Introduction
In May 2022, a quickly spreading monkeypox infection
outbreak took place in more than 20 countries across the Middle
East, North and South America and Europe. Cases are rising
worldwide, with an increased concern that the virus could evolve
into a pandemic alongside COVID-19(1). The monkeypox virus, belonging to the
Orthopoxvirus genus in the Poxviridae family, causes the monkeypox
infection (2). This virus is
native to Central and West Africa. Person-to-person transmission
takes place by close, direct contact with an individual throughout
the infectious phase through contact with infected bodily fluids,
droplets or via fomites (such as linens). It appears that airborne
transmission is less frequent (3).
Regarding the incubation period, this varies from 5-21 days
(4). The lesions start as papules
or macules, develop into pustules, umbilicated vesicles, ulcers
and, finally, into crusty scabs (4,5).
Unlike varicella, for instance, this infection's lesions usually
erupt and recede in unison in a single anatomic area. Herpes
simplex, syphilis, varicella zoster, chancroid, mulloscum
contagiousum, cryptococcus and hand-foot-and-mouth disease, are
considered for differential diagnoses. Most likely, the patients
are infectious from the outbreak of the symptoms up until all of
the scabs have subsided (6). Even
though no specific vaccine or treatment for monkeypox is available,
human populations may benefit from some protection by
cross-immunity with smallpox vaccination. However, the rate of
monkeypox mortality ranges from 1-10% (2). Reverse transcription PCR of samples
collected via dry swabs of unroofed lesions or ulcers is used to
establish diagnosis (6).
Case report
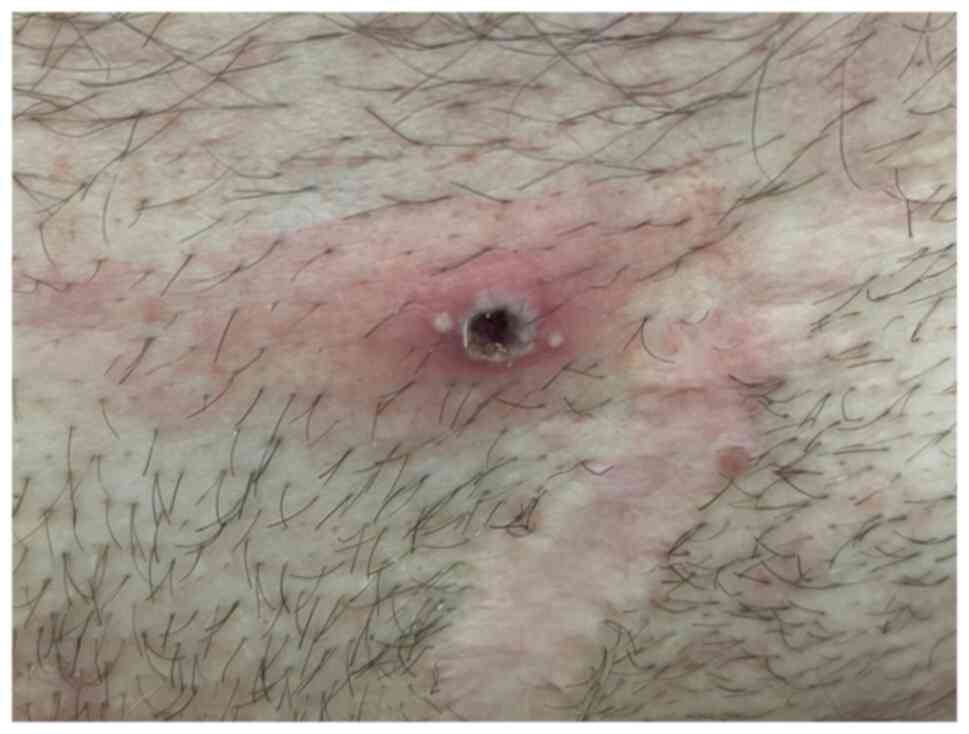
A 37-year-old homosexual man presented at the
Department of Dermatology of Ponderas Academic Hospital, Bucharest,
Romania in June 2022 for multiple well-circumscribed umbilicated
erythemato-necrotic skin lesions located in the perigenital area
and the inner part of the thighs, which appeared suddenly in the
last 5 days (Fig. 1, Fig. 2 and Fig. 3). The patient reported fever 3 days
prior. In addition, he disclosed having had unprotected sexual
intercourse with an individual who had recently traveled from the
UK, who had been diagnosed with syphilis 2 weeks before the
appearance of the skin lesions. Urethral samples for the screening
of sexually transmitted diseases were collected after prostatic
massage. The tests included bacteriological and mycological exams
from the urethral secretion and the balanopreputial sulcus and
swabs for Chlamydia, Ureaplasma spp and Mycoplasma. Blood tests for
syphilis [quantitative Rapid Plasma Reagin (RPR) and Treponema
pallidum haemagglutination TPHA], HIV and hepatitis B and C were
also collected. All the screening tests were negative for the
aforementioned diseases. A PCR test for monkeypox was recommended,
which came back positive. A vaccine against monkeypox virus was
recommended to the patient. The present study was approved by the
Ethics Committee of Ponderas Academic Hospital (approval no.
402/06.06.2022).
Discussion
A zoonotic orthopoxvirus, monkeypox causes
infections in humans in a similarly to smallpox; however, its
mortality rate is markedly lower. The relevance of this virus lies
in its endemicity to Central and Western Africa, with outbreaks in
the western hemisphere associated with the exotic pet trade, as
well as international travel. Vaccinia vaccination previously
granted coincident immunity to monkeypox virus; nonetheless,
smallpox eradication and consequent absence of vaccination enabled
monkeypox to become clinically relevant (7).
Sexual behavior, as presented in this case report,
alongside the initial appearance of the lesions particularly in the
genital and anal areas point to the fact that close contact during
sexual intercourse was essential in the transmission of the
virus.
In the present case, the main differential diagnosis
was primary syphilis since the patient reported condomless sexual
activities with a syphilis positive patient. However, during a
subsequent visit to the Department of Dermatology of Ponderas
Academic Hospital, Bucharest, the patient reported that his partner
was tested only with a nonspecific treponemal test (RPR). In order
to make a certain diagnosis of syphilis, a specific treponemal test
should be used. Treponemal tests represent qualitative assays
performed on serum in order to detect antibodies (typically IgG,
occasionally IgM) against a range of T. pallidum antigens; these
antibodies are detectable 2-4 weeks after exposure. Treponemal
tests are generally more sensitive in early infection; once
positive, they generally remain reactive indeterminately. It is not
possible to use them for monitoring treatment response or for
diagnosing reinfection because of the weak correlation with disease
activity. Conversely, non-treponemal tests are performed on
serially diluted serum in order to detect total antibodies (IgG and
IgM) directed against lipoidal antigens, like lecithin and
cardiolipin, which are released from damaged host cells and
bacteria. These antibodies are nonspecific; generally they are not
detectable until several weeks after infection (8). Subsequently, the patient's partner
was tested for monkeypox; the result was also positive. Another
clinical clue that made us doubt that the patient had syphilis was
the presence of multiple umbilicated lesions instead of
spontaneously subsiding painless ulcer (chancre) at the inoculation
site, representative for primary syphilis (Figs. 1 and 2).
A positive RPR test is the result of unspecific
cytolysis and it can be modified in a number of infectious
conditions, not only luetic infection. Moreover, a recent study
reports a high titer of RPR in patients with monkeypox, as a result
of damaged host cells that release specific antigens (9).
In case of vesicular or pustular genital rash, the
differential should consider monkeypox, as it requires a swift
diagnosis, as well as a public health response. Considering
interventions like isolation and post-exposure prophylaxis with
smallpox vaccine if indicated, as well as tracing close contacts
should be among the measures taken (9). Presently, no specific clinically
proven treatments for monkeypox infection are available. Supportive
symptom management represents the treatment approach, as for most
viral infections (7).
Acknowledgements
Professional editing, linguistic and technical
assistance performed by Ms. Irina Radu, Individual Service Provider
(credentials: E0048/2014; Medicine-Pharmacy; Bucharest,
Romania).
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
AC performed a critical review of literature
findings, made substantial contributions to acquisition and
interpretation of data, and revised the manuscript critically for
important intellectual content. DB examined the patient and
collected the urethral swabs from the patient. The two authors read
and approved the final manuscript. AC and DB confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Ponderas Academic Hospital (approval no.
402/06.06.2022).
Patient consent for publication
Written informed consent was obtained from the
patient prior to publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Le Page M: Monkeypox: Key questions
answered. New Sci. 254:8–9. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Berthet N, Descorps-Declère S, Besombes C,
Curaudeau M, Nkili Meyong AA, Selekon B, Labouba I, Gonofio EC,
Ouilibona RS, Simo Tchetgna HD, et al: Genomic history of human
monkey pox infections in the Central African Republic between 2001
and 2018. Sci Rep. 11(13085)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bunge EM, Hoet B, Chen L, Lienert F,
Weidenthaler H, Baer LR and Steffen R: The changing epidemiology of
human monkeypox-A potential threat? A systematic review. PLoS Negl
Trop Dis. 16(e0010141)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Monkeypox: Information for clinicians.
Centres for Disease Control and Prevention, Atlanta, GA, 2019.
https://www.cdc.gov/poxvirus/monkeypox/clinicians/index.html.
Accessed May 24, 2022.
|
|
5
|
Monkeypox: Information for healthcare
providers about monkeypox. Centre for Disease Control, Vancouver,
BC, 2022. http://www.bccdc.ca/health-professionals/clinical-resources/monkeypox.
Accessed May 26, 2022.
|
|
6
|
Halani S, Mishra S and Bogoch II: The
monkeypox virus. CMAJ. 194(E844)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Moore MJ, Rathish B and Zahra F:
Monkeypox. In: StatPearls [Internet]. StatPearls Publishing,
Treasure Island, FL, 2022.
|
|
8
|
Satyaputra F, Hendry S, Braddick M,
Sivabalan P and Norton R: The laboratory diagnosis of syphilis. J
Clin Microbiol. 59(e0010021)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hammerschlag Y, MacLeod G, Papadakis G,
Adan Sanchez A, Druce J, Taiaroa G, Savic I, Mumford J, Roberts J,
Caly L, et al: Monkeypox infection presenting as genital rash,
Australia, May 2022. Euro Surveill. 27(2200411)2022.PubMed/NCBI View Article : Google Scholar
|