1. Introduction
The removal of one entire lung-pneumonectomy-is not
a surgical decision to be taken lightly. Although technically
considered the simplest anatomical resection, its high mortality
[10-60% (1)] and difficulty to
manage possible post-operative complications warrant careful
selection of eligible cases.
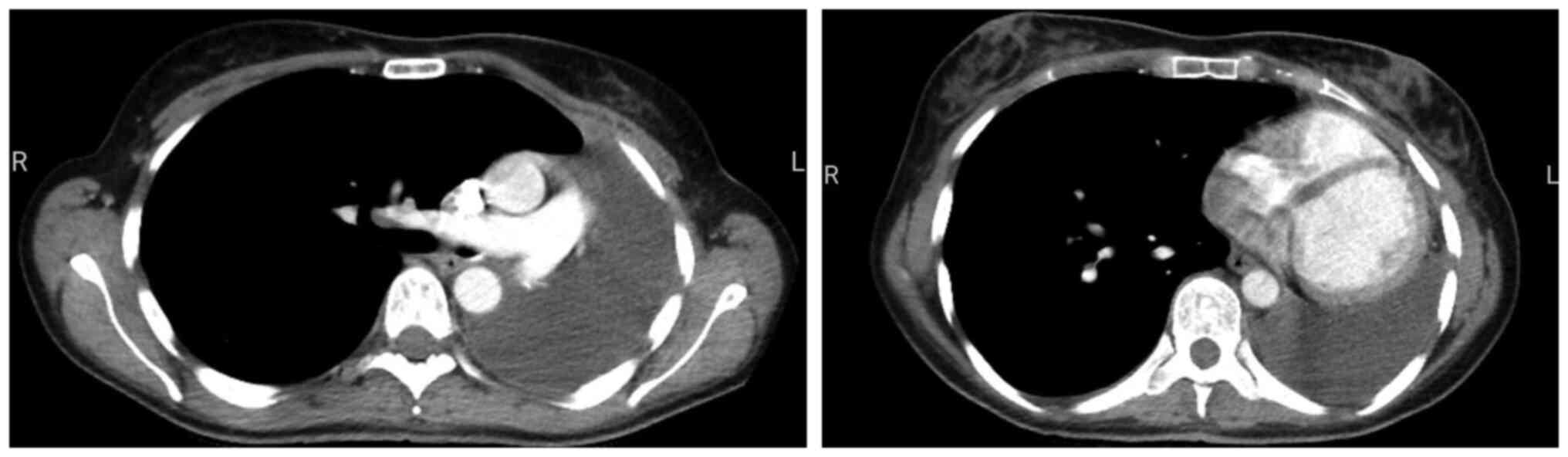
As it is the only type of pulmonary resection that
leaves the entire pleural cavity empty, specific changes are
expected after pneumonectomy. Typically, after surgery, the empty
space is filled with air, which is then gradually replaced by
fluid. Then, in a course of 1-7 months (2), the pleural cavity should be entirely
obliterated. Obviously, these changes also have an anatomic impact,
such as the rise of the diaphragm and the shift of the mediastinum
towards the empty cavity, also narrowing the intercostal spaces on
the same side (Fig. 1).
Although patients eligible for pneumonectomy undergo
a rigorous workup prior to surgery, certain post-operative
complications still do occur. Complications may occur more
frequently when oncological elective surgeries are delayed or even
cancelled, e.g., due to associated comorbidities or due to the
COVID-19 pandemic (3-5).
As for the post-operative management of any other
type of pulmonary anatomical resection, the standard cautions and
care apply when it comes to pneumonectomies, but there are specific
post-operative complications that the patient must be monitored
for: post-pneumonectomy empyema, post-pneumonectomy pulmonary
oedema and post-pneumonectomy syndrome (1), followed by other more or less
frequent complications (1,6,7) that
are outlined in Table I,
stratified by acute or chronic state.
 | Table IMost common complications after
pneumonectomy (6,7). |
Table I
Most common complications after
pneumonectomy (6,7).
| Type | Items |
|---|
| Acute
complications | Early bronchopleural
fistula |
| | Cardiac
herniation |
| | Haemorrhage |
| | Early empyema |
| | Chylothorax |
| | Pulmonary edema |
| | Pneumonia |
| | Acute lung
injury |
| Chronic
complications | Tumor recurrence |
| | Late on-set
empyema |
| | Postpneumonectomy
syndrome |
| | Late bronchopleural
fistula |
| Other common
complications | Intrathoracic
transdiaphragmatic |
| | herniation after
extrapleural |
| | pneumonectomy |
| | Cardiovascular
complications: |
| | Arrythmias,
myocardial infarction, acute heart failure |
| | Pulmonary
embolism |
| | Vocal cord paralysis
(permanent or transitory) |
| | Cor
pulmonale |
2. Methodology of the review
Search strategy
Search strategy and selection criteria: All of the
available studies were searched on PubMed (pubmed.ncbi.nlm.nih.gov) and MedLine (lwwreprints.ovidds.com/?utm_source=google&utm_medium=paidsearch&utm_campaign=2022-ga-las-rd-reprints-portal&gclid=CjwKCAjwtIaVBhBkEiwAsr7-c8oqHpC-9zEiptQ4xQxiCUAsMK-gmcSQ5fDQY3YNXkD8XslYfiSMOxoCSj4QAvD_BwE).
Case reports and studies on the chosen topic were retrieved using
different combinations of the following key words: tension,
hypertensive, hypertension, hydrothorax, haemothorax, pneumothorax,
chylothorax, pneumonectomy, lung cancer, lung malignancy, and
mesothelioma. No language restrictions were applied to the search.
Cases regarding pneumonectomies for lung malignancy (carcinoma,
sarcoma, mesothelioma) were included, while cases of traumatic
tension pneumothorax or another non-neoplastic disease, such as
dialysis-related or traumatic haemothorax, were excluded. The
publication dates were set from inception until April 2021. The
search was performed between May and August 2021 by authors VM and
MN, independently.
Study screening and selection
After a rigorous search, a total of 19 case reports
that matched the selection criteria were identified (2,8-20).
Of these cases, 18 were with liquid in tension and 1 with air in
tension into the post-pneumonectomy space, all after pneumonectomy
for malignancy, as presented in Table
II. As mentioned above, those cases that had pneumonectomy for
other reasons than malignancy and patients that had a complication
after pneumonectomy on the contralateral side were excluded.
 | Table IICases screened in literature matching
the review criteria, presented according to the type of tensioned
fluid from the post-pneumonectomy space. |
Table II
Cases screened in literature matching
the review criteria, presented according to the type of tensioned
fluid from the post-pneumonectomy space.
| Nr. crt | Author (year) | Initial
diagnosis | Right/ left lung | Type of surgery | Time between surgery
and complication (number of post-operative time units) | Time of
complication | Sex | Pleural fluid | First management | Analysis of pleural
liquid | Definitive
management | Known follow-up | (Refs.) |
|---|
| 1 | Ammori (2006) | Lung squamous cell
carcinoma T2N1M0) | Right | Intrapleural
extrapericardial pneumonectomy | 14 days | Tension
chylothorax | M | Chyle | Diagnosys
thoracentesis | N/A | Surgery-mass ligation
of the thoracic duct at the level of the diaphragm | No recurrence | (8) |
| 2 | Coco (2020) | Adenocarcinoma | Left | Intrapleural
extrapericardial pneumonectomy | 48 h | Tension chylothorax
Tension | F | Chyle | Evacuatory
thoracentesis | 1,922 leu/µl, trgly
825 mg/dl, chol 83 mg/dl | Chest drain | No recurrence | (9) |
| 3 | Hemang (2014) | Lung squamous cell
carcinoma (st.IIB T2N1M0) | Right | Intrapleural
extrapericardial pneumonectomy | 9 days | chylothorax | F | Chyle | Chest drain | Milky white, trgly
1,729 mg/dl | First case without
duct ligation: Pigtail catheter, daily instillation of antibiotic
solution (gentamicin/ polymixin B) | Day 13 pigtail
catheter removed | (10) |
| 4 | Huwer (1991) | N/A | Left | Intrapleural
extrapericardial pneumonectomy | Between the 5th and
the 8th day | Tension
chylothorax | N/A | Chyle | Chest drain | N/a | Surgery-ductal
ligature | N/A | (11) |
| 5 | Huwer (1991) | N/A | Left | Intrapleural
extrapericardial pneumonectomy | Between the 5th and
the 8th day | Tension
chylothorax | N/A | Chyle | Surgery | N/a | Surgery-ductal
ligature | N/A | (11) |
| 6 | Van Mulders
(1984) | Lung squamous cell
carcinoma | Left | Intrapleural
extrapericardial pneumonectomy | 4 days | Tension
chylothorax | M | Chyle | Evacuatory
thoracentesis | Trgly 387 mg/dl,
LDH 176, chol 46 mg/100 ml | Surgery-ductal
ligature | 3 days post-
discharge from ICU | (12) |
| 7 | Sarsam (1994) | Primary lung
cancer | Left | Intrapleural
extrapericardial pneumonectomy | Between the 5th and
the 6th day | Tension
chylothorax | N/A | Chyle | Chest drain | Chyle | Reinsertion of the
chest drain. Surgery-direct suturing of the leak site | No recurrence | (13) |
| 8 | Sarsam (1994) | Primary lung
cancer | Left | Intrapleural
intrapericardial pneumonectomy | Between the 5th and
the 6th day | Tension
chylothorax | N/A | Chyle | Surgery-ductal
ligature-below the aortic arch, posterior to the bronchial suture
line | Chyle | Surgery-ductal
ligature-below the aortic arch, posterior to the bronchial suture
line | No recurrence | (13) |
| 9 | Sarsam (1994) | Primary lung
cancer | Right | Intrapleural
Extrapericardial pneumonectomy | Between the 5th and
the 6th day | Tension
chylothorax | N/A | Chyle | Surgery-ductal
ligature-in the vicinity of the inferior pulmonary vein stump,
medial to the esophagus | Chyle | Surgery-ductal
ligature-in the vicinity of the inferior pulmonary vein stump,
medial to the esophagus | No recurrence | (13) |
| 10 | Sarsam (1994) | Primary lung
cancer | Right | Intrapleural
intrapericardial pneumonectomy | Between the 5th and
the 6th day | Tension
chylothorax | N/A | Chyle | Surgery-ductal
ligature-in the vicinity of the Inferior pulmonary vein stump,
medial to the esophagus | Chyle | Surgery-ductal
ligature-in the vicinity of the inferior pulmonary vein stump,
medial to the esophagus | No recurrence | (13) |
| 11 | Karwande
(1986) | Lung squamous cell
carcinoma | Right | Intrapleural
intrapericardial pneumonectomy | 5th day | Tension
chylothorax | M | Chyle | Evacuatory
thoracentesis | High trgly, low
chol | Surgery-supra
diaphragmatic ligation of the thoracic duct and mattressed suture
of the leak at the hilum area | No recurrence | (14) |
| 12 | Karwande
(1986) | Hilar
adenocarcinoma | Right | Intrapleural
extrapericardial pneumonectomy | 15th day | Tension
chylothorax | F | Chyle | Evacuatory
thoracentesis | High trgly, low
chol | Repeated evacuatory
thoracentesis followed by 18 gauge chest drain | Patient deceased
due to comorbidities (hemoragic duodenal ulcer). The high-output
chylothorax persisted until her death | (14) |
| 13 | Kanjanauthai
(2009) | Primary lung
cancer | Left | Intrapleural
extrapericardial pneumonectomy | 14 days | Tension
chylothorax | N/A | Chyle | Evacuatory
thoracentesis | Chylothorax | Surgery-thoracic
duct ligation | no recurrence | (2) |
| 14 | Valliers
(1993) | NSCLC
adenocarcinoma | Right | Intrapleural
extrapericardial pneumonectomy | 11 days | Tension
chylothorax | F | Chyle | Diagnosis
thoracentesis | High trgly, low
chol | Chest drain with
instillation of antibiotic solution | No recurrence. 96 h
after the pleurostomy, the chest drain was removed | (15) |
| 15 | Maguire (2013) | Mesothelioma | Left | Extrapleural
pneumonectoy | 6 months | Tension
hydrothorax | M | Exudative pleural
effusion | Evacuatory
thoracentesis | No malignant
cells | (Cefazolin+
gentamicin) | N/A | (16) |
| 16 | Sawar (2006) | Mesothelioma | Left | Extrapleural
pneumonectoy | 9 months | Tension
hydrothorax | M | Exudative pleural
effusion | Evacuatory
thoracentesis | No malignant
cells | Thoracoscopy,
laparoscopy- | N/A | (17) |
| 17 | Vakil (2017) | Lung high grade
spindle cell sarcoma | Left | Intapleural
pneumonectomy with partial pericardiectomy | 17 months | Tension
hydrothorax | F | Exudative pleural
effusion | Evacuatory
thoracentesis | Cytology negative
for malignancy. Cultures negative for microorganisms | Malignancy
excluded; pigtail | No recurrence | (18) |
| 18 | Sakuraba
(2018) | Thymoma st.
IVb | Invasion of right
lung hilum | Extrapleural
pneumonectoy | 0 (zero) days | Tension
pneumothorax | M | Air | Suction pressure
increased from -5 to -15 cm H2O | N/A | Catheter | No recurrence | (19) |
| 19 | Rus (2014) | Adenocarcinoma
(T3N0M0) | Left | Intrapleural
extrapericardial pneumonectomy | 15 months | Tension
hemothorax | F | Hematic pleural
liquid | Thoracoscopy | N/A | Evacuatory
thoracentesis | No recurrence;
alive and well in March 2022 | (20) |
These complications after pneumonectomy are not
frequent in daily practice but they present usually as emergencies
and their impact may be fatal.
The reviewed pneumonectomies were performed for
spindle lung sarcoma (1 case), mesothelioma (3 cases), and primary
lung carcinoma (15 cases).
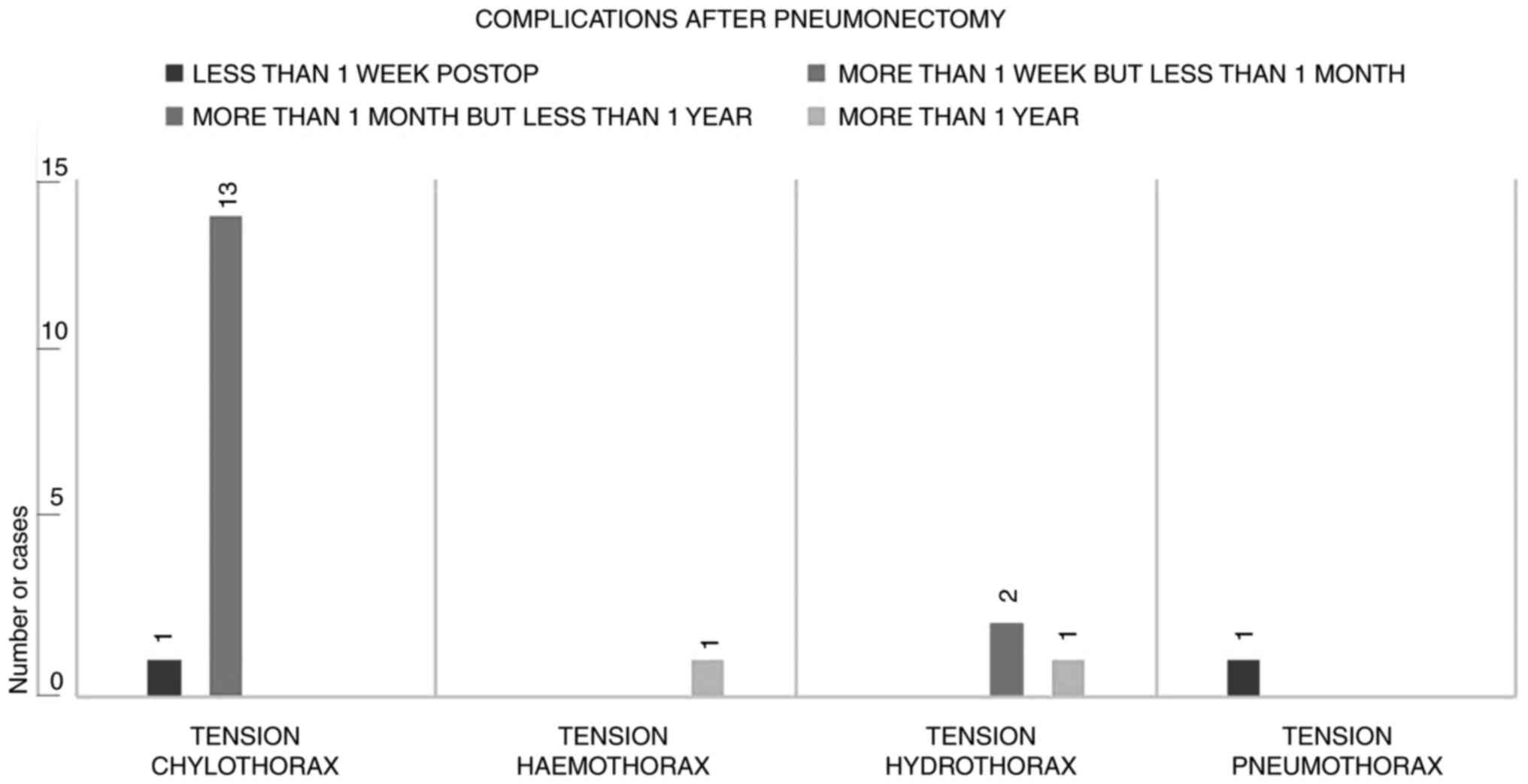
All 19 patients underwent pneumonectomy for
malignancy. There were 16 intrapleural pneumonectomies (of which 3
were with intrapericardial approach) and 3 extrapleural
pneumonectomies (Table II). The
complications appeared immediately after surgery (1 case), early
after surgery-in the first 15 postoperative days (14 cases), and
late after surgery-between 6 and 17 months (4 cases), as presented
in Fig. 2.
3. Types of fluid in the post-pneumonectomy
space
Occurrence
Tension chylothorax after pneumonectomy for
malignancy was the most frequent complication described, accounting
for 14 patients out of 19 (73.68%); however, chylothorax is a rare
complication with an incidence of <0.7% (10). Tension chylothorax was followed in
incidence by tension hydrothorax (3 cases; 15.78%), tension
haemothorax (1 case; 5.26%) and tension pneumothorax (1 case;
5.26%).
Tension chylothorax
The development of tension chylothorax after
pneumonectomy for malignancy may be explained by the injury during
subcarinal or subaortic dissection of small lymphatics that drain
the lung or the mediastinal lymph nodes directly into the thoracic
duct (21).
Tension chylothorax occurred only after classic
pneumonectomies (intrapleural extrapericardial), 7 right and 7 left
(Table II; cases 1-14). On the
right, it occurred between post-operative days 5 and 15 (mean, 9.14
days) and on the left between post-operative days 2 and 14 (mean,
6.22 days). Perhaps after left pneumonectomy, recovery is faster
compared to the right and the patient is allowed to ingest normal
food earlier, thus causing the chylothorax to manifest earlier.
Tension hydrothorax
After pneumonectomy, given an uneventful
post-operative course, effusion in the post-pneumonectomy space
usually accumulates ex vacuo as pleural pressure
equilibrates to zero (18). The
fluid builds up gradually in weeks to months as the air resorbs
partially or totally, as exemplified in Fig. 1. As this happens, the mediastinum
is still shifted to the operated site but when an abnormal level of
fluid rapidly accumulates or air is present, the mediastinum is
pushed to the contralateral side, the heart is compressed and the
patient usually has a certain form of cardiovascular and
respiratory symptomatology (tachycardia, hypotension, high venous
pressure, tachypnoea, marked dyspnoea at rest, cardiac tamponade,
pericarditis).
Tension hydrothorax after pneumonectomy is more
frequent in patients who undergo peritoneal dialysis (22). However, after pneumonectomy for
cancer, tension hydrothorax was reported for only 3 cases-two left
extra-pleural-pneumonectomies for diffuse malignant mesothelioma
(16,17) and 1 left intrapericardial
pneumonectomy with partial pericardiectomy for lung sarcoma
(18). They occurred at 6, 9 and
17 post-operative months, respectively (Table II; cases 15, 16, 17). The first
suspicion was of malignancy progression causing fluid accumulation,
but this was excluded by cytology/pleural biopsy. In all 3 cases,
the pericardium was resected and the heart cavities were exposed to
the pressure of the fluid from the post-pneumonectomy space,
causing cardiac compression.
Tension pneumothorax
One case of tension pneumothorax after pneumonectomy
for malignancy was reported, which was attributed by the authors to
the chest wall damage after extrapleural pneumonectomy and a lower
suction pressure of the chest drain was selected in order to avoid
cardiac herniation (19). It
occurred on the first post-operative day (case 18-Table II).
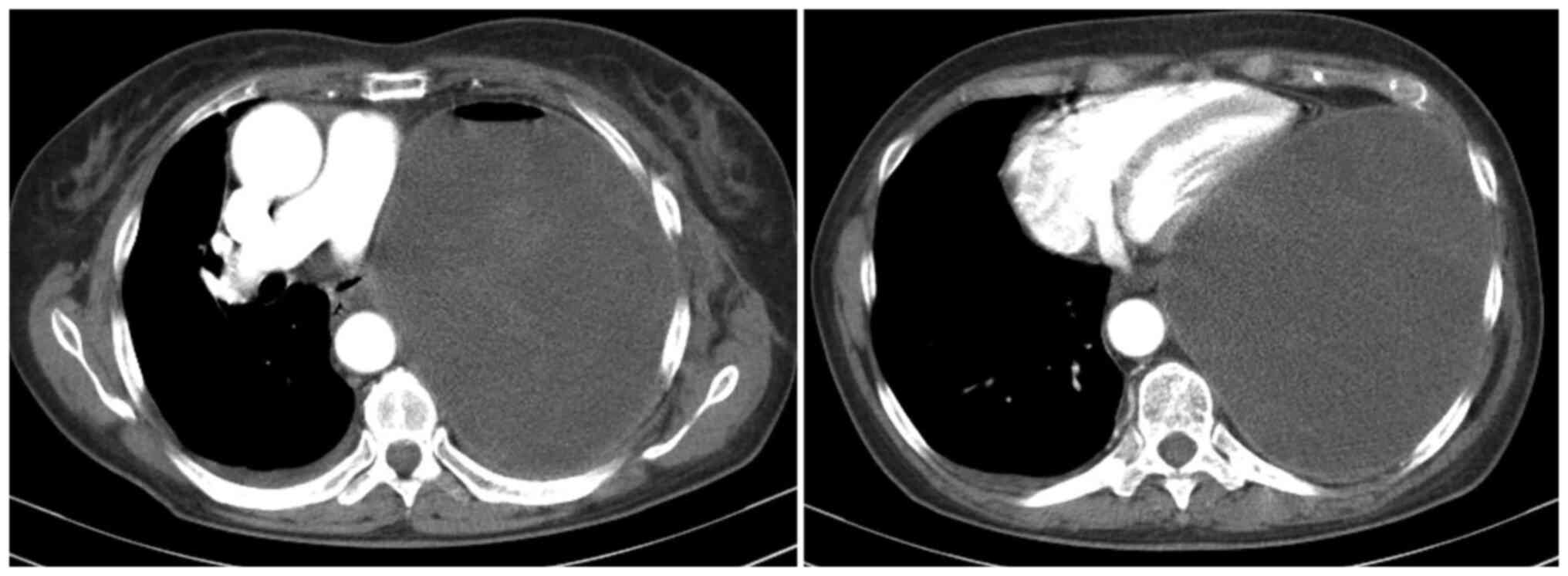
Tension haemothorax
One case of tension haemothorax was reported and the
complication appeared almost 1 year after pneumonectomy, causing
fatigue, dyspnoea, and oedema of the left arm; internal jugular,
subclavian and axillary left veins presented thrombosis; the case
was presented by our group in 2014(20) (case 19-Table II). Thoracoscopic evacuation and
pleural biopsies were performed. The liquid analysis indicated no
malignancy but given the pleural aspect found during surgery, it
was deemed to be the mechanism of appearance. However, pleural
biopsies proved no malignancy. At four months after therapeutic
anticoagulation for the deep venous thrombosis, left haemothorax
recurrence developed, with cardiac compression and hypodiastolia
(Fig. 3), and emergency evacuation
was performed. At present, 8 years after left pneumonectomy, the
patient is alive and in a good clinical condition.
4. Treatment of the tensioned
post-pneumonectomy space
Once the diagnosis is established, the treatment for
the tensioned space is imperative, as this complication frequently
poses a fatal risk. Normally, without a strong reason,
thoracentesis and pleural puncturing are not the best solutions
after pneumonectomy, since seeding the pleural cavity may lead to
empyema. However, thoracentesis may be a lifesaving intervention in
tension fluid-thorax; which was the most common initial approach in
the literature: 9 thoracenteses, 2 for diagnostic and 7 for
therapeutic purposes (Table
II).
The final treatment was surgical in 12 cases, either
by video-assisted thoracic surgery or open surgery: 10 thoracic
duct ligations, 1 thoracoscopic exclusion of malignancy, and 1
evacuation of clots (Table
II).
For tensioned chylothorax (14 cases), initial
management was decompression in 10 cases, followed by either
conservative or surgical management. In 4 cases of tensioned
chylothorax, the initial management was surgical duct ligation. The
general management of chylothorax is not the subject of this paper
and will therefore not be further discussed, but the cause is the
same: lymphatics interrupted during the mediastinal lymph node
dissection.
For tension hydrothorax (3 cases), the initial
management was evacuation thoracentesis, followed by exclusion of
malignancy through cytology in one case, thoracoscopy and
laparoscopy with pigtail catheter in another case and indwelling
pleural catheter in the third case. No specific causes were
observed.
In the case of tensioned pneumothorax, the adopted
solution was the simplest and solved the problem: Increasing
suction pressure and maintaining the drainage until the air leak
disappeared.
In the case of tensioned haemothorax with
recurrence, the evacuation of haemorrhagic fluid was performed
thoracoscopically the first time and through thoracotomy the second
time (fluid + clots). The cause was determined to be the
anticoagulant therapy administered for venous thrombosis of the
left internal jugular, subclavian and axillary veins.
5. Conclusions
Tensioned post-pneumonectomy space is a rare but
potentially fatal complication. To date, a total of 19 cases of
tensioned post-pneumonectomy space after pneumonectomy for cancer
were published in the literature.
Tension chylothorax is the most frequent type (14
cases) and is most probably caused by mediastinal lymph node
dissection (MLND); it is an assumed complication because MLND is
mandatory for radical resection of lung cancer. It appeared after a
maximum of 15 days post-pneumonectomy and it was solved similarly
to any post-operative chylothorax.
Tension hydrothorax is the second-most frequent type
(3 cases) and it appeared after complex pneumonectomies for
mesothelioma and sarcoma.
Tension haemothorax and tension pneumothorax have
one published case each, and each was caused by a particular
condition of the case.
Shifted mediastinum with cardiac compression
(leading to cardiac tamponade) causes haemodynamic instability and
dyspnoea; in such cases, emergency thoracentesis may be required.
After stabilization, a major surgical procedure may be necessary to
definitively treat the cause of the tensioned post-pneumonectomy
space.
Acknowledgements
The authors thank Professor Teodor Horvat (Clinic of
Thoracic Surgery, Institute of Oncology ‘Prof. Dr. Al.
Trestioreanu’ Bucharest, University of Medicine and Pharmacy Carol
Davila Bucharest) for mentorship.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
NM and VM contributed to the conception and design
of the study, performed the literature review and wrote the
manuscript. OR, MD, MCCI and OGT analyzed the data, integrated the
medical information and prepared the figures. NM, VM, BS and MCC
contributed to manuscript revision. All authors have read and
approved the final manuscript. Data authentication is not
applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Collau S and Dartevelle P: Pneumonectomy
and its modifications. In: LoCicero J III, Feins RH, Colson YL and
Rocco G (eds). Shields' General Thoracic Surgery. 8th edition.
Philadelphia: Wolters Kluwer, pp412-418, 2018.
|
|
2
|
Kanjanauthai S, Kanluen T and Bergman M:
Tension chylothorax: A rare life threatening entity after
pneumonectomy. Heart Lung Circ. 18:55–56. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
COVIDSurg Collaborative: Effect of
COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour
types in 61 countries: An international, prospective, cohort study.
Lancet Oncol. 22:1507–1517. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Serban D, Socea B, Badiu CD, Tudor C,
Balasescu SA, Dumitrescu D, Trotea AM, Spataru RI, Vancea G,
Dascalu AM and Tanasescu C: Acute surgical abdomen during the
COVID-19 pandemic: Clinical and therapeutic challenges. Exp Ther
Med. 21(519)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Serban D, Papanas N, Dascalu AM, Stana D,
Nicolae VA, Vancea G, Badiu CD, Tanasescu D, Tudor C, Balasescu SA
and Pantea-Stoian A: Diabetic retinopathy in patients with diabetic
foot ulcer: A systematic review. Int J Low Extrem Wounds.
20:98–103. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Alloubi I, Jougon J, Delcambre F, Baste JM
and Velly JF: Early complications after pneumonectomy:
Retrospective study of 168 patients. Interact Cardiovasc Thorac
Surg. 11:162–165. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sugarbaker DJ, Jaklitsch MT, Bueno R,
Richards W, Lukanich J, Mentzer SJ, Colson Y, Linden P, Chang M,
Capalbo L, et al: Prevention, early detection, and management of
complications after 328 consecutive extrapleural pneumonectomies. J
Thorac Cardiovasc Surg. 128:138–146. 2004.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ammori JB, Pickens A, Chang AC and
Orringer MB: Tension chylothorax. Ann Thorac Surg. 82:729–730.
2006.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Coco LF, Redondo Enríquez JM, Pardo Romero
G and Barba Orejudo A: Tension chylothorax in the late
postoperative period of left-sided pneumonectomy. Rev Esp
Anestesiol Reanim (Engl Ed). 67:49–50. 2020.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
10
|
Hemang Y, Matthew E, Nolan FC III and
Daniels CE: Tension chylothorax following pneumonectomy. Respir Med
Case Rep. 14:16–18. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Huwer H, Volkmer I and Feindt P: Tension
chylothorax following left-side lung surgery. Pneumologie.
45:337–339. 1991.PubMed/NCBI(In German).
|
|
12
|
Van Mulders A, Lacquet LM, Van Mieghem W
and Deneffe G: Chylothorax complicating pneumonectomy. Thorax.
39:954–955. 1984.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sarsam MA, Rahman AN and Deiraniya AK:
Postpneumonectomy chylothorax. Ann Thorac Surg. 57:689–690.
1994.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Karwande SV, Wolcott MW and Gay WA Jr:
Postpneumonectomy tension chylothorax. Ann Thorac Surg. 42:585–586.
1986.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Vallieres E, Shamji FM and Todd TR:
Postpneumonectomy chylothorax. Ann Thorac Surg. 55:1006–1008.
1993.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Maguire K, Leung C, Kodali V, Taylor B,
Fontaine JP, Rojas CA and Maya G: Heart failure due to tension
hydrothorax after left pneumonectomy. Heart Surg Forum.
16:E319–E323. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sawar A and Schocken DD: Cardiac tamponade
complicating trimodal therapy for malignant mesothelioma. Heart
Lung. 35:355–357. 2006.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Vakil E, Faiz SA, Iliescu C, Balachandran
DD, Ong P, Debiane LG and Mehran R: Managing post-pneumonectomy
tension hydrothorax. Ann Am Thorac Soc. 14:1031–1035.
2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Sakuraba S, Omae T, Kawagoe I, Koh K and
Inada E: Respiratory failure caused by impending tension
pneumothorax after extrapleural pneumonectomy: A case report. JA
Clin Rep. 4(45)2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rus O, Motas C, Motas N, Achim D and
Horvat T: Hypertensive late hemothorax following left
pneumonectomy. Chirurgia (Bucur). 109:827–831. 2014.PubMed/NCBI
|
|
21
|
Nistor C, Ciuche A and Horvat T:
Chilothorax. In: Textbook of Surgery. Popescu I (ed). Vol. 4.
Editura Academiei Romane, Bucharest, pp297-314, 2008.
|
|
22
|
Chow KM, Szeto CC, Wong TY and Li PK:
Hydrothorax complicating peritoneal dialysis: Diagnostic value of
glucose concentration in pleural fluid aspirate. Perit Dial Int.
22:525–528. 2002.PubMed/NCBI
|