Introduction
The most common cardiac tumors in adults are
metastatic tumors (1). In
autopsies, the incidence of primary cardiac tumors is <0.2%
(2). Cardiac lipomas are rare
entities, with a 2.9-8% incidence among all benign cardiac tumors,
which positions them at the third place after myxomas and papillary
fibroelastomas (3). Most cardiac
lipomas do not cause symptoms, but they can be fatal when they
cause arrhythmic or obstructive symptoms (1). They can be associated with symptoms
that are related to the size and location (4). For example, lipomas that are large
can cause left ventricular outflow tract obstruction and lead to
symptoms ranging from syncope to cardiogenic shock, while lipomas
situated near the atrioventricular valves can lead to valvular
insufficiency or stenosis and manifest clinically as heart failure.
The current case report presented a rare case of a large right
atrial (RA) mass, in a completely asymptomatic patient who was in
the otolaryngology service for a frontal osteoma resection.
Echocardiography is the most useful imaging
technique to diagnose cardiac tumors due to its availability,
accuracy and safety, but cardiac magnetic resonance can better
characterize the tumors (5). In
this case, echocardiography revealed the tumor and cardiac magnetic
resonance raised the suspicion of cardiac lipoma, but the
differential diagnosis with a liposarcoma remained. Conservative
management requires periodic clinical and echocardiographic
monitoring. Surgery is the treatment of choice and is considered
curative, but the risk-benefit ratio must be considered, and shared
decision making must be taken into account. Whether one approach is
superior to the other is unknown (6). Due to the lack of large studies on
cardiac lipomas, there are no exact data regarding risk factors or
mortality in these patients; however, literature reviews can be
helpful.
Case report
In February 2018, a 30-year-old male was admitted to
the Otolaryngology service of the Coltea Clinical Hospital
(Bucharest, Romania) for a frontal osteoma resection. The patient
was completely asymptomatic, with good effort tolerance, practicing
sports during adolescence, without significant family history. The
physical examination did not yield any pathological results. In
addition, laboratory tests were within normal limits: Hemoglobin
level, 15.7 g/dl (normal limits, 14-17 g/dl); white blood cell
count, 7,600/µl (normal limits, 4,000-11,000/µl; C reactive
protein, 0.31 mg/dl (normal limits, 0-0.32 mg/dl); and D-Dimer,
0.23 (normal limits, 0-0.5 µg/ml).
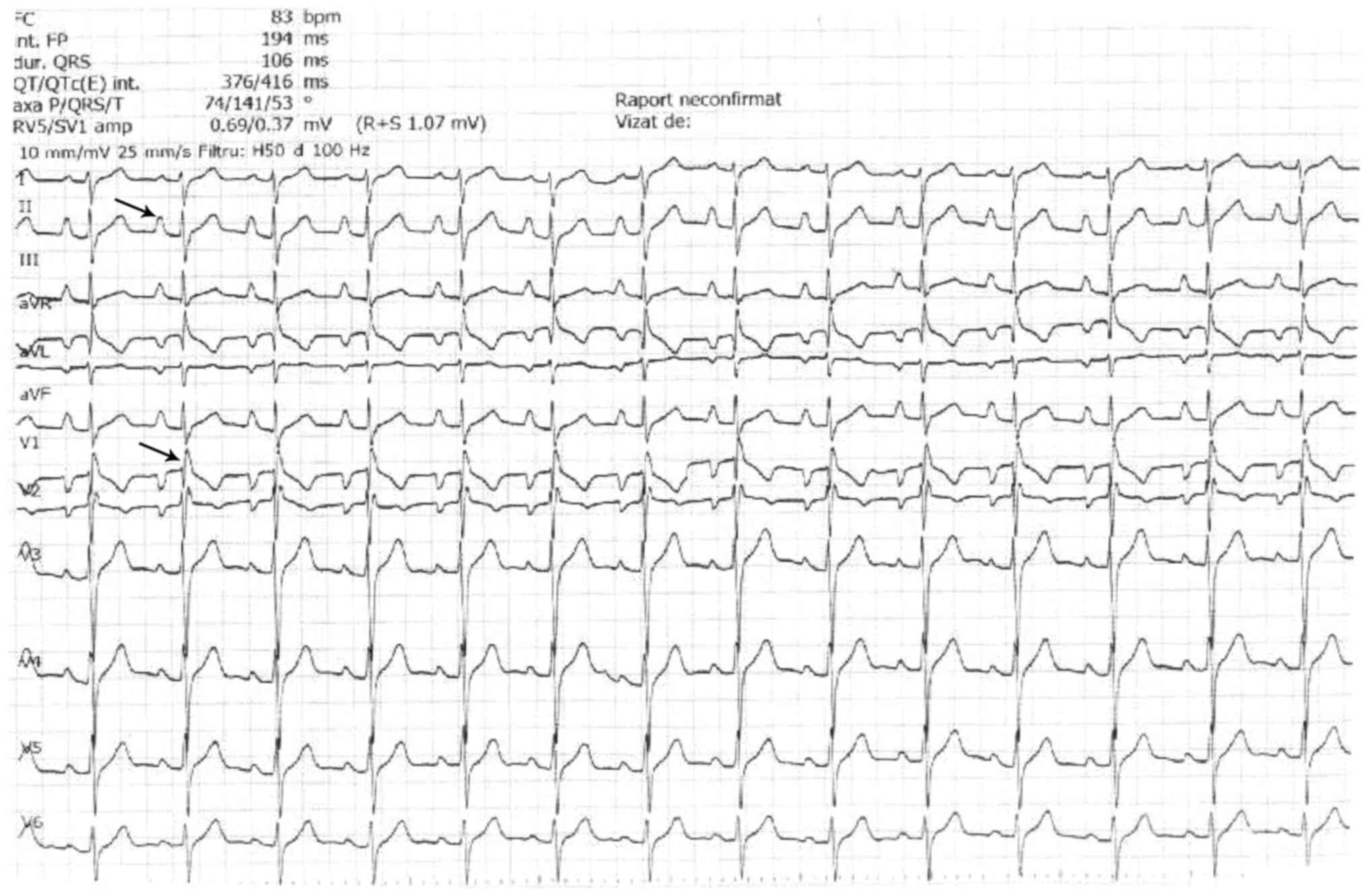
Preoperative standard twelve-lead electrocardiogram
(Fig. 1) showed sinus rhythm,
ventricular rate of 83 beats per minute ‘pulmonale P waves’ (tall
and peaked, height of 3 mm in D II) and QRS with right bundle
branch block aspect. The findings suggested the presence of RA
enlargement. Because of these electrical abnormalities, the patient
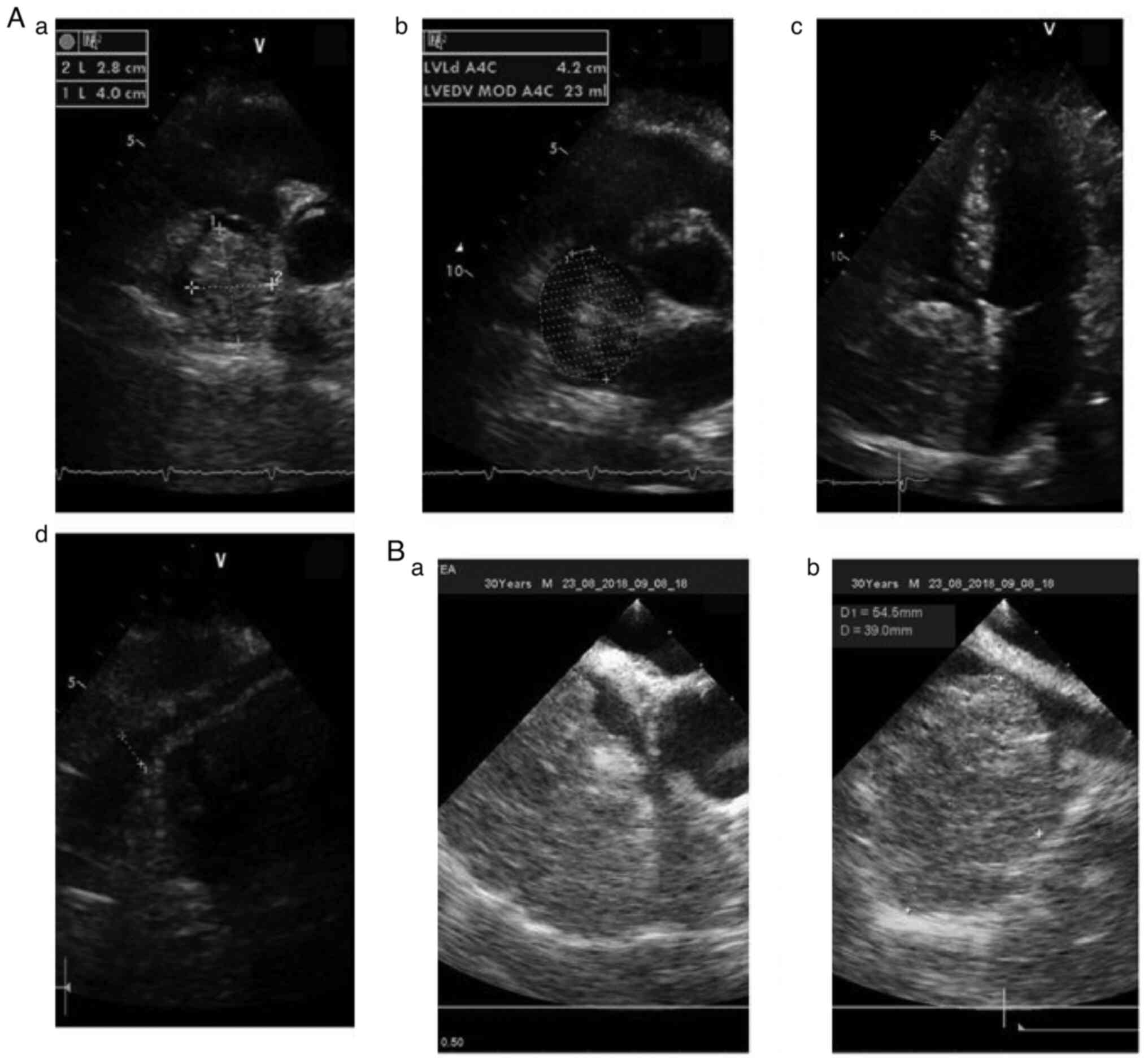
was sent to the cardiologist. Transthoracic echocardiogram showed a
large mass occupying the right atrium (40x28 mm), oval-shaped,
hyperechoic, homogenous, with borders attached to the free wall of
the right atrium (Fig. 2Aa-Ac),
which was compatible with a benign tumoral mass. Inferior vena cava
was normal (Fig. 2Ad).
Transesophageal echocardiogram was performed to appreciate better
the mass and to search for associated abnormalities and indicated
the size of the atrial tumor (54x39 mm) (Fig. 2Ba and Bb). To improve tumor characterization and
differential diagnosis, cardiac magnetic resonance was considered
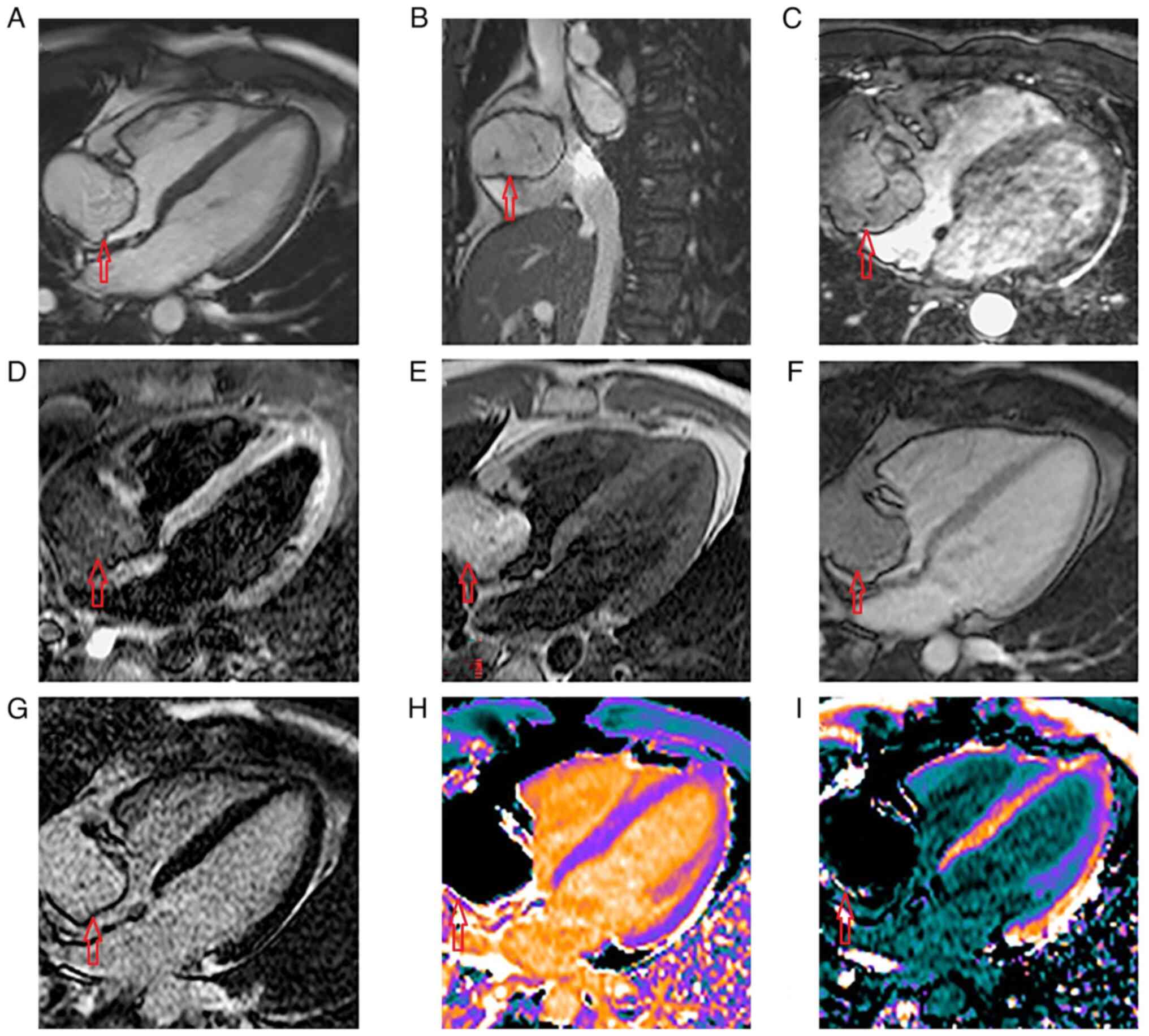
appropriate. Cardiac magnetic resonance showed a large mass
originating on the RA lateral wall and occupying almost the entire
RA cavity without any contact with the inter-atrial septum
(Fig. 3A; cine 4 chamber view),
which did not interfere with the blood flow from either superior or
inferior vena cava (Fig. 3B; cine
bi-caval view). The three-dimensional whole heart sequence revealed
that the mass had a poli-lobulated and septate appearance (Fig. 3C). The mass was hypointense in
T2-weighted short inversion time inversion recovery (Fig. 3D). In T1-weighted turbo spin-echo
dark blood sequence, the mass appeared hyperintense (Fig. 3E). Early gadolinium enhancement
imaging showed no evidence of thrombus attached to the surface of
the mass (Fig. 3F) and late
gadolinium enhancement imaging with a time of inversion chosen for
myocardial nulling showed homogenous intensity of the RA mass
(Fig. 3G). Advanced tissue
characterization techniques (T1 mapping) were performed that
definitely identified the lipomatous nature of the RA mass: Native
T1 maps showed homogenous and significantly lower T1 values 250
msec of the mass compared with the normal myocardium and blood,
while it was similar to subcutaneous and epicardial fat (Fig. 3H). Post-contrast administration T1
mapping of the RA mass showed a T1 of 260 msec, similar to the
native T1 value, indicating that the tumor did not retain contrast
(Fig. 3I). These findings were
consistent with a diagnosis of cardiac lipoma.
The patient was referred with their consent to
cardiac surgery where the option was the excision of the tumor.
Further, the RA wall was reconstructed with ‘XenoSure’ patch
(LeMaitre Vascular, Inc.) in extracorporeal circulation through a
minimally invasive approach (right mini-thoracotomy). The
intervention was performed under general anesthesia with selective
intubation. Transesophageal echocardiography monitoring was set up.
A 4-cm incision was made in the right groin and the femoral vessels
were dissected. Extracorporeal circulation was performed through
the insertion of a right femoral artery cannula (size 20) and two
venous derivations (the superior cava vein percutaneous using a
cannula size 17 and the inferior cava vein through the right
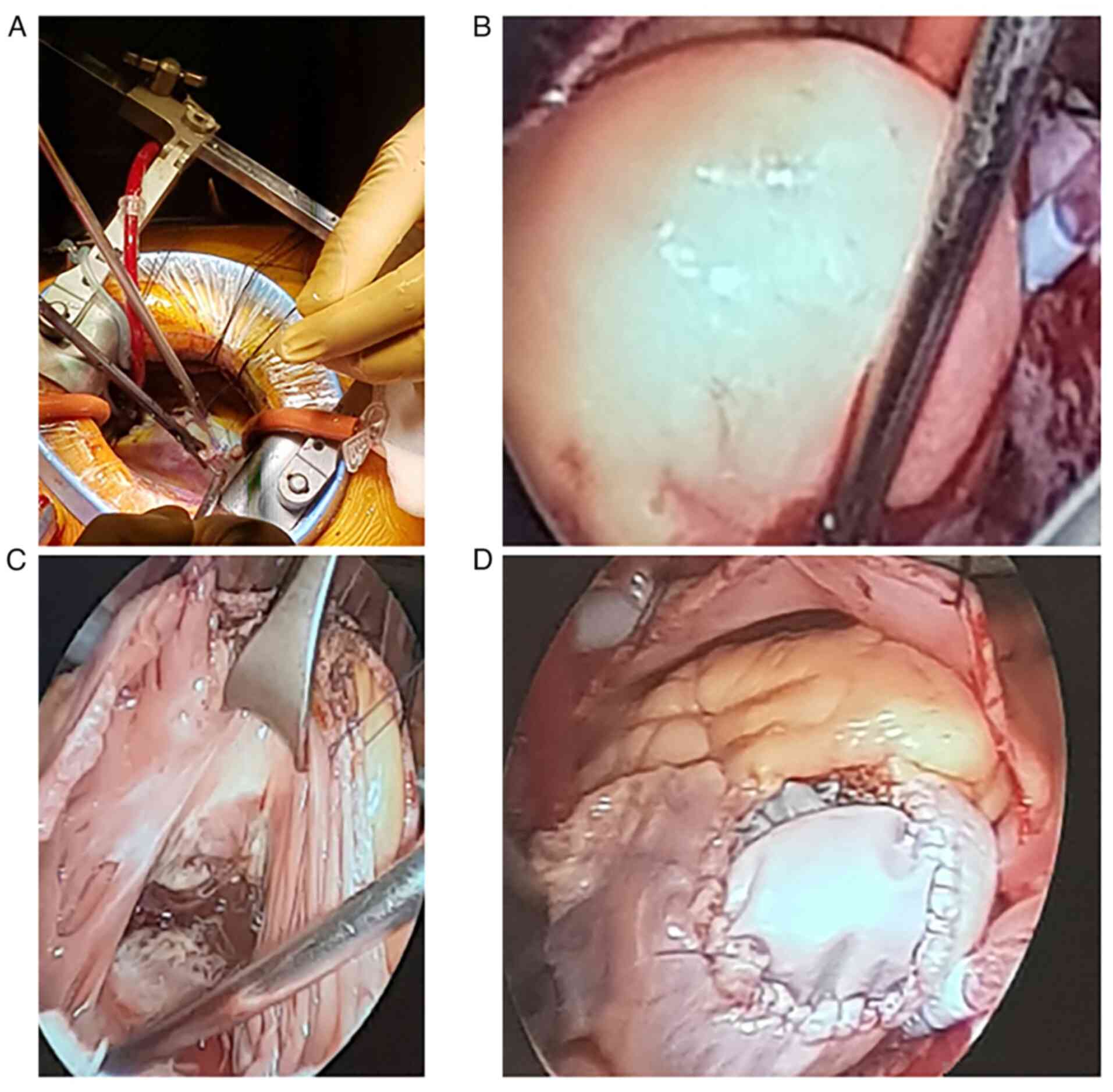
femoral vein using a long venous cannula size 25). Right
mini-thoracotomy was performed in the third intercostal right space
(Fig. 4A). After lung deflation,
lateral pericardiotomy was performed (3 cm anterior to the phrenic
nerve) and a cardioplegia cannula was applied. Myocardial
protection was achieved via administration of anterograde
cardioplegia in the aortic bulb, thereby inducing hypothermia at
34˚C. Inspection of the right atrium revealed dilated atrium due to
the tumor invasion of the anterior atrial wall (Fig. 4B).
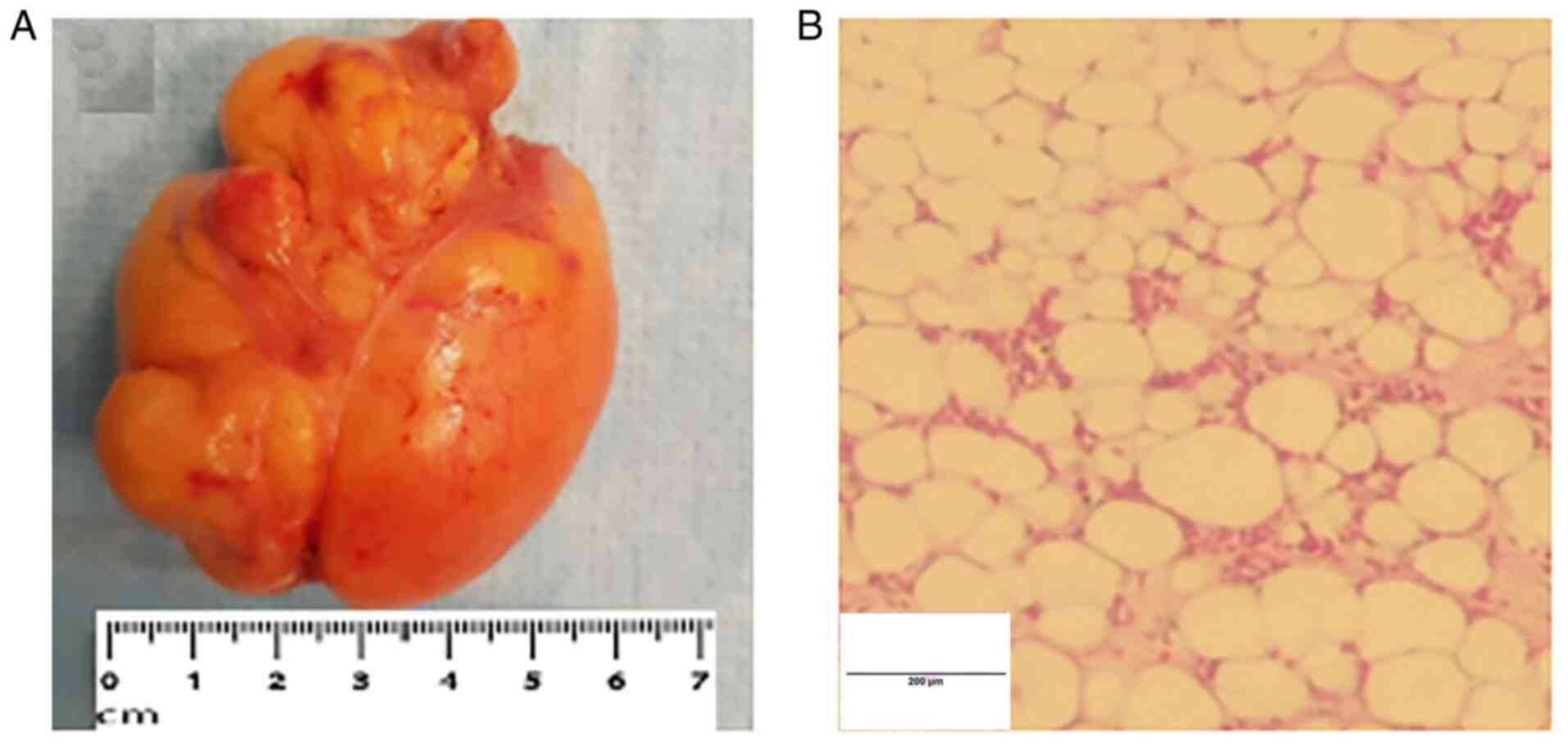
A 5-cm long right atriotomy was performed. Exposure
revealed a lipomatous mass, oval in shape, encapsulated, with
estimated dimensions of 6.5x5.5x3.5 cm (Fig. 5A), attached to the anterior wall of
the right atrium. The tumor was removed along with the implantation
base from the anterior wall of the right atrium (Fig. 4C). Reconstruction of the right
atrium was operated with a ‘XenoSure’ patch of 4/5 cm sutured with
Prolene 5.0. The right atriotomy was closed using continuous
Prolene 5.0 running suture (Fig.
4D). The bypass was stopped after rewarming the patient to
36.5˚C. The total operative time was 120 min. After the surgery,
transesophageal echocardiography examination was performed and did
not show any complications.
The sampled tissue was fixed with formalin (10%) for
18-24 h at 22˚C, then the sections were placed in paraffin blocks.
The thickness of tissue section was 2-3 µm, and it was sent for
histopathological analysis by the Department of Pathology, where a
light microscope was used for analysis. Hematoxylin and eosin
staining of the specimen revealed mature white adipose tissue
without atypia, findings consistent with a lipoma (Fig. 5B). Short-term evolution was
favorable, with rapid clinical recovery.
At the 1-year follow-up, conventional
echocardiography was normal, with no signs of atrial enlargement
and aforementioned echocardiographic changes resolved.
Discussion
Cardiac lipomas may be asymptomatic even in large
dimensions and are typically found incidentally on autopsies or via
imaging methods (1,4). Regarding their incidence, there are
no differences between age groups or sexes (4). Cardiac lipomas can be associated with
symptoms that are related to the size and location of the lipoma
(1,4). The present one is a rare case, where
the tumor was large and asymptomatic. The etiology of cardiac
lipomas is unknown. The origin of lipomas can be from all the three
cardiac tissues: Subendocardial (the majority), pericardial or
myocardial (7).
They are usually encapsulated masses, but sometimes
they can infiltrate the walls of the heart (4). The most common complications of these
tumors can be due to intracardiac obstruction of blood flow, which
can cause symptoms varying from fatigue to even syncope (4), or electrical disorders such as
atrioventricular or intraventricular conduction disorders, which
are manifested by arrhythmias, interfering in the cardiac dynamic
and leading to sudden death (8,9). In
the present case, the patient had right bundle branch block and
abnormal P wave, which resigned after the surgery. Pulmonary
thromboembolism and pericardial effusion have also been reported in
certain studies (10-13).
An intra-aortic lipoma, that invaded the left coronary ostium and
was responsible for sudden cardiac death in a 52-year-old man was
reported (9).
Echocardiography is the most useful imaging
technique to diagnose cardiac tumors due to its large availability,
accuracy and safety (14). Surgery
is the treatment of choice in these cases, but the risk-benefit
ratio must be considered, and shared decision making must be taken
into account. Shared decision making is not widely used in Romania,
and it depends on numerous factors, such as the level of education
(15). Shared decision making is
very important as these patients are subjected to significant
mental stress, being sent for cardiac surgery even though they are
asymptomatic.
After reviewing the literature, only one case of RA
lipoma treated via a minimally invasive cardiac surgery technique
was found (16). The main
particularities of the case were the absence of clinical signs
considering the dimensions of the tumor (6.5x5.5x3.5 cm; no right
ventricular filling abnormalities) and the minimally invasive
cardiac surgery technique, which was also permissive for rapid
recovery of the patient. Cardiac lipomas are rare entities, with a
2.9-8% incidence among all benign cardiac tumors (2). Reviewing the location of cardiac
lipomas revealed that ~40% were in the right atrium (4).
In the present study, a short PubMed literature
review (https://pubmed.ncbi.nlm.nih.gov/) was performed to
analyze the RA lipoma cases reported from 1995-2021. Search
criteria included the following key words: ‘Right atrial lipoma’.
The cases that had patients <16 years of age and with patients
that had no follow-up data were excluded. Collected data are
illustrated in Table I. A total of
26 cases of RA lipomas with available details were found. Among
these cases, no significant difference in the distribution between
genders (13 female, 12 male and 1 transgender) was found. The
median age of the included patients was 55.5 years old (age range,
17-74 years).
 | Table IDocumented cases of right atrial
lipoma based on PubMed based search. |
Table I
Documented cases of right atrial
lipoma based on PubMed based search.
| First author,
year | Age, years/sex | Symptoms | Size, cm | Diagnostic
Method | Obstruction | Interatrial septum
involvement | Treatment | (Refs.) |
|---|
| Present case,
2019 | 30/m | Asymptomatic | 6.5x5.5x3.5 | ECHO, CMR | No | No | Mini-thoracotomy | Not applicable |
| Mullen et al,
1995 | 17/f | Dyspnea | 25x15x8 | ECHO, CMR | No data | No data | Sternotomy | (18) |
| Sankar et al,
1998 | 38/m | Palpitations | 5x4 | X-RAY, ECHO | No data | No | Sternotomy | (20) |
| Maurea et
al, 2001 | 54/f | No data | No data | ECHO, CCT | Yes | Yes | Sternotomy | (21) |
| Pego-Fernandes
et al, 2003 | 48/m | High blood
pressure, epistaxis | 5x4.5x4 | ECHO, CMR | Yes | No | Sternotomy | (22) |
| Templin et
al, 2008 | 51/m | Dyspnea | 7.3x4.2 | ECHO, CMR | Yes | No | Sternotomy | (23) |
| Smith, 2007 | 53/f | Fatigue,
dyspnea | 3 lipomas: 7x4x2;
6x3x2; 4x2.5x1.5 | ECHO | Yes | Yes | Sternotomy | (24) |
| Gulmez et
al, 2009 | 68/f | Asymptomatic | 5x4x4 | ECHO, CT | No | Yes | Sternotomy | (25) |
| Joaquim et
al, 2009 | 27/m | Fatigue,
tachycardia | 5.5x5.3 | ECHO | No data | No data | Sternotomy | (26) |
| Ceresa et
al, 2010 | 62/m | Palpitations | No data | ECHO, CMR | No data | Yes | Sternotomy | (27) |
| Alameddine et
al, 2011 | 21/transgender
m | Dyspnea, dry
cough | 15x13x6 | X-RAY, CCT,
CMR | Yes | No data | Sternotomy | (28) |
| Habertheuer et
al, 2014 | 71/f | Dyspnea Cardiac
tamponade | No data | ECHO, CCT | Yes | No | Sternotomy | (29) |
| Barbuto et
al, 2015 | 66/m | Asymptomatic | 7.6x5.5 | CCT, CMR | No | No | Sternotomy | (30) |
| Khalili et
al, 2015 | 56/m | Dyspnea, cardiac
tamponade | 11x7.5 | ECHO, CCT | Yes | Yes | Sternotomy | (31) |
| Singh et al,
2015 | 74/f | Dizziness,
syncope | 6x6 | ECHO | No | Yes | Sternotomy | (1) |
| Wang et al,
2015 | 55/f | Asymptomatic | 3.2x1.7x7 | ECHO, CCT | No | No | Sternotomy | (32) |
| Wu et al,
2015 | 65/f | Chest pain | 1.4x1.1 | X-RAY, ECHO,
CCT | Yes | No | Sternotomy | (2) |
| Rainer et
al, 2016 | 67/f | Acute limb
ischemia | 7.7x5.5x4 | X-RAY, ECHO | No | No | Sternotomy | (33) |
| Wahab et al,
2017 | 70/f | Palpitations,
headaches | 2.6x1.6x1.6 | MRI | Yes | No | Sternotomy | (34) |
| Lapinskas et
al, 2017 | 49/m | Dizziness,
fatigue | 3.2x2.7x4.9 | ECHO, CMR | Yes | No | Sternotomy | (19) |
| Naseerullah et
al, 2018 | 50/f | Chest pain | 4x5.7, 8x7 | ECHO | No | Yes | Sternotomy | (7) |
| Shah et al,
2019 | 61/f | Chest pain | No data | ECHO, CCT, CMR | Yes | Yes | Sternotomy | (35) |
| Wang et al,
2019 | 49/m | Chest pain | 1.5x1.2x0.8 | ECHO, CCT, CMR | No | No | Sternotomy | (36) |
| Bath et al,
2019 | 74/m | Asymptomatic | 3.0x4.3x5.9 | ECHO, CMR | No | Yes | Monitoring | (37) |
| D'Errico et
al, 2019 | 67/m | Sudden death | 4x3x3 | Autopsy | No | Yes | Not applicable | (8) |
| Molek et al,
2021 | 67/f | Dyspnea, cough | 3x3 | CT, ECHO, CMR | No | No | Monitoring | (16) |
| Fan et al,
2021 | 44/m | Asymptomatic | 4.6x3.0 | CT, ECHO | No | No |
Mini-thoracotomy | (38) |
Cardiac tumors may cause clinical presentation via
different pathways. Symptoms related to RA lipoma were present in
21 out of 26 patients (80%). The symptoms varied greatly, dyspnea
being the most common of them (35%), followed by chest pain (15%)
and palpitation (12%). Although it has been reported that cardiac
lipomas are generally silent (4),
the present literature review, which included RA lipomas, showed
that only 5 out of 26 patients (19%) were completely asymptomatic.
In one particular case, the lipoma was found during the autopsy of
a patient with sudden death (8).
Large cardiac lipomas can lead to complications such
as obstruction of ventricular outflow tract, electrical disorders,
embolism or pericardial effusion (10,12,13,17).
Obstruction of right ventricular outflow tract was reported in 11
out of 26 patients (42%) diagnosed with RA lipoma (2,16-25).
Generally, atrial lipomas can have various sizes
(4). In the present review, the
largest lipoma was 25 cm and was found in a 17-year-old girl in
1995(18).
The most useful imaging technique was transthoracic
echocardiography. Among these patients, 9 out of 26 cases (35%) of
RA lipoma underwent cardiac magnetic resonance for a better tumor
characterization. Accurate diagnosis and evaluation of cardiac
lipomas is therefore dependent on multimodality imaging
methods.
The present literature review showed that 23 out of
25 patients (92%) underwent surgery. Among these patients, only 1
out of 23 received a minimally invasive approach in 2021(16). Minimally invasive surgical
techniques should be considered in certain patients with cardiac
lipoma in the future.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
MB is the corresponding author and participated in
the design of the case report. SO performed and described the
cardiac magnetic resonance. VC performed and described the surgery.
SB performed the histopathology. AG performed additional literature
review and revised the draft. MB and AG confirm the authenticity of
all the raw data. All authors read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
Ethics approval was obtained from the Medical Ethics
Committee of Coltea Clinical Hospital (approval no.
26/07.12.2021).
Patient consent for publication
Written informed consent was obtained from the
patient prior to publication at the time of admission.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Singh S, Singh M, Kovacs D, Benatar D,
Khosla S and Singh H: A rare case of a intracardiac lipoma. Int J
Surg Case Rep. 9:105–108. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wu S, Teng P, Zhou Y and Ni Y: A rare case
report of giant epicardial lipoma compressing the right atrium with
septal enhancement. J Cardiothorac Surg. 10(150)2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Valenti V, Zia MI, Uretsky S and Wolff SD:
Intra-myocardial left ventricular lipoma associated with
non-compaction cardiomyopathy. Eur Heart J Cardiovasc Imaging.
13(963)2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Shu S, Wang J and Zheng C: From
pathogenesis to treatment, a systemic review of cardiac lipoma. J
Cardiothorac Surg. 16(1)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Altbach MI, Squire SW, Kudithipudi V,
Castellano L and Sorrell VL: Cardiac MRI is complementary to
echocardiography in the assessment of cardiac masses.
Echocardiography. 24:286–300. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Abdelradi A and Yekta A: A case of
asymptomatic cardiac lipoma and literature review. CJC Open.
3:207–209. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Naseerullah FS, Javaiya H, Murthy A, Heart
SI, Place SW and Vernon M: Cardiac lipoma : An uncharacteristically
large intra-atrial mass causing symptoms. Case Rep Cardiol.
2018:3–6. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
D'Errico S, Mazzanti A, Frati P and
Fineschi V: Conduction disorder and primary cardiac tumor: A fatal
case of multiple lipomas of the right atrium. J Geriatr Cardiol.
16:431–433. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bagwan IN and Sheppard MN: Cardiac lipoma
causing sudden cardiac death. Eur J Cardiothorac Surg.
35(727)2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Miller CA and Schmitt M: Epicardial
lipomatous hypertrophy mimicking pericardial effusion:
Characterization with cardiovascular magnetic resonance. Circ
Cardiovasc Imaging. 4:77–78. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liu L, Zuo Y, Huang Y and Cao L:
Echocardiographical findings of giant cardiac lipoma. Medicine
(Baltimore). 98(e14456)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Steinberg I, Sherman RS and Waldman I:
Intrapericardial lipoma simulating pericardial effusion. Report of
two cases. Radiology. 81:949–952. 1963.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Steger CM: Intrapericardial giant lipoma
displacing the heart. ISRN Cardiol. 2011(243637)2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gurghean AL, Savulescu-Fiedler I and
Mihailescu A: Multiple cardiac complications after adjuvant therapy
for breast cancer: The importance of echocardiography. A case
report and review of the literature. Med Ultrason. 19:117–120.
2017.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Baicus C, Balanescu P, Zeh S, Oprisan E,
Lapadatu R, Gurghean A, Padureanu V, Rezus C, Mitu F, Jurcut R, et
al: Characteristics of shared decision making in Romania from the
patient perspective: A cross-sectional multicentric study. J Eval
Clin Pract. 25:1152–1159. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Molek P, Urbańczyk-Zawadzka M, Mielnik M,
Szlosarczyk B, Nessler J and Gackowski A: Right atrial lipoma: The
significance of multimodality imaging. Kardiol Pol. 79:893–894.
2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chien RN, Kao JH, Peng CY, Chen CH, Liu
CJ, Huang YH, Hu TH, Yang HI, Lu SN, Ni YH, et al: Taiwan consensus
statement on the management of chronic hepatitis B. J Formos Med
Assoc. 118:7–38. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Mullen JC, Schipper SA, Sett SS and
Trusler GA: Right atrial lipoma. Ann Thorac Surg. 59:1239–1241.
1995.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lapinskas T, Kouwenhoven M, Schnackenburg
B, Bigvava T, Wassilew K, Gebker R, Jacobs S, Zaliunas R, Pieske B
and Kelle S: Cardiac MRI quantitative tissue characterization of
right atrial mass using mDixon and parametric mapping. Clin Res
Cardiol. 106:840–845. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sankar NM, Thiruchelvam T,
Thirunavukkaarasu K, Pang K and Hanna WM: Symptomatic lipoma in the
right atrial free wall. A case report. Tex Hear Inst J. 25:152–154.
1998.PubMed/NCBI
|
|
21
|
Maurea N, Mollo A, Boccalatte M, Esposito
S, Agozzino L and Bellitti R: Lipoma of the heart: A case report.
Ital Heart J. 2:621–623. 2001.PubMed/NCBI
|
|
22
|
Pego-Fernandes PM, Costa PL, Fernandes F,
Benvenuti LA and Oliveira SA: Right atrial lipoma. Arq Bras
Cardiol. 80:97–99, 94-96. 2003.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
23
|
Templin C, Ghadri JR, Wilkens L and
Niehaus M: Difficult differential diagnosis of a right atrial
intracardiac mass. Int J Cardiol. 125:e19–e20. 2008.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Smith MA: Multiple synchronous atrial
lipomas. Cardiovasc Pathol. 16:187–188. 2007.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Gulmez O, Pehlivanoglu S, Turkoz R,
Demiralay E and Gumus B: Lipoma of the right atrium. J Clin
Ultrasound. 37:185–188. 2009.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Joaquim MR, Braile DM, Arruda MV and
Soares MJ: Right atrial lipoma resection and partial reconstruction
using bovine pericardium. Rev Bras Cir Cardiovasc. 24:239–241.
2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ceresa F, Calarco G, Franzì E and Patanè
F: Right atrial lipoma in patient with Cowden syndrome. Interact
Cardiovasc Thorac Surg. 11:803–804. 2010.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Alameddine AK, Alimov VK, Turner GS and
Deaton DW: Surgical pitfalls of excising an intramyocardial lipoma.
J Thorac Cardiovasc Surg. 141:592–594. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Habertheuer A, Andreas M, Wiedemann D,
Rath C and Kocher A: A rare case of obstructive right atrial
lipoma. Ann R Coll Surg Engl. 96:e39–e41. 2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Barbuto L, Ponsiglione A, Del Vecchio W,
Altiero M, Rossi G, De Rosa D, Pisani A and Imbriaco M: Humongous
right atrial lipoma: A correlative CT and MR case report. Quant
Imaging Med Surg. 5:774–777. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Khalili A, Ghaffari S, Jodati A, Shokoohi
B and Pourafkari L: Giant right atrial lipoma mimicking tamponade.
Asian Cardiovasc Thorac Ann. 23:317–319. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Wang H, Hu J, Sun X, Wang P and Du Z: An
asymptomatic right atrial intramyocardial lipoma: A management
dilemma. World J Surg Oncol. 13(20)2015.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Rainer WG, Bailey DJ and Hollis HW Jr:
Giant cardiac lipoma: Refined hypothesis proposes invagination from
extracardiac to intracardiac sites. Texas Hear Inst J. 43:461–464.
2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Wahab A, Chaudhary S, Munir A and Smith
SJ: Lipoma of superior vena cava: A rare occurrence. BMJ Case Rep:
Jul 24, 2017 (Epub ahead of print).
|
|
35
|
Shah OA, Badran A, Kaarne M and Velissaris
T: Right atrial and SVC infiltrating mass-the entity of
infiltrating lipoma. J Cardiothorac Surg. 14(210)2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Wang X, Yu X, Ren W and Li D: A case
report: A giant cardiac atypical lipoma associated with pericardium
and right atrium. BMC Cardiovasc Disord. 19(247)2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Bath AS, Gupta V and Kalavakunta JK: A
right atrial fat ball: Rare case of cardiac lipoma. Clin Case Rep.
7:1798–1799. 2019.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Fan W, Liao B and Li X: Lipoma across the
wall of the right atrium. J Card Surg. 36:3390–3392.
2021.PubMed/NCBI View Article : Google Scholar
|