Introduction
The aim of root canal treatment is to clean and
shape the root canal system and to fill it with an inert filling
material. The inability to appropriately understand the anatomical
configuration of teeth and identify all the root canals for
subsequent disinfection and obturation may lead to endodontic
treatment failure (1). It is
essential to adequately know about the root canal system for
successful endodontic treatment; however, there are frequent
variations in the root canal system (2).
The mesial and distal roots of the mandibular first
molars typically include two mesial canals and one or two distal
canals, respectively. Rarely, the mesiolingual and mesiobuccal
canals are separated by a third canal called the middle mesial
canal, which is situated in the developing groove. The incidence of
a middle mesial (MM) canal is reported to range from 1 to 15%
(3). The middle distal (MD) canal,
which is situated in between the distolingual and distobuccal
canals, is another uncommon occurrence. Three canals in the distal
root are uncommon, with a prevalence of 0.2-3% (4,5).
The present study reported on the successful
endodontic treatment of a Chinese female patient with a mandibular
first molar with six root canals (three in the mesial root and
three in the distal root).
Case report
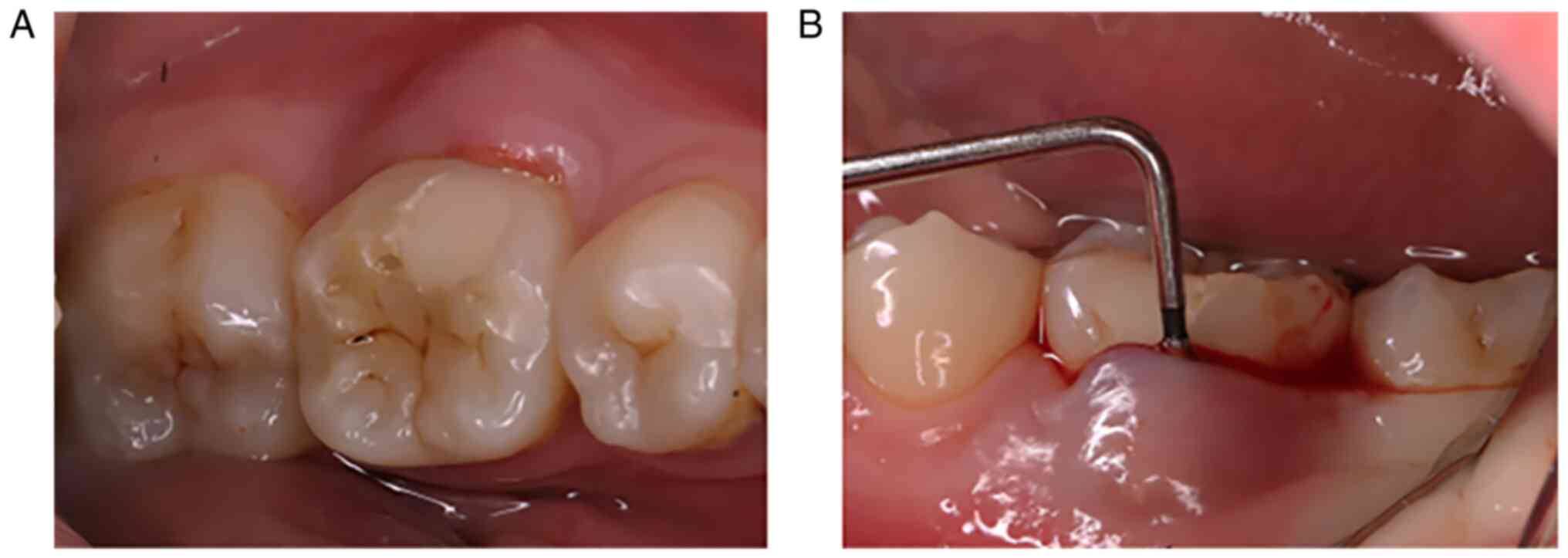
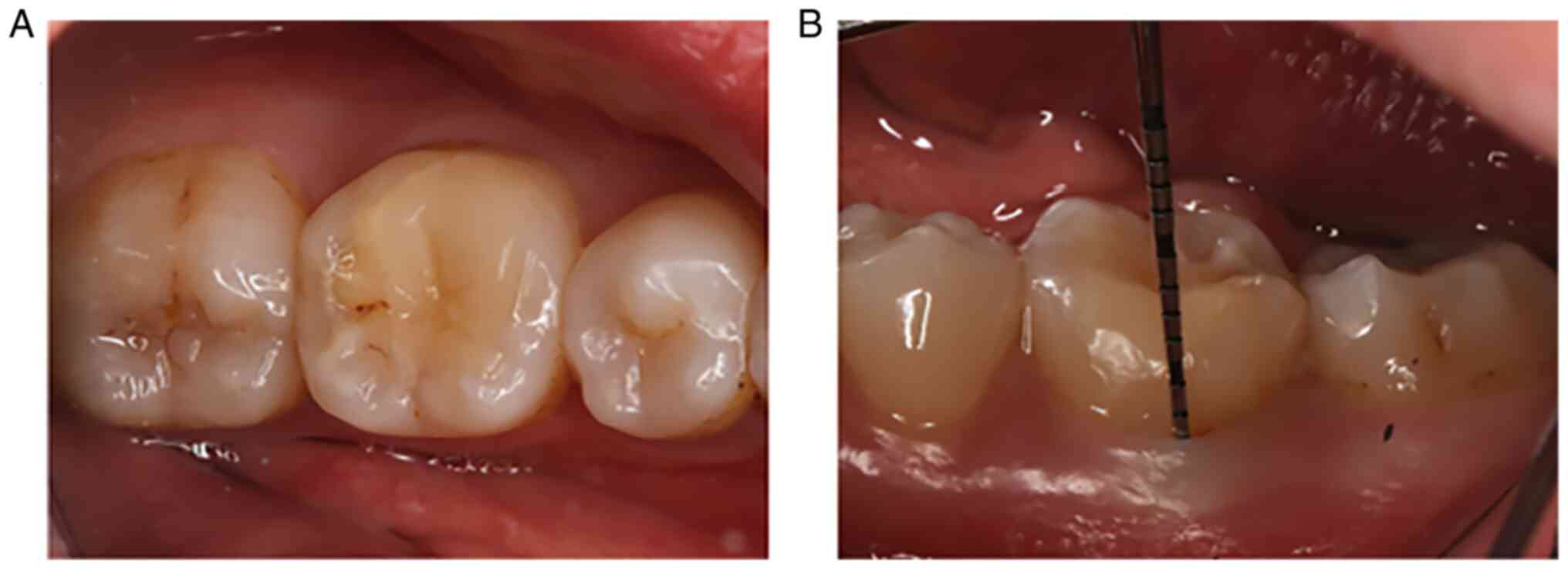
A 28-year-old Chinese female patient presented at
the Department of Endodontics, the Affiliated Hospital of Qingdao
University (Qingdao, China) in September 2017 with the chief
complaint of swelling and discomfort in the gum of a lower right
tooth for one month. Clinical examination revealed that the gingiva
of the mandibular right first molar (tooth #46) was swollen and
there was a previous filling on the mesio-occlusal surface of the
tooth (Fig. 1A). The gingiva bled
excessively on probing and a 13.5-mm deep periodontal pocket was
found in the buccal center of the tooth (Fig. 1B). The probing depth of the
periodontal pocket at the remaining points was 1-3 mm. Horizontal
percussion of the tooth caused moderate pain, whereas the pain was
more intense during vertical percussion of the tooth. Thermal
testing (heated gutta-percha and popsicles) caused no reaction and
electric pulp testing indicated complete necrosis of the pulp.
Neither distinct mobility nor clinical fractures were discovered.
All adjacent teeth were normal.
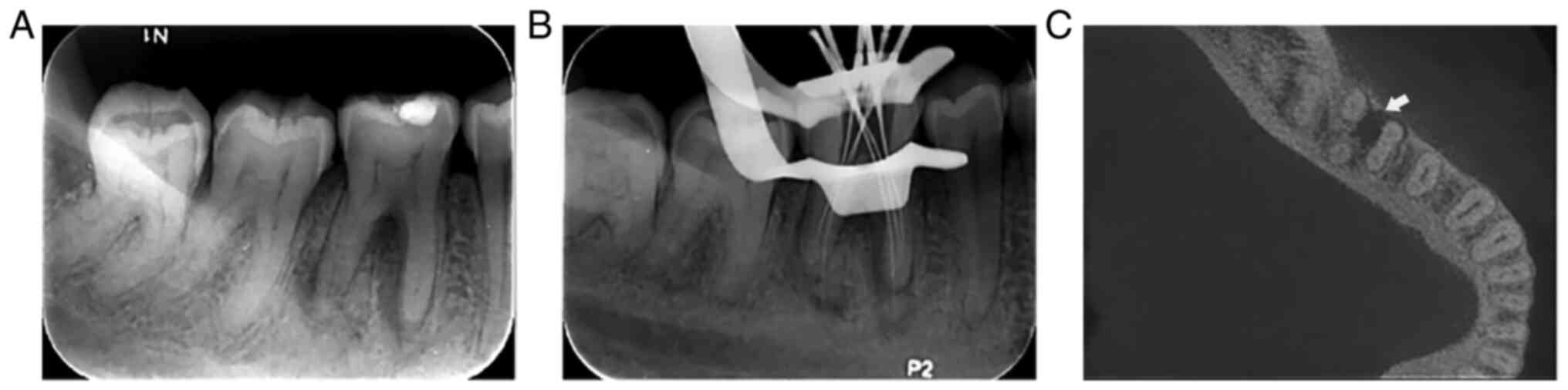
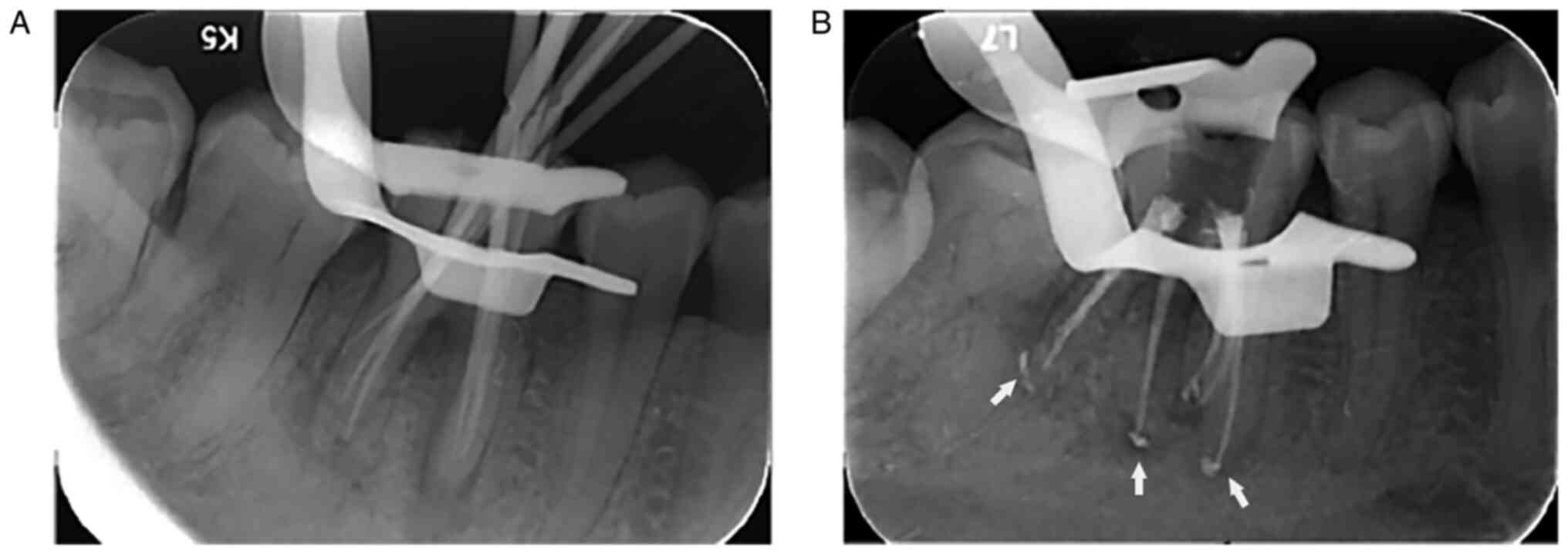
The preoperative periapical radiograph of tooth #46
revealed a low-density area surrounding the filling on the
mesio-occlusal area of the crown, approaching the pulp (Fig. 2A). The radiographic images of the
root canals were inconspicuous and they overlapped with each other.
The radiograph also indicated that the periapical periodontal
ligament space with regard to the mesial root apex and root
bifurcation had widened. To further clarify the morphology of the
root canals and the scope of lesions, cone-beam computed tomography
(CBCT; i-CAT CBCT; KaVo Dental) was proposed, and the patient
agreed to undergo the same. CBCT images (Fig. 2B) confirmed the six canals and the
scope of periapical inflammation; while the distal apical
inflammation was limited to the apical third, the proximal apical
inflammation expanded to the apical half.
Based on the clinical and radiographic examination
findings, a diagnosis of necrotic pulp with symptomatic apical
periodontitis (chronic apical periodontitis) in tooth #46 was made.
After explaining the clinical condition, the dentist recommended
nonsurgical endodontic treatment and informed the patient that
periodontal surgery may be required. The risks and benefits of the
treatment were explained to the patient and written informed
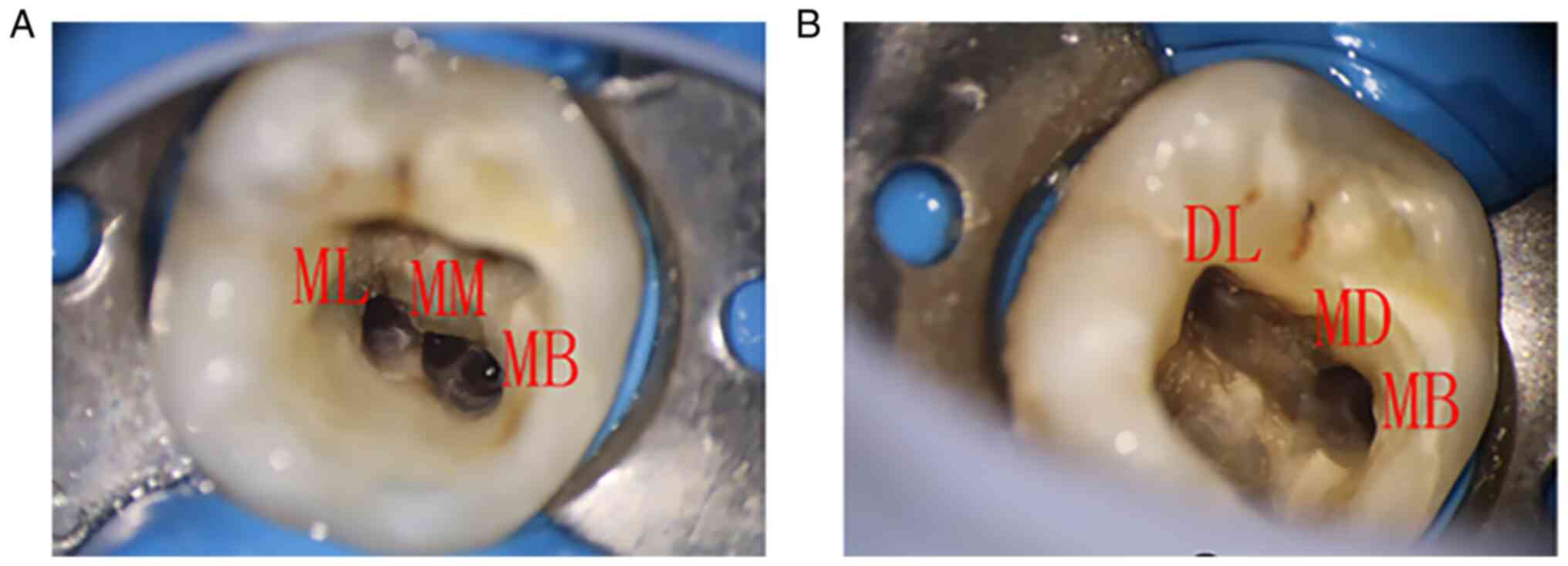
consent was obtained prior to starting the treatment. Tooth #46 was
first isolated with a rubber dam; subsequently, the previous
filling and dental caries were removed and a conventional
endodontic access was established. The pulp chamber was examined
with a DG-16 endodontic explorer and four canal orifices were
observed: Two in the mesial root mesiobuccal (MB) and mesiolingual
(ML) and two in the distal root distolingual (DL) and distobuccal
(DB). Using an operating microscope (Zumax Medical Co., Ltd), a
third orifice, MM, was located between MB and ML and an additional
orifice, MD, was located between DB and DL. The canals were
explored with a size 10 ISO K-file (Dentsply Sirona); it was
observed that each of the six separate root canals had an
independent apical foramen. The working length of each root canal
was measured with an electronic apex locator (Root ZX; J. Morita
Corp.) and confirmed by a radiograph with size 10 K-files (Fig. 2C). The root canals were then
cleaned and shaped with ProTaper nickel-titanium rotary instruments
(Dentsply Sirona) till F2 (tip diameter, 25 mm; taper, 8) using the
crown-down technique (Fig. 3).
During the procedure, 17% EDTA gel was used as a lubricant and
5.25% sodium hypochlorite solution was used as an irrigant. For the
final irrigation, ultrasonic irrigation with normal saline was
used. Calcium hydroxide was used as intracanal medication and zinc
oxide eugenol was used as a sealer.
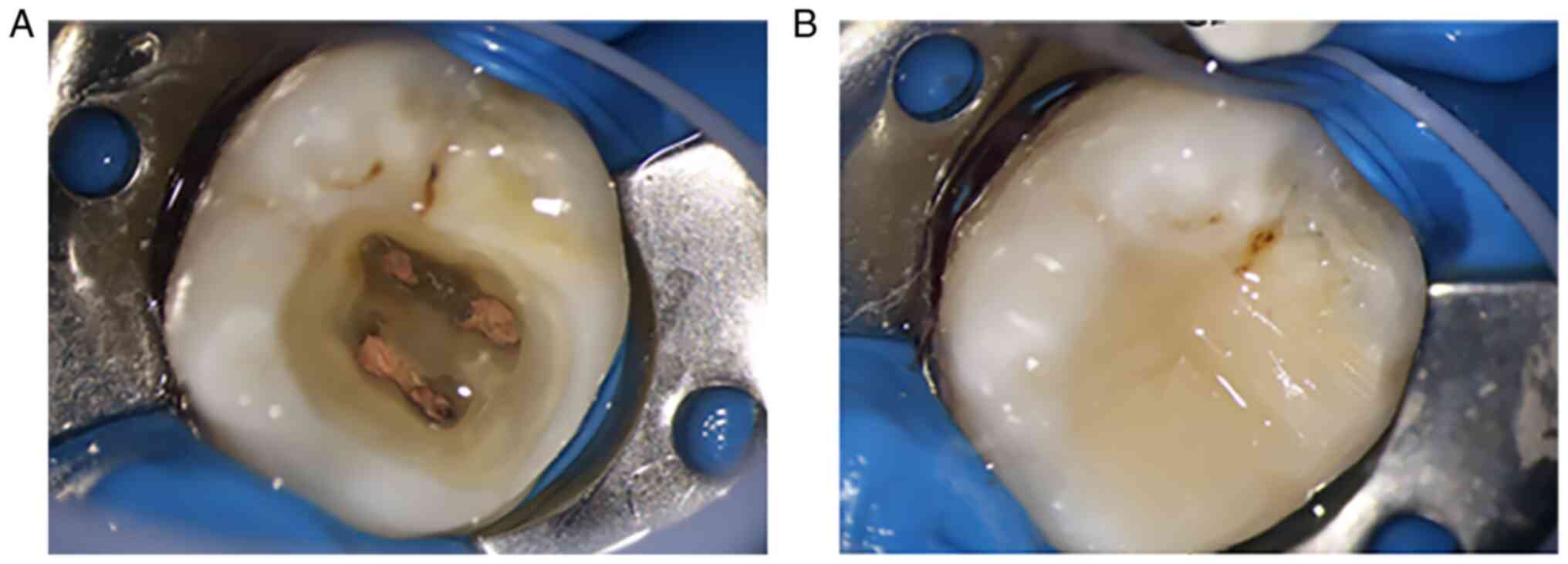
At the next appointment after 2 weeks, the patient
had improved. There was no pain when the tooth was percussed and
the gingival swelling was significantly reduced. After placing a
rubber dam, the canals were finally rinsed by ultrasonic irrigation
with normal saline and the canals were dried with absorbent paper
points and obturated using the warm gutta-percha condensation
technique with AH Plus (Dentsply Sirona) as the sealer (Fig. 4A). After completion of root canal
treatment, the tooth was restored with a composite resin (Z350 3M;
Filtek) (Fig. 4B). A final
radiograph was taken to assess the quality of the obturation. The
filling in the root canal was uniform and the gutta-percha points
did not extend beyond the apical hole; however, overfilling was
observed in certain root canals, because excessive paste was
utilized during root filling to maximise root canal sealing
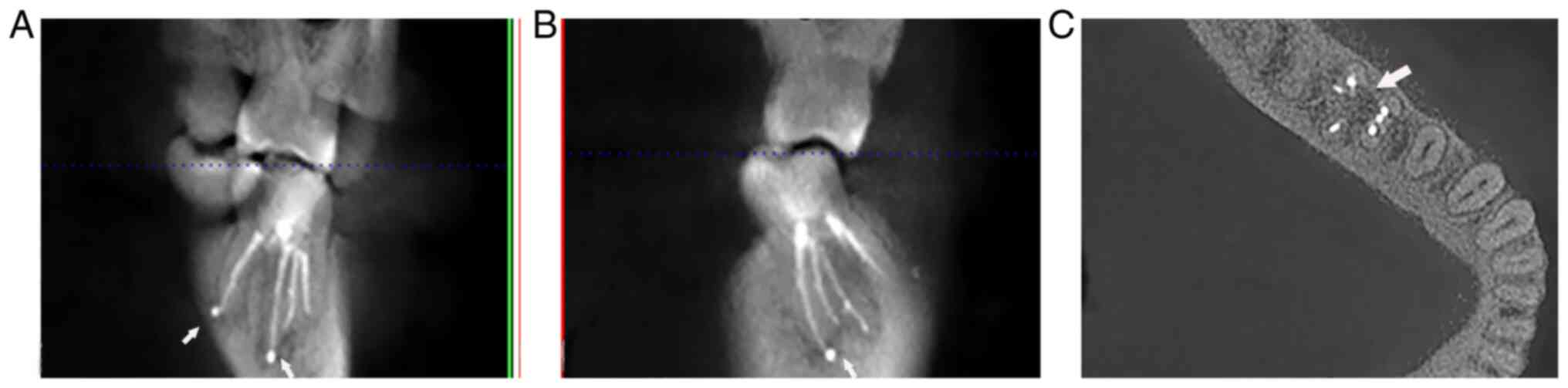
(Fig. 5).
After one year, the patient experienced no
post-treatment discomfort. The color and texture of the gums
returned to normal (Fig. 6A). The
tooth was not tender on palpation or percussion. The periodontal
probing depths around the tooth were within the physiological
limits (Fig. 6B). The CBCT images
(Fig. 7) indicated that the sealer
was still present in certain root tips, the range of radiolucency
near the mesial root and the root bifurcation had narrowed and the
bone mineral density had increased. It takes ~4 years for the AH
plus to completely absorb (6) and
in follow-up visits, the patient's subjective symptoms and apical
shadow healing will be continuously observed. If periapical
inflammation does not heal well, apical surgery may be performed
when necessary.
Discussion
Root canal treatment is currently recognized as an
effective therapy for pulpitis and periapical periodontitis.
Mandibular first molars are the first permanent posterior teeth to
erupt and most frequently have carious lesions that may necessitate
endodontic treatment. Recently, there has been an ongoing trend of
case reports that highlight the presence of more than four root
canals in mandibular first molars. However, there are a limited
number of case reports on the rare anatomical configuration with
six root canals in the mandibular right first molar. A detailed
review of case reports of mandibular first molars with six or more
root canals in the last 12 years is summarized in Table I (7-22).
These studies were retrieved from a database (https://www.x-mol.com/) using the following search
terms: Mandibular first molar, middle distal canal, middle mesial
canal, six canals, tooth anatomy, extra root.
 | Table ICase reports on mandibular first
molar. |
Table I
Case reports on mandibular first
molar.
| | Number of root
canals | |
|---|
| Author, year | Mesial root | Distal root | Total | (Refs.) |
|---|
| Ramachandran,
2019 | 3 | 3 | 6 | (7) |
| Jabali, 2018 | 3 | 3 | 6 | (8) |
| Vineet, 2018 | 4 | 2 | 6 | (9) |
| Kamble, 2017 | 3 | 3 | 6 | (10) |
| Banode, 2016 | 3 | 4 | 7 | (11) |
| Acharya, 2015 | 3 | 3 | 6 | (12) |
| Martins, 2015
(A) | 3 | 3 | 6 | (13) |
| Martins, 2015
(B) | 4 | 2 | 2 | (13) |
| Maniglia-Ferreira,
2015 | 3 | 3 | 6 | (14) |
| Baziar, 2014 | 2 | 4 | 6 | (15) |
| Sinha, 2014 | 4 | 2 | 6 | (16) |
| Hasan, 2014 | 3 | 3 | 6 | (17) |
| Martins, 2014 | 4 | 3 | 7 | (18) |
| Alves, 2012 | 3 | 3 | 6 | (19) |
| Gupta, 2012 | 3 | 3 | 6 | (20) |
| Ryan, 2011 | 3 | 3 | 6 | (21) |
| Mohsen, 2010 | 4 | 2 | 6 | (22) |
There have been certain reports of mandibular first
molars with extra roots and canals from different authors.
Maniglia-Ferreira et al (14) reported a case with six canals in a
mandibular first molar; during the 18-month follow-up, healing of a
periapical lesion was achieved. Ryan et al (21) published a case report that
discussed the endodontic management of a rare anatomical variation
in the root canal system of a mandibular first molar with six
canals (3 mesial and 3 distal); the patient was asymptomatic during
a follow-up period of 3 years and recall radiographs after
treatment indicated resolution of the previous apical
periodontitis. Regarding the ideal apical preparation size and
taper, the literature is divided. Previous research has indicated
that by enlarging the apical size and taper, it is possible to more
easily remove bacteria and debris from the root canal, increase the
effectiveness of irrigation solutions relative to the working
length and improve the distribution of the lateral and vertical
forces produced during filling (23). When compared to size 20, the apical
size of 25 produced noticeably cleaner canal walls in the top third
(24). According to a study, the
fracture strength of mandibular molar teeth is decreased when the
apical diameter and taper in the MM canal are increased. When
instrumentation sizes of >25.04 were used, the fracture strength
among the evaluated instrumentation sizes markedly decreased
(25). Since the patient of the
present study was a young female with a wide root canal lumen, the
root canal was prepared to F2 (tip diameter, 25 mm; taper, 8) to
better clean the root canal infection.
This tendency warns dentists to be more careful when
dealing with mandibular first molars requiring endodontic
treatment. Certain canals may be left untreated if their presence
is not detected by the dentist. Thus, all possible methods should
be used to locate and detect the entire root canal system.
Traditional periapical radiography is essential for preoperative
diagnosis; however, it may only provide two-dimensional
information. When root canals overlap with each other and complex
anatomies are present, such as multi-canal systems or dens
invaginatus, three-dimensional CBCT images may be beneficial to
form an accurate diagnosis and morphological evaluation in
endodontics (26). In the present
case, the standard periapical radiograph indicated that the root
canal images were overlapped and blurry. To confirm this, a CBCT
was advised for the right mandibular molar. The CBCT images
provided a clearer view of the anatomical morphology of the root
canal and inflammatory range and indicated that there were 3 apical
holes in the mesial root and distal root, respectively, which was
similar to the present findings. The use of CBCT affected the
reviewers' choices when making pulpal and periapical diagnoses and
more notably when determining etiologic factors and recommending a
treatment. This was confirmed in a study by Chogle et al
(27), in which CBCT imaging had a
significant effect in determining the etiologic factors
contributing to endodontic pathosis (55% change overall) and making
treatment recommendations (49% change overall).
DOM provides dentists with superior lighting and
magnification capacity, and enhanced illumination and visibility
enable endodontists to improve the predictability of their
procedures and may help dentists identify morphological deviations
and thoroughly understand the anatomy of the pulp chamber floor and
the exact location of canal orifices (28). These advantages of DOM provide
physicians with the ability to treat cases that previously may have
been deemed untreatable or which may have resulted in a compromised
prognosis, which is evident from numerous studies and clinical
practice in endodontics. The use of magnification is considered
helpful for the successful completion of endodontic treatment.
Maniglia-Ferreira et al (14) reported on a mandibular first molar
with four separate mesial and two separate distal canals observed
under the magnification of DOM. Wu et al (29) from the Affiliated Stomatology
Hospital of Nanjing Medical University used DOM to treat patients
whose treatment had failed by conventional methods. The patients
previously had unsuccessful treatments due to canal calcification,
separated instruments, missed canals or canal perforation. Using
DOM, 74.4% of canals were successfully treated and for the affected
teeth whose treatment failed due to missing root canal, the success
rate of retreatment through the microscope was 80%. even more to
the point that the treatment success rate of missing root canal
cases was ~80%. In the present case, with the help of DOM, the six
independent root canal openings at the bottom of the pulp chamber
were clearly observed and it was possible to check whether the pulp
cavity and root canal were cleaned and ready for root canal
filling.
The use of DOM and CBCT images in certain
challenging cases may facilitate a better understanding of the
complex root canal anatomy, which ultimately enables dentists to
better explore the root canal system and clean, shape and obturate
it more efficiently. The present case report contributes to our
knowledge of the anatomical variability of the mandibular first
molar.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data anad materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ML and YZ contributed to the study design. ML, PS,
YQ and KP collected the presurgical and intrasurgical clinical
data. ML, YZ, PS, YQ and KP participated in the postsurgical data
acquisition and interpretation and were involved in drafting the
manuscript. KP supervised the research and critically revised the
manuscript for important intellectual content. ML and KP confirm
the authenticity of all the raw data. All authors read and approved
the final manuscript as submitted and agree to be accountable for
all aspects of the work.
Ethics approval and consent to
participate
The present study was approved by the Medical Ethics
Committee of the Affiliated Hospital of Qingdao University
(Qingdao, China; approval no. QYFYWZLL27005).
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wolcott J, Ishley D, Kennedy W, Johnson S,
Minnich S and Meyers J: A 5 yr clinical investigation of second
mesiobuccal canals in endodontically treated and retreated
maxillary molars. J Endod. 31:262–264. 2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Albuquerque S, Kottoor J and Hammo M:
Endodontic and clinical considerations in the management of
variable anatomy in mandibular premolars: A literature review.
Biomed Res Int. 2014(512574)2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Fabra-Campos H: Three canals in the mesial
root of mandibular first permanent molars: A clinical study. Int
Endod J. 22:39–43. 1989.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gulabivala K, Opasanon A, Ng YL and Alavi
A: Root and canal morphology of Thai mandibular molars. Int Endod
J. 35:56–62. 2002.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Moor RJGD, Deroose CAJG and Calberson FLG:
The radix entomolaris in mandibular first molars: An endodontic
challenge. Int Endod J. 37:789–799. 2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ricucci D, Rôças IN, Alves FRF, Loghin S
and Siqueira JF Jr: Apically extruded sealers: Fate and influence
on treatment outcome. J Endod. 42:243–249. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ramachandran VS, Shankari V, Rathakrishnan
M, Chandrasegaran V and Kumaraguru K: Management of three rooted
mandibular first molar with six canals: A case report. Cureus.
11(e6280)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Jabali AH: Middle Mesial and Middle Distal
canals in mandibular first molar. J Contemp Dent Pract. 19:233–236.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Vineet A, Sonali K and Dhwani B: Rare case
of a mandibular first molar with seven canals confirmed by cone
beam computed tomography and its endodontic management. Int J
Health Sci (Qassim). 12:91–93. 2018.PubMed/NCBI
|
|
10
|
Kamble AP, Pawar RR, Mattigatti S, Mangala
TM and Makandar S: Cone-beam computed tomography as advanced
diagnostic aid in endodontic treatment of molars with multiple
canals: Two case reports. J Conserv Dent. 20:273–277.
2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Banode AM, Gade V, Patil S and Gade J:
Endodontic management of mandibular first molar with seven canals
using cone-beam computed tomography. Contemp Clin Dent. 7:255–257.
2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Acharya N, Singh A, Samant PS and Gautam
V: Endodontic management of radix paramolaris with six canals: A
clinical case report. Kathmandu Univ Med J (KUMJ). 11:338–341.
2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Martins JNR and Anderson C: Endodontic
treatment of the mandibular first molar with six roots canals-two
case reports and literature review. J Clin Diagn Res. 9:ZD06–ZD08.
2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Maniglia-Ferreira C, de Almeida Gomes F
and Sousa BC: Management of six root canals in mandibular first
molar. Case Rep Med. 2015(827070)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Baziar H, Daneshvar F, Mohammadi A and
Jafarzadeh H: Endodontic management of a mandibular first molar
with four canals in a distal root by using cone-beam computed
tomography: A case report. J Oral Maxillofac Res.
5(e5)2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sinha N, Singh B, Langaliya A, Mirdha N,
Huda I and Jain A: Cone beam computed topographic evaluation and
endodontic management of a rare mandibular first molar with four
distal canals. Case Rep Dent. 2014(306943)2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hasan M, Rahman M and Saad N: Mandibular
first molar with six root canals: A rare entity. BMJ Case Rep.
2014(bcr2014205253)2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Martins JNR: Endodontic treatment of a
maxillary first molar with seven root canals confirmed with cone
beam computer tomography-case report. J Clin Diagn Res.
8:ZD13–ZD15. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Alves FRF, Rôças IN, Almeida BM, Neves
MAS, Zoffoli J and Siqueira JF: Quantitative molecular and culture
analyses of bacterial elimination in oval-shaped root canals by a
single-file instrumentation technique. Int Endod J. 45:871–877.
2012.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Gupta S, Jaiswal S and Arora R: Endodontic
management of permanent mandibular left first molar with six root
canals. Contemp Clin Dent. 3:S130–S133. 2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ryan JL, Bowles WR, Baisden MK and
McClanahan SB: Mandibular first molar with six separate canals. J
Endod. 37:878–880. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Aminsobhani M, Shokouhinejad N, Ghabraei
S, Bolhari B and Ghorbanzadeh A: Retreatment of a 6-canalled
mandibular first molar with four mesial canals: A case report. Iran
Endod J. 5:138–140. 2010.PubMed/NCBI
|
|
23
|
Kılıç Y, Karataşlıoğlu E and Kaval ME: The
effect of root canal preparation size and taper of middle mesial
canals on fracture resistance of the mandibular molar teeth: An in
vitro study. J Endod. 47:1467–1471. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Plotino G, Özyürek T, Grande NM and
Gündoğar M: Influence of size and taper of basic root canal
preparation on root canal cleanliness: A scanning electron
microscopy study. Int Endod J. 52:343–351. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Keleş A, Keskin C, Karataşlıoğlu E, Kishen
A and Versiani MA: Middle Mesial canal preparation enhances the
risk of fracture in mesial root of mandibular molars. J Endod.
46:1323–1329. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Patel S, Durack C, Abella F, Roig M,
Shemesh H, Lambrechts P and Lemberg K: European Society of
Endodontology position statement: The use of CBCT in endodontics.
Int Endod J. 47:502–504. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chogle S, Zuaitar M, Sarkis R, Saadoun M,
Mecham A and Zhao Y: The recommendation of cone-beam computed
tomography and its effect on endodontic diagnosis and treatment
planning. J Endod. 46:162–168. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yoshioka T, Kobayashi C and Suda H:
Detection rate of root canal orifices with a microscope. J Endod.
28:452–453. 2002.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wu D, Shi W, Wu J, Wu Y, Liu W and Zhu Q:
The clinical treatment of complicated root canal therapy with the
aid of a dental operating microscope. Int Dent J. 61:261–266.
2011.PubMed/NCBI View Article : Google Scholar
|