Introduction
Vesicovaginal fistula is an abnormal anatomical
passage between the bladder and vagina and is mainly characterized
by spontaneous vaginal leakage. It is one of the most common types
of genitourinary fistulas in women, and it markedly affects the
patients' quality of life and physical and mental health (1-3).
Vesicovaginal fistula is most commonly related to iatrogenic
injuries, including gynecological and pelvic tumor surgeries as
well as radiotherapy, with abdominal hysterectomy as its most
common cause (1). Its diagnosis is
mainly based on the patient's clinical symptoms, including
persistent vaginal leakage, genital itching and pain, macerated
dermatitis, and recurrent urogenital infection. The diagnosis may
be confirmed using imaging methods, such as intravenous pyelography
or computed tomography urography (CTU). The bladder methylene blue
injection test and cystoscopy may further clarify the location,
size, and number of fistulas, along with other relevant
information.
At present, the treatment methods for vesicovaginal
fistula vary, each having its advantages and disadvantages. In
general, for treating newly formed and simple vesicovaginal
fistulas, conservative continuous bladder drainage may be adopted
(4), along with an indwelling
catheter placement for 3-4 weeks. Concurrently, antibiotics should
be used to prevent infections. If conservative treatment fails,
surgical repair is recommended (5). Surgical repairs are categorized as
follows (6-9):
i) transabdominal repair for patients with poor vaginal
conditions-laparoscopic or robotic-assisted laparoscopic repair is
recommended; ii) repair through the bladder for high bladder
fistulas located in the upper part of the bladder trigone and
bottom of the bladder; iii) transvaginal repair for patients with
sufficient vaginal volume, soft vaginal wall with good blood
supply, and sufficient healthy tissue in the vaginal wall around
the fistula; iv) filling with a pedunculated graft, at times used
in complex cases, as in patients with poor local tissue condition
after radiotherapy; v) urinary diversion, a palliative treatment
that may be performed after failed treatments for complex
vesicovaginal fistulas, or when repair is difficult due to poor
local tissue conditions.
At present, there is no unified standard protocol
for optimal operative timing and methods of treatment, as all the
above methods have their own advantages and disadvantages. These
methods are associated with either prolonged treatment or
substantial trauma. The present study reports a case of
vesicovaginal fistula that was successfully treated with bilateral
ureteral single J-tube placement and drainage through a suprapubic
bladder puncture with indwelling catheterization.
Case report
A 56-year-old woman was admitted to the Department
of Urology of Hexi University Affiliated Zhangye People's Hospital
(Zhangye, China) due to vaginal leakage for 1 week, occurring 22
days after hysterectomy. The patient had undergone laparoscopic
total hysterectomy and bilateral salpingectomy at the gynecology
department of our hospital in late November 2020 for multiple
uterine leiomyomas, stress urinary incontinence, and stage II
anterior vaginal wall prolapse. The patient had intermittent fever
after surgery and received anti-infective drug therapy. The patient
was discharged from the hospital after the fever subsided. In early
December 2020, 1 week after surgery, the patient noted a large
amount of clear vaginal discharge. The patient had no frequent
urination, urinary urgency or fever. During admission, a large
amount of clear vaginal discharge was observed. The vaginal mucosa
was smooth and rosy. The suspected diagnosis was vesicovaginal
fistula due to hysterectomy.
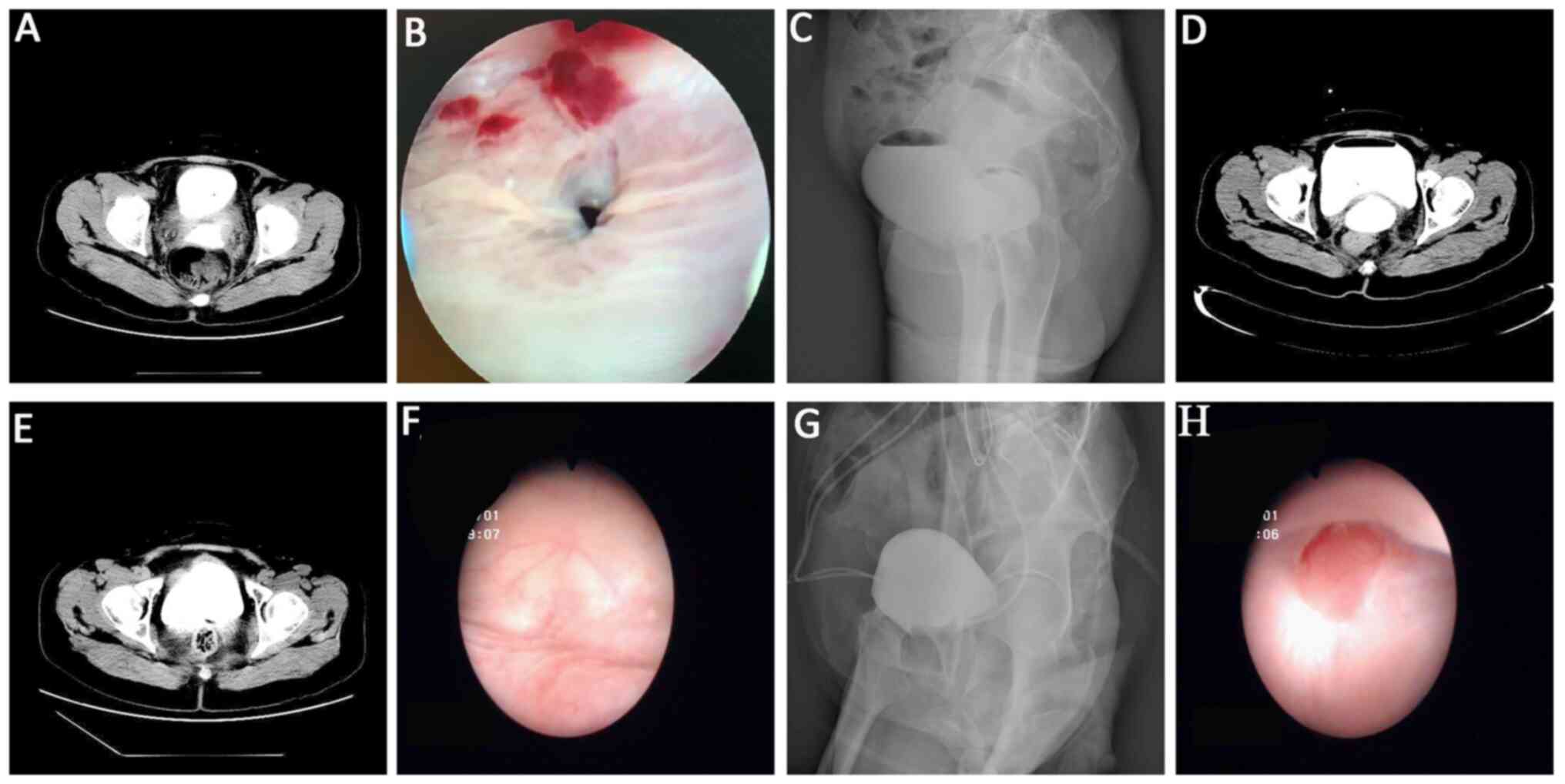
CTU examination indicated a liquid-density shadow at
the operative site connecting the bladder and vagina, and enhanced
images revealed contrast agent overflow, suggesting the presence of
a vesicovaginal fistula. During cystoscopy, the bilateral ureteral
orifices were clearly visible, and a fistula of approximately 1 cm
in diameter was noted in the posterior bladder wall (Video S1). The stump suture and fistula
were visible through the vagina. Cystography was performed using
250 ml of iodofluorohydrin-sodium chloride solution injected
through the catheter, revealing an accumulation of contrast medium
behind the bladder, with a circular appearance. Furthermore, the
upright plain radiograph revealed an air-fluid level in the bladder
and contrast medium extravasation. Immediately following the
cystography, a full-abdominal CT examination was performed, and it
displayed contrast medium at the operative site, suggesting the
presence of a vesicovaginal fistula (Fig. 1). The patient's final diagnosis was
post-hysterectomy vesicovaginal fistula.
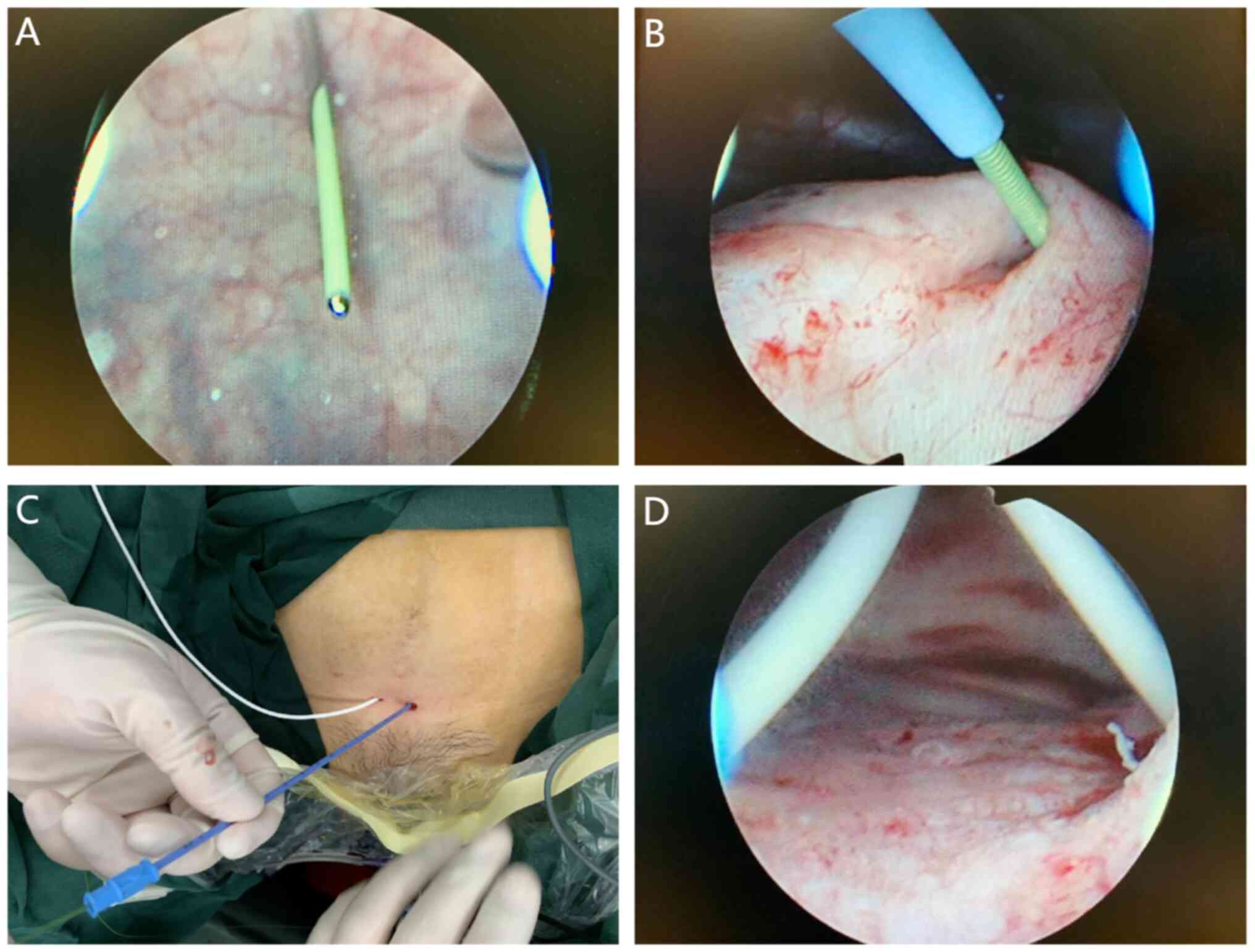
After explaining the procedure to the patient and
obtaining written informed consent, a bilateral ureteral single
J-tube placement and drainage through a suprapubic bladder puncture
with indwelling catheterization were performed. First, a
resectoscope was inserted into the bladder through the urethra for
examination, revealing slit-shaped bilateral ureteral orifices and
normal peristaltic effluent. A fistula was visible on the posterior
bladder wall, with an approximate diameter of 1 cm. Vaginal
examination revealed the absorbable sutures at the vaginal stump
and a fistula on the anterior wall. A ureteroscope was used to
enter the bladder through the urethra, and both ureteral lumens
were checked for patency under the guidance of a zebra wire. The
ureteroscope was replaced with the resectoscope, and the bladder
was entered through the urethra. After filling the bladder with
isotonic sodium chloride solution, bladder puncture was performed
using a 20-ml syringe needle, which was inserted 2 cm above the
pubic bone in the midline. The puncture needle smoothly entered the
bladder, and a guide wire was placed through the inner core of the
puncture needle. An 8-F dilation tube was used to expand the
puncture channel after withdrawing the needle. The resectoscope was
replaced with a nephroscope, again entering the bladder through the
urethra. With the aid of forceps, the guide wire and the front end
of the single J-tube was slowly inserted into the ureteral orifice
(Video S2). A single J-tube was
successfully placed into each ureter and properly attached to the
skin with sutures, with the end of each connected to a sterile
drainage bag. Subsequently, a catheter was inserted, and the
operation was successfully completed (Fig. 2). The urine drainage volumes from
the catheter and single J-tubes were closely observed after the
operation. The drainage output of the J-tube in each ureter was
satisfactory. Most of the urine drained through the J-tubes; the
daily urine volume through the urinary catheter was <10 ml. The
urinary catheter was removed 1 week after the minimally invasive
drainage treatment, improving the patient's quality of life. At 3
months postoperatively, a follow-up CTU (Fig. 1E), cystoscopy (Fig. 1F), cystography (Fig. 1G), and colposcopy (Fig. 1H) confirmed complete healing of the
vesicovaginal fistula, and both ureteral J-tubes were removed. No
urinary catheter was placed after the J-tubes were removed, because
the injury was minimal and located on the anterior bladder wall.
After the J-tubes were removed, the patient was monitored for
symptoms such as fever or lower abdominal pain. At the 6-month and
1-year follow-ups, there was no urinary incontinence, bladder
spasm, vaginismus, or any other complications. The patient was
satisfied with the treatment outcomes.
Discussion
Vesicovaginal fistula is the most common type of
female genitourinary fistula and has serious physical and
psychological effects (3,10,11).
Considering the iatrogenic causes of the disease, physicians are
cautious regarding its diagnosis and treatment, and the final
diagnosis may only be confirmed by standard and convincing evidence
(10). The treatment plan for this
disease must also be carefully designed, particularly when surgery
is to be performed. A reasonable surgical plan is required to
ensure operational success, as the local condition of the operative
site is optimal during the first operation, providing the greatest
probability of treatment success (12,13).
If the first repair fails, the subsequent treatment attempts may
encounter difficulties. However, there is currently no unified
standard protocol for the optimal route and timing of surgical
treatment of vesicovaginal fistulas (1,10,13-15).
The adverse consequences of urinary leakage not only
markedly affect the patients' physical and mental health, but also
cause great psychological distress to the surgeon who caused the
fistula (16). Thus, it is
important to remedy the condition and help the patients reintegrate
back into the community as soon as possible (17). However, for open surgery or
laparoscopic repair, patients are generally required to wait 10-12
weeks; during this period, the local inflammation of the fistula
subsides, the scar softens, and the local tissue obtains adequate
blood supply, leading to the best possible surgical conditions
(13,18). However, during this time, patients
continue to endure the physical and mental distress of urinary
leakage, which significantly affects their quality of life
(11,19). Traditional repair surgery, whether
through the abdominal, bladder, or vaginal route, causes secondary
trauma and carries a risk of complications, such as fistula
recurrence, urinary incontinence, vaginismus, and bladder spasm
(9,12).
It is important to identify the optimal method for
early treatment of vesicovaginal fistulas - a treatment that not
only relieves the physical pain and psychological distress from
urinary leakage, but also creates favorable conditions for fistula
healing and minimizes postoperative trauma and complications. Such
a method would be beneficial for both doctors and patients. The new
surgical method presented in the current study completely addresses
the current dilemma of long waiting time for patients with small,
new-onset vesicovaginal fistulas for secondary surgical treatment.
After discussion with our multi-disciplinary treatment team, we
decided to perform a minimally invasive procedure-single J-tube
placement and drainage in the bilateral ureters through a
suprapubic bladder puncture-for the present case. The surgical
outcome was good, the reexamination findings were satisfactory, and
the patient was satisfied with the treatment outcome. The fistula
in this patient was approximately 1 cm in diameter; therefore, we
may assume that the method is safe in patients with fistulas <1
cm. Mechanical bladder injuries are easier to repair; however, our
method may potentially be used for small thermal injuries, as the
method of treatment is the same for both types of injury. Our
reasoning is that if the bladder is kept in a low-tension state and
free of urine, the small fistulas heal naturally. Previous studies
have reported that conservative treatment of bladder rupture with
an indwelling catheter may be successful for small mechanical
injuries, just as in transurethral resection of bladder tumors;
small gaps leading to bladder rupture may also be treated
conservatively with an indwelling catheter (4,5). The
approach of the present study is more precise than using an
indwelling catheter, as the ureteral effluent is completely drained
through a single J-tube, and the bladder maintains a relatively dry
and clean microenvironment, which is helpful for healing a
vesicovaginal fistula. The procedure has not been attempted to
treat a 3-cm fistula; however, it may be possible to pursue this in
order to expand patient reports and develop more precise treatment
plans.
Single J-tube placement in the bilateral ureters for
drainage through a suprapubic bladder puncture with indwelling
catheterization is an effective method for treating vesicovaginal
fistulas. It utilizes common urological techniques and surgical
instruments used for inspection procedures, making it simple and
convenient to perform. This minimally invasive method has few
complications, and because the approach has no treatment delay, it
immediately reduces the physical and mental stress experienced by
patients due to urinary leakage, thereby improving their quality of
life. There are still certain limitations to this study. Although
the patient had no urinary incontinence, bladder spasm, vaginismus,
or other complications after surgery, this study is only one case
report, and a case series study and comparisons with other
treatment modalities are still required to verify the efficacy of
this treatment. In addition, follow-up is required to determine the
long-term treatment effect of this approach.
Supplementary Material
Cystoscopy revealed clearly visible
bilateral ureteral orifices and a fistula of approximately 1 cm in
diameter in the posterior bladder wall.
Under the guidance of the guide wire,
a single J-tube was slowly inserted into the ureteral orifice.
Video S1
Video S2
Acknowledgements
Not applicable.
Funding
Funding: This study was funded by grants from Gansu Province
Science and Technology Planning Project (grant no. 20JR10RG310) and
the Higher Education Innovation Development Fund of Gansu Province
(grant no. 2020B-200).
Availability of data and materials
All data generated and analysed during this study
are included in this published article.
Authors' contributions
SHN, YPL and FYY contributed to the drafting of the
manuscript and the design of the study. ST, SJN, JQ and JXY
contributed substantially to the conceptualization and design of
the study, as well as the completion of the surgery. FYY and JXY
approved the final version of the manuscript for publication. Data
authentication is not applicable. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was performed according to the guidelines
of the Declaration of Helsinki and was approved by the Ethics
Committee of Hexi University Affiliated Zhangye People's Hospital
(Zhangye, China). Written informed consent was obtained from the
patient.
Patient consent for publication
Written consent was obtained from the patient for
publication of the patient's data/images in this manuscript.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hillary CJ, Osman NI, Hilton P and Chapple
CR: The aetiology, treatment, and outcome of urogenital fistulae
managed in well- and low-resourced countries: A systematic review.
Eur Urol. 70:478–492. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Marks P, Kluth LA, Lang IJ and Fisch M:
Vesicovaginal fistulas: Diagnosis and surgical management. Urologe
A. 59:432–441. 2020.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
3
|
Raji MO, Raji IA, Hassan M, Raji HO,
Bashir AM, Suleiman IN and Abubakar HU: Assessment of
health-related quality of life of vesicovaginal fistula patients
attending a repair center in Northwest Nigeria. Ann Afr Med.
20:132–137. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fouad LS, Chen AH, Santoni CJ, Wehbe C and
Pettit PD: Revisiting conservative management of vesicovaginal
fistula. J Minim Invasive Gynecol. 24:514–515. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
He Z, Cui L, Wang J, Gong F and Jia G:
Conservative treatment of patients with bladder genital tract
fistula: Three case reports. Medicine (Baltimore).
99(e21430)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Pope R and Beddow M: A review of surgical
procedures to repair obstetric fistula. Int J Gynaecol Obstet. 148
(Suppl 1):S22–S26. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Thayalan K, Parghi S, Krause H and Goh J:
Vesicovaginal fistula following pelvic surgery: Our experiences and
recommendations for diagnosis and prompt referral. Aust N Z J
Obstet Gynaecol. 60:449–453. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kim M, Park N and Yun H: Factors affecting
surgical treatment and outcomes of vesico-vaginal fistula: A
retrospective study. Asian J Surg. 44:427–428. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mörgeli C and Tunn R: Vaginal repair of
nonradiogenic urogenital fistulas. Int Urogynecol J. 32:2449–2454.
2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lee D and Zimmern P: Vaginal approach to
vesicovaginal fistula. Urol Clin North Am. 46:123–133.
2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fujisaki A, Kinjo M, Shimoinaba M, Honda S
and Yoshimura Y: An evaluation of the impact of post-hysterectomy
vesicovaginal fistula repair on the mental health of patients in a
developed country. Int Urogynecol J. 31:1371–1375. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Malik MA, Sohail M, Malik MT, Khalid N and
Akram A: Changing trends in the etiology and management of
vesicovaginal fistula. Int J Urol. 25:25–29. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Breen M and Ingber M: Controversies in the
management of vesicovaginal fistula. Best Pract Res Clin Obstet
Gynaecol. 54:61–72. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ramphal SR: Laparoscopic approach to
vesicovaginal fistulae. Best Pract Res Clin Obstet Gynaecol.
54:49–60. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Moses RA and Ann Gormley E: State of the
art for treatment of vesicovaginal fistula. Curr Urol Rep.
18(60)2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chen GD, Rizk DEE and Richter HE: Surgical
repair of vesico-vaginal fistula: the need for an evidence-based
approach. Int Urogynecol J. 30:169–170. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wella K, Chilemba E, Namathanga A and
Chakhame B: Social support for women after fistula repair: A
scoping review. Sex Reprod Healthc. 29(100649)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Rajaian S, Pragatheeswarane M and Panda A:
Vesicovaginal fistula: Review and recent trends. Indian J Urol.
35:250–258. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Giusti G and De Lisa A: Repair of
post-hysterectomy vesicovaginal fistulae: the state of the art.
Urologia. 82:10–21. 2015.PubMed/NCBI View Article : Google Scholar : (In Italian).
|