Introduction
Coronavirus disease 2019 (COVID-19) has spread
rapidly across the globe, with high rates of transmission and
substantial sequelae (1). Patients
infected with COVID-19 display various symptoms ranging from mild,
self-limited respiratory disease to moderate to severe progressive
pneumonia (2). The main clinical
symptoms of patients with COVID-19 include fever, cough, myalgia,
fatigue, expectoration, dyspnea, headache, diarrhea, nausea and
vomiting (3). Of note, most
patients with COVID-19 present without fever and numerous patients
do not have any abnormal radiologic findings (4,5). At
present, although vaccines to prevent COVID-19 have been developed
with unprecedented speed (6), the
increase of infected patients with existing illnesses and
multi-morbidity cause massive loss of life and economic hardship
(7). Worldwide, the cumulative
number of COVID-19 cases has reached 5,139,555,910 and the number
of COVID-19-related deaths is now thought to exceed 15 million as
of May 7, 2022. In China, 865,592 COVID-19 cases have been recorded
and the number of deaths is only 15,417, as of May 7, 2022.
A wide range of clinical outcomes has been observed
in patients with COVID-19 after various treatment strategies
(8). Nursing care of patients with
COVID-19 is necessary, supportive and beneficial, which includes a
strong focus on mitigating the spread of infection to others and
the community (9). Transitional
care is an important aspect of the healthcare systems, and yet, it
is necessary to improve the quality of life of patients (10). Transitional care has an essential
role in the response to COVID-19 by responding rapidly and
flexibly. Transitional care ensures protocols for symptom
management to provide psychosocial care and communication with
patients (11). Of note,
transitional care is indispensable to successfully guide patients
at discharge or post-discharge to prevent adverse events in
patients with COVID-19, making it essential for efficient medical
and nursing practice (12).
The most common symptoms and complications of
patients with COVID-19 are inflammation and respiratory infection
(13). Inflammation and the innate
immune system have been recently recognized as pivotal players in
the progression of COVID-19, characterized by significantly
elevated levels of pro-inflammatory cytokines (14). In the present study, the effects of
transitional care on psychological symptoms, inflammation, and
pulmonary function in patients with COVID-19 were investigated. The
quality of life, recurrence rate, duration of hospital stay and
psychological symptoms such as depression, anxiety, fear,
perception of helplessness and worry were also compared in COVID-19
patients between transitional care and usual care group.
Patients and methods
Patient and public involvement
Patient and public involvement have been central to
the design of the present study. All patients with COVID-19 were
recruited at the Affiliated Hongqi Hospital of Mudanjiang Medical
University (Mudanjiang, China), randomly assigned to receive
transitional care or usual care and followed up for 12 months. All
patients were recently diagnosed with mild or moderate COVID-19.
All outcomes from each participant were assessed and recorded by
medical staff. The results of the present study were disseminated
to the study researchers in written form, which comprised
professionals within the area of COVID-19.
Case definition
The severity of COVID-19 was categorized into four
types according to officially published guidelines in China
(15): a) Mild type: Asymptomatic
or certain upper respiratory tract infection signs and no evidence
of pneumonia on imaging; b) Moderate type: Febrile respiratory
symptoms and imaging findings of pneumonia; c) Severe type: Disease
progression with danger signs (respiratory rate of >30
beats/min, oxygen saturation of <93%, oxygen partial pressure of
>300 mmHg, or lung imaging indicating significant progression of
>50% within 24-48 h); d), Critical type: Shock or organ failure
requiring intensive care.
Study design
The present clinical trial was a randomized,
double-blinded, single-center study. A total of 252 patients with
recently diagnosed mild or moderate COVID-19 were recruited at the
Affiliated Hongqi Hospital of Mudanjiang Medical University
(Mudanjiang, China) between May 2020 and October 2020. A total of
10 patients were excluded according to selection criteria. Patients
were randomly assigned to transitional care (n=126) or usual care
(n=116) and followed up for 12 months. Included were patients with
COVID-19 who met the following criteria: i) Aged 18 years or above;
ii) diagnosis of mild to moderate COVID-19 infection; iii)
hospitalization duration of less than two days; iv) patients
without any physical disability or depressive disease. Exclusion
criteria were patients in intensive care unit admission, advanced
age with multiple comorbidities, patients with severe COVID-19,
individuals with dementia or delirium and patients with advanced or
metastatic tumors. The protocol was reviewed and approved by the
ethics committees of Mudanjiang Medical University (Mudanjiang,
China). All patients provided written informed consent. The trial
was entered in the Chinese Clinical Trial Registry (ChiCTR);
registration no. ChiCTR2200060295; 26.05.2022.
Transitional care
The transitional care program is designed based on
the Omaha System (16), which is a
method to describe the needs of patients and to solve patient
problems. In brief, the Omaha System includes a problem
classification scheme, intervention scheme and problem rating
scale. The transitional care intervention scheme also includes
guidance, teaching and counseling, clinical treatments,
postoperative management and four broad surveillance categories.
Transitional care of predischarge interventions includes early
assessment after hospital admission, medication reconciliation and
planning of patient education in sporting and dieting upon
discharge.
Biochemical analysis
Blood samples were collected from each patient with
COVID-19. Routine blood tests and arterial blood gas tests were
performed for all patients and the following parameters were
evaluated: D-dimer, lymphocyte count, alanine aminotransferase,
aspartate aminotransferase, total bilirubin, albumin, platelets,
white blood cells, lactate, creatinine, hemoglobin, and saturation
of peripheral oxygen/fraction of inspired oxygen ratio.
Inflammatory cytokine assay
Serum levels of C-reactive protein (CRP),
interleukin-1β (IL-1β) (cat. no. KAC1211), IL-6 (cat. no. KHC0061),
IL-8 (cat. no. BMS204-3), IL-17 (cat. no. A35611) and TNF-α (cat.
no. BMS223-4) were measured using ELISA kits (Thermo Fisher
Scientific, Inc.) according to the manufacturer's protocol.
Mental health symptoms
The severity of symptoms of depression in each
patient with COVID-19 was assessed using the Patient Health
Questionnaire (PHQ-9) (17). The
total score of PHQ-9 ranges from 0 to 27 (depressive symptoms,
score ≥5; moderate to severe depression, score ≥10). Anxiety in
patients with COVID-19 was evaluated using the Generalized Anxiety
Disorder (GAD-7) questionnaire (18). The total score of GAD-7 ranges from
0 to 21 (anxiety symptoms, score ≥5; moderate to severe anxiety,
score >8) (19). Stress, fear,
perception of helplessness, worry and empathy of patients with
COVID-19 were evaluated using standard questionnaires (PSS 10, and
DASS 21) as described previously (20).
Quality of life
Quality of life of patients with COVID-19 was
assessed using the SF-36 questionnaire (21). The SF-36 questionnaire includes 36
multiple-choice questions by measuring 8 distinct domains (physical
functioning, physical health, general health perceptions, emotional
problems, energy/fatigue, emotional well-being, social functioning
and bodily pain). Scores of quality of life range from 0 to 100
with a higher score indicating a higher quality of life.
Pulmonary function tests
Airway function, including spirometry, pulmonary
volume and diffusing capacity, was measured in all patients using a
flow spirometer (MasterScreen; Jaeger) according to the
manufacturer's protocol. Parameters of pulmonary function,
including total pulmonary capacity (TLC), forced vital capacity
(FVC), residual volume, forced expiratory volume in 1 sec
(FEV1), FEV1/FVC and diffusing capacity of
the pulmonary for carbon monoxide (DLCO) were
measured according to the American Thoracic Society (ATS) and
European Respiratory Society (ERS) guidelines (22). Pulmonary function was analyzed
using SentrySuite software V03.0.5 (Vyaire Medical). The 6-min
walking test (6MWT) was evaluated according to ATS/ERS guidelines
(23).
Symptom score
The symptom score of the patients with COVID-19 was
evaluated from their electronic medical records (24). The severity of symptoms was scored
from 0 to 10 points. The 10-scale symptom scoring system for
patients with COVID-19 included nausea, dyspnea, chest pain, cough,
asthenia, myalgia, dizziness, conjunctivitis, loss of appetite and
diarrhea. Lower scores indicated a lower level of symptoms.
Statistical analyses
Values are expressed as the mean ± standard
deviation or n (%). The data were analyzed using Stata V.13.0
(StataCorp LP). Data were analyzed using SPSS v20 software (IBM
Corporation). Differences between two groups were analyzed by using
the χ2 or Fisher's exact test for categorical variables,
the two-samples t-test or Wilcoxon rank-sum test for continuous
variables as applicable. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
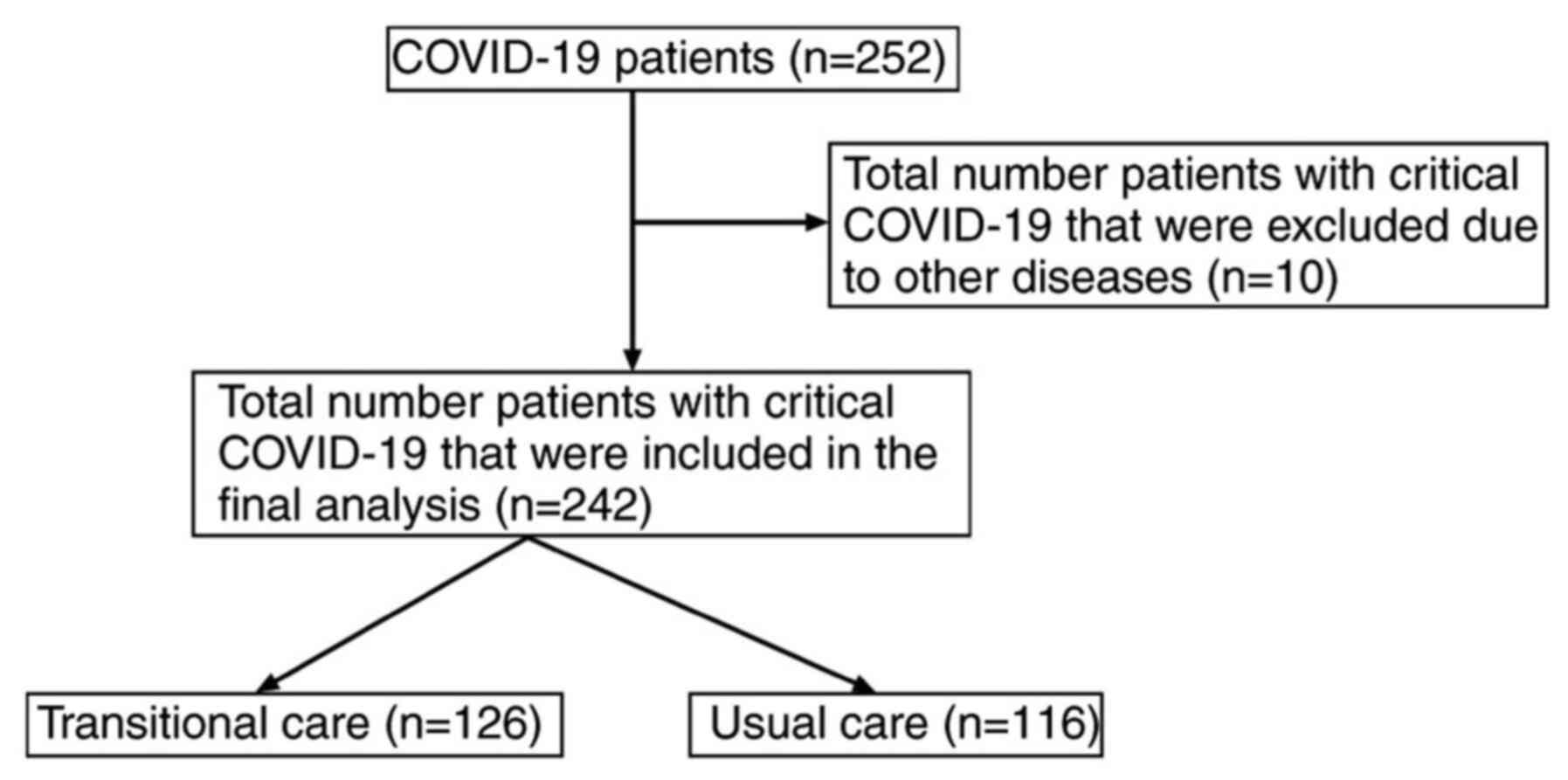
A total of 252 patients with COVID-19 pneumonia were
included in the analysis. A total of 10 patients were excluded
according to the exclusion criteria. Demographic and baseline
clinical characteristics of the patients with COVID-19 (n=242) are
presented in Table I. The most
common symptoms of the patients were fever, dyspnea, asthenia and
cough. The cohort included 128 male (52.9%) and 114 female patients
(47.1%) with a median age of 56.0 years (range, 45.0-65.0 years).
The patients with COVID-19 were assigned to receive either
transitional care (n=126) or usual care (n=116) (Fig. 1). All patients were generally well
balanced at the time of enrollment, i.e. there were no significant
differences between the two groups.
 | Table IPatient demographics and baseline
clinical characteristics. |
Table I
Patient demographics and baseline
clinical characteristics.
| Characteristic | Usual care
(n=116) | Transitional care
(n=126) | P-value |
|---|
| Age, years | 52.5±10.5 | 52.0±11.5 | 0.91 |
| Sex | | | |
|
Male | 62 (25.6) | 66 (27.3) | 0.96 |
|
Female | 58 (24.0) | 56 (23.1) | 0.85 |
| BMI,
kg/m2 | 28.0±4.2 | 28.2±4.5 | 0.96 |
| COVID-19
severity | | | |
|
Moderate | 46 (36.5) | 51 (40.1) | 0.87 |
|
Mild | 70 (63.5) | 75 (59.9) | 0.92 |
| Clinical
parameters | | | |
|
Respiratory
rate, cycles/min | 37.4±3.6 | 37.2±3.2 | 0.98 |
|
Heart rate,
beats/min | 97.5±14.6 | 96.5±13.5 | 0.95 |
|
Systolic
blood pressure, mmHg | 128.5±14.8 | 126.8±16.5 | 0.93 |
| Hospital admission
symptoms | | | |
|
Cough | 86 (74.1) | 88 (69.8) | 0.85 |
|
Fever
>38˚C | 72 (62.1) | 76 (60.3) | 0.96 |
|
Shortness of
breath | 56 (48.3) | 62 (49.2) | 0.91 |
|
Myalgia | 40 (34.5) | 45 (35.7) | 0.92 |
| Laboratory
parameters (normal ranges) | | | |
|
Hemoglobin,
g/dl (12-17) | 12.8±0.5 | 12.4±0.7 | 0.90 |
|
Creatinine,
mg/dl (0.6-1.2) | 1.1±0.3 | 1.2±0.4 | 0.93 |
|
Lactate,
mmol/l (1.0-2.5) | 1.8±0.6 | 1.7±0.5 | 0.98 |
|
INR
(0.8-1.2) | 1.4±0.3 | 1.5±0.4 | 0.96 |
|
White blood
cells, cells/mm3 (4-10) | 22.4±4.8 | 23.8±5.7 | 0.90 |
|
Lymphocytes,
109/l (1.1-3.2) | 0.9±0.3 | 1.0±0.4 | 0.99 |
|
Platelets,
cells/mm3 (150-450) | 214.5±54.2 | 225.8±60.4 | 0.86 |
| d-dimer, mcg/ml
(<1) | 2.8±1.2 | 3.0±1.4 | 0.95 |
| ALT, µ/l
(9-50) | 29.5±8.8 | 31.2±9.4 | 0.97 |
| AST, µ/l
(15-40) | 29.2±12.6 | 28.5±13.0 | 0.93 |
| Total bilirubin,
µmol/l (0-26) | 15.5±6.0 | 16.4±6.6 | 0.90 |
| Albumin, µ/l
(15-40) | 26.8±6.8 | 28.4±7.3 | 0.99 |
|
Positive-end-expiratory-pressure, cm x
H2O | 11.8±3.6 | 12.4±4.2 | 0.94 |
|
SpO2/FiO2 ratio | 155.4±30.8 | 162.6±33.5 | 0.95 |
Inflammation in patients with
COVID-19
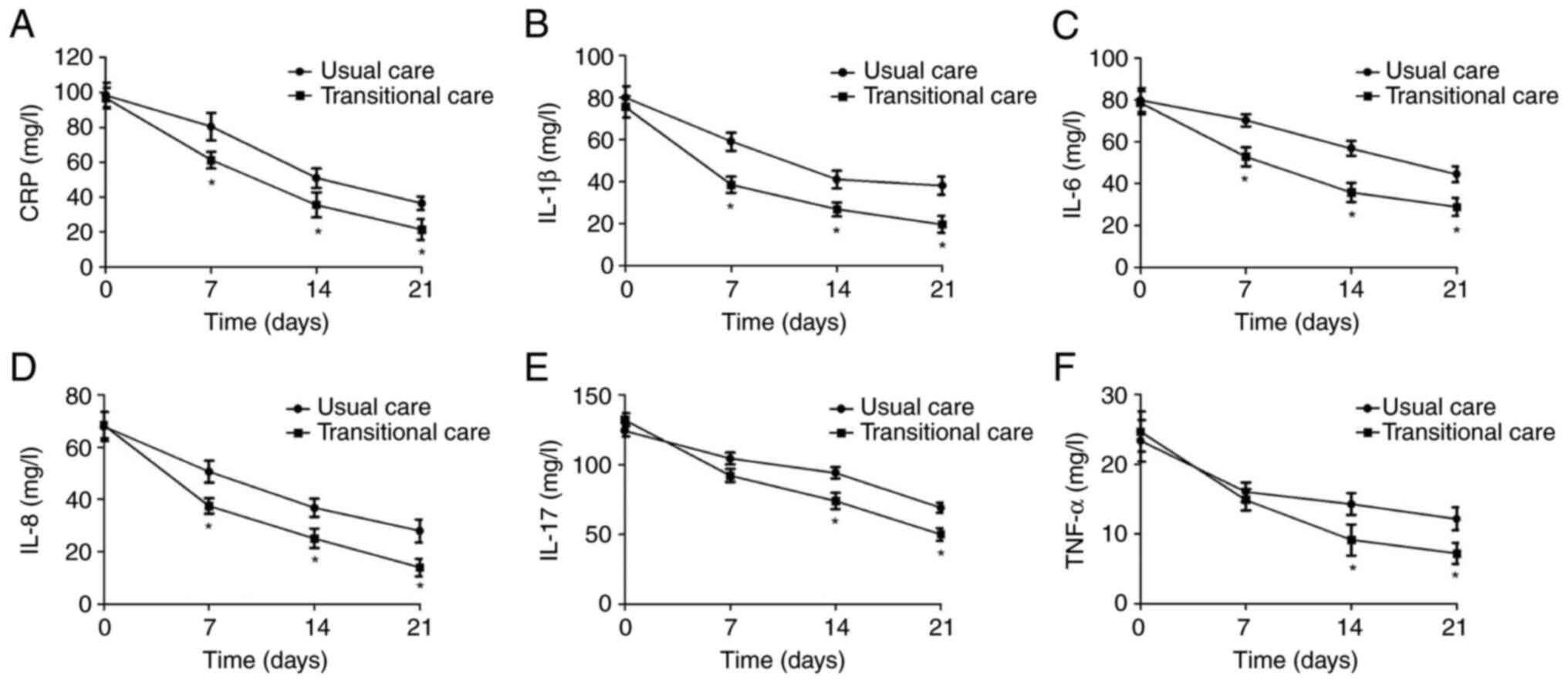
Inflammatory cytokines, including CRP, IL-1β, IL-6,
IL-8, IL-17 and TNF-α, analyzed in patients with COVID-19 at
discharge, were compared between the two groups. The baseline
levels of the inflammatory cytokines in the two groups are listed
in Table II. As indicated in
Fig. 2A, a decrease of CRP in
patients with COVID-19 in the transitional care group compared with
that in the usual care group was present on day 7, 14 and 21 during
hospitalization. A lower serum level of IL-1β was observed in
patients with COVID-19 in the transitional care group as compared
with that in the usual care group on day 7, 14 and 21 during
hospitalization (Fig. 2B). The
outcomes demonstrated that IL-6 and IL-8 levels were markedly
decreased in patients with COVID-19 on days 7, 14 and 21 of
hospitalization (Fig. 2C and
D). Compared with the usual care
group, transitional care decreased the serum levels of IL-17 and
TNF-α in patients with COVID-19 on days 14 and 21 of
hospitalization (Fig. 2D-F). At
discharge (median, 21.5; range, 14.5-27.5 days after the day of
hospitalization), no significant differences were observed between
the two groups (data not shown).
 | Table IIBaseline levels of inflammatory
cytokines in patients with coronavirus disease 2019 (mg/l). |
Table II
Baseline levels of inflammatory
cytokines in patients with coronavirus disease 2019 (mg/l).
| Parameter | Usual care | Transitional
care | P-value |
|---|
| CRP | 93.6±8.7 | 94.8±10.2 | 0.84 |
| IL-1β | 78.2±12.0 | 75.7±12.1 | 0.94 |
| IL-6 | 78.2±12.0 | 80.3±14.4 | 0.95 |
| IL-8 | 68.5±16.4 | 71.2±18.8 | 0.96 |
| IL-17 | 124.5±25.8 | 132.0±22.5 | 0.83 |
| TNF-α | 22.4±5.7 | 23.0±4.9 | 0.88 |
Pulmonary function in patients with
COVID-19
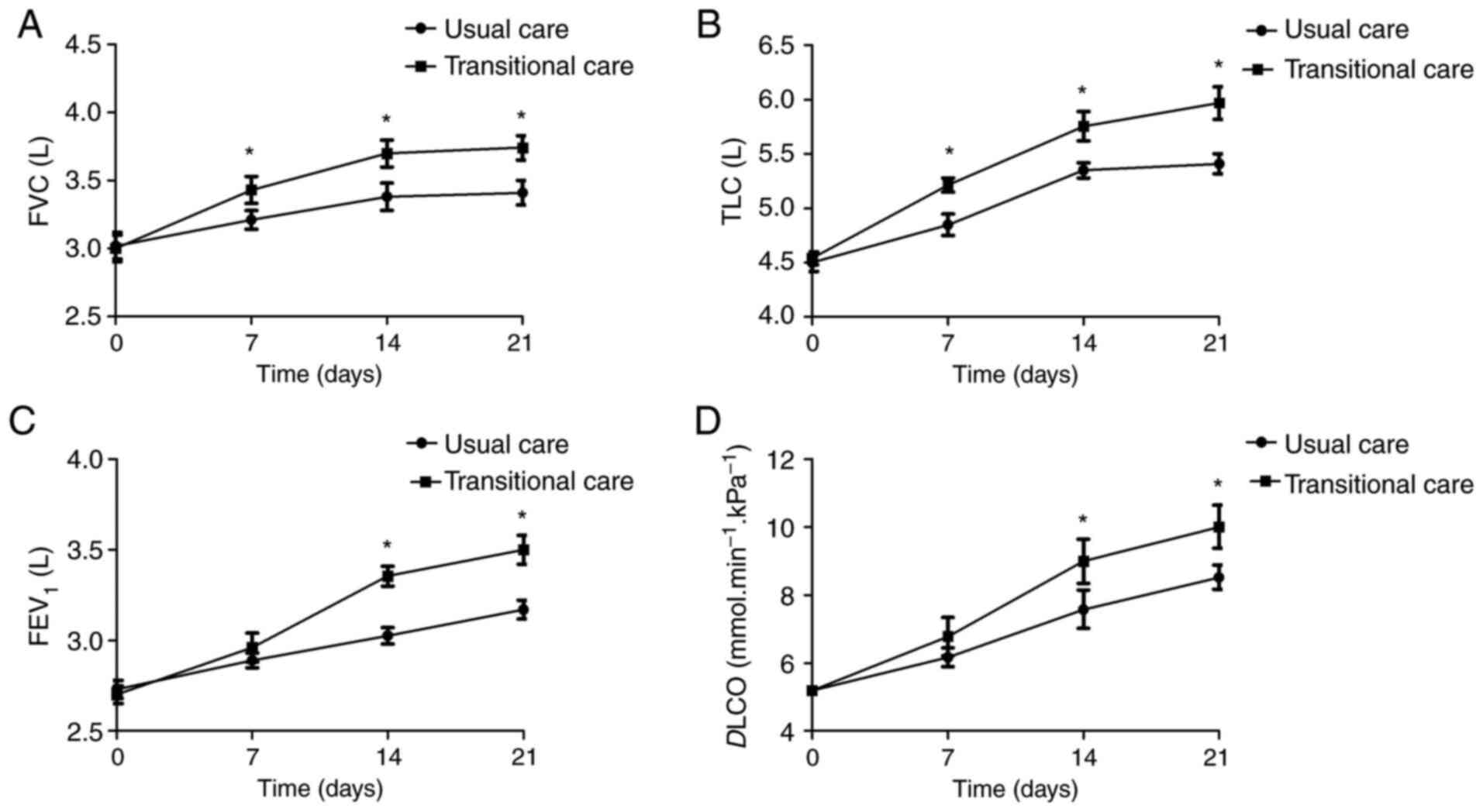
Pulmonary function was recorded in patients with
COVID-19 between the transitional care and usual care group. The
baseline parameters of pulmonary function in the two groups are
listed in Table III. Fig. 3 provides the results of pulmonary
function in patients with COVID-19 in the two groups over the
course of hospitalization. Patients in transitional care had better
pulmonary function than those in the usual care group. The mean
values of FVC, TLC, FEV1 and DLCO were relatively
higher in patients with COVID-19 in the transitional care group
compared to those in the usual care group. Only a small number of
the patients required oxygen supplementation in the two groups and
none of the patients was intubated or admitted to the intensive
care unit. Pulmonary function of patients post-discharge did not
significantly differ between the two groups (P>0.05; data not
shown).
 | Table IIIBaseline pulmonary function in
patients with coronavirus disease 2019. |
Table III
Baseline pulmonary function in
patients with coronavirus disease 2019.
| Pulmonary function
parameter | Usual care | Transitional
care | P-value |
|---|
| FEV1/FVC, % | 86.0±13.6 | 84.3±11.9 | 0.90 |
| TLC, l | 4.5±1.5 | 4.4±1.3 | 0.88 |
| TLC, % pred | 105.2±16.7 | 102.2±12.8 | 0.93 |
| FVC, l | 2.7±0.5 | 2.7±0.6 | 0.97 |
| FVC, % pred | 93.2±18.7 | 91.8±15.4 | 0.95 |
| FEV1,
l | 2.80±0.63 | 2.72±0.57 | 0.88 |
| FEV1, l pred | 95.6±17.2 | 92.6±14.8 | 0.86 |
| DLCO, % pred | 94.1±15.8 | 93.5±16.2 | 0.98 |
|
PImax, kPa | 8.4±1.9 | 8.2±1.7 | 0.97 |
|
PEmax, kPa | 10.0±3.0 | 10.2±3.2 | 0.98 |
Mental and physical state of patients
with COVID-19
Patients with COVID-19 had reduced levels of
physical function and fitness in comparison to healthy controls.
Physical symptoms, including the quality of life and hospital stay,
as well as stress, fear, perception of helplessness, worry and
empathy of the patients for other patients affected were recorded
for patients with COVID-19 and compared between the transitional
care and usual care groups. Transitional care significantly
improved the quality of life and decreased stress, fear,
helplessness, worry and empathy in patients with COVID-19 at
discharge or post-discharge compared to usual care (Table IV). Transitional care also
decreased stress, fear, helplessness, worry and empathy of the
patients for other human patients affected in patients with
COVID-19 post-discharge compared with that in the usual care group
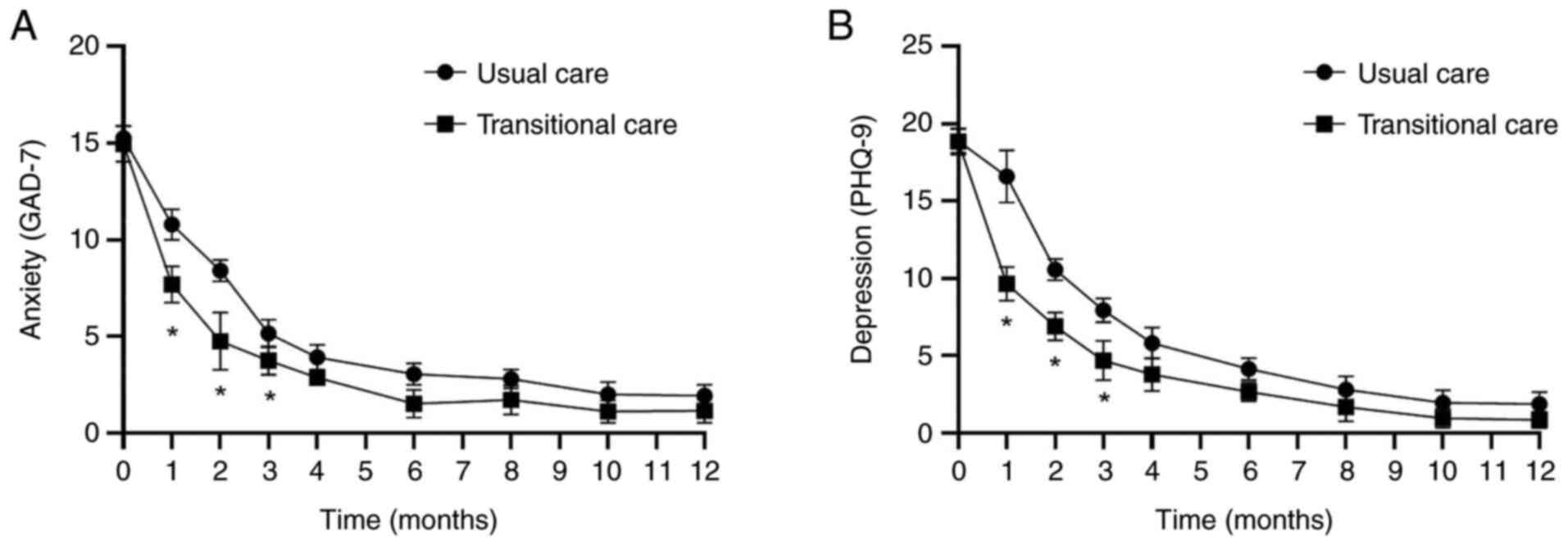
(Table IV). As indicated in
Table V, patients with COVID-19 at
discharge in the transitional care group exhibited significantly
decreased levels of depression and anxiety in comparison with those
in the usual care group at the indicated time-point (P<0.05).
Transitional care also improved depression and anxiety in patients
with COVID-19 during the first 3 months post-discharge. Data of
patients with COVID-19 with transitional care indicated that no
significant differences in depression and anxiety were present
between the two groups at the 12-month follow-up (Fig. 4). In addition, patients in the
transitional care group had a better 6-min walking distance than
those in the usual care group.
 | Table IVMental and physical state of patients
with coronavirus disease 2019. |
Table IV
Mental and physical state of patients
with coronavirus disease 2019.
| A, At
discharge |
|---|
| Item | Usual care | Transitional
care | P-value |
|---|
| Quality of
lifea | 74.0±8.2 | 82.8±12.4 | 0.032 |
| Hospital stay,
days | 15.5±4.5 | 12.0±3.5 | 0.046 |
| Fear | 46 (39.7) | 32 (25.4) | 0.017 |
| Feeling/perception
of helplessness | 58 (50.0) | 25 (19.8) | 0.0028 |
| Worry | 72 (62.1) | 30 (23.8) | 0.0030 |
| Empathy of the
patients for other patients affected | 50 (43.1) | 21 (16.7) | 0.040 |
| 6MWD, m | 465±56 | 582±64 | 0.010 |
| B,
Post-discharge |
| Item | Usual care | Transitional
care | P-value |
| Quality of
lifea | 83.3±7.6 | 89.5±8.5 | 0.048 |
| Fear | 15 (12.9) | 5 (4.0) | 0.013 |
| Feeling/perception
of helplessness | 18 (15.5) | 10 (7.9) | 0.024 |
| Worry | 14 (12.1) | 7 (5.6) | 0.016 |
| Empathy of the
patients for other patients affected | 10 (8.6) | 6 (4.8) | 0.038 |
| 6MWD, m | 618±94 | 676±104 | 0.042 |
| C, At
discharge |
| Item | Usual care | Transitional
care | P-value |
| Anxiety
(GAD-7) | 15.8±6.9 | 10.2±4.0 | 0.032 |
| Depression
(PHQ-9) | 16.2±5.2 | 9.2±4.5 | 0.027 |
| D, Post-discharge
(during three months) |
| Item | Usual care | Transitional
care | P-value |
| Anxiety
(GAD-7) | 8.4±3.1 | 5.0±2.5 | 0.020 |
| Depression
(PHQ-9) | 7.9±2.8 | 4.7±1.5 | 0.045 |
 | Table VSymptoms/complaints of patients with
coronavirus disease 2019 at discharge. |
Table V
Symptoms/complaints of patients with
coronavirus disease 2019 at discharge.
| Adverse event | Usual care | Transitional
care | P-value |
|---|
| Dyspnea | 18 (15.5) | 9 (7.1) | 0.037 |
| Asthenia | 16 (13.8) | 9 (7.1) | 0.043 |
| Cough | 26 (22.4) | 16 (12.7) | 0.035 |
| Headache | 10 (8.6) | 5 (4.0) | 0.016 |
| Chest pain | 32 (27.6) | 20 (15.9) | 0.019 |
| Nausea | 17 (14.7) | 10 (7.9) | 0.048 |
| Fever | 86 (74.1) | 60 (47.6) | 0.011 |
| Myalgia | 45 (38.8) | 32 (25.4) | 0.045 |
| Diarrhea | 15 (12.9) | 8 (6.3) | 0.034 |
| Dizziness | 20 (17.2) | 13 (10.3) | 0.030 |
| Conjunctivitis | 23 (19.8) | 13 (10.3) | 0.040 |
| Loss of smell | 36 (31.0) | 25 (19.8) | 0.025 |
| Loss of taste | 38 (32.8) | 27 (21.4) | 0.046 |
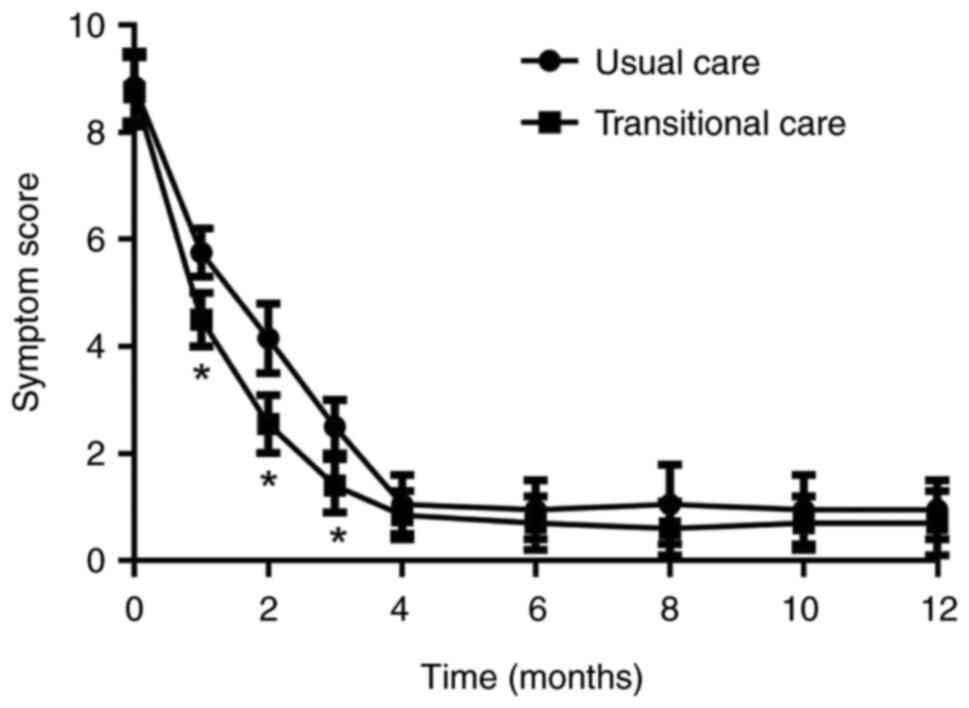
Symptoms and complaints in patients
with COVID-19 at discharge and post-discharge
Symptoms/complaints in patients with COVID-19 at
discharge or post-discharge were compared between the two groups.
Transitional care efficiently improved the most common
symptoms/complaints of patients, including dyspnea, asthenia,
cough, nausea, chest pain, myalgia, headache, fever, diarrhea,
chest pain, dizziness, conjunctivitis, disorders of smell and taste
compared to patients in usual care (Table V). There were no significant
differences in the most common symptoms for patients post-discharge
between the two groups. Symptom scores were higher in the
transitional care group than those in the usual care group for
patients with COVID-19 during the first three months after
discharge (P<0.05), while no significant differences were
observed for patients with COVID-19 after 3 months post-discharge
(P>0.05; Fig. 5).
Recurrence of patients with COVID-19
post-discharge
The recurrence rate (patients having a
relapse/re-infection with COVID-19) of patients with COVID-19 was
recorded during the 12-month follow-up. Data revealed that
transitional care decreased the recurrence of patients with
COVID-19 post-discharge compared with that in the usual care group
(Table VI). A total of 3 (2.4%)
patients had complications that required readmission to the
hospital in the transitional care group, while the number of
recurrences of patients with COVID-19 post-discharge was 10 (8.6%).
Furthermore, one (0.7%) patient with COVID-19 in the transitional
care group and 4 (3.4%) patients with COVID-19 in the usual care
group required oxygen therapy again during the recurrence.
 | Table VIRecurrence of patients with
coronavirus disease 2019 post-discharge. |
Table VI
Recurrence of patients with
coronavirus disease 2019 post-discharge.
| Parameter | Usual care | Transitional
care | P-value |
|---|
| Recurrence | 10 (8.6) | 3 (2.4) | 0.011 |
| Oxygen therapy (at
the hospital) | 1 (0.7) | 4 (3.4) | 0.044 |
Discussion
Care for patients with COVID-19 during
hospitalization and discharge may be necessary. The interventions
necessary to care for patients with COVID-19 are performed by
nurses under the condition of adequate prevention (25). Adequate transitional care possibly
results in good post-discharge outcomes in patients with
COVID-19(12). The present study
demonstrated that transitional care not only improved the mental
health, inflammation and pulmonary function in patients with
COVID-19, but also decreased the adverse events and recurrence of
COVID-19.
The pulmonary characteristics in patients with
COVID-19 are ground-glass opacity admixed with reticulation and
linear opacities, along with signs of architectural distortion and
bronchial dilatation (26). The
results of a previous study indicated that lymphocyte percentages,
neutrophils and CRP may be used as markers for COVID-19, helping to
prioritize certain individuals (27). Correlations between severity and
levels of IL-1 and IL-18 were previously reported to be useful in
COVID-19 treatment (28). Serum
IL-6 is one promising novel biomarker for evaluating the severity
of COVID-19(29). In hospitalized
patients with severe COVID-19, decreasing IL-17 levels may mitigate
the inflammatory response and improve oxygenation, but does not
affect the requirement for mechanical ventilation and psychological
symptoms (30). Serum
concentrations of TNF-α and IL-17A are more elevated in patients
with COVID-19, which opens a new field of research for
COVID-19(31). The present results
suggested that transitional care efficiently improved the serum
levels of inflammatory cytokines, including CRP, IL-1β, IL-6, IL-8,
IL-17 and TNF-α, of patients with COVID-19 at discharge. Certain
evidence demonstrated that inflammation in certain patients with
COVID-19 was closely related to the severity of this disease and
subsequent sequelae (32).
Overall, the present results indicated that transitional care
significantly improved pulmonary function of patients with COVID-19
at discharge and post-discharge. In addition, transitional care
decreased inflammatory cytokines in patients with COVID-19 at
discharge. Of note, transitional care contributed to the decrease
of adverse events and recurrence. However, it remains elusive
whether transitional care will progress to symptomatic pulmonary
function or if transitional care for COVID-19 may influence the
treatment outcome at discharge.
COVID-19 may have caused mental health changes in
numerous individuals (33).
Certain hospitalized patients who have already been affected by the
virus may still receive medical treatment. In the present study,
patients with COVID-19 receiving transitional care had markedly
improved mental health issues, including depression and anxiety
symptoms at discharge or post-discharge. Compared to the control,
transitional care markedly improved the emotional wellbeing of the
patients, including stress, fear, perception of helplessness, worry
and empathy, as determined by using standard questionnaires for
patients with COVID-19. All questionnaires on emotions for certain
variables were available for each patient with COVID-19. Regarding
psychological symptoms in the patients with COVID-19, patients who
received management with transitional care had an overall
improvement of 92.7%, which was higher compared to the control
group, and this has been recognized as one of the best indicators
of prognosis. Consistent with previous studies (34,35),
the present data indicated that the hospital stay was shorter in
the transitional care group, although no significant differences of
nausea, chest pain, fever, diarrhea, chest pain, dizziness,
conjunctivitis, disorders of smell and taste for patients
post-discharge were observed between the transitional care and
usual care group. Of note, an inflammatory rebound triggered by an
inadequate immune response may constitute an alternative
explanation for the recurrence of patients with COVID-19(36). The results of the present study
suggested that transitional care reduced the recurrence of patients
with COVID-19, which may be due to the decrease of serum levels of
inflammatory cytokines. Data from patients suggested that
transitional care improved psychosocial stress, depression and
anxiety by post-discharge hospital visits, home health supervision,
monitoring of medications and discontinuation of isolation, which
may contribute to the decrease of adverse events and recurrence in
patients with COVID-19. However, these preliminary data are only
supportive and suggest the requirement for further study to
determine whether patients with COVID-19 with risk factors of
recurrence should be prioritized for transitional care.
Of note, the present study had certain limitations.
The study involved transitional care from a single center and may
not reflect all the effects of transitional care on the recurrence
of patients with COVID-19 in different countries. In addition,
although data in the present study indicate that transitional care
decreases serum levels of inflammatory cytokines, it cannot be
excluded that different populations of patients with COVID-19 with
different medical treatments may have different tendencies.
Furthermore, it is important to mention that long-term follow-up
was not investigated in the present study, at best the efficacy of
transitional care has been explored.
In conclusion, the fact that patients with COVID-19
may experience re-activation of the virus or re-infection, as well
as potential sequelae of this disease, highlights the importance of
transitional care for the management and prevention of the pandemic
in the world. The results of the present study indicate that
transitional care provides benefits in the recovery of COVID-19
virus-induced inflammation, improving physical symptoms and mental
health, as well as decreasing adverse events and recurrence. The
present study highlighted the value of transitional care for health
care systems, which suggests that transitional care should be
developed to ensure better pulmonary function, quality of life,
physical symptoms, mental health status and lower recurrence in
patients with COVID-19.
Acknowledgements
The authors thank Dr Haili Zhang (Nursing School,
Qiqihar Medical University, Qiqihar, China) for language editing
and acting as an advisor for the recruitment of patients.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LLS designed the project, wrote the manuscript and
performed data analysis. BXL and JL performed experiments. CYH
designed the study and wrote the manuscript. LLS and CYH authors
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Ethical approval was granted by the ethics
committees of Mudanjiang Medical University (Mudanjiang, China;
approval no. 20201001X1). All patients provided written informed
consent to participate in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhong M, Sun A, Xiao T, Yao G, Sang L,
Zheng X, Zhang J, Jin X, Xu L, Yang W, et al: A randomized,
single-blind, group sequential, active-controlled study to evaluate
the clinical efficacy and safety of α-lipoic acid for critically
Ill patients with coronavirus disease 2019 (COVID-19). Front Med
(Lausanne). 8(566609)2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Danion F, Letscher-Bru V, Guitard J,
Sitbon K, Dellière S, Angoulvant A, Desoubeaux G, Botterel F,
Bellanger AP, Gargala G, et al: Coronavirus disease 2019-associated
Mucormycosis in France: A rare but deadly complication. Open Forum
Infect Dis. 9(ofab566)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He
JX, Liu L, Shan H, Lei CL, Hui DSC, et al: Clinical characteristics
of coronavirus disease 2019 in China. N Engl J Med. 382:1708–1720.
2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Popov GT, Baymakova M, Vaseva V,
Kundurzhiev T and Mutafchiyski V: Clinical characteristics of
hospitalized patients with COVID-19 in Sofia, Bulgaria. Vector
Borne Zoonotic Dis. 20:910–915. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lechien JR, Chiesa-Estomba CM, Place S,
Van Laethem Y, Cabaraux P, Mat Q, Huet K, Plzak J, Horoi M, Hans S,
et al: Clinical and epidemiological characteristics of 1420
European patients with mild-to-moderate coronavirus disease 2019. J
Intern Med. 288:335–344. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kim PS, Schildhouse RJ, Saint S, Bradley
SF, Chensue S, Houchens N and Gupta A: Vaccine breakthrough
infections in veterans hospitalized with coronavirus infectious
disease-2019: A case series. Am J Infect Control. 50:273–276.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ahmad Khidir K: Coronavirus disease 2019
vaccine hesitancy in the kurdistan region: A cross-sectional
national survey. Arch Razi Inst. 76:751–759. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zafari M, Rad MTS and Mohseni F:
Coronavirus disease 2019 (COVID-19) and pregnancy: A narrative
review. Curr Pediatr Rev. 18:97–102. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lima GRG, Albuquerque GMA, Amaral TLM and
Prado PRD: Nursing care to COVID-19 patients on hemodialysis and in
prone position: An experience report. Rev Esc Enferm USP.
55(e20210118)2021.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
10
|
Fonss Rasmussen L, Grode LB, Lange J,
Barat I and Gregersen M: Impact of transitional care interventions
on hospital readmissions in older medical patients: A systematic
review. BMJ Open. 11(e040057)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Borgen I, Romney MC, Redwood N, Delgado B,
Alea P, George BH, Puzziferro J and Shihabuddin L: From hospital to
home: An intensive transitional care management intervention for
patients with COVID-19. Popul Health Manag. 24:27–34.
2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sumikawa Y and Yamamoto-Mitani N:
Transitional care during COVID-19 pandemic in Japan: Calls for new
strategies to integrate traditional approaches with information and
communication technologies. Biosci Trends. 15:55–57.
2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wang Z, Deng H, Ou C, Liang J, Wang Y,
Jiang M and Li S: Clinical symptoms, comorbidities and
complications in severe and non-severe patients with COVID-19: A
systematic review and meta-analysis without cases duplication.
Medicine (Baltimore). 99(e23327)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Pamukcu B: Inflammation and thrombosis in
patients with COVID-19: A prothrombotic and inflammatory disease
caused by SARS coronavirus-2. Anatol J Cardiol. 24:224–234.
2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wang Y, Zhang D, Du G, et al: Remdesivir
in adults with severe COVID-19: A randomised, double-blind,
placebo-controlled, multicentre trial. Lancet. 395:1569–1578.
2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zhang X, Li Y, Li H, Zhao Y, Ma D, Xie Z
and Sun J: Application of the OMAHA System in the education of
nursing students: A systematic review and narrative synthesis.
Nurse Educ Pract. 57(103221)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Stocker R, Tran T, Hammarberg K, Nguyen H,
Rowe H and Fisher J: Patient health questionnaire 9 (PHQ-9) and
general anxiety disorder 7 (GAD-7) data contributed by 13,829
respondents to a national survey about COVID-19 restrictions in
Australia. Psychiatry Res. 298(113792)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Obbarius A, van Maasakkers L, Baer L,
Clark DM, Crocker AG, de Beurs E, Emmelkamp PMG, Furukawa TA,
Hedman-Lagerlöf E, Kangas M, et al: Standardization of health
outcomes assessment for depression and anxiety: Recommendations
from the ICHOM depression and anxiety working group. Qual Life Res.
26:3211–3225. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Karahan I: The COVID-19 anxiety of
hospitalised patients in a palliative care unit. Int J Palliat
Nurs. 26(267)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bai Y, Lin CC, Lin CY, Chen JY, Chue CM
and Chou P: Survey of stress reactions among health care workers
involved with the SARS outbreak. Psychiatr Serv. 55:1055–1057.
2004.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Greco F, Altieri VM, Esperto F, Mirone V
and Scarpa RM: Impact of COVID-19 pandemic on health-related
quality of life in Uro-oncologic patients: What should we wait for?
Clin Genitourin Cancer. 19:e63–e68. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Graham BL, Brusasco V, Burgos F, Cooper
BG, Jensen R, Kendrick A, MacIntyre NR, Thompson BR and Wanger J:
2017 ERS/ATS standards for single-breath carbon monoxide uptake in
the lung. Eur Respir J. 49(1600016)2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chirico D, Davidson TW, Terada T, Scott K,
Keast ML, Reid RD, Pipe AL and Reed JL: Using the 6-min walk test
to monitor peak oxygen uptake response to cardiac rehabilitation in
patients with heart failure. J Cardiopulm Rehabil Prev. 40:378–382.
2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Perez-Gomez B, Pastor-Barriuso R,
Perez-Olmeda M, Hernán MA, Oteo-Iglesias J, Fernández de Larrea N,
Fernández-García A, Martín M, Fernández-Navarro P, Cruz I, et al:
ENE-COVID nationwide serosurvey served to characterize asymptomatic
infections and to develop a symptom-based risk score to predict
COVID-19. J Clin Epidemiol. 139:240–254. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Jia Y, Chen O, Xiao Z, Xiao J, Bian J and
Jia H: Nurses' ethical challenges caring for people with COVID-19:
A qualitative study. Nurs Ethics. 28:33–45. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Tomidokoro D, Hayama H, Okazaki T, Hara H
and Hiroi Y: The effect of the COVID-19 pandemic on incidence and
characteristics of pulmonary embolism. Glob Health Med. 3:122–124.
2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ibnouf AO, Khalil MH, Khalid R, Elshibli
EM, Elsayed O and Fadl-Elmula I: Blood markers (lymphocyte
percentages, neutrophils, CRP and ESR) can help in prioritizing
rRT-PCR test for suspected COVID-19 patients in countries with
limited health resources. Pan Afr Med J. 37(331)2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kerget B, Kerget F, Aksakal A, Askin S,
Saglam L and Akgun M: Evaluation of alpha defensin, IL-1 receptor
antagonist, and IL-18 levels in COVID-19 patients with macrophage
activation syndrome and acute respiratory distress syndrome. J Med
Virol. 93:2090–2098. 2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Tang J, Lin J, Zhang E, Zhong M, Luo Y, Fu
Y and Yang Y: Serum IL-6 and procalcitonin are two promising novel
biomarkers for evaluating the severity of COVID-19 patients.
Medicine (Baltimore). 100(e26131)2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Avdeev SN, Trushenko NV, Tsareva NA,
Yaroshetskiy AI, Merzhoeva ZM, Nuralieva GS, Nekludova GV, Chikina
SY, Gneusheva TY, Suvorova OA and Shmidt AE: Anti-IL-17 monoclonal
antibodies in hospitalized patients with severe COVID-19: A pilot
study. Cytokine. 146(155627)2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Leija-Martinez JJ, Huang F,
Del-Rio-Navarro BE, Sanchéz-Muñoz F, Muñoz-Hernández O,
Giacoman-Martínez A, Hall-Mondragon MS and Espinosa-Velazquez D:
IL-17A and TNF-α as potential biomarkers for acute respiratory
distress syndrome and mortality in patients with obesity and
COVID-19. Med Hypotheses. 144(109935)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Guo J, Lin WW, Zucker JE, Nandakumar R,
Uhlemann AC, Wang S and Shivakoti R: Inflammation and mortality in
COVID-19 hospitalized patients with and without type 2 diabetes. J
Clin Endocrinol Metab. 107:e1961–e1968. 2022.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Shaku F, Ishiburo M, Miwa M and Maruoka S:
Mental Health Status before and during the COVID-19 pandemic in
patients first visiting a psychosomatic internal medicine clinic in
Tokyo, Japan. Int J Environ Res Public Health.
19(2488)2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Loerinc LB, Scheel AM, Evans ST, Shabto
JM, O'Keefe GA and O'Keefe JB: Discharge characteristics and care
transitions of hospitalized patients with COVID-19. Healthc (Amst).
9(100512)2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
McDonagh JE, Tattersall R, Clinch J, Swan
J, Foster HE and McCann L: Developmentally appropriate transitional
care during the Covid-19 pandemic for young people with
juvenile-onset rheumatic and musculoskeletal diseases: The
rationale for a position statement. Pediatr Rheumatol Online J.
19(136)2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Adrielle Dos Santos L, Filho PGG, Silva
AMF, Santos JVG, Santos DS, Aquino MM, de Jesus RM, Almeida MLD, da
Silva JS, Altmann DM, et al: Recurrent COVID-19 including evidence
of reinfection and enhanced severity in thirty Brazilian healthcare
workers. J Infect. 82:399–406. 2021.PubMed/NCBI View Article : Google Scholar
|