Introduction
Terrible triad injury of the elbow (TTIE) refers to
dislocation of the elbow joint, accompanied by fractures of the
radial head and coronoid process. TTIE is one of the more serious
and complex injuries in the elbow joint (1). TTIE was first proposed by Hotchkiss
in 1996(2). The injury is often
accompanied by valgus, rotation, axial and other stresses, as well
as damage to the medial and lateral ligament complexes, which make
the elbow joint markedly unstable even after reduction (3). Conservative treatment cannot restore
the stability of the key structures of the elbow, resulting in
traumatic instability of the elbow joint (4). Patients often experience repeated
dislocation or subluxation, and the immobilization time is too long
during treatment, resulting in stiffness of the elbow joint and
loss of mobility (5). The overall
outcome of treatment is therefore not ideal for patients. With
in-depth understanding of the mechanism and anatomical structure
related to TTIE, the latest research shows that the key to a
successful recovery from TTIE is to restore the stability of the
elbow joint as soon as possible (6). At present, more active surgical
treatment is advocated.
The stability of the elbow joint is generally
maintained by the distal humerus, radial head and other bony
structures, as well as the ligaments and soft tissues around the
elbow joint. In addition to repairing the damaged ligaments, the
method of restoration of the physiological function of the radial
head has become the top priority in the treatment of TTIE (7). Among them, the surgical methods for
radial head fractures are mainly open reduction internal fixation
(ORIF) and radial head arthroplasty (RHA). It is believed that ORIF
can achieve good clinical efficacy in restoring the anatomical
structure of the radial head, but complications also arise, such as
internal fixation loosening and nonunion. Other studies have shown
that RHA can also effectively treat complex elbow injuries,
although RHA has complications too, such as internal fixation
loosening and excessive filler (1,8).
Consequently, Carroll and Morrissey (9) suggested that even with surgical
treatment, instability and arthritis may be predisposed.
Furthermore, in numerous cases, the choice of surgical approach is
one of the key factors that contribute to instability, limited
range of motion (ROM) and elbow stiffness (10). Therefore, selecting the most
suitable surgical method for patients has become the focus of
clinical attention.
Certain researchers have previously conducted
studies to compare the efficacy of two surgical approaches for
radial head fractures. For example, Chen et al (11) indicated that RHA for the treatment
of TTIE had better postoperative outcomes than ORIF, along with
fewer complications. However, Kyriacou et al (12) found no difference in functional
outcomes between the two procedures. In recent years, there have
been new reports (13-16)
of clinical case-control studies on the subject of TTIE surgical
treatment that meet the inclusion criteria of the present study. In
order to compare the differences between the two treatments more
objectively, the current study included an updated meta-analysis
compared with the aforementioned studies to provide a theoretical
basis for clinical practice.
Materials and methods
Inclusion and exclusion criteria
Study subjects included those in published,
controlled clinical studies. Based on the patient's medical
history, physical examination and imaging examination, the patient
must have been diagnosed with TTIE and required surgery on the
radial head. Non-case-control studies, case reports, review
articles, letters and duplicate reports were excluded. Literature
without sufficient relevant data were also excluded. The
interventions were RHA and ORIF. The outcome indicators were the
Mayo Elbow Performance Score (MEPS), the Disabilities of the Arm,
Shoulder and Hand (DASH) score, the range of the flexion-extension
arc and of the pronation-supination arc and complications.
Search strategy
The databases used to retrieve the studies included
Embase, PubMed, Cochrane Central Register of Controlled Trials,
Cumulative Index to Nursing and Allied Health Literature, ProQuest
Dissertations and Theses, Cochrane Library and Chinese Biomedical
Literature Database. The date limits for the search were January
2002 to April 2022. Journal catalogues and bibliographical
references were also searched in an effort to find grey literature,
such as unpublished academic papers or chapters in monographs. All
relevant documents were searched for in any language and translated
if necessary. The searched keywords were terrible triad of the
elbow, radial head fracture, replacement, open reduction internal
fixation, and the retrieval strategy was (‘repair’ OR ‘fixation’ OR
‘open reduction internal fixation’ OR ‘restore’ OR ‘renovate’) AND
(‘replacement’ OR ‘arthroplasty’) AND (‘terrible triad of the
elbow’ OR ‘terrible triad’ OR ‘elbow’ OR ‘radial head
fracture’).
Quality assessment
The included literature was independently analyzed
by two physicians, and any disagreements were resolved through
discussion or handed over to a third senior physician to jointly
determine the quality of the literature. The Cochrane bias risk
assessment criteria was strictly followed (17), including: i) Whether the
experimental design adopted the principle of randomization; ii)
whether the subjects, performers and measurers used the
double-blind principle; iii) whether the experimental data was
complete and credible; iv) whether the allocation concealment
method was used; v) whether the experiment used a selective data
reporting method; and vi) other factors of bias. The quality of the
literature was also evaluated according to the modified Jadad scale
(18), with a total possible score
of 7 points (2 points for adequate randomization, 2 points for
randomization concealment, 2 points for adopting the double-blind
principle and 1 point for lost follow-up). The literature was
divided into low-quality (1-3 points), medium-quality (4 points)
and high-quality (5-7 points) according to score.
Statistical analysis
Meta-analysis of the extracted data was performed
using ReviewManager 5.4 software (Cochrane). Data from dichotomous
variables are presented as an odds ratio with a 95% confidence
interval (CI), while data from continuous variables are presented
as the mean ± standard deviation and a 95% CI. The I²,
tau2, χ2, degrees of freedom and Z values
were calculated to assess the heterogeneity between different
studies (minimum of 6 papers, maximum of 13 papers). If the
calculated I²-value was <50%, indicating that the heterogeneity
between the studies was small, a fixed effects model was used. If
an I²-value was ≥50%, indicating that the heterogeneity between the
studies was large, the reasons for the heterogeneity were analyzed
and a random effects model was used. Sensitivity analyses were
performed when heterogeneity was high, and funnel plots were
constructed to assess publication bias (the abscissa is generally
the effect size of a single study, and the ordinate is the scatter
plot of the sample size). P<0.05 was considered to indicate a
statistically significant difference.
Results
Essential features of the included
literature
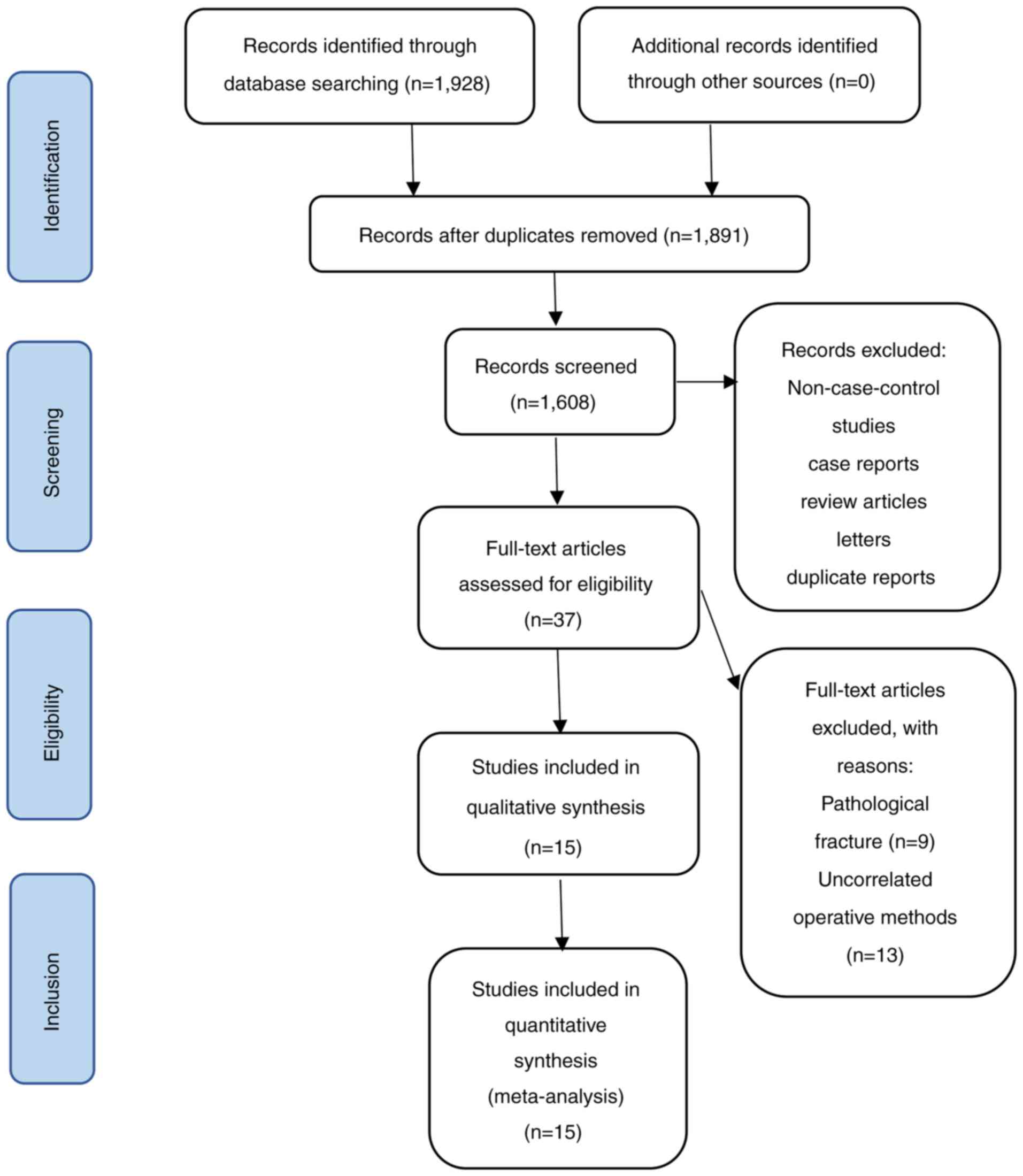
According to the above search strategy, a total of
1,928 related publications were retrieved. By reading the titles
and abstracts, 1,891 uncontrolled studies, duplicate publications
and publications irrelevant to the research aim were excluded, and
37 relevant publications were preliminarily included. The full text
was then screened according to the inclusion and exclusion
criteria, to finally include 15 articles. After analysis, it was
found that a total of 189 cases underwent RHA and 266 cases
underwent ORIF in the included literature. The baseline conditions,
such as patient age and disease course, of all the included studies
were compared and found to be similar (P>0.05). The literature
screening process and results are illustrated in Fig. 1, and the fundamental
characteristics of the included studies are presented in Table I (13-16,19-29).
 | Table IFundamental characteristics of the
included studies. |
Table I
Fundamental characteristics of the
included studies.
| First author,
year | Study design | Country | Group | Number of
patients | Age, years (mean ±
standard deviation) | Sex, male/
female | Outcome measures | Modified Jadad
score | (Refs.) |
|---|
| Afifi et al,
2020 | Prospective | Egypt | RHA | 16 | 40.40±14.90 | 17/13 | a, b, c, d | 6 | (13) |
| | | | ORIF | 14 | | | | | |
| Giannicola et
al, 2015 | Prospective | Italy | RHA | 16 | 53.13±12.49 | 7/9 | a, b, c, d, e | 6 | (19) |
| | | | ORIF | 9 | 48.89±20.25 | 5/4 | | | |
| Hou et al,
2021 | Retrospective | China | RHA | 3 | 37.33±5.86 | 1/2 | a, b, c, d, e | 4 | (14) |
| | | | ORIF | 21 | 33.81±7.30 | 15/6 | | | |
| Jeong et al,
2010 | Retrospective | Korea | RHA | 3 | 43.80±38.00 | 7/6 | a, c, d, e | 4 | (20) |
| | | | ORIF | 10 | | | | | |
| Klug et al,
2020 | Retrospective | Germany | RHA | 26 | 53.90±43.57 | 8/18 | a, b, c, d | 4 | (15) |
| | | | ORIF | 51 | NA | NA | | | |
| Leigh and Ball,
2012 | Retrospective | New | RHA | 11 | 45.50±22.50 | 6/5 | b, c, d | 5 | (21) |
| | | Zealand | ORIF | 13 | 42.20±16.29 | 6/7 | | | |
| Li et al,
2018 | Retrospective | China | RHA | 24 | 37.50±75.63 | 34/20 | a, e | 4 | (22) |
| | | | ORIF | 30 | | | | | |
| Liu et al,
2018 | Retrospective | China | RHA | 4 | 48.23±10.95 | 29/12 | a, c, d, e | 4 | (23) |
| | | | ORIF | 37 | | | | | |
| Matar et al,
2017 | Retrospective | England | RHA | 9 | 55.67±8.56 | 4/5 | a, c, d, e | 5 | (24) |
| | | | ORIF | 4 | 61.50±12.26 | 0/4 | | | |
| Pierrart et
al, 2015 | Retrospective | France | RHA | 7 | NA | NA | a, c | 3 | (25) |
| | | | ORIF | 10 | | | | | |
| Toros et al,
2012 | Retrospective | Turkey | RHA | 5 | 40.60±6.39 | 3/2 | a, b, c, d | 4 | (26) |
| | | | ORIF | 11 | 33.00±8.68 | 8/3 | | | |
| Watters et
al, 2014 | Retrospective | USA | RHA | 30 | 48.00±64.49 | 21/18 | c | 2 | (27) |
| | | | ORIF | 9 | | | | | |
| Yan et al,
2015 | Retrospective | China | RHA | 20 | 36.54±6.58 | 11/9 | a, c, d, e | 6 | (28) |
| | | | ORIF | 19 | 35.51±6.28 | 7/12 | | | |
| Zhang et al,
2014 | Retrospective | China | RHA | 2 | NA | NA | a, c, d, e | 5 | (29) |
| | | | ORIF | 18 | | | | | |
| Zheng et al,
2020 | Retrospective | China | RHA | 13 | 47.08±6.20 | 9/4 | a | 3 | (16) |
| | | | ORIF | 10 | 48.20±7.22 | 6/4 | | | |
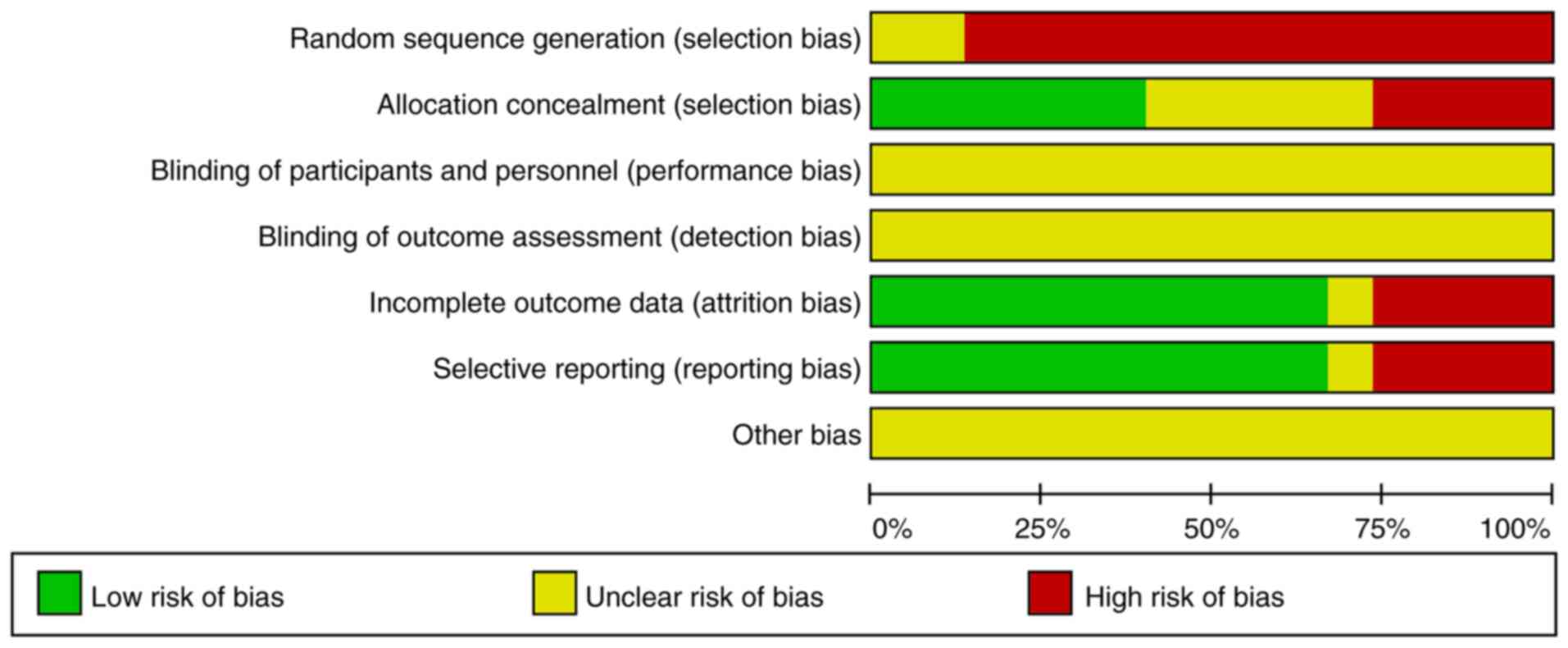
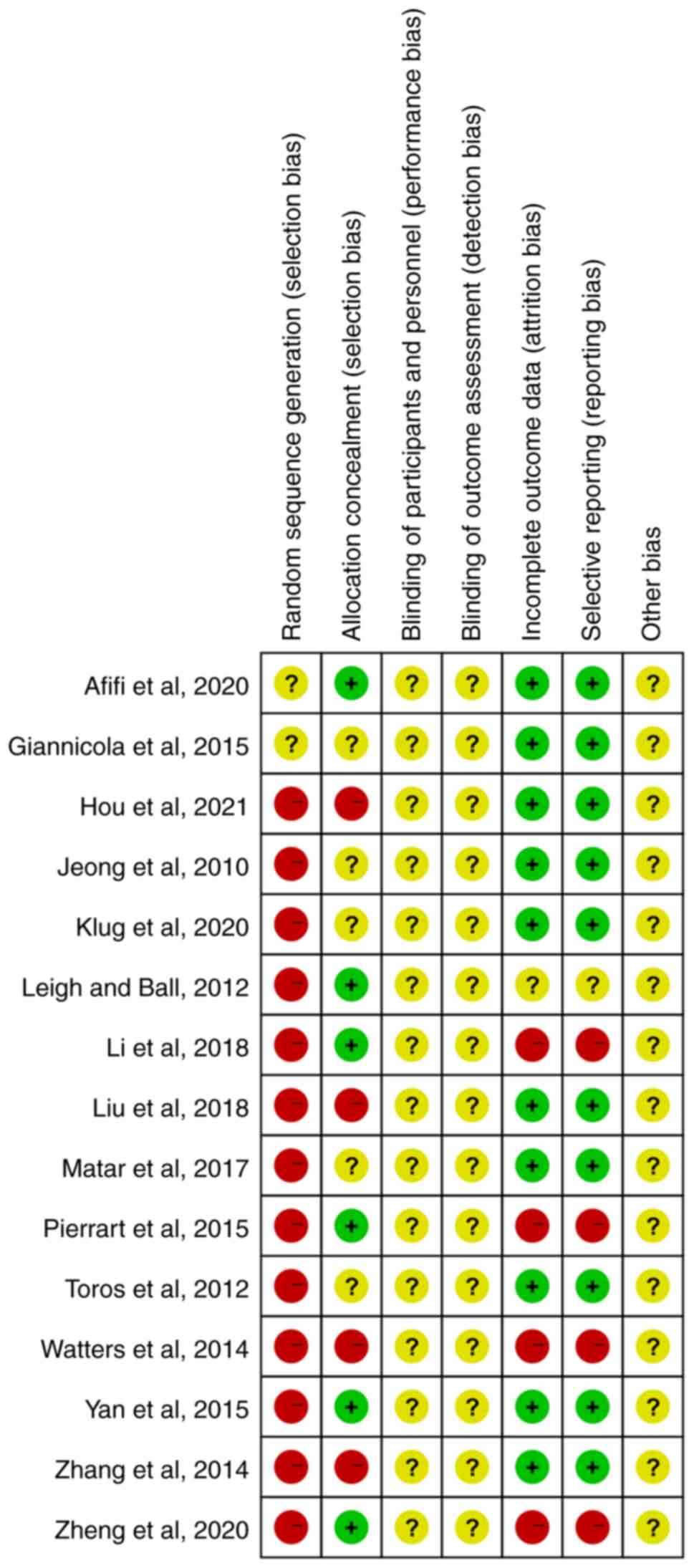
Quality assessment of included
literature
The present study included two prospective studies,
13 retrospective studies and no randomized controlled trials. After
following the Cochrane bias risk assessment criteria, the quality
was then evaluated using the modified Jadad score. Of the fifteen
studies, there were six high-quality papers (three of which scored
6 points and three of which scored 5 points), eight medium-quality
papers (six of which scored 4 points and two of which scored 3
points) and one low-quality paper (which scored 2 points). Although
the number of included papers is limited and there is a certain
bias, the overall quality is moderate.
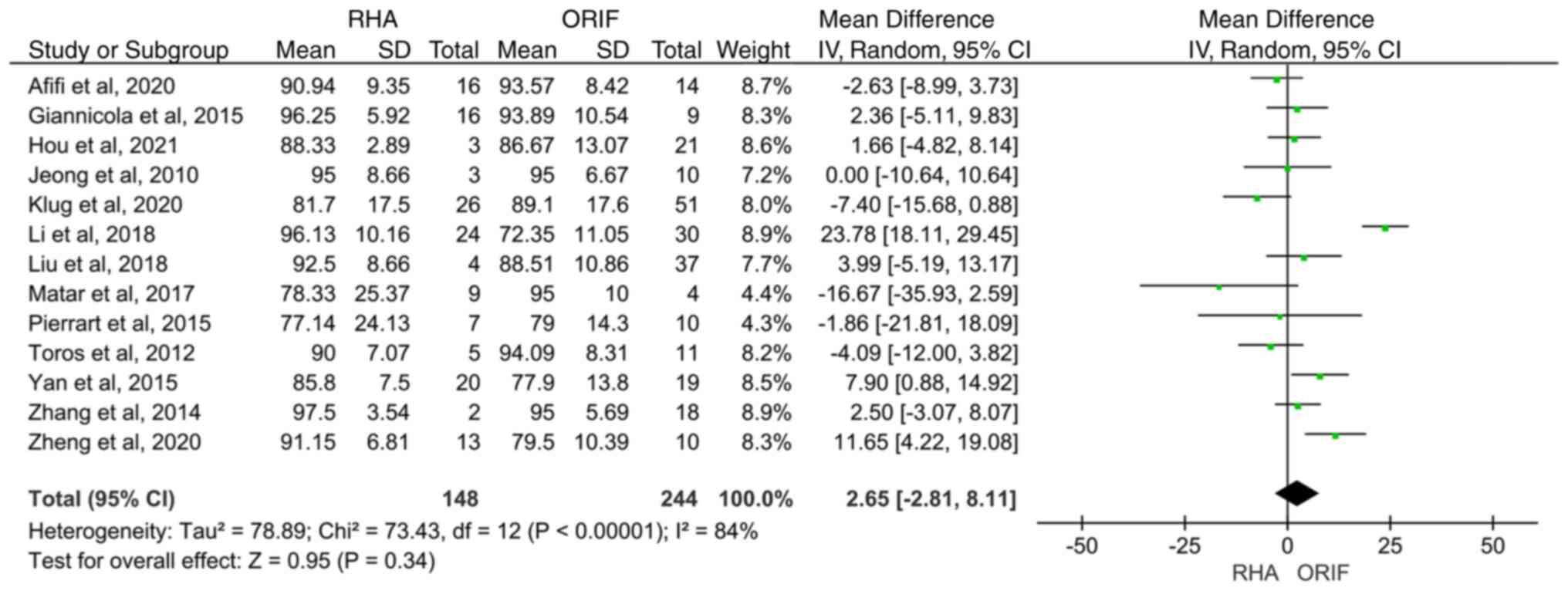
Outcome measures MEPS
A total of 13 studies including 392 patients
compared the MEPS between RHA and ORIF. The heterogeneity test
showed that there was significant heterogeneity among studies
(I2=84.0%; P<0.00001). Therefore, the random effects
model was used. A total of seven studies had a greater mean MEPS in
the RHA group compared with the ORIF group, while five studies
favored ORIF. The remaining one showed no difference between the
two groups. However, MEPS was found to be similar in the two
groups, and the difference was not statistically significant [95%
CI (-2.81, 8.11); P=0.34] (Fig.
2).
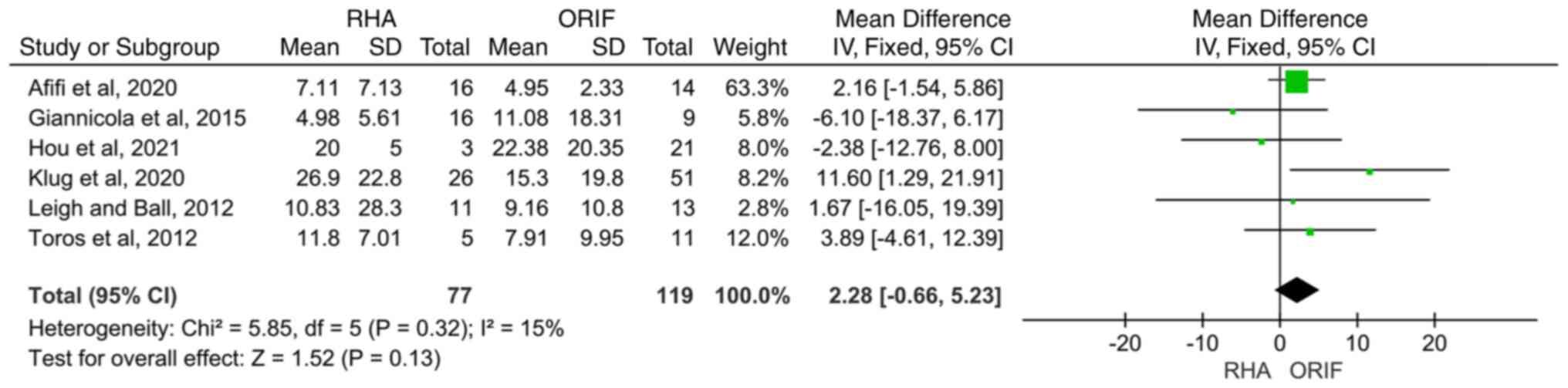
DASH score. A total of six articles provided
detailed information on the DASH score. The fixed effect model was
employed for meta-analysis since there was no significant
heterogeneity among the results (I²=15%). From the meta-analysis,
no significance was observed [95% CI (-0.66, 5.23); P=0.13] for the
DASH score between the RHA and ORIF groups (Fig. 3).
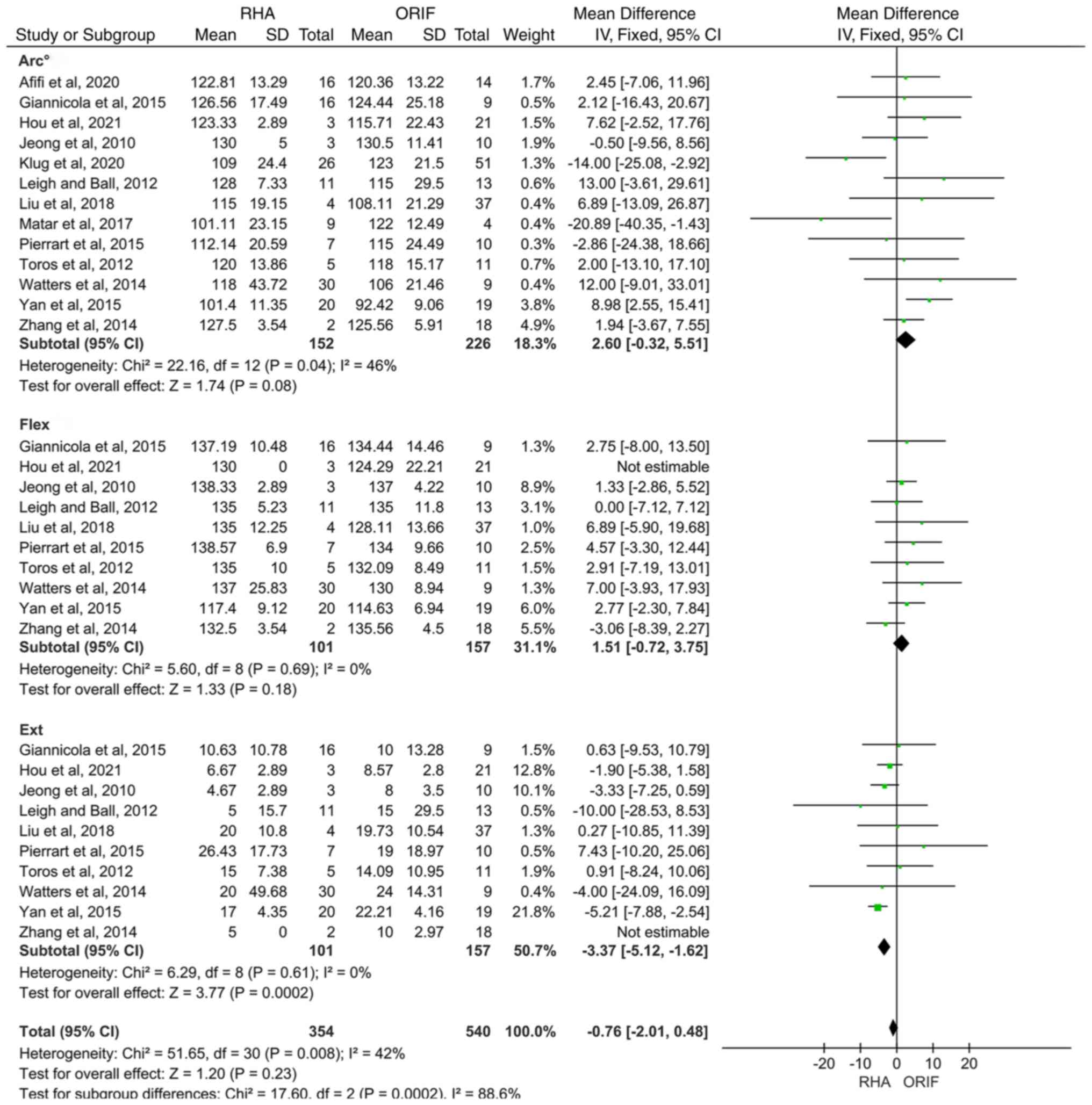
Range of the flexion-extension arc. Data were
divided into three groups: Range of the flexion-extension arc,
flexion and extension. The heterogeneity test performed on the
studies and subgroups showed that there was no significant
heterogeneity among them (I2=42.0%; P=0.008), so the
fixed effect model was employed in the meta-analysis. A total of 13
studies assessed the range of the flexion-extension arc, with nine
studies showing that the mean range of the flexion-extension arc
for the RHA group was higher than that in the ORIF group. However,
the result was not significant [95% CI (-0.32, 5.51); P=0.08].
Furthermore, 10 studies showed that the range of flexion [95% CI
(-0.72, 3.75); P=0.18] did not differ significantly between the
treatment groups, whereas the range of extension in the RHA group
was significantly lower than that in the ORIF group [95% CI (-5.12,
-1.62); P=0.0002] (Fig. 4).
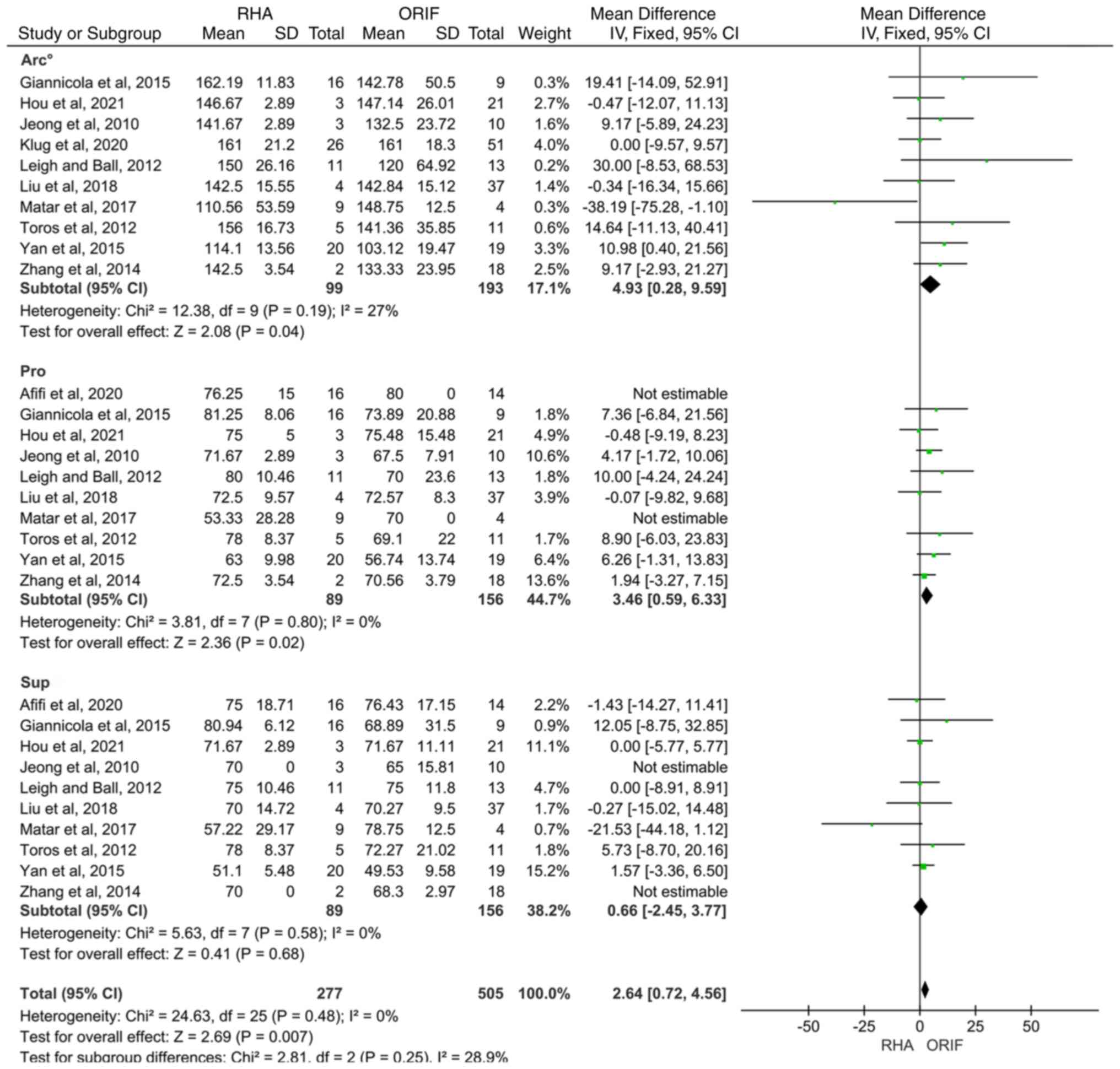
Range of the pronation-supination arc. A
total of 10 articles reported on forearm rotational ROM, and these
were divided into three subgroups according to the range of forearm
pronation, supination and the pronation-supination arc. Since the
heterogeneity of each subgroup and that of the overall study was
not significantly different (I²=28.9%), a fixed-effects model was
used for meta-analysis. Subgroup analysis showed that when RHA was
used to treat TTIE, the maximum pronation degree of the forearm
[95% CI (0.59, 6.33); P=0.02] and the pronation-supination arc [95%
CI (0.28, 9.59); P=0.04] was significantly superior to patients
treated with ORIF. The curative effect on forearm supination ROM
was similar between the two groups [95% CI (-2.45, 3.77); P=0.68],
and the difference was not statistically significant (Fig. 5).
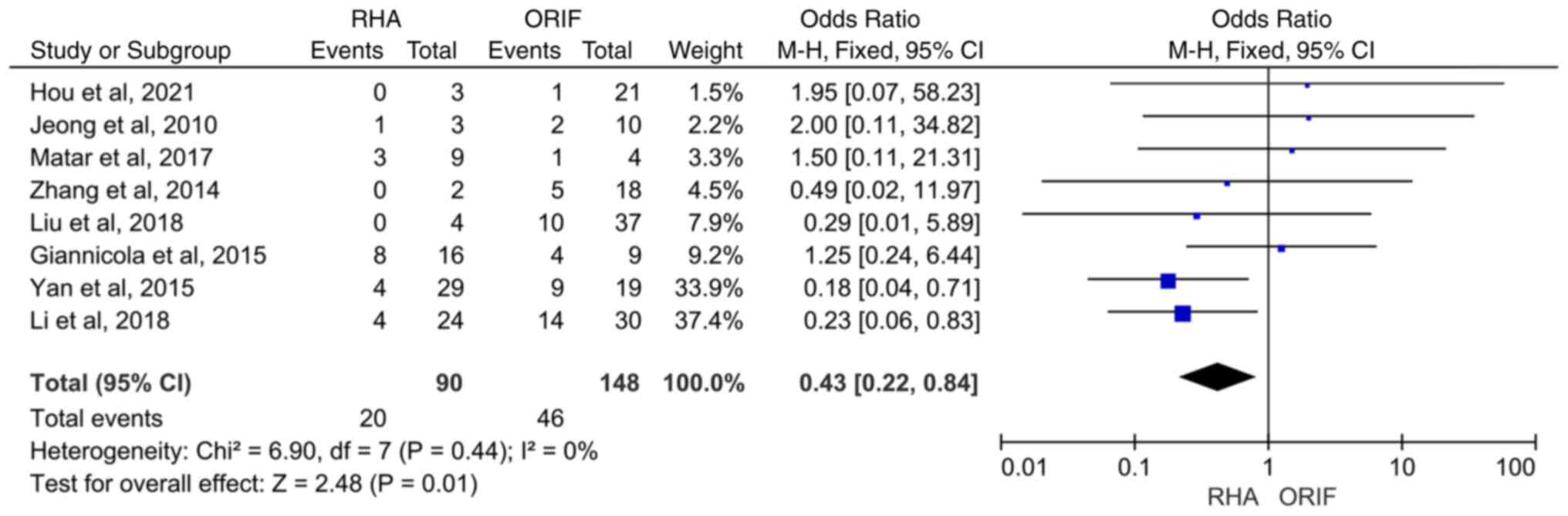
Complications. A total of eight articles
investigated the difference in postoperative complications between
RHA and ORIF, with a total of 66 cases. The present analysis found
that the postoperative complication rate (number of cases with
complications to the total number of cases) of the RHA group was
22%, which was significantly lower than that of the ORIF group at
31% [95% CI (0.22, 0.84); P=0.01]. The heterogeneity test resulted
in I2=0%, indicating that there was no significant
heterogeneity among the studies. Therefore, a fixed effect model
was decided upon for classification. The results showed that the
incidence of postoperative complications in the RHA group was
significantly lower than that in the ORIF group for the treatment
of TTIE [95% CI (0.22, 0.84); P=0.01] (Fig. 6).
Publication bias and sensitivity
analysis
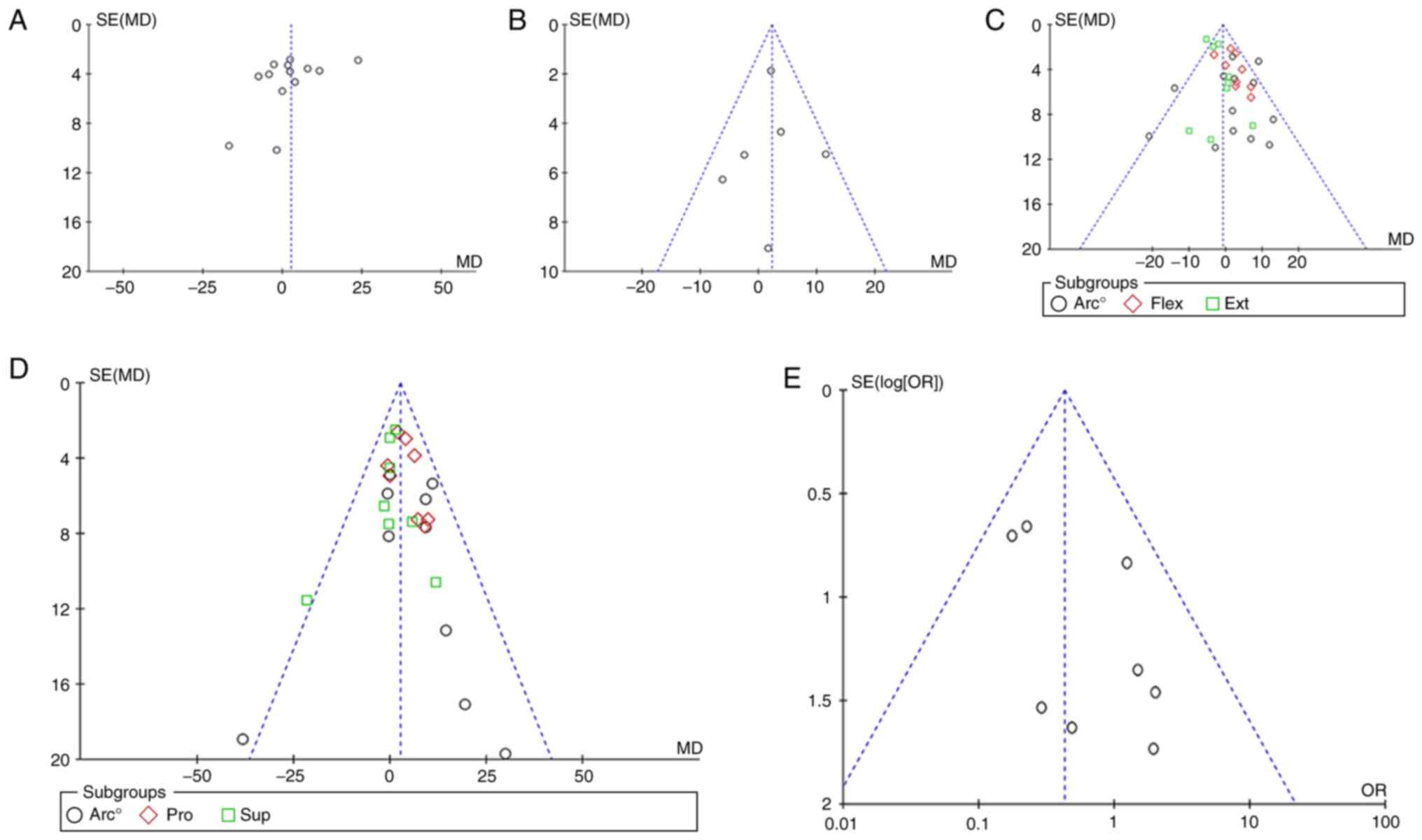
The ReviewManager 5.4 software (Cochrane) was used
to evaluate the postoperative MEPS, DASH score, flexion-extension
arc, pronation-supination arc and complications of TTIE.
Publication bias analysis was carried out on all outcome
indicators, and the results showed that the funnel plots were
essentially symmetrical, indicating that there was no evident
publication bias (Fig. 7, Fig. 8 and Fig. 9). After sensitivity analysis, the
data were considered to be stable and reliable.
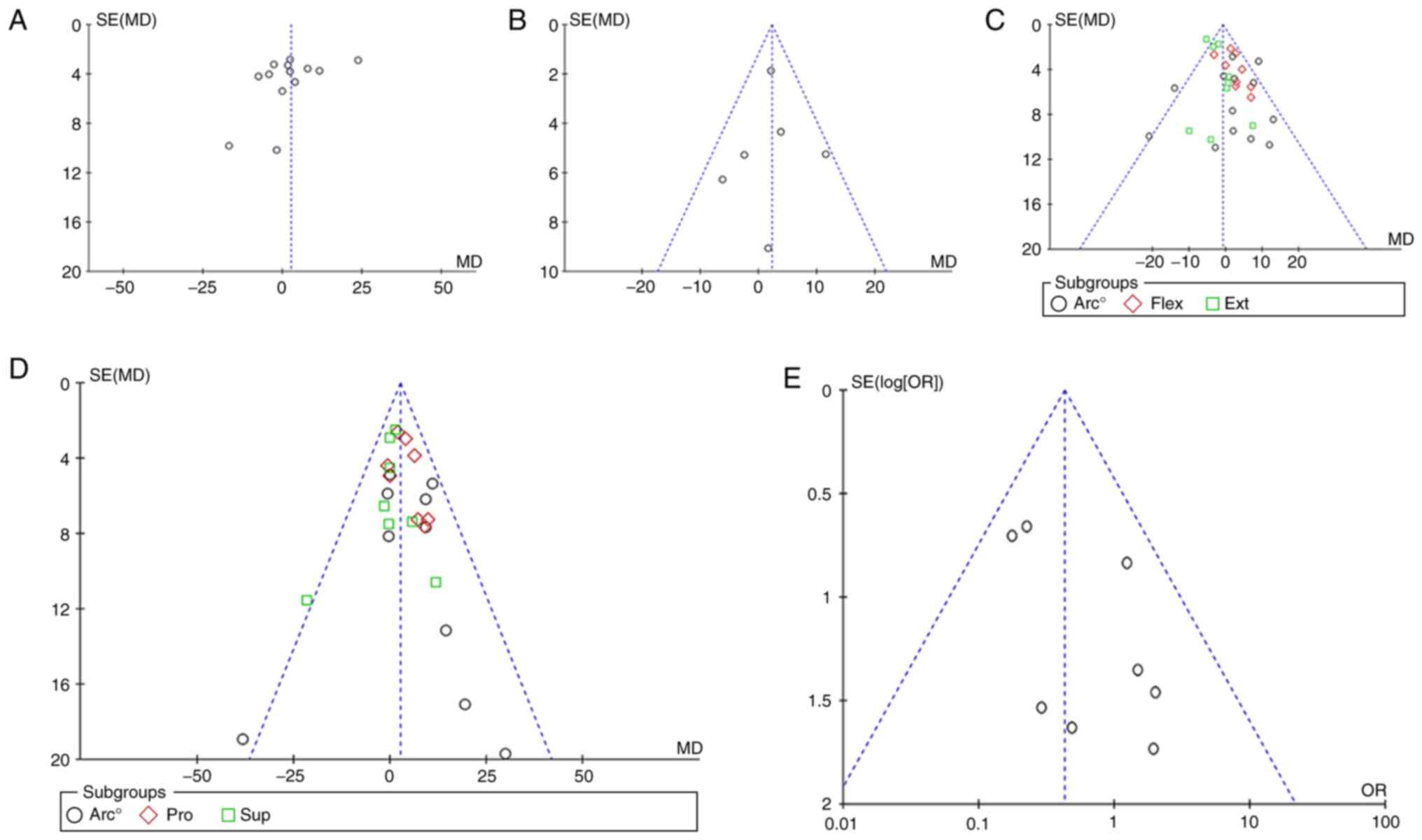 | Figure 9Funnel plots created to assess
publication bias for (A) Mayo Elbow Performance Score, (B)
disabilities of the arm, shoulder and hand score, (C)
flexion-extension arc, (D) pronation-supination arc and (E)
complications. SE, standard error; MD, mean difference; Flex,
flexion; Ext, extension; Pro, pronation; Sup, supination; OR, odds
ratio. |
Discussion
Previous studies have shown that the radial head is
a key structure involved in maintaining the stability of the
lateral side of the elbow joint and bears 20-30% of the valgus
stability (30). When subjected to
valgus stress, the radial head can reduce the tension stress on the
inside of the elbow joint by acting on the fulcrum of the force arm
(12,31). TTIE is often accompanied by damage
to the lateral collateral ligament complex. At this time, if the
radial head is removed, the valgus deformity and instability of the
elbow joint will be aggravated, resulting in various complications,
such as muscle weakness, wrist pain and elbow pain (32). It is widely believed that ORIF is
effective in the treatment of simple radial head fractures
(33), and the elbow joints are
also stabilized after surgery, which coincides with the view of
Leigh and Ball (21). To that end,
ORIF should be prioritized in the treatment of radial head
fractures. However, it has been demonstrated that in the case of
complex fractures of the radial head, especially when there are
>3 articular fracture fragments of the radial head, the
reduction of the radial head cause difficulties because the
fracture fragments are mostly comminuted and displaced (34). When this occurs, the blood supply
of the radial head is notably damaged and forced reduction can
easily lead to complications, such as nonunion of fractures,
loosening of internal fixation and fractures even after internal
fixation. In addition, it is believed that although the internal
fixation materials are increasingly miniaturized, they may still
cause slight scratches to the surrounding tissue, thereby reducing
the enthusiasm of patients for postoperative functional exercise
(35). Therefore, Watters et
al (27) concluded that RHA
has better stability and forearm rotational ROM than ORIF in the
treatment of high-energy injury and comminuted complex radial head
fractures. However, radial head replacement requires accurate
restoration of the biomechanical relationship of the joint
(36), which puts forward certain
requirements for the operator, such as selecting the appropriate
prosthesis and the degree of mastery of the operation. Therefore,
there is still certain controversy about which surgical method to
choose.
At present, the way to obtain a good therapeutic
effect from TTIE is still one of the major problems perplexing
surgeons. Chen et al (11)
concluded that patients with TTIE who received RHA had better
clinical outcomes and fewer postoperative complications compared
with patients who received ORIF. However, the present meta-analysis
found that the postoperative MEPS [95% CI (-2.81, 8.11); P=0.34]
and DASH score [95% CI (-0.66, 5.23); P=0.13] are fundamentally
similar, with no statistical significance between the two groups.
After analysis, it was found that a total of 189 cases underwent
RHA and 266 cases underwent ORIF in the included literature. Most
of the patients in the RHA group had Mason type III fractures
caused by high-energy injury (37), and their soft tissue conditions
were poor, which may be one of the reasons why the RHA group did
not have a significant advantage in postoperative functional scores
compared with ORIF. It has also been shown that early elbow surgery
is one of the influencing factors for restoration of elbow function
(38), and the soft tissue edema
caused by the severe injury in the RHA group was likely to delay
the optimum time for surgery, so it could be difficult to achieve
the desired functional efficacy. However, in terms of postoperative
complications, the results of the present study are consistent with
the results from Chen et al (11). The present analysis found that the
postoperative complication rate of the RHA group was 22%, which was
significantly lower than that of the ORIF group at 31% [95% CI
(0.22, 0.84); P=0.01]. Although both surgical methods have various
complications, such as postoperative elbow instability, heterotopic
ossification and elbow stiffness, the results of the present study
suggested that the RHA group may have better postoperative elbow
stability than the ORIF group, perhaps due to early functional
exercise reducing the risk of complications, such as elbow
stiffness. In addition, Kyriacou et al (12) concluded that there was no
statistical difference in forearm ROM after RHA and ORIF. The
current study found that the RHA group had certain significant
advantages, for example in elbow extension [95% CI (-5.12, -1.62);
P=0.0002], forearm rotation [95% CI (0.28, 9.59); P=0.04] and
maximum pronation range [95% CI (0.59, 6.33); P=0.02]. There was no
significant difference in the maximum flexion angle [95% CI (-0.72,
3.75); P=0.18] and flexion-extension ROM [95% CI (-0.32, 5.51);
P=0.08] between the two groups. Theoretically, the RHA group should
achieve better ROM of the forearm during early functional exercise
due to its better stability (39).
However, this result shows that the ROM advantage of the RHA group
is not evident compared with the ORIF group. We hypothesize that
this may be related to the difficulty in choosing the ideal height
and size of the prosthesis during RHA surgery. Inappropriate
prosthesis may lead to changes in the alignment of the elbow joint,
thereby limiting the ROM of the forearm (40).
In summary, although ORIF can achieve good
functional scores after surgery, RHA can still achieve comparable
functional scores even with poor soft tissue conditions, and leads
to better forearm rotation ROM with fewer complications. Therefore,
in the treatment of radial head fractures of TTIE, RHA is superior
to ORIF.
The present study still has the following
shortcomings, which need to be further investigated and improved:
i) A total of 15 publications were included in the present
meta-analysis and systematic review, of which no randomized
controlled trials were included, and the number of studies was not
sufficient; ii) the Jadad score was used to evaluate the included
non-randomized controlled studies; iii) certain literature that met
the inclusion criteria failed to provide detailed classification of
radial head fractures, therefore conducting a detailed group study
of the results according to fracture classification was not
possible, and the surgical techniques varied between different
literature, which would produce certain bias; iv) regarding outcome
measures, a maximum of 13 articles and a minimum of 6 articles were
included in the same evaluation method, thereby slightly increasing
the heterogeneity between groups; v) furthermore, the difference in
the final follow-up time within the literature may have a certain
impact on the results, and the longer-term efficacy is unknown.
Therefore, the above conclusions need to be further verified by
more randomized controlled studies with large samples. Due to the
lack of included literature, the conclusions of the present study
may be different from the actual situation, thus further follow-up
is needed. It would be beneficial if more literature reports were
to emerge in the future to reduce bias, so that more authentic and
reliable conclusions can be drawn.
Acknowledgements
Not applicable.
Funding
Funding: Funding for the present study was provided by the
Scientific and Technological Innovation Project of Higher Education
Institutions of Shanxi Province (grant no. 2020L0388), the
Scientific Research Project of Health Commission of Shanxi Province
(grant no. 2020133) and the Doctoral Research Start-up Fund Project
(grant no. BS202004).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XYL and YLW were responsible for the design of the
current study, and both performed the statistical analysis. XYL and
YLW confirmed the authenticity of all the raw data. SY is
responsible for the acquisition and sorting of data. PFH performed
the interpretation of the data. All authors have read and approved
the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ohl X and Siboni R: Surgical treatment of
terrible triad of the elbow. Orthop Traumatol Surg Res. 107 (Suppl
1)(S102784)2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hotchkiss RN: Fractures and dislocations
of the elbow. In: Rockwood CA, Green DP Jr, Bucholz RW and Heckman
JD (eds). Rockwood and Green's Fractures in Adults. 4th edition.
Vol 1. Lippincott-Raven, Philadelphia, PH, pp929-1024, 1996.
|
|
3
|
Ma CH, Hsueh YH, Wu CH, Yen CY and Tu YK:
Does an internal joint stabilizer and standardized protocol prevent
recurrent instability in complex persistent elbow instability? Clin
Orthop Relat Res. 480:1354–1370. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Chen HW and Huang SM: Risk factors of
efficacy for patients receiving surgical treatment following
terrible triad of the elbow joint: A comparative study. Medicine
(Baltimore). 98(e13836)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Giannicola G, Sessa P, Calella P, Gumina S
and Cinotti G: Chronic complex persistent elbow instability: A
consecutive and prospective case series and review of recent
literature. J Shoulder Elbow Surg. 29:e103–e117. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Reinares F, Rojas N, Calvo A, Aravena C,
Rieutord JP, Callejas O, Montegu R and Paccot D: Results of
standardized treatment of elbow fracture dislocations as per their
injury pattern: A retrospective cohort of 89 patients. JSES Int.
5:588–596. 2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mathew PK, Athwal GS and King GJ: Terrible
triad injury of the elbow: Current concepts. J Am Acad Orthop Surg.
17:137–151. 2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kusnezov N, Eisenstein E, Dunn JC, Fares
A, Mitchell J, Kilcoyne K and Waterman BR: Operative management of
unstable radial head fractures in a young active population. Hand
(NY). 13:473–480. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Carroll PJ and Morrissey DI: Posterior
(Boyd) approach to terrible triad injuries. JSES Int. 6:315–320.
2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Galbiatti JA, Cardoso FL, Ferro JAS, Godoy
RCG, Belluci SOB and Palacio EP: Terrible triad of the elbow:
Evaluation of surgical treatment. Rev Bras Ortop. 53:460–466.
2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Chen H, Shao Y and Li S: Replacement or
repair of terrible triad of the elbow: A systematic review and
meta-analysis. Medicine (Baltimore). 98(e13054)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kyriacou S, Gupta Y, Bains HK and Singh
HP: Radial head replacement versus reconstruction for the treatment
of the terrible triad injury of the elbow: A systematic review and
meta-analysis. Arch Orthop Trauma Surg. 139:507–517.
2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Afifi A, Lymona AM and Galal S: Radial
head fixation vs replacement in terrible triad: Preliminary results
of a prospective cohort study with patient reported outcome. Indian
J Orthop. 54 (Suppl 2):S254–S259. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hou F, Liang X, Fan W, Zhao F and Li D:
Analysis of twenty-five cases of terrible triad injury of the elbow
surgically treated with a single lateral approach. Int Orthop.
45:241–246. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Klug A, Nagy A, Gramlich Y and Hoffmann R:
Surgical treatment of the radial head is crucial for the outcome in
terrible triad injuries of the elbow. Bone Joint J.
102-B:1620–1628. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zheng WK, Tang JF, Ge T and Cai WS: Choice
of management strategy for Hotchkiss Ⅲ fracture of radial head in
the terrible triad of elbow joint: Internal fixation or
replacement? Lingnan Mod Clin Surg. 20:496–502. 2020.
|
|
17
|
Higgins JP, Altman DG, Gøtzsche PC, Jüni
P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, et
al: The cochrane collaboration's tool for assessing risk of bias in
randomised trials. BMJ. 343(d5928)2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jadad AR, Moore RA, Carroll D, Jenkinson
C, Reynolds DJ, Gavaghan DJ and McQuay HJ: Assessing the quality of
reports of randomized clinical trials: Is blinding necessary?
Control Clin Trials. 17:1–12. 1996.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Giannicola G, Calella P, Piccioli A,
Scacchi M and Gumina S: Terrible triad of the elbow: Is it still a
troublesome injury? Injury. 46 (Suppl 8):S68–S76. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jeong WK, Oh JK, Hwang JH, Hwang SM and
Lee WS: Results of terrible triads in the elbow: The advantage of
primary restoration of medial structure. J Orthop Sci. 15:612–619.
2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Leigh WB and Ball CM: Radial head
reconstruction versus replacement in the treatment of terrible
triad injuries of the elbow. J Shoulder Elbow Surg. 21:1336–1341.
2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Li B, Liu D and Li J: Clinical effect of
prosthesis replacement and microplate internal fixation in the
treatment of triad of elbow joint with comminuted fracture of the
radial head. China Coal Ind Med. 21:498–501. 2018.
|
|
23
|
Liu G, Ma W, Li M, Feng J, Xu R and Pan Z:
Operative treatment of terrible triad of the elbow with a modified
Pugh standard protocol: Retrospective analysis of a prospective
cohort. Medicine (Baltimore). 97(e0523)2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Matar HE, Akimau PI, Stanley D and Ali AA:
Surgical treatment of Monteggia variant fracture dislocations of
the elbow in adults: Surgical technique and clinical outcomes. Eur
J Orthop Surg Traumatol. 27:599–605. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Pierrart J, Bégué T and Mansat P: GEEC.
Terrible triad of the elbow: Treatment protocol and outcome in a
series of eighteen cases. Injury. 46 (Suppl 1):S8–S12.
2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Toros T, Ozaksar K, Sügün TS, Kayalar M,
Bal E and Ada S: The effect of medial side repair in terrible triad
injury of the elbow. Acta Orthop Traumatol Turc. 46:96–101.
2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Watters TS, Garrigues GE, Ring D and Ruch
DS: Fixation versus replacement of radial head in terrible triad:
Is there a difference in elbow stability and prognosis? Clin Orthop
Relat Res. 472:2128–2135. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yan M, Ni J, Song D, Ding M, Liu T and
Huang J: Radial head replacement or repair for the terrible triad
of the elbow: Which procedure is better? ANZ J Surg. 85:644–648.
2015.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zhang C, Zhong B and Luo CF: Treatment
strategy of terrible triad of the elbow: Experience in Shanghai 6th
people's hospital. Injury. 45:942–948. 2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
van Riet RP, van den Bekerom M, Van Tongel
A, Spross C, Barco R and Watts AC: Radial head fractures. Shoulder
Elbow. 12:212–223. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Mebouinz FN, Kasse A and Habib Sy M:
Results of radial head resection after Mason type 3 or 4 fracture
of the elbow. Clin Shoulder Elb. 23:131–135. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Chaijenkij K, Arirachakaran A and
Kongtharvonskul J: Clinical outcomes after internal fixation,
arthroplasty and resection for treatment of comminuted radial head
fractures: A systematic review and network meta-analysis.
Musculoskelet Surg. 105:17–29. 2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ryu SM, Park SG, Kim JH, Yang HS, Na HD
and Seo JS: Treatment of modified mason type III or IV radial head
fracture: Open reduction and internal fixation versus arthroplasty.
Indian J Orthop. 52:590–595. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Yang HS, Kim JW, Lee SH and Yoo BM:
Comminuted radial head fracture in all-arthroscopic repair of elbow
fracture-dislocation: Is partial excision of the radial head an
acceptable treatment option? Clin Shoulder Elb. 21:234–239.
2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Adams JE, Sems SA and Steinmann SP: Open
treatment of radial head fractures. JBJS Essent Surg Tech.
7(e35)2017.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Hemmingsen CK, Thillemann TM, Elmengaard
B, Raedt S, Nielsen ET, Mosegaard SB, Stentz-Olesen K and Stilling
M: Elbow biomechanics, radiocapitellar joint pressure, and
interosseous membrane strain before and after radial head
arthroplasty. J Orthop Res. 38:510–522. 2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Scoscina D, Facco G, Luciani P, Setaro N,
Senesi L, Martiniani M and Gigante AP: Mason type III fractures of
the radial head: ORIF, resection or prosthetic replacement?
Musculoskelet Surg: Apr 16, 2022 (Epub ahead of print).
|
|
38
|
He X, Fen Q, Yang J, Lei Y, Heng L and
Zhang K: Risk factors of elbow stiffness after open reduction and
internal fixation of the terrible triad of the elbow joint. Orthop
Surg. 13:530–536. 2021.PubMed/NCBI View
Article : Google Scholar
|
|
39
|
Ostergaard PJ, Tarabochia MA, Hall MJ,
Dyer G, Earp BE, Blazar P and Zhang D: What factors are associated
with reoperation after operative treatment of terrible triad
injuries? Clin Orthop Relat Res. 479:119–125. 2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Marcheix PS, Cuenca C, Vergnenegre G,
Mabit C, Hardy J and Charissoux JL: Factors influencing the
mid-term radiological and functional outcomes of 41 post-fracture
bipolar radial head arthroplasty cases at a mean follow-up of 87
months. Orthop Traumatol Surg Res. 107(102818)2021.PubMed/NCBI View Article : Google Scholar
|