Introduction
Vaginal leiomyoma is a rare benign solid tumor that
typically occurs in females of reproductive age (1). It usually originates from the
anterior vaginal wall and exhibits a single nodular growth pattern.
The clinical manifestations depend on the size and location of the
tumor and include dyspareunia, abdominal pain and dysuria. Vaginal
leiomyomas may occur with leiomyomas in other parts of the body.
Careful assessment is required for clinical diagnosis, as this
condition may be easily misdiagnosed (2). Care should be taken during its
clinical diagnosis, as it may easily be misdiagnosed as a
cystocele, urethral bulge, uterine prolapse, urethral diverticulum,
vaginal cyst, vaginal cancer, cervical cancer or vaginal sarcoma
(3). The diagnosis is usually
confirmed through histopathological examination. The present case
was reported to increase awareness of the disease and reduce the
likelihood of its misdiagnosis and incorrect treatment.
Case report
A 48-year-old female presented at the Emergency
Department of a external hospital with a 2-day history of vaginal
bleeding and a prolapsed hard vaginal mass, which was goose
egg-sized. On examination, there was heavy vaginal bleeding with
blood clots. Subsequently, the patient observed a hard mass that
was the size of a goose egg in the vagina. The mass was able to be
retracted when the patient was in the supine position, but it
prolapsed when the patient stood or squatted. The patient also
experienced urinary incontinence when coughing or sneezing. Pelvic
magnetic resonance imaging (MRI) performed at another hospital
indicated cervical cancer. As the exact diagnosis was unclear, the
patient visited the gynecological clinic of Hexi University
Affiliated Zhangye People's Hospital (Zhangye, China) in July 2021.
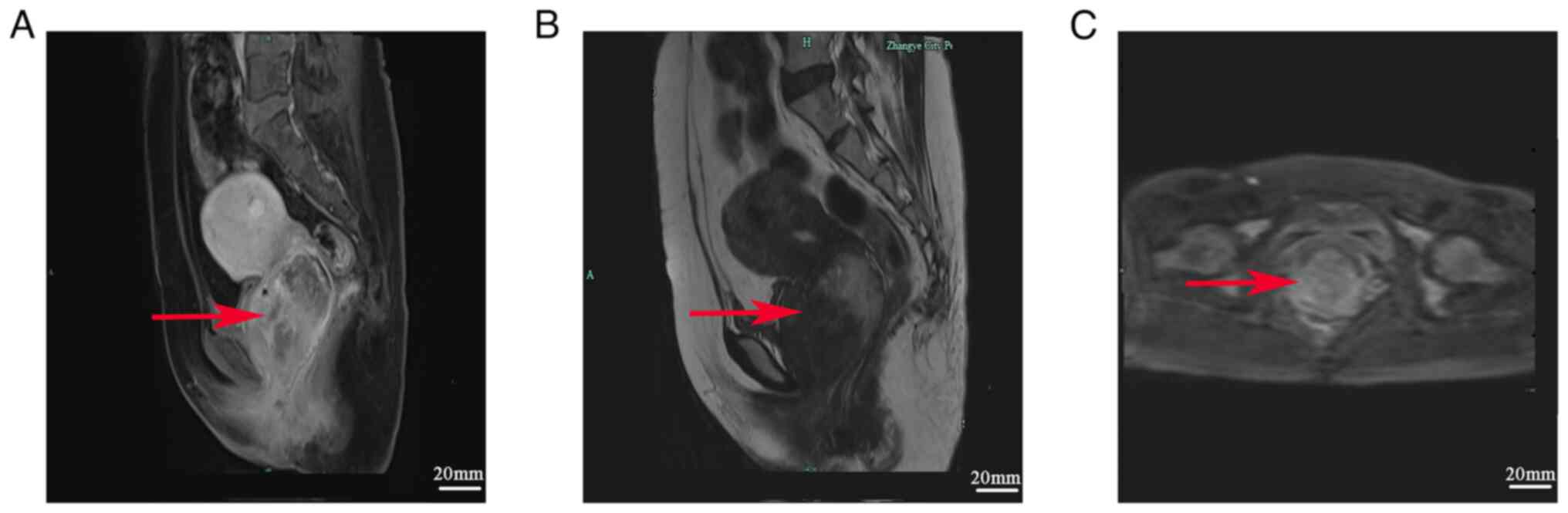
Lower abdominal diffusion-weighted MRI performed on the first day
after admission at Hexi University Affiliated Zhangye People's
Hospital (Zhangye, China) revealed a soft tissue mass of ~65x46 mm
at the anterior vaginal wall. The mass was isointense on
T1-weighted imaging, iso-to hypointense on T2-weighted imaging and
slightly hyperintense on diffusion-weighted imaging. Apparent
diffusion coefficient imaging with a b-value of 800 revealed the
tumor contour, and contrast-enhanced imaging revealed progressive
and uneven enhancement. The solid mass was considered to be
cervical cancer (Fig. 1).
A biopsy specimen of the mass was procured in the
outpatient department of our hospital and pathological staining
showed debris without structure. The patient was admitted to the
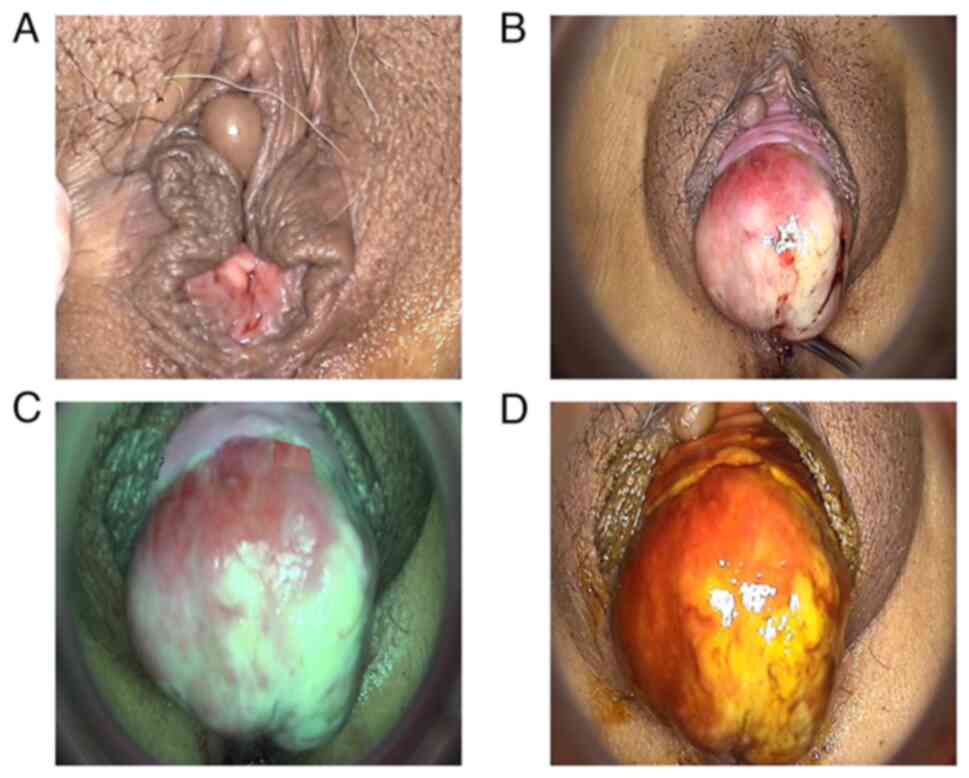
hospital for further diagnosis and treatment. Gynecological
examination revealed a 10x8 mm cystic neoplasm at the labia minora
and hardening of the middle third of the anterior vaginal wall
(Fig. 2A and B). A 65x46 mm solid, non-tender mass with
hyperemia and superficial edema, but without obvious ulceration,
was noted in the anterior vaginal wall. The mass was covered with
necrotic and purulent yellow tissue. After the tumor was plugged
back into the vagina, a slight increase in abdominal pressure was
sufficient to prolapse it. Vulval development was normal, no
abnormalities of the labia majora were detected, the cervix and
uterus were normal in size, the cervical surface was smooth and
there were no obvious abnormalities in the double appendage area.
Pelvic organ prolapse measurement was performed. The results of
Pelvic Organ Prolapse Quantification System (POP-Q) staging were as
follows (4-6):
Anterior vaginal wall, POP-Q III; uterus, POP-Q I; and posterior
vaginal wall, POP-Q 0 (Table
I).
 | Table IPOP staging of the patient. |
Table I
POP staging of the patient.
| | Preoperative | Immediately
post-surgery | 3 months
post-surgery |
|---|
| Location | Distance from Aa/Ap
to hymen | Distance from vaginal
fornix to fornix to Aa/Ap | Distance from the top
of the vagina to the edge of the hymen | POP-Q score | Distance from Aa/Ap
to hymen | Distance from vaginal
fornix to Aa/Ap | Distance from the top
of the vagina to the edge of the hymen | POP-Q score | Distance from Aa/Ap
to hymen | Distance from vaginal
fornix to Aa/Ap | Distance from the top
of the vagina to the edge of the hymen | POP-Q score |
|---|
| Anterior vaginal
wall | +3Aa | +8Ba | -4C | III | +1Aa | +1Ba | -8C | II | 0Aa | 0Ba | -8C | II |
| Uterus | 7.5Gh | 3Pb | 10TVL | I | 6.5Gh | 3Pb | 10TVL | 0 | 5.0Gh | 3Pb | 10TVL | 0 |
| Posterior vaginal
wall | -3Ap | -3Bp | -10D | 0 | -3Ap | -3Bp | -10D | 0 | -3Ap | -3Bp | -10D | 0 |
On colposcopy, when the vulva was fully exposed, the
prolapsed mass was visible inside the vagina; however, on breath
holding, the mass was visible at the middle third of the anterior
vaginal wall. The tumor was solid and covered by necrotic and
purulent yellow tissue. There were local congestion and edema but
no obvious ulceration. The acetic acid test was performed but
whitening of the epithelium was not noted. No irregular vascular
shadow was observed under green light or after iodine staining
(Fig. 2C and D). The gynecological examination of this
patient indicated that the cervix was smooth and hypertrophic, and
due to the special location of the fibroids in the anterior vaginal
wall, the placement of the speculum was affected and it was not
possible to fully expose the fibroid. The speculum was therefore
not placed and it was difficult to obtain images, and no picture
data are thus available. Histopathological examination of the
biopsy specimen obtained under colposcopy revealed eosinophilic
granuloma. The patient initially went to the doctor with the main
complaint of ‘prolapse of vaginal mass for 2 days after vaginal
bleeding’. At our hospital, it was confirmed that the patient's
vaginal bleeding did not arise from the anterior vaginal wall
tumor. Through cervical cancer and HPV testing, cervical lesions
and cervical cancer were excluded as the cause of the vaginal
bleeding. Therefore, a hysteroscopy was performed to further
clarify the source of the vaginal bleeding. Endometrial polyps were
found during hysteroscopy, which were the cause of the vaginal
bleeding. The endometrium was thin and pale, and the openings of
both fallopian tubes were visible. The cervical canal exhibited no
irregularities. Based on these findings, the patient was diagnosed
with endometrial polyps. According to the patient's symptoms and
the above examination results, the patient's preoperative diagnosis
was benign vaginal tumor, malignant cannot be excluded; uterine
polyps; and labia minora cyst.
Hence, the patient underwent surgical resection.
First, the bladder stone site was identified and disinfected. The
urinary catheter was retained and the course of the urethra was
explored, without disturbing the urethra and bladder. The vagina
was then sterilized and the anterior vaginal wall tumor was exposed
using a vaginal retractor. The upper and lower poles of the tumor
root, in the anterior vaginal wall, were clamped with forceps for
fixation and a transverse incision of ~6-7 cm was made along the
junction of the tumor root and vaginal wall. The incision was made
deep enough to reach the tumor surface capsule and the connective
tissue between the tumor and vaginal wall was bluntly separated.
The blood vessels of the tumor were cut off and ligated with a silk
thread to arrest the bleeding completely. Excess vaginal wall
tissue was trimmed and the intraluminal space between the ends was
closed by suturing with 2-0 absorbable thread; 1-0 absorbable
thread was used for suturing continuously and longitudinally along
the vaginal wall and no bleeding was noted on the wound surface. A
gauze roll was placed in the closed vagina to provide compression
for avoiding bleeding; it was removed 24 h after surgery.
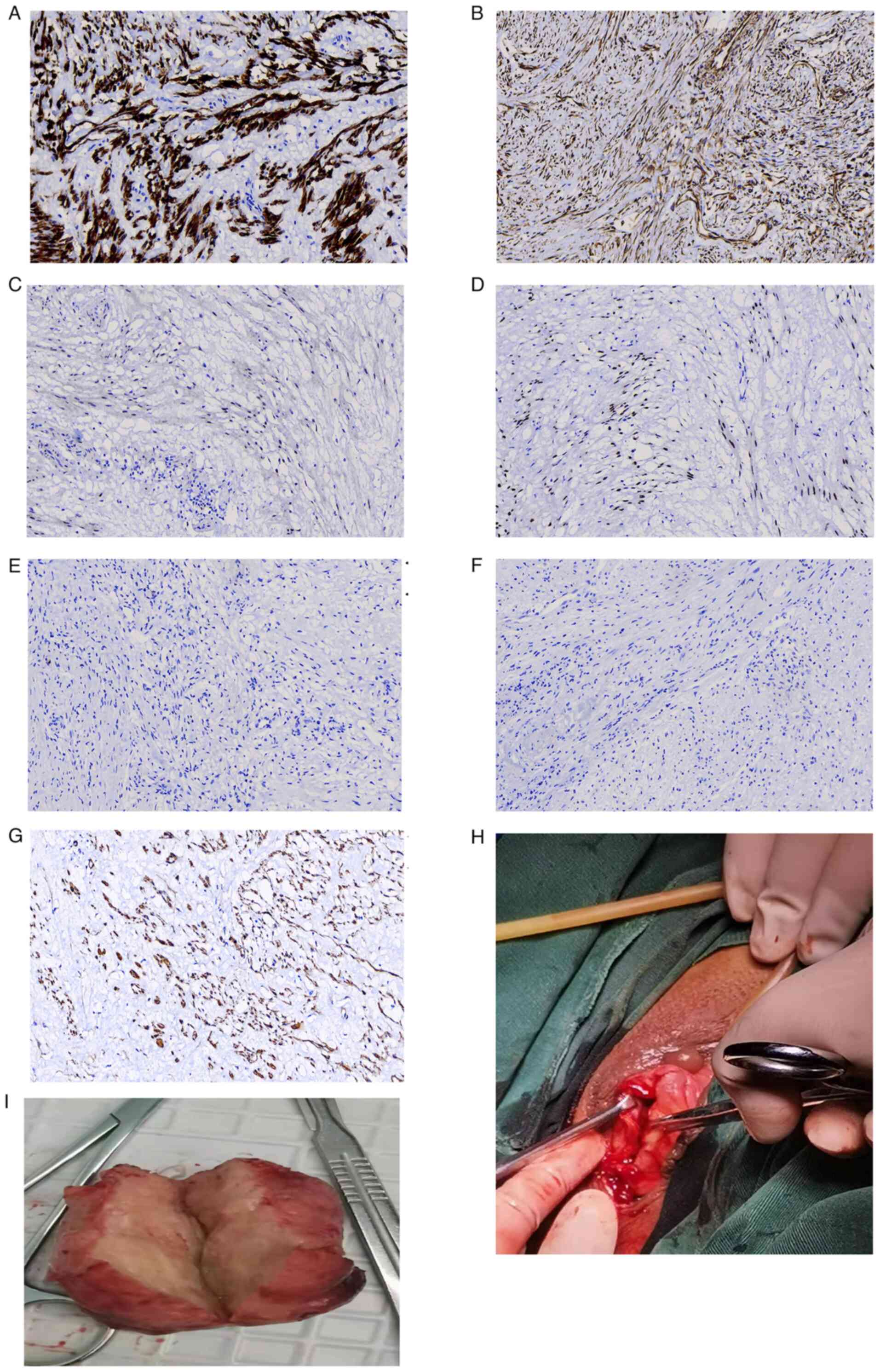
Frozen-section analysis revealed that the lesion was benign.
Therefore, simple mass resection was performed. Postoperative
immunohistochemical analysis (4)
indicated that the samples were positive for desmin and smooth
muscle actin, and negative for CD34 (cat. no. Kit-0004), S100 (cat.
no. Kit-0007) and STAT6 (cat. no. RMA-0845; all ready-to-use
without dilution; all from Fuzhou Maixin Biotechnology Development
Co., Ltd). Based on the histomorphology that was performed
according to standard protocols and immunohistochemistry results,
the patient was pathologically diagnosed with vaginal leiomyoma
(Fig. 3). Following this, the
pelvic organ prolapse was measured again. The results of the
postoperative POP-Q staging were as follows (5-7):
Anterior vaginal wall, POP-Q II; uterus, POP-Q 0; and posterior
vaginal wall, POP-Q 0. The patient recovered well after surgery: At
6 h postoperatively, the patient was able to eat normally; at 1 day
postoperatively, the patient passed flatus and stool, and 3 days
postoperatively, the urinary catheter could be removed, as the
incontinence resolved; the patient had no increased urinary
frequency or urgency, and no urine leakage while coughing or
sneezing. At seven days postoperatively, the patient was
discharged, as she was recovering well. The patient experienced
menstrual cramps 28 days postoperatively but had no discomfort 3
months postoperatively. The results of the gynecological
examination, pelvic organ prolapse measurement and POP-Q staging
were normal: Anterior vaginal wall, POP-Q II; uterus, POP-Q 0; and
posterior vaginal wall; POP-Q 0 (Table
I). The patient is currently being followed-up and is
recovering well.
Discussion
Vaginal leiomyoma is a rare benign tumor that
frequently occurs in females aged between 35 and 50 years. Its
clinical manifestations are insidious, and it is often found during
gynecological examination. It mostly occurs at the anterior vaginal
wall and grows as a single nodule (8,9). It
has a cystic, cystic-solid or solid texture, which is related to
its degeneration. Preoperative assisted ultrasonography, MRI,
computed tomography, urethral angiography, cystoscopy and
proctoscopy may help to determine the degree of displacement of the
bladder, urethra and rectum, which aids in the differential
diagnosis and guides surgical treatment planning (10,11).
The patient of the present study had a leiomyoma at
the anterior vaginal wall, which is the most common site of vaginal
leiomyoma, but the clinical features of this patient have rarely
been reported in previous cases. The present case is unique in
terms of the growth pattern, location and size of the tumor.
Prolapse of the tumor from the vagina may cause symptoms of pelvic
floor dysfunction and stress urinary incontinence. In this patient,
vaginal bleeding and vaginal masses were obviously considered to be
cervical cancer according to clinical symptoms and MRI suggested
cervical cancer. These tumors may easily be misdiagnosed as
cervical cancer. In addition, the patient's condition was
complicated by pelvic floor dysfunction and stress urinary
incontinence, and the combination of multiple diseases made the
patient more likely to be misdiagnosed. The report of the diagnosis
and treatment of this patient therefore has important clinical
value. Furthermore, the patient's routine blood and biochemical
examination results indicated no anomalies and at present, there
are no good hematological markers to judge the nature of the tumor.
However, in the clinic, markers for leiomyoma are required.
After a multidisciplinary discussion at our
hospital, the following conclusions were reached: i) If the tumor
surface envelope exceeds 4 mm, it is difficult to perform
histological diagnosis. Therefore, multi-needle biopsy and
frozen-section analysis should be performed to rule out malignancy.
ii) No obvious symptoms of stress urinary incontinence before tumor
prolapse and frequent stress urinary incontinence after tumor
prolapse indicates that there is a vaginal tumor. The orientation
of the structures that support the urethra and bladder may change
due to the effect of gravity. Pelvic floor dysfunction and symptoms
of stress urinary incontinence may disappear after tumor removal.
Therefore, tumor resection should be performed first, followed by
observation. There is no need to temporarily treat the urinary
incontinence. iii) Vaginal tumors should be considered during the
preoperative MRI evaluation of pelvic floor dysfunction and dynamic
MRI should be used to evaluate pelvic floor function, if necessary.
iv) Pelvic prolapse may be evaluated intraoperatively.
Gynecological examination, pelvic organ prolapse measurement and
POP-Q staging should be repeated after solid vaginal tumor
resection and the subsequent treatment should be determined based
on the results (12,13).
Pathological examination of the present case after
tumor resection revealed vaginal leiomyoma. Vaginal leiomyoma has a
high misdiagnosis rate, both locally in China and globally, and
diagnosis based on imaging findings alone is difficult.
Misdiagnosis occurs most frequently in patients with a ‘prolapsed
vaginal mass’. These patients present with a prolapsed vaginal
mass, abdominal pain and discomfort, and discomfort during
defecation and urination (14).
Most frequently, the initial diagnosis is ‘uterine prolapse’ and
the patient then receives delayed or incorrect treatment.
Furthermore, pelvic floor diseases were frequently overlooked in
the past and numerous cases may have gone undetected due to missed
diagnosis and misdiagnosis (15,16).
The use of inappropriate methods of specimen collection for
pathological examination may delay diagnosis and treatment and make
it impossible to confirm the diagnosis prior to surgery,
particularly in patients with associated pelvic floor dysfunction
and stress urinary incontinence. There is a lack of large studies
on the treatment of such patients and this area requires to be
further explored.
In conclusion, although vaginal leiomyoma is easy to
misdiagnose, it is associated with a favorable prognosis. The
present case suggests that intraoperative frozen-section analysis
should be performed in all patients with vaginal wall tumors with
MRI findings suggestive of malignancy, and once diagnosis is
confirmed, surgical treatment should be performed to prevent
misdiagnosis and incorrect treatment.
Acknowledgements
Not applicable.
Funding
Funding: This study was funded by Gansu Province Science and
Technology Planning Project (grant no. 20JR10RG310) and Hexi
University Young Teacher Research Fund Project (grant no.
QN2019004).
Availability of data and materials
All data generated or analysed in this study are
included in this published article.
Authors' contributions
YG and YQ made substantial contributions to the
conception and design of the work and drafted and revised the
manuscript. JL and JQ collected clinical information, designed the
study and assisted with the drafting of the manuscript. JY and JQ
made substantial contributions to the design of the study, drafted
the manuscript and confirmed the authenticity of all raw data. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki and approved by the Ethics Committee
of Hexi University Affiliated Zhangye People's Hospital (Zhangye,
China). Written informed consent was obtained from the patient.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of the data and images in this case
report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Egbe TO, Kobenge FM, Metogo JAM, Manka'a
Wankie E, Tolefac PN and Belley-Priso E: Vaginal leiomyoma: Medical
imaging and diagnosis in a resource low tertiary hospital: Case
report. BMC Womens Health. 20(12)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zhang NN, Li D, Chen SL, Zuo N, Sun TS and
Yang Q: An effective method using laparoscopy in treatment of upper
vaginal leiomyoma. Fertil Steril. 114:185–186. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Shah M, Saha R and Kc N: Vaginal
leiomyoma: A case report. JNMA J Nepal Med Assoc. 59:504–505.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Yao J, Xi W, Zhu Y, Wang H, Hu X and Guo
J: Checkpoint molecule PD-1-assisted CD8+ T lymphocyte
count in tumor microenvironment predicts overall survival of
patients with metastatic renal cell carcinoma treated with tyrosine
kinase inhibitors. Cancer Manag Res. 10:3419–3431. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Madhu C, Swift S, Moloney-Geany S and
Drake MJ: How to use the pelvic organ prolapse quantification
(POP-Q) system? Neurourol Urodyn. 37 (Suppl 1):S39–S43.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Pollock GR, Twiss CO, Chartier S,
Vedantham S, Funk J and Arif Tiwari H: Comparison of magnetic
resonance defecography grading with POP-Q staging and Baden-Walker
grading in the evaluation of female pelvic organ prolapse. Abdom
Radiol (NY). 46:1373–1380. 2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Deshpande HG, Madkar CS and Kiwalkar SR:
Relationship of decubitus ulcer on cervix in pelvic organ prolapse
with POP-Q staging. J Obstet Gynaecol India. 69:266–271.
2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Jordanov A, Strateva D and Hinkova N:
Vaginal leiomyoma-a case report and review of the literature. Akush
Ginekol (Sofiia). 53:33–35. 2014.PubMed/NCBI(In Bulgarian).
|
|
9
|
Elsayes KM, Narra VR, Dillman JR, Velcheti
V, Hameed O, Tongdee R and Menias CO: Vaginal masses: Magnetic
resonance imaging features with pathologic correlation. Acta
Radiol. 48:921–933. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Liu JH, Zheng Y and Wang YW: Transvaginal
natural orifice transluminal endoscopic surgery (vNOTES) as
treatment for upper vaginal leiomyoma: A case report. Med (Baltim).
100(e25969)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Malik S, Mahendru R and Rana SS: Vaginal
leiomyoma presenting as dysfunctional uterine bleeding. Taiwan J
Obstet Gynecol. 49:531–532. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Riss P and Dwyer PL: The POP-Q
classification system: Looking back and looking forward. Int
Urogynecol J. 25:439–440. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Harmanli O: POP-Q 2.0: Its time has come!
Int Urogynecol J. 25:447–449. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Meniru GI, Wasdahl D, Onuora CO, Hecht BR
and Hopkins MP: Vaginal leiomyoma co-existing with broad ligament
and multiple uterine leiomyomas. Arch Gynecol Obstet. 265:105–107.
2001.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Akkamahadevi CH, Neekita P, Pooja S,
Bhavana N, Prashanth R and Shivakumar KS: Benign primary vaginal
leiomyoma-A diagnostic challenge: Rare case report. Eur J Obstet
Gynecol Reprod Biol. 247:261–262. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yarci A, Bayramov V, Sükür YE, Yüce T and
Berker B: Vaginal vault leiomyoma: 25 years after total abdominal
hysterectomy. J Minim Invasive Gynecol. 17:116–117. 2010.PubMed/NCBI View Article : Google Scholar
|