Introduction
Cervical spondylotic myelopathy (CSM) is primarily
caused by chronic compression or insufficient blood supply to the
cervical spinal cord due to cervical disc herniation, spinal
stenosis or instability (1).
Clinical manifestations include sensory, motor, reflex and
defecation dysfunction of the spinal nerves. If the disease is
allowed to progress, it may cause complications such as paralysis
and death (2,3). To the best of our knowledge, there is
currently no evidence that indicates the optimal treatment for
patients with CSM and decompression surgery remains the most
effective long-term treatment for this disease (3). Anterior cervical corpectomy and
fusion (ACCF) is a commonly used surgical method for CSM with good
clinical results (1). Neurological
deficits leading to paralysis or paraplegia are rare; however,
there remains a serious potential postoperative complication. White
cord syndrome (WCS) is hypothesized to be a reperfusion injury
following sudden decompression of compressed spinal cord segments.
The blood supply to the affected area is notably increased, which
leads to direct blood trauma or subsequent injury caused by oxygen
free radicals (4,5). Postoperative MRI shows typical
sagittal T2-weighted magnetic resonance imaging (T2WI)
intramedullary high signal changes (6). It is a rare cause of acute onset
severe neurological deficit following cervical decompression.
However, WCS is a diagnosis of exclusion. Medically induced
technical trauma, postoperative hematoma, implant misalignment or
dislocation need to be excluded before WCS diagnosis (6).
Case presentation
A 54-year-old man was admitted to Jinhua Municipal
Central Hospital (Jinhua, China) in March 2021 with complaints of
numbness and weakness in limbs and swelling in the neck. His
myelopathic neurological examinations were negative. Physical
examination determined that the strength in his limbs was normal.
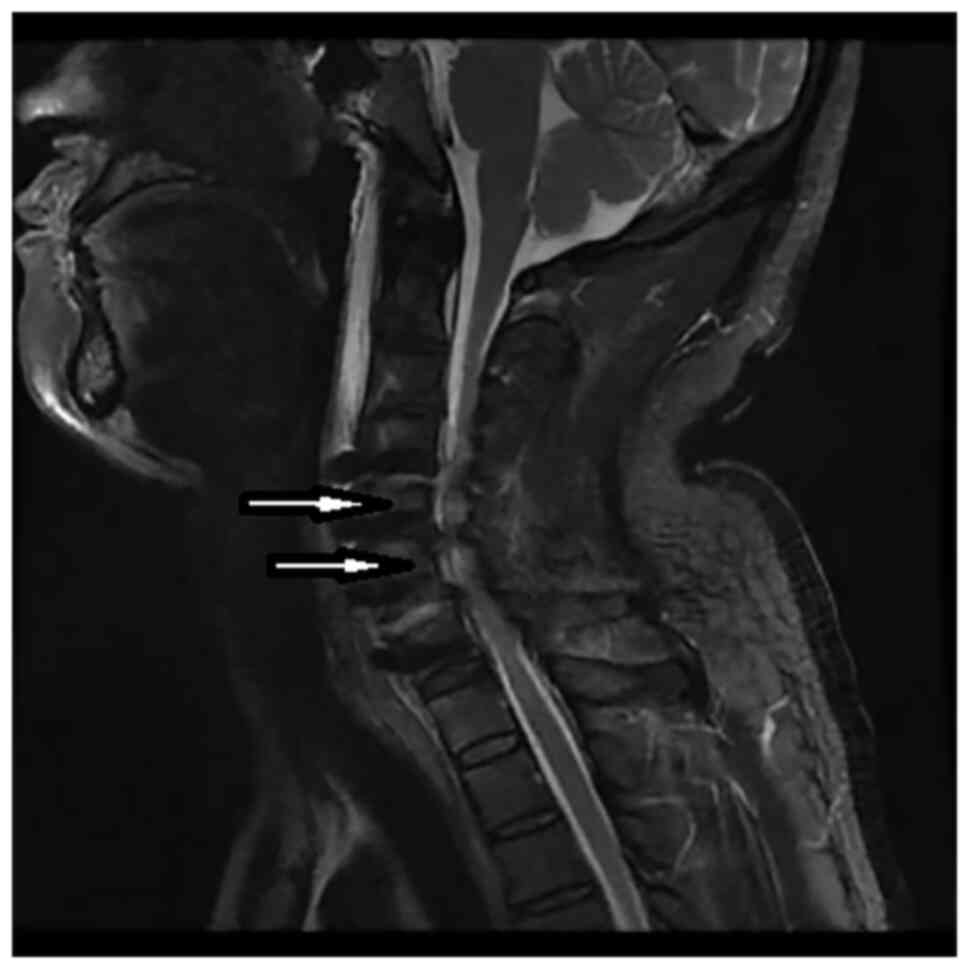
The preoperative cervical MRI scan showed degeneration and
herniation of the C4-C7 discs (Fig.
1). He was diagnosed with CSM. Following routine preoperative
preparation, ACCF C4-C7 surgery was performed. The cord was
decompressed by removing the C4-7 disc material. The interbody
cages were inserted into the C4-7 disc space and the plate was
fixed on the C4-7 body anterior surface. X-ray imaging displayed
satisfactory positioning of the pedicle screws. Following surgery,
the patient's motor and sensory impairments gradually improved.
However, on the 7th postoperative day, the patient was unable to
move his legs and arms. Physical examination revealed upper limb
strength of 3/5 and leg strength of 3/5 according to the Medical
Research Council scale (7).
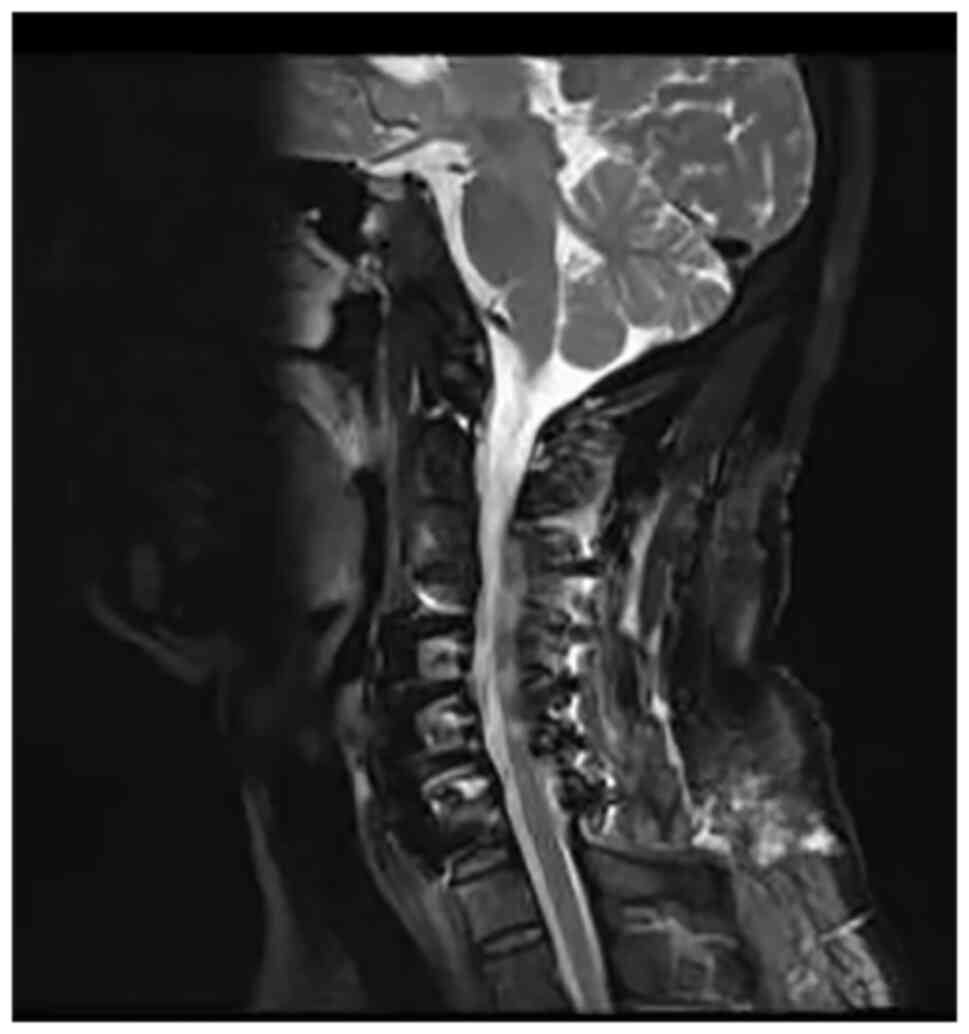
Emergency MRI demonstrated T2 high intramedullary signal at C5-C6
level (Fig. 2). He was diagnosed
with WCS and high dose methylprednisolone (80 mg, intravenously
twice/day) combined with mannitol (250 ml, intravenously twice/day)
and neurotrophic drug mecobalamin (0.5 mg, orally three times/day)
were administered. However, symptoms did not improve and posterior
cervical decompression surgery was performed 11 days after the
initial ACCF operation. The second postoperative cervical MRI scan
suggested that T2 high signal intensity had faded (Fig. 3). The patient recovered well
postoperatively. On day 5 post-surgery, the patient was treated
with hyperbaric oxygen therapy to decrease spinal cord edema and
improve reperfusion injury (8). On
the 10th day after the second surgery, the patient's muscle
strength in the limbs recovered to grade 4/5 and the strength in
the legs recovered to grade 5/5. The patient was discharged to an
inpatient rehabilitation center. The patient's neurological
function had not deteriorated at the 7-month postoperative
follow-up.
Discussion
There are multiple reasons for paralysis following
cervical spine surgery, including spinal cord compression due to
poor implantation or hematoma formation, edema and
ischemia-reperfusion injury (9).
Preoperative MRI can clarify the site and type of cervical disc
herniation and the extent of damage to the spinal cord and nerve
roots. It provides a reference for the diagnosis, choice of
treatment and prognosis of cervical spondylosis (10). Postoperative MRI can exclude WCS if
it detects extramedullary hematoma, residual exogenous spinal cord
compression, intraoperative spinal cord injury or postoperative
graft displacement (6). WCS is a
rare surgical complication that is characterized by spinal cord
ischemic-reperfusion injury following anterior or posterior
cervical decompression (5). It is
characterized by an increased intramedullary cord signal on
postoperative T2WI scan (9). In
the chronically compressed ischemic spinal cord, the blood-spinal
cord barrier is destroyed and exposed to a large blood supply
following decompression surgery (11). This triggers an inflammatory
cascade and the release of oxygen free radicals that leads to
neuronal membrane damage (12).
Surgical techniques and drug interventions, such as
methylprednisolone, have been shown to decrease ischemic spinal
cord injury (5). Potent
antioxidants also serve a role in the treatment of spinal cord
ischemia-reperfusion injury (13).
Chin et al (5) first proposed the concept of WCS in
2013 and highlighted the increased intramedullary signal in the
postoperative T2WI scan. It was reported that a patient developed
quadriplegia following C4-C6 anterior cervical discectomy and
fusion surgery and was immediately given more extensive
decompression and steroid therapy. The patient's condition
partially improved. Subsequently, WCS received increasing
attention. Vinodh et al (14) reported that a 51-year-old woman
diagnosed with a metastatic intraspinal tumor developed WCS
following posterior cervical laminectomy and tumor resection and
fusion. Zhang et al (9)
reported three cases of transient paralysis within 4 h after ACCF.
All three patients received high-dose methylprednisolone treatment.
Symptoms were resolved in two of the patients however, the third
continued to show incomplete quadriplegia. The surgeon decided to
perform C3-C6 laminoplasty to provide additional decompression. The
second postoperative MRI showed a decrease in both the intrinsic
cord edema and high intramedullary cord signal. After one week, the
patient's nerve function was fully restored. Sepulveda et al
(15) reported the first case of
WCS in a pediatric patient. A 12-year-old child underwent posterior
cervical decompression surgery and fenestration of arachnoid cyst.
On the 4th postoperative day, the patient developed monoplegia of
the right arm and had a favorable clinical response to high-dose
steroids. With rehabilitation treatment, the mobility of the right
arm began to improve. More than ten cases have been reported in the
literature and all cases of WCS were managed with high doses of
steroids (4,5,9,11,12,14,15).
In the present case report, high intramedullary signal was observed
on postoperative sagittal T2WI scans, suggesting potential spinal
cord edema. However, there is still debate regarding the clinical
relevance of high signal intensity on T2WI (10). Localized spinal cord edema, nerve
cell demyelination and cystic degeneration of the spinal cord may
contribute to high signal intensity on T2WI. In previous case
reports, the neurological deficit occurred intraoperatively or 24 h
postoperatively, whereas in the present case the deficit first
manifested 7 days postoperatively. It was hypothesized that this
late-onset of WCS was caused by subacute reperfusion due to
endothelial injury and atherosclerosis.
Although the incidence of WCS is low, clinicians
should be aware of this potentially harmful complication. Once
paralysis occurs, early diagnosis and intervention are essential to
restoring spinal function. High-dose methylprednisolone is the
first step in intervention. Additional surgery is dependent on the
efficacy of the drug. In addition, it is recommended that surgeons
include this complication in written consent before spinal
surgery.
The insufficient number of cases limits the
identification of specific WCS risk factors. Further research is
required to investigate the exact mechanism of WCS to establish
timely treatment or prevention of this rare but destructive
complication.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated and/or analyzed during the
present study are included in this published article.
Authors' contributions
CZL designed the study, collected clinical data and
drafted the manuscript. DJG and YFZ designed the study and
critically revised the manuscript. CZL, YFZ and DJG confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki and approved by the Ethics Committee
of Jinhua Municipal Central Hospital (approval no. 2021-213).
Written informed consent was provided by the patient.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Badhiwala JH, Ahuja CS, Akbar MA, Witiw
CD, Nassiri F, Furlan JC, Curt A, Wilson JR and Fehlings MG:
Degenerative cervical myelopathy-update and future directions. Nat
Rev Neurol. 16:108–124. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tetreault LA, Karadimas S, Wilson JR,
Arnold PM, Kurpad S, Dettori JR and Fehlings MG: The natural
history of degenerative cervical myelopathy and the rate of
hospitalization following spinal cord injury: An updated systematic
review. Global Spine J. 7 (Suppl 3):28S–34S. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tu J, Vargas Castillo J, Das A and Diwan
AD: Degenerative cervical myelopathy: Insights into its
pathobiology and molecular mechanisms. J Clin Med.
10(1214)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Antwi P, Grant R, Kuzmik G and Abbed K:
‘White cord syndrome’ of acute hemiparesis after posterior cervical
decompression and fusion for chronic cervical stenosis. World
Neurosurg. 113:33–36. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Chin KR, Seale J and Cumming V: ‘White
cord syndrome’ of acute tetraplegia after anterior cervical
decompression and fusion for chronic spinal cord compression: A
case report. Case Rep Orthop. 2013(697918)2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Epstein NE: Reperfusion injury (RPI)/white
cord syndrome (WCS) due to cervical spine surgery: A diagnosis of
exclusion. Surg Neurol Int. 11(320)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Vanpee G, Hermans G, Segers J and
Gosselink R: . Assessment of limb muscle strength in critically ill
patients: A systematic review. Crit Care Med. 42:701–711.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Brugniaux JV, Coombs GB, Barak OF, Dujic
Z, Sekhon MS and Ainslie PN: Highs and lows of hyperoxia:
Physiological, performance, and clinical aspects. Am J Physiol
Regul Integr Comp Physiol. 315:R1–R27. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zhang JD, Xia Q, Ji N, Liu YC, Han Y and
Ning SL: Transient paralysis shortly after anterior cervical
corpectomy and fusion. Orthop Surg. 5:23–28. 2013.PubMed/NCBI View
Article : Google Scholar
|
|
10
|
Zileli M, Borkar SA, Sinha S, Reinas R,
Alves ÓL, Kim SH, Pawar S, Murali B and Parthiban J: Cervical
spondylotic myelopathy: Natural course and the value of diagnostic
techniques-WFNS spine committee recommendations. Neurospine.
16:386–402. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Busack CD and Eagleton BE: White cord
syndrome causing transient tetraplegia after posterior
decompression and fusion. Ochsner J. 20:334–338. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wiginton J IV, Brazdzionis J, Mohrdar C,
Sweiss R and Lawandy S: Spinal cord reperfusion injury: Case
report, review of the literature, and future treatment strategies.
Cureus. 11(e5279)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Shirley R, Ord ENJ and Work LM: Oxidative
stress and the use of antioxidants in stroke. Antioxidants (Basel).
3:472–501. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Vinodh VP, Rajapathy SK, Sellamuthu P and
Kandasamy R: White cord syndrome: A devastating complication of
spinal decompression surgery. Surg Neurol Int.
9(136)2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sepulveda F, Carballo L, Carnevale M and
Yañez P: White cord syndrome in a pediatric patient: A case report
and review. Radiol Case Rep. 15:2343–2347. 2020.PubMed/NCBI View Article : Google Scholar
|