein level (Fig. 5B).
To determine change of TTP expression by the DNA
methylation effect we performed an MSP assay. Basically, HN31 cells
showed unmethylation status of the TTP promoter, however, HN31R
cells aberrant, hypermethylated DNA in this region. (Fig. 5C). To confirm the regulation of TTP
by DNMT1 in HN31R cells, MSP was performed after 5 µM 5-AZAdC on
HN31R cells. Following treatment with 5-AZAdC, TTP methylation was
decreased (Fig. 5D). These results
suggest that TTP is suppressed by DNA methylation in radioresistant
HNC cells.
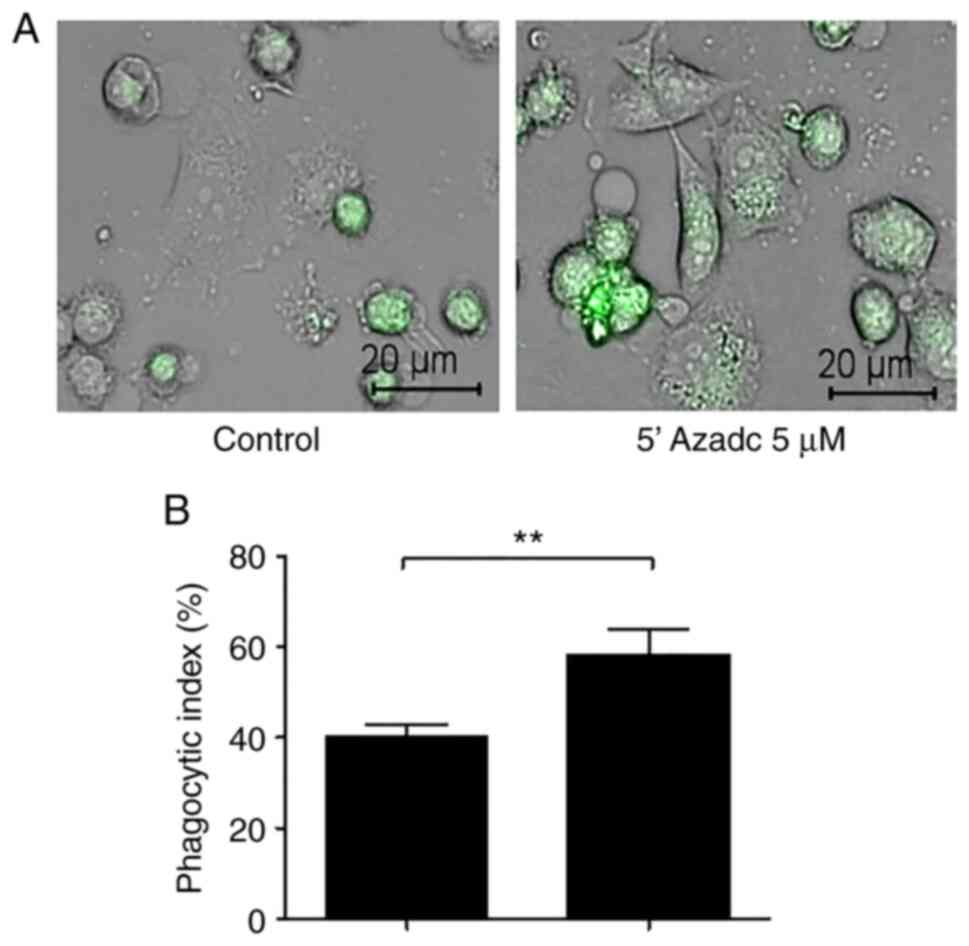
We confirmed whether DNMT1-mediated DNA methylation
of TTP could regulate binding with CD47 AREs using a luciferase
activity and DMNT1 inhibition could induce phagocytosis After
treatment with 5-AZAdC, the activity of CD47 AREs 8-13
significantly decreased compared with that of the control through
TTP expression (Fig. 5E). And
following treatment with 5-AZAdC, we identified the significant
increase of phagocytosis (Fig. 6A
and B). These findings suggest
that TTP suppression by DNMT1-mediated DNA methylation maintains
sustained CD47 activation in radioresistant HNC cells.
Additionally, we investigated the CD47 related
signal pathway in radioresistant HNC. We investigated the
relationship of EphA3, CD47 and AKT activation, mediate tumor
aggressiveness and radioresistance based on previous our study
(18). We found that CD47
silencing decreased phosphor-AKT expression on western blot
(Fig. S1). And we assessed which
EphA3 could regulate CD47 and phosphor-AKT expression. The decrease
of CD47 and phosphor-AKT was detected following EphA3 silencing
compared to that in the control cells. These results suggest that
CD47 antibody may have dual effect in increase of phagocytosis and
suppression of AKT activation although these results are
preliminary data in radioresistant HNC.
Discussion
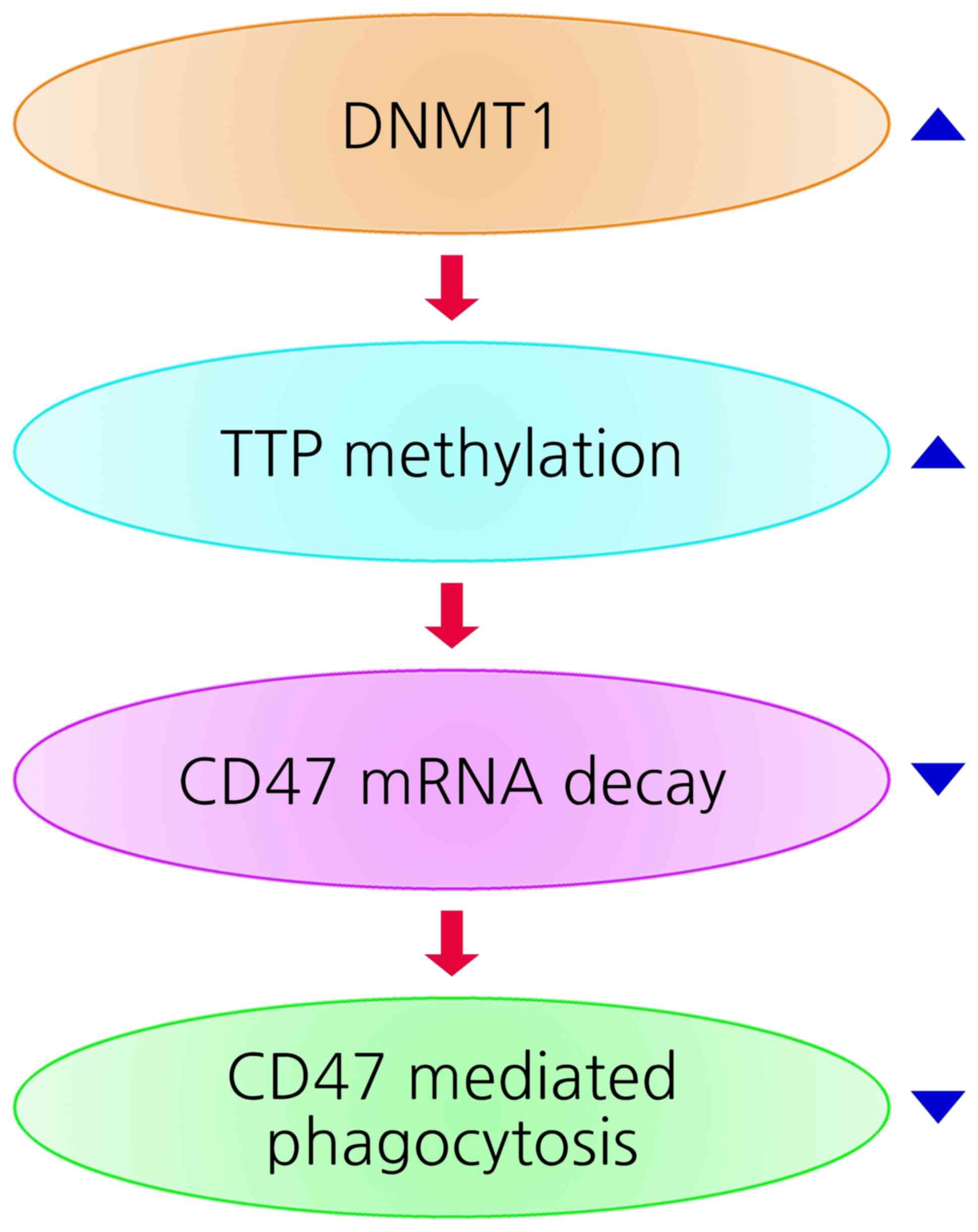
In this study, we demonstrated that DNMT1 suppressed
TTP expression through DNA methylation in radioresistant HNC cells,
which in turn, prevented binding to the ARE within the CD47 3'UTR
and inhibited CD47 mRNA decay. Thus, up-regulation of TTP can
induce CD47 mRNA degradation and increase phagocytosis in
radioresistant HNC cells.
It was known that the overexpression of TTP can
induce inhibition of tumor growth, implicating TTP as a tumor
suppressor (8). Specifically, TTP
can regulate the posttranscriptional regulation of various
inflammatory mediators and immune gene expression thus exert
anti-cancer effects (8,17,21).
Based on these findings, we studied the role of TTP in CD47
expression. In previous study, it was known that NF-κB and
Hypoxia-inducible factor-1 (HIF-1) can regulate CD47 expression by
binding to at transcription level (22,23).
However, little is known about the regulation of CD47 expression
through ARE motifs present in 3'UTR of mRNA,
post-transcriptionally. We discovered that the CD47 3'UTR contained
AREs and overexpression of TTP enhanced degradation of CD47 mRNA
through ARE binding in HNC cells, in turn increased phagocytosis.
Moreover, we demonstrated that TTP targeted CD47 directly by
binding to the ARE flag 9 of CD47 mRNA, and CD47 expression was
downregulated by TTP. Our results also indicated that TTP enhances
phagocytosis through repression of CD47. To our knowledge, this is
the first report suggesting the regulation of CD47 expression
mediated by TTP post-transcriptionally.
Currently, several CD47-blocking antibodies are
being investigated in clinical trials, alone or as combination
therapy (5,24-26).
However, the clinical limitation of current CD47-blocking
antibodies is the expression of CD47 on normal cells such as
myeloid cells which forms a ‘antigen sink’ that may restrict
sufficient antibody acceleration at therapeutic sites (26,27).
Thus, combination therapy with SIRPα-blocking agents or other
target therapeutic agents can help a smaller antigen sink.
Combination with TTP overexpression agents can help to reduce
antigen sink of CD47 antibody, but currently, there is no drugs
which can induce TTP overexpression. These findings suggest that
TTP has important role in development of radioresistance in HNC and
as biomarker to predict efficacy of CD47 antibody in recurrent HNC
patients after radiation therapy.
Recently, one open-label, multicenter, phase 1 study
with evorpacept (CD47 antibody) in advanced solid tumors including
HNC showed a favorable safety with stable disease control (27). Evorpacept is being studied in
combination with other drugs for both solid and hematological
malignancies and can be a new approach to CD47 targeted therapies
in advanced or recurrent HNC.
Finally, we investigated the mechanism of TTP
suppression in radioresistant HNC cells. A various signaling
pathways have been reported which regulate TTP expression at the
transcription, post-transcriptional, or post-translational levels
(11). Here, we demonstrated that
TTP can be regulated epigenetically. Previously, we reported DNMT1
overexpression in radioresistant HNC (18) and found that TTP suppression was
regulated by DNA methylation through DNMT1 overexpression in
radioresistant HNC cells Our findings suggest a model (Fig. 7) in which suppression of CD47 mRNA
decay through DNMT1-mediated TTP methylation induces sustained CD47
activation and inhibition of phagocytosis in radioresistant HNC.
Thus, the present study demonstrates a previously unrecognized CD47
mRNA regulation by TTP in radioresistant HNC. The relationship of
EphA3 and CD47/Akt pathway remains unclear in radioresistance. Our
results indicate that EphA3 may regulate the CD47 and AKT signaling
pathway but, further studies are needed to analyze the exact
association in the signaling pathway, additionally.
In conclusion, we demonstrated that TTP could
regulate CD47 gene expression in HNC, post-transcriptionally. We
discovered that TTP could decay its mRNA by binding to the 9th ARE
of the CD47 mRNA. As a result, TTP-mediated suppression of CD47
results in increased phagocytosis. TTP suppression by DNA
methylation mediates sustained CD47 activation in radioresistant
HNC. These findings suggest that TTP has important role in
development of radioresistance in HNC. Our findings provide novel
insight into role as biomarker of TTP to predict efficacy of CD47
antibody in recurrent HNC patients after radiation therapy.
Supplementary Material
EphA3-CD47-Akt signaling pathway may
induce radioresistance in HNC. (A) p-AKT expression was
investigated after CD47-silencing in the HN31R cell line for
identification of relationship of CD47 and AKT using western
blotting. (B) CD47 and p-AKT expression was assessed after
EphA3-silencing using western blotting in HN31R cell line for the
investigation of EphA3/CD47/p-AKT signaling pathway. p-,
phosphorylated; HNC, head and neck cancer; scRNA, small conditional
RNA; si, small interfering; EphA3, EPH receptor A3.
Acknowledgements
Not applicable.
Funding
Funding: This work was supported by the National Research
Foundation (NRF) grant funded by the Korea government (MSIT grant
nos. MRC-2018R1A5A2020732, NRF-2020R1A2C1011879,
NRF-2019R1A2C1006788 and NRF-2021R1A2C1010046) and Ulsan University
Hospital Research Grant (grant no. UUH -2020-06).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SHK, WHL and HJC made substantial contributions to
conception and design of experiments, and to the acquisition,
analysis and interpretation of data. JHA and HWC made substantial
contributions to the design of experiments, and to the acquisition,
analysis and interpretation of data. TKK made substantial
contributions to acquisition, analysis and interpretation of data.
MWH made substantial contributions to conception and design of
experiments, the acquisition, analysis and interpretation of data
and drafted and revised the manuscript critically for important
intellectual content. SYK and SWK made substantial contributions to
conception and design of experiments, the analysis and
interpretation of data and revised the manuscript critically for
important intellectual content. All authors read and approved the
final manuscript. MWH, SYK, SHK and WHL confirm the authenticity of
the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ozpiskin OM, Zhang L and Li JJ: Immune
targets in the tumor microenvironment treated by radiotherapy.
Theranostics. 9:1215–1231. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Shi L, Wang X, Hu B, Wang D and Ren Z:
miR-222 enhances radiosensitivity of cancer cells by inhibiting the
expression of CD47. Int J Clin Exp Pathol. 12:4204–4213.
2019.PubMed/NCBI
|
|
3
|
Vermeer DW, Spanos WC, Vermeer PD, Bruns
AM, Lee KM and Lee JH: Radiation-induced loss of cell surface CD47
enhances immune-mediated clearance of human papillomavirus-positive
cancer. Int J Cancer. 133:120–129. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tong B and Wang M: CD47 is a novel potent
immunotherapy target in human malignancies: Current studies and
future promises. Future Oncol. 14:2179–2188. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhang J, Jin S, Guo X and Qian W:
Targeting the CD47-SIRPα signaling axis: Current studies on B-cell
lymphoma immunotherapy. J Int Med Res. 46:4418–4426.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sun J, Muz B, Alhallak K, Markovic M,
Gurley S, Wang Z, Guenthner N, Wasden K, Fiala M, King J, et al:
Targeting CD47 as a novel immunotherapy for multiple myeloma.
Cancers (Basel). 12(305)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Miller TW, Soto-Pantoja DR, Schwartz AL,
Sipes JM, DeGraff WG, Ridnour LA, Wink DA and Roberts DD: CD47
receptor globally regulates metabolic pathways that control
resistance to ionizing radiation. J Biol Chem. 290:24858–24874.
2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Brooks SA and Blackshear PJ:
Tristetraprolin (TTP): Interactions with mRNA and proteins, and
current thoughts on mechanisms of action. Biochim Biophys Acta.
1829:666–679. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lee WH, Han MW, Kim SH, Seong D, An JH,
Chang HW, Kim SY, Kim SW and Lee JC: Tristetraprolin
posttranscriptionally downregulates TRAIL death receptors. Cells.
9(1851)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ross CR, Brennan-Laun SE and Wilson GM:
Tristetraprolin: Roles in cancer and senescence. Ageing Res Rev.
11:473–484. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sanduja S, Blanco FF, Young LE, Kaza V and
Dixon DA: The role of tristetraprolin in cancer and inflammation.
Front Biosci (Landmark Ed). 17:174–188. 2012.PubMed/NCBI View
Article : Google Scholar
|
|
12
|
Park JM, Lee TH and Kang TH: Roles of
tristetraprolin in tumorigenesis. Int J Mol Sci.
19(3384)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zhang D, Zhou Z, Yang R, Zhang S, Zhang B,
Tan Y, Chen L, Li T and Tu J: Tristetraprolin, a potential
safeguard against carcinoma: Role in the tumor microenvironment.
Front Oncol. 11(632189)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Jiang W, Zhu D, Wang C and Zhu Y: Tumor
suppressing effects of tristetraprolin and its small
double-stranded RNAs in bladder cancer. Cancer Med. 10:269–285.
2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lee HH, Yang SS, Vo MT, Cho WJ, Lee BJ,
Leem SH, Lee SH, Cha HJ and Park JW: Tristetraprolin down-regulates
IL-23 expression in colon cancer cells. Mol Cells. 36:571–576.
2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Deng K, Wang H, Shan T, Chen Y, Zhou H,
Zhao Q and Xia J: Tristetraprolin inhibits gastric cancer
progression through suppression of IL-33. Sci Rep.
6(24505)2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wang Q, Ning H, Peng H, Wei L, Hou R, Hoft
DF and Liu J: Tristetraprolin inhibits macrophage IL-27-induced
activation of antitumour cytotoxic T cell responses. Nat Commun.
8(867)2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kim SH, Kang BC, Seong D, Lee WH, An JH,
Je HU, Cha HJ, Chang HW, Kim SY, Kim SW and Han MW: EPHA3
contributes to epigenetic suppression of PTEN in radioresistant
head and neck cancer. Biomolecules. 11(599)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kim SH, Lee WH, Kim SW, Je HU, Lee JC,
Chang HW, Kim YM, Kim K, Kim SY and Han MW: EphA3 maintains
radioresistance in head and neck cancers through epithelial
mesenchymal transition. Cell Signal. 47:122–130. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lee JC, Lee WH, Min YJ, Cha HJ, Han MW,
Chang HW, Kim SA, Choi SH, Kim SW and Kim SY: Development of TRAIL
resistance by radiation-induced hypermethylation of DR4 CpG island
in recurrent laryngeal squamous cell carcinoma. Int J Radiat Oncol
Biol Phys. 88:1203–1211. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Tu Y, Wu X, Yu F, Dang J, Wang J, Wei Y,
Cai Z, Zhou Z, Liao W, Li L and Zhang Y: Tristetraprolin
specifically regulates the expression and alternative splicing of
immune response genes in HeLa cells. BMC Immunol.
20(13)2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Betancur PA, Abraham BJ, Yiu YY,
Willingham SB, Khameneh F, Zarnegar M, Kuo AH, McKenna K, Kojima Y,
Leeper NJ, et al: A CD47-associated super-enhancer links
pro-inflammatory signalling to CD47 upregulation in breast cancer.
Nat Commun. 8(14802)2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zhang H, Lu H, Xiang L, Bullen JW, Zhang
C, Samanta D, Gilkes DM, He J and Semenza GL: HIF-1 regulates CD47
expression in breast cancer cells to promote evasion of
phagocytosis and maintenance of cancer stem cells. Proc Natl Acad
Sci USA. 112:E6215–E6223. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Liu J, Xavy S, Mihardja S, Chen S,
Sompalli K, Feng D, Choi T, Agoram B, Majeti R, Weissman IL and
Volkmer JP: Targeting macrophage checkpoint inhibitor SIRPα for
anticancer therapy. JCI Insight. 5(e134728)2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Hendriks M, Ploeg EM, Koopmans I, Britsch
I, Ke X, Samplonius DF and Helfrich W: Bispecific antibody approach
for EGFR-directed blockade of the CD47-SIRPα ‘don't eat me’ immune
checkpoint promotes neutrophil-mediated trogoptosis and enhances
antigen cross-presentation. Oncoimmunology.
9(1824323)2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Veillette A and Chen J: SIRPα-CD47 immune
checkpoint blockade in anticancer therapy. Trends Immunol.
39:173–184. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Lakhani NJ, Chow LQM, Gainor JF, LoRusso
P, Lee KW, Chung HC, Lee J, Bang YJ, Hodi FS, Kim WS, et al:
Evorpacept alone and in combination with pembrolizumab or
trastuzumab in patients with advanced solid tumours (ASPEN-01): A
first-in-human, open-label, multicentre, phase 1 dose-escalation
and dose-expansion study. Lancet Oncol. 22:1740–1751.
2021.PubMed/NCBI View Article : Google Scholar
|