Introduction
As the prevalence of kidney stone disease rises, a
number of patients will need a minimally invasive procedure to
remove kidney stones. In the 1970s, percutaneous nephrolithotomy
(PCNL) was introduced as a less invasive option for kidney stone
removal and it underwent additional development in the following
years (1). However, extracorporeal
shock wave lithotripsy was introduced in the early 1980s,
decreasing PCNL frequency. Recent years have seen a redefining of
the function of PCNL for treating urolithiasis, as clinical
experience with ESWL has highlighted its limits (1). Nowadays, PCNL is a ubiquitous
technique. In a recent survey by Jiang et al (2), ~80.5% of urologists in China practice
PCNL and 96.2% said they like to perform it. According to the
European Association of Urology, PCNL is recommended as the
first-line treatment for kidney stones >2 cm and/or staghorn
stones (3).
Technical advances have led to a significant
reduction in the morbidity and mortality of this surgical
technique. However, PCNL is not a risk-free intervention. According
to Sharma et al (4), the
rate of complications varies considerably, being between 3-83%. The
most common are bleeding, pneumothorax, hydro/hemothorax, urinary
fistula, pleural effusion and urosepsis. Although postoperative
fever can be encountered in ≤30% of patients who undergo PCNL,
urosepsis is diagnosed, according to Michel et al (5), in 0.9-4.7%. A number of authors have
studied the factors that could favor the appearance of sepsis
following PCNL, but the results are inconclusive. Postoperative
infection is a common complication that, if untreated, can result
in septic shock. According to Yang et al (6), the fatality rate for urinary septic
shock can range from 25-60%, advances rapidly and is challenging to
treat. There is currently no standard recommendation for the risk
factors connected to postoperative infection. Preoperative urine
culture positivity, stone bacterial culture positivity, stone
burden, female gender, elderly gender, diabetes mellitus and
urinary tract obstruction are the key factors that lead to
postoperative infection (6). The
purpose of the present study was to analyze the data from the
literature to date to help clinicians manage the risks of PCNL so
that they become minimal.
Materials and methods
The present study performed this meta-analysis using
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
(PRISMA) 2020 reporting guidelines (7). A systematic Medline (https://pubmed.ncbi.nlm.nih.gov/) and Embase
(https://www.embase.com/) databases search was
performed, using the following words: ‘PCNL’ [MeSH Terms] AND
[‘sepsis’ (All Fields) OR ‘PCNL’ (All Fields)] AND [‘septic shock’
(All Fields)] AND [‘urosepsis’ (MeSH Terms) OR ‘Systemic
inflammatory response syndrome (SIRS)’ (All Fields)].
Inclusion criteria
Due to the technological advances in endourology,
the present study searched articles published between 2012 and
2022. Non-English language articles and those for which the full
text was unavailable were excluded. The leading search, as well as
screening for eligibility of titles, abstracts and full-text
articles, was completed independently by two authors and any
discrepancies were solved by consensus.
The present study selected studies with a control
group (non-SIRS/sepsis) and analyzed elements that favored the
appearance of sepsis after urological maneuvers. These have been
patients' age, diabetes mellitus, preoperative pyuria, positive
preoperative urine culture, operative time-minutes, multitract and
body mass index (BMI).
Statistical analysis
Heterogeneity in PCNL's infectious complications
outcome rate was assessed using I2 statistics. Review
Manager (RevMan), Version 5.4.1, and The Cochrane Collaboration,
2020, (both Cochrane) were used to calculate the individual odds
ratios (OR), P-value and personal and pooled mean differences with
corresponding 95% confidence interval (CI). A P-value <0.05 has
been considered statistically significant. The mean difference was
used to compare the outcomes following PCNL from the infectious
complications point of view. While random-effect models are
considered less statistically powerful, they may produce more
logical estimates if absolute heterogeneity exists. Furthermore,
random-effects models may overestimate the extent of error
variance, whereas fixed-effects models may underestimate it. Due to
the heterogeneity of the included studies, a fixed effect size
would be very implausible. Therefore, a standard random effect
model was applied. Considering that all of the included studies
were observational, the risk of bias was assessed using the
Newcastle-Ottawa quality assessment scale.
Results
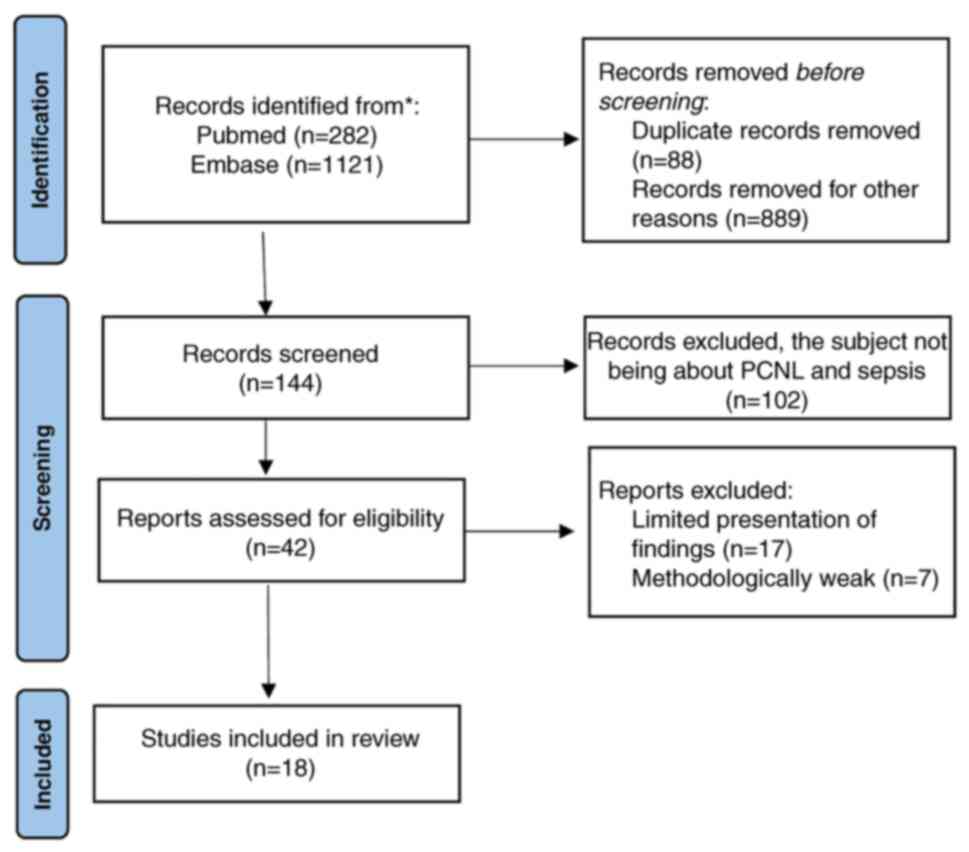
Of the 1,403 results of the search, only 18 articles
were selected. The flowchart of selection is shown in Fig. 1. The chosen studies, published
between 2014 and 2022, included a total of 7,507 patients on which
PCNL was performed. Details of the included studies are shown in
Table I.
 | Table ICharacteristics of included
studies. |
Table I
Characteristics of included
studies.
| Author, year | Factor studied | Number of
patients | Analyzed
outcome | (Refs.) |
|---|
| Amier et al,
2022 | B,D,E,F | 171 | Sepsis | (8) |
| Chen et al,
2019 | A,B,C,D,E,F | 802 | Sepsis | (9) |
| Chhetri et
al, 2018 | A,C,D,E,F | 97 | Sepsis | (10) |
| He et al,
2018 | A,B,C,D,E,G | 1,030 | SIRS | (11) |
| Koras et al,
2015 | A,D,E,F,G | 303 | SIRS | (12) |
| Kumar et al,
2021 | B,D,E,F | 320 | SIRS | (13) |
| Liu et al,
2020 | A,B,D,E,F | 303 | SIRS | (14) |
| Liu et al,
2021 | A,C,D,F,G | 241 | Sepsis | (15) |
| Lorenzo Soriano
et al, 2019 | A,B,D,E,F,G | 203 | SIRS | (16) |
| Rashid and
Fakhulddin, 2016 | A,D,E, | 60 | Sepsis | (17) |
| Tabei et al,
2016 | A,B,C,D,E,F,G | 370 | SIRS | (18) |
| Tang et al,
2021 | A,B,C,D,E,F,G | 758 | SIRS + Sepsis | (19) |
| Teh and Tham,
2021 | B,C,D,F | 425 | Sepsis | (20) |
| Wang et al,
2020 | A,D,E,F,G | 843 | Sepsis | (21) |
| Wei et al,
2015 | A,B,E,F,G | 411 | SIRS | (22) |
| Xu et al,
2022 | A,B,C,D,E,F,G | 220 | SIRS | (23) |
| Yang et al,
2017 | A,B,E | 164 | SIRS | (24) |
| Zhu et al,
2020 | A,B,C,D,E,F,G | 786 | Sepsis | (25) |
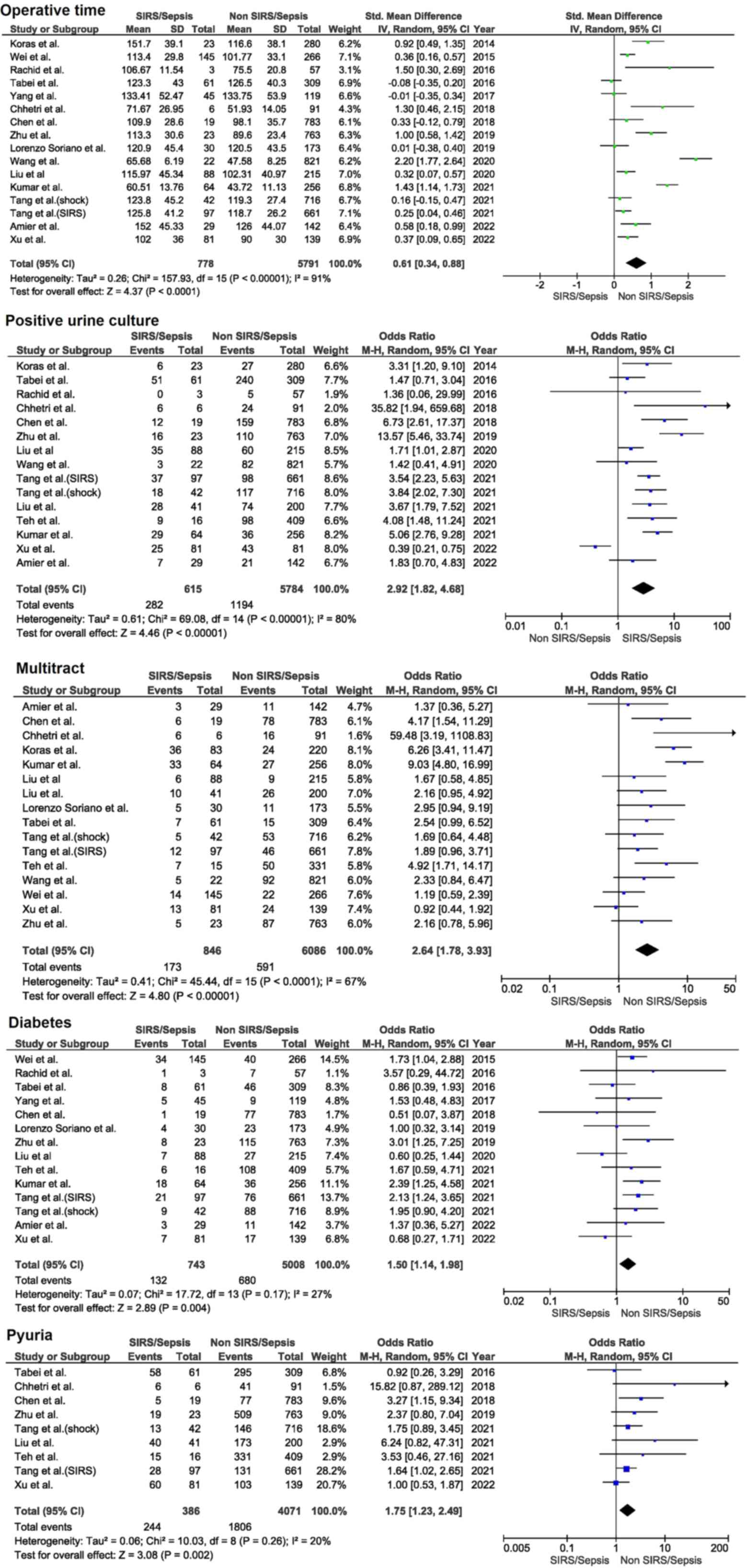
All authors applied antibiotic prophylaxis to all
patients and in some cases, the infection was treated
preoperatively in those with positive urine cultures. According to
the analysis of the present study, the operative time has been
significantly longer in patients who developed SIRS/sepsis
post-operatively (P=0.0001) with the highest heterogeneity
(I2=91%) compared with other factors. Patients with a
positive preoperative urine culture have a significantly higher
risk of developing SIRS/sepsis following PCNL (P=0.00001), OD=2.92
(1.82, 4.68) and there is also a high degree of heterogeneity
(I2=80%). Performing a multi-tract PCNL also increases
the incidence of postoperative SIRS/sepsis (P=0.00001), OD=2.64
(1.78, 3.93) and the heterogeneity was a little smaller
(I2=67%). Diabetes mellitus (P=0.004), OD=1.50 (1.14,
1.98), I2=27% and preoperative pyuria (P=0.002), OD=1.75
[1.23, 2.49], I2=20%, as shown in Fig. 2, were other factors that
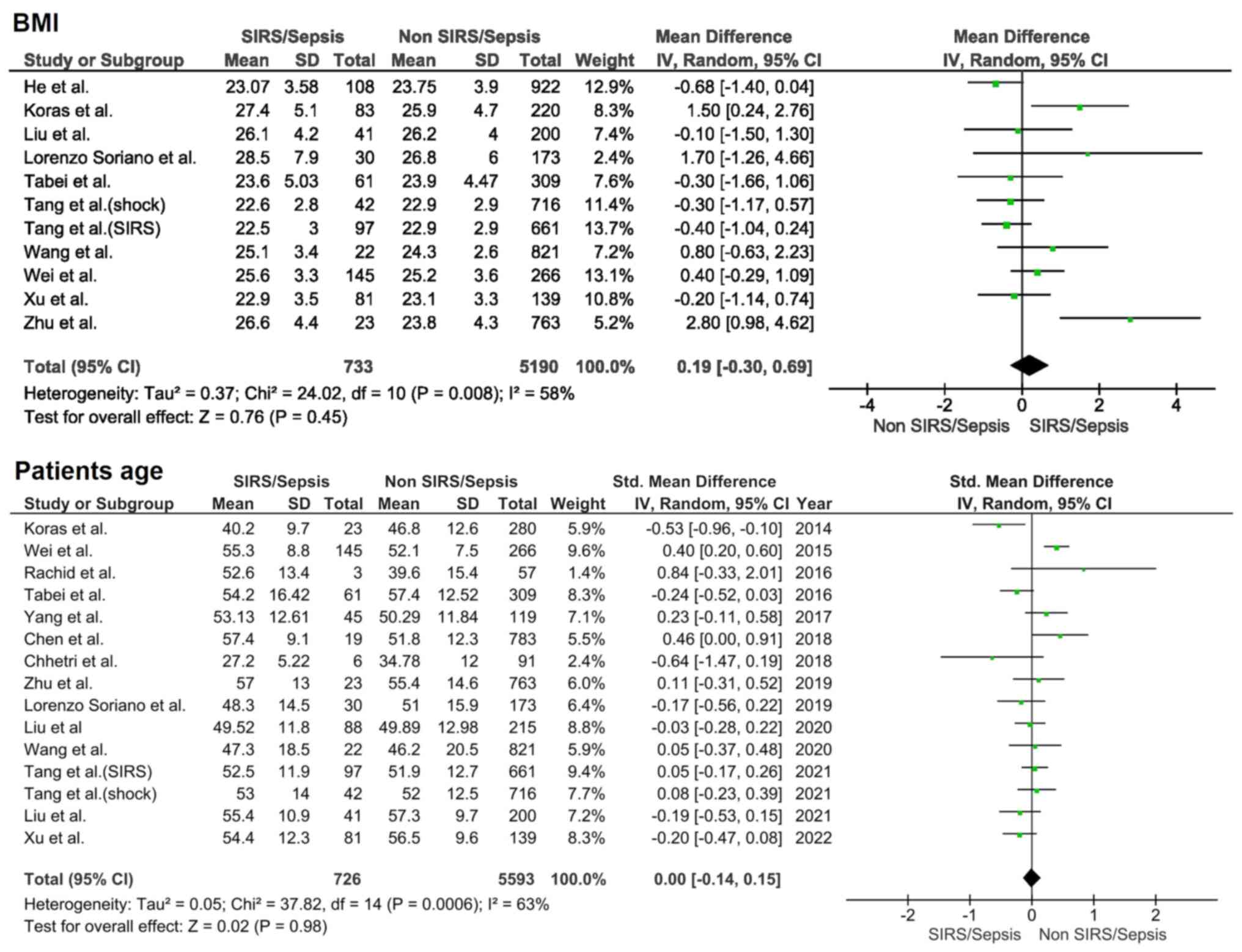
significantly influenced postoperative evolution. However, BMI and
patient's age did not influence the outcome; P=0.45,
I2=58% and P=0.98, I2=63%, as shown in
Fig. 3.
Non-randomized study
quality evaluation is an essential key part of a comprehensive
meta-analysis of non-randomized research. Poor research might have
a negative effect on the estimation of the overall effect. As the
present meta-analysis included non-randomized studies, the
Newcastle-Ottawa scale was used to assess the risk of bias. The
Newcastle-Ottawa scale consists of eight criteria divided into
three categories: Selection, comparability and outcome and
exposure. Several answer alternatives are offered for each issue. A
star system is employed to provide a semi-quantitative evaluation
of study quality, the only exception being the comparability item,
which permits the allocation of two stars, with the highest quality
papers receiving a maximum of one star for each item. The risk of
bias total score, assessed by the Newcastle-Ottawa scale, varied
between five and eight, the mean risk of bias being 6.16, resulting
in an average level of study quality, as seen in Table II.
 | Table IINewcastle-Ottawa scale of included
studies. |
Table II
Newcastle-Ottawa scale of included
studies.
| Author, year | Selection | Comparability | Exposure | Total score | (Refs.) |
|---|
| Amier et al,
2022 | **** | | *** | 7 | (8) |
| Chen et al,
2019 | *** | * | ** | 6 | (9) |
| Chhetri et
al, 2018 | ** | * | *** | 6 | (10) |
| He et al,
2018 | **** | | ** | 6 | (11) |
| Koras et al,
2015 | *** | * | * | 5 | (12) |
| Kumar et al,
2021 | *** | | ** | 5 | (13) |
| Liu et al,
2020 | *** | * | ** | 6 | (14) |
| Liu et al,
2021 | *** | * | * | 5 | (15) |
| Lorenzo Soriano
et al, 2019 | *** | * | *** | 7 | (16) |
| Rashid and
Fakhulddin, 2016 | **** | | ** | 6 | (17) |
| Tabei et al,
2016 | *** | * | ** | 6 | (18) |
| Tang et al,
2021 | *** | | *** | 6 | (19) |
| Teh and Tham,
2021 | *** | * | **** | 8 | (20) |
| Wang et al,
2020 | **** | * | ** | 7 | (21) |
| Wei et al,
2015 | *** | * | *** | 7 | (22) |
| Xu et al,
2022 | *** | | ** | 5 | (23) |
| Yang et al,
2017 | *** | * | *** | 7 | (24) |
| Zhu et al,
2020 | **** | | *** | 7 | (25) |
Discussions
PCNL is an increasingly widespread intervention that
increases the incidence of complications. According to Ghani et
al (26), sepsis following
PCNL rose from 1.2% in 1999 to 2.4% in 2009 in the United States.
Although not very common, postoperative urosepsis can be a
life-threatening complication of PCNL.
Aging brings changes that can influence patients'
immunity. A low-grade inflammatory condition characterizes elderly
patients. According to Aiello et al (27), this situation is responsible for
increased oxidative stressors and pro-inflammatory cytokines.
Furthermore, in these patients, a decrease in peripheral naive T
and B cells is found (28).
According to Bajaj et al (28), neutrophils are involved in the
immune response to bacterial aggression. They present an alteration
of neutrophil extracellular traps, one of the mechanisms involved
in the fight against pathogens. In addition, there is a reduction
in phagocytosis and a lowered intracellular killing activity
(28). In an animal model, an
impairment of the migration of neutrophils was observed, despite a
high level of chemokines (29).
Other authors have suggested that age-related alteration of
hormonal status could be responsible. According to Hao et al
(30), lower estrogen levels in
women predispose them to infections, adding other factors such as
poor perineal hygiene and menopause, making the incidence of
urosepsis double in women. Understanding the surgical risk of PCNL
in elderly patients is necessary, given the rise in life expectancy
and the number of elderly individuals undergoing surgery. The
results from the present study showed that, when conducted by a
skilled surgeon and with compensated comorbidities, PCNL can be
reasonably safe and efficiently performed on elderly patients.
A positive bladder urine culture before surgery will
lead to better antibiotic prophylaxis, although a complete
obstruction of the collecting system can lead to a sterile bladder
urine culture. For this reason, some authors suggested that the
renal pelvis urine culture could be more reliable for making
preoperative prophylaxis. In a cohort of 138 patients, Dogan et
al (31) noted that 10.1% of
patients with previous sterile bladder urine cultures had positive
renal pelvis urine cultures. Also, in a group of 122 patients,
Walton-Diaz et al (32),
bladder urine cultures were negative in all patients who developed
infectious complications following PCNL. Of these, 57.1% had
positive renal pelvis urine culture. For this reason, the authors
recommend pelvic urine culture, especially in high-risk patients,
because bladder urine culture is a poor predictor of the infectious
complications outcome. However, the analysis results of the present
study told a different story.
On the other hand, to get the renal pelvis urine
culture, placing a needle in the collecting system is necessary.
After obtaining the urine, the urologist can perform the
intervention simultaneously or place a drainage tube until the
result is available after ~48 h. The presence of a nephrostomy tube
before PCNL is a debatable factor. In a cohort of 217 patients,
Aghdas et al (33) noticed
a higher incidence of postoperative fever in those who had a
nephrostomy placed preoperatively. However, according to Benson
et al (34), it has a
protective role. There is no clear explanation for this situation.
Although the tube will drain the infected urine, it would act as a
foreign body, and the fast colonization of any urinary stent is
well known. According to Verma et al (35), 43% of bladder catheters will be
colonized after only five days and 20% will be with biofilm-forming
bacteria.
A complex relationship exists between elevated BMI,
kidney stones and urinary tract infections (UTIs). We are
witnessing a concomitant increase in the prevalence of kidney stone
disease and obesity. According to Poore et al (36), obesity in adults increased by 27.5%
from 1980 to 2013. In women with an elevated BMI, there is a
1.30-fold increased risk for kidney stone development compared with
those with a normal BMI. The explanation may be that obesity is
associated with metabolic changes that favor stone formation.
According to Taylor et al (37), urinary pH is more acidic in
patients with greater BMI and urinary oxalate, sodium, uric acid
and phosphate concentrations are higher. Similar findings were also
reported by Ekeruo et al (38); the authors noticed that
hyperoxaluria, hypercalciuria and hyperuricosuria are more commonly
found in obese stone formers compared with a non-obese cohort.
Although the present study analyzed the impact of BMI on infectious
complications following PCNL, according to Poore et al
(36), it seems that visceral
obesity is the more predictive of kidney stone risk. However, it is
more difficult to quantify because it requires imaging studies. In
the present study, the BMI did not influence the infectious
outcomes of PCNL, although some authors link obesity to a higher
chance of developing UTI. In a cohort of 95,598 subjects, Semins
et al (39) noticed that
males with a BMI between 30.0-34.9 have a higher chance of
developing UTI compared with patients with a BMI>50 (OR 1.59 vs.
2.35). A higher BMI does not influence PCNL outcome, not from the
infection's point of view but overall. According to Ortiz et
al (40), there is no
significant difference in the stone-free rate, postoperative
complication incidence, hemoglobin loss, or hospital stay.
Diabetes mellitus, obesity and arterial hypertension
are essential elements of metabolic syndrome. Urinary abnormalities
indicate a definite association between metabolic syndrome and
kidney stones. According to Domingos et al (41), these patients have excessively
acidic urine, high urinary calcium and oxalate levels and low
urinary citrate. As in the case of patients with elevated BMI,
there is a link between diabetes and UTI. According to Chiu et
al (42), a UTI in a diabetic
patient is 10 times more likely to progress to pyelonephritis.
According to Murtha et al (43), one explanation is that the immunity
to bacteria in the urinary tract is insulin-dependent. The authors
proved in an animal model that insulin resistance leads to a
suppression of urinary antimicrobial peptides suggesting that
urinary sugar is not the essential element behind UTIs in these
patients. In addition, elevated blood sugar influences resistance
to UTIs. In diabetic patients, some immune alterations have been
observed, such as an elevation in CD4+CD28null T-lymphocytes count,
lower levels of serum complement factor 4 concentration and plasma
zinc levels and also significantly lower PMNs chemotaxis (44,45).
The results of the present study show that diabetes is a
predisposing factor for postoperative infections. Considering that
PCNL is an elective operation, it is assuming that the patient's
blood sugar was within normal limits at the time of the
intervention. However, an unbalanced history of diabetes may
contribute to the unfavorable evolution. Future studies would help
identify the relationship between hemoglobin A1c and SIRS/sepsis
following PCNL.
In patients with staghorn stones, surgical
management can be complex. Performing multiple tracts, PCNL can
increase the rate of complications and the period of
hospitalization. In a cohort of 27 patients where multiple tract
PCNL was performed, Liang et al (46) obtained a stone-free rate within
three sessions in 88.9% of cases. The authors did not report
significant blood loss, while postoperative fever was encountered
in only 22.22% of cases. A group of 65 patients evaluated by Rashid
et al (47), who underwent
multiple tract PCNL, had a significant decrease in hemoglobin
level, while serum creatinine remained relatively unchanged. In
their cohort, 11% had a postoperative fever, while only 3%
presented an infection that required additional antibiotics. In a
much larger cohort of 773 patients with staghorn calculi in which
PCNL was performed, of which 514 with multiple tracts, Desai et
al (48) reported
postoperative fever in up to 28.2% of patients.
Given the risk of infectious complications, a
logical strategy would be to use antibiotic prophylaxis. However,
it remains a debatable topic related to the categories of patients
who would benefit the most and the treatment regimen, a single
preoperative dose or treatment for several days. In a meta-analysis
by Yu et al (1), which
included 13 studies with a total of 1,549 patients, the results
indicated that for those receiving prophylactic treatment for a few
days compared with those receiving a single dose, the symptoms of
sepsis were significantly lower as well as positive cultures in the
renal pelvis. Moreover, according to Xu et al (23), optimal antibiotic prophylaxis in
those with preoperative positive urine cultures should last at
least seven days. Schnabel et al (49) compared 98 patients who received
antibiotics one day preoperatively with 76 patients who did not
receive prophylaxis. The authors found no significant differences
in fever, grade 1-3 complications, or hospitalization. The authors
considered that antibiotic prophylaxis might not be necessary in
selected cases, such as those with negative urine culture,
non-staghorn stones and no history of urinary tract infections.
Some authors have tried to evaluate the role of the urine dipstick
test before the PCNL. In a group of 806 patients, Xu et al
(50) reported that positive urine
dipstick infection prior to surgery strongly predicted SIRS.
Paradoxically, extensive preoperative antibiotic use was linked to
a greater risk of SIRS.
According to European Association of Urology
recommendations, 2022 edition, the probability of infection during
PCNL is high and antibiotic prophylaxis has been demonstrated to
minimize the risk for infectious complications significantly with a
single dosage being adequate (51). Antibiotic prophylaxis should be
given even with a negative urine culture, according to American
Urological Association Guidelines, which are regarded as a clinical
principle (52). In this part, the
American Urological Association panel makes the case that there is
insufficient evidence to suggest giving patients with a negative
urine culture one week of preventive antibiotics. In a recent
survey that included over 3,000 Chinese urologists, Zhang et
al (53) reported that
antibiotic prophylaxis for 1-3 days before surgery was most often
used regardless of whether the urine culture was positive or
negative (54.5 vs. 65.5%). Cephalosporins are the most used
antibiotic type, followed by quinolones. Considering that urine
cultures are not specific for the colonization status, He et
al (54) compared two types of
antibiotic regimens with the presence of white blood cells (WBC)
and nitrites in urine. The authors showed that one 1.5 g dose of
cefuroxime before PCNL compared with 3-day treatment statistically
lowered the incidence of SIRS in patients with positive nitrites in
urine but did not influence the outcome in patients with absent
nitrites in urine. In the cohort studied by Xu et al
(23), the urine culture result
was unavailable before the procedure in some patients. In these
cases, they received an empirical antibiotic prophylaxis 30 before
the surgery and postoperatively, the antibiotic therapy was
adjusted after obtaining the result. The authors evaluated the
effects of antibiotic prophylaxis schemes. Although a more extended
antibiotic prophylaxis was significantly associated with a better
outcome, the administration of sensitive antibiotics did not prove
a significant advantage over non-sensitive antibiotics.
From the data of the present study, between
2017-2021, of the 463 cases in which PCNL was performed, 5.18%
(n=24) developed postoperative sepsis/SIRS. Of these, 54.2% (n=13)
were men and 45.8% (n=11) were women. The stone-free rate was 75%
and the overall stone-free rate was 69.11%. The bladder
preoperative urine culture was positive in 58.33% (n=14) of
patients compared with 25.20% in the non-sepsis group. Also, the
preoperative presence of urinary stents was noted more frequently
in the sepsis/SIRS group (62.5% vs. 17.71%). The majority (93.33%)
had JJ ureteral stents. In all cases, developing sepsis/SIRS
symptoms led to a change in the postoperative antibiotic regimen
(55).
The present meta-analysis has some limitations:
First, the studies are somewhat heterogenous; the authors came from
different continents, the number of patients varied from 60 to
1,030 and renal pelvic urine culture was not available in all
cases. Also, the dilatation technique, balloon compared with
telescopic/serial dilation, was not known in all studies. Another
drawback of the meta-analysis is the need to evaluate the type of
kidney stones according to the various scoring systems. Only one of
the included studies reported that a higher STONE (Stone size,
Tract length, Obstruction, Number of involved calices and Essence
or stone density) score correlates significantly with sepsis/SIRS
(19). From the present study
authors' experience with the Guy stone score, it was also found
that patients with the highest grade (IV) have significantly more
preoperative positive urine culture and complications according to
the Clavien scale and the lowest stone-free rate (56).
Despite this, the present meta-analysis has some
strong points. All patients in the included studies underwent the
same type of intervention. The outcomes are well defined, SIRS
respectively sepsis, or quantified such as WBC, preoperative urine
culture, or BMI. Thus, some elements are easy to compare, such as
the operative time, which depends on several factors. According to
Akman et al (56), some of
these factors are the previous presence of hydronephrosis, stone
characteristics and surgeon experience, which could not be
evaluated in the present analysis. Further studies should evaluate
supplemental sepsis indicators such as C-reactive protein,
hemoglobin A1c or procalcitonin. Also, the type of PCNL technique
(standard or miniPCNL) could be an influencing factor considering
as, according to Jiao et al (57), there is no difference regarding
postoperative fever between standard compared with miniPCNL.
However, the operative time was significantly shorter in patients
in which minPCNL and, according to the data of the present
analysis, a longer operative time favors the development of
SIRS/sepsis.
The present analysis showed that diabetes mellitus,
multitract PCNL, pyuria, operative time and positive urine culture
are factors that, if not controlled, favor the appearance of SIRS
or urosepsis. In some high-risk patients, such as those with
diabetes, a history of urinary tract infections, or positive urine
cultures, antibiotic prophylaxis should be mandatory and performed
for at least one week before surgery.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Data sharing is not applicable to this article, as
no data sets were generated or analyzed during the current
study.
Authors' contributions
DP and CP were responsible for conceiving the study
and DP was responsible for the methodology, formal analysis and
software. Validation was performed by DP, CP and SG and
investigation by GR and SG. Data curation was by SG, GR and VJ. DP,
GR and SG wrote the original draft of the manuscript, which was
reviewed and edited by VJ and CP. CP and VJ were responsible for
visualization and supervision. Data authentication is not
applicable. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yu J, Guo B, Yu J, Chen T, Han X, Niu Q,
Xu S, Guo Z, Shi Q, Peng X, et al: Antibiotic prophylaxis in
perioperative period of percutaneous nephrolithotomy: A systematic
review and meta-analysis of comparative studies. World J Urol.
38:1685–1700. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jiang Y and Zhang J, Kang N, Niu Y, Li Z,
Yu C and Zhang J: Current Trends in percutaneous nephrolithotomy in
China: A spot survey. Risk Manag Health Policy. 14:2507–2515.
2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Türk C, Petřík A, Sarica K, Seitz C,
Skolarikos A, Straub M and Knoll T: EAU guidelines on
interventional treatment for urolithiasis. Eur Urol. 69:475–482.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sharma K, Sankhwar SN, Goel A, Singh V,
Sharma P and Garg Y: Factors predicting infectious complications
following percutaneous nephrolithotomy. Urol Ann. 8:434–438.
2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Michel MS, Trojan L and Rassweiler JJ:
Complications in percutaneous nephrolithotomy. Eur Urol.
51:899–906. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Yang Z, Lin D, Hong Y, Hu M, Cai W, Pan H,
Li Q, Lin J and Ye L: The effect of preoperative urine culture and
bacterial species on infection after percutaneous nephrolithotomy
for patients with upper urinary tract stones. Sci Rep.
12(4833)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Amier Y, Zhang Y, Zhang J, Yao W, Wang S,
Wei C and Yu X: Analysis of preoperative risk factors for
postoperative urosepsis after mini-percutaneous nephrolithotomy in
patients with large kidney stones. J Endourol. 36:292–297.
2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chen D, Jiang C, Liang X, Zhong F, Huang
J, Lin Y, Zhao Z, Duan X, Zeng G and Wu W: Early and rapid
prediction of postoperative infections following percutaneous
nephrolithotomy in patients with complex kidney stones. BJU Int.
123:1041–1047. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chhetri RK, Baral S and Thapa N:
Prediction of infectious complications after percutaneous
nephrolithotomy. J Soc Surg Nepal. 21:12–18. 2018.
|
|
11
|
He Z, Tang F, Lei H, Chen Y and Zeng G:
Risk factors for systemic inflammatory response syndrome after
percutaneous nephrolithotomy. Prog Urol. 28:582–587.
2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Koras O, Bozkurt IH, Yonguc T, Degirmenci
T, Arslan B, Gunlusoy B, Aydogdu O and Minareci S: Risk factors for
postoperative infectious complications following percutaneous
nephrolithotomy: A prospective clinical study. Urolithiasis.
43:55–60. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kumar GC, Devraj R, Sagar V, Chandraiah R,
Prasad D and Ch R: Factors determining postoperative infectious
complications of percutaneous nephrolithotomy: Experience from a
single center. Int J Health Clin Res. 4:127–130. 2021.
|
|
14
|
Liu J, Zhou C, Gao W, Huang H, Jiang X and
Zhang D: Does preoperative urine culture still play a role in
predicting post-PCNL SIRS? A retrospective cohort study.
Urolithiasis. 48:251–256. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Liu J, Yang Q, Lan J, Hong Y, Huang X and
Yang B: Risk factors and prediction model of urosepsis in patients
with diabetes after percutaneous nephrolithotomy. BMC Urol.
21(74)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lorenzo Soriano L, Ordaz Jurado DG, Pérez
Ardavín J, Budía Alba A, Bahílo Mateu P, Trassierra Villa M and
López Acón D: Predictive factors of infectious complications in the
postoperative of percutaneous nephrolithotomy. Actas Urol Esp (Engl
Ed). 43:131–136. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Rashid AO and Fakhulddin SS: Risk factors
for fever and sepsis after percutaneous nephrolithotomy. Asian J
Urol. 3:82–87. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tabei T, Ito H, Usui K, Kuroda S, Kawahara
T, Terao H, Fujikawa A, Makiyama K, Yao M and Matsuzaki J: Risk
factors of systemic inflammation response syndrome after endoscopic
combined intrarenal surgery in the modified Valdivia position. Int
J Urol. 23:687–692. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tang Y, Zhang C, Mo C, Gui C, Luo J and Wu
R: Predictive model for systemic infection after percutaneous
nephrolithotomy and related factors analysis. Front Surg.
8(696463)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Teh KY and Tham TM: Predictors of
post-percutaneous nephrolithotomy sepsis: The Northern Malaysian
experience. Urol Ann. 13:156–162. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wang S, Yuan P, Peng E, Xia D, Xu H, Wang
S, Ye Z and Chen Z: Risk factors for urosepsis after minimally
invasive percutaneous nephrolithotomy in patients with preoperative
urinary tract infection. Biomed Res Int.
2020(1354672)2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wei W, Leng J, Shao H and Wang W:
Diabetes, a risk factor for both infectious and major complications
after percutaneous nephrolithotomy. Int J Clin Exp Med.
8:16620–16626. 2015.PubMed/NCBI
|
|
23
|
Xu P, Zhang S, Zhang Y, Zeng T, Chen D and
Wu W, Tiselius HG, Li S, Huang J, Zeng G and Wu W: Preoperative
antibiotic therapy exceeding 7 days can minimize infectious
complications after percutaneous nephrolithotomy in patients with
positive urine culture. World J Urol. 40:193–199. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Yang T, Liu S, Hu J, Wang L and Jiang H:
The evaluation of risk factors for postoperative infectious
complications after percutaneous nephrolithotomy. Biomed Res Int.
2017(4832051)2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhu Z, Cui Y, Zeng H, Li Y, Zeng F, Li Y,
Chen Z and Hequn C: The evaluation of early predictive factors for
urosepsis in patients with negative preoperative urine culture
following mini-percutaneous nephrolithotomy. World J Urol.
38:2629–2636. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ghani KR, Sammon JD, Bhojani N,
Karakiewicz PI, Sun M, Sukumar S, Littleton R, Peabody JO, Menon M
and Trinh QD: Trends in percutaneous nephrolithotomy use and
outcomes in the United States. J Urol. 190:558–564. 2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Aiello A, Farzaneh F, Candore G, Caruso C,
Davinelli S, Gambino CM, Ligotti ME, Zareian N and Accardi G:
Immunosenescence and its hallmarks: how to oppose aging
strategically? A review of potential options for therapeutic
intervention. Front Immunol. 10(2247)2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Bajaj V, Gadi N, Spihlman AP, Wu SC, Choi
CH and Moulton VR: Aging, immunity, and COVID-19: How age
influences the host immune response to coronavirus infections?
Front Physiol. 11(571416)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zhou YY and Sun BW: Recent advances in
neutrophil chemotaxis abnormalities during sepsis. Chin J
Traumatol. 25:317–324. 2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Hao Z, Wang J, Wang Q, Luan G and Qian B:
Preoperative risk factors associated with urosepsis following
percutaneous nephrolithotomy: A meta-analys. Int J Clin Exp Med.
12:9616–9628. 2019.
|
|
31
|
Dogan HS, Guliyev F, Cetinkaya YS,
Sofikerim M, Ozden E and Sahin A: Importance of microbiological
evaluation in management of infectious complications following
percutaneous nephrolithotomy. Int Urol Nephrol. 39:737–742.
2007.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Walton-Diaz A, Vinay JI, Barahona J, Daels
P, González M, Hidalgo JP, Palma C, Díaz P, Domenech A, Valenzuela
R and Marchant F: Concordance of renal stone culture: PMUC, RPUC,
RSC and post-PCNL sepsis-a non-randomized prospective observation
cohort study. Int Urol Nephrol. 49:31–35. 2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Aghdas FS, Akhavizadegan H, Aryanpoor A,
Inanloo H and Karbakhsh M: Fever after percutaneous
nephrolithotomy: Contributing factors. Surg Infect (Larchmt).
7:367–371. 2006.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Benson AD, Juliano TM and Miller NL:
Infectious outcomes of nephrostomy drainage before percutaneous
nephrolithotomy compared to concurrent access. J Urol. 192:770–774.
2014.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Verma A, Bhani D, Tomar V, Bachhiwal R and
Yadav S: Differences in bacterial colonization and biofilm
formation property of uropathogens between the two most commonly
used indwelling urinary catheters. J Clin Diagn Res. 10:PC01–PC03.
2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Poore W, Boyd CJ, Singh NP, Wood K, Gower
B and Assimos DG: Obesity and its impact on kidney stone formation.
Rev Urol. 22:17–23. 2020.PubMed/NCBI
|
|
37
|
Taylor EN, Stampfer MJ and Curhan GC:
Obesity, weight gain, and the risk of kidney stones. JAMA.
293:455–462. 2005.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Ekeruo WO, Tan YH, Young MD, Dahm P,
Maloney ME, Mathias BJ, Albala DM and Preminger GM: Metabolic risk
factors and the impact of medical therapy on the management of
nephrolithiasis in obese patients. J Urol. 172:159–163.
2004.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Semins MJ, Shore AD, Makary MA, Weiner J
and Matlaga BR: The impact of obesity on urinary tract infection
risk. Urology. 79:266–269. 2012.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Torrecilla Ortiz C, Meza Martínez AI,
Vicens Morton AJ, Vila Reyes H, Colom Feixas S, Suarez Novo JF and
Franco Miranda E: Obesity in percutaneous nephrolithotomy. Is body
mass index really important? Urology. 84:538–543. 2014.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Domingos F and Serra A: Metabolic
syndrome: A multifaceted risk factor for kidney stones. Scand J
Urol. 48:414–419. 2014.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Chiu PF, Huang CH, Liou HH, Wu CL, Wang SC
and Chang CC: Long-term renal outcomes of episodic urinary tract
infection in diabetic patients. J Diabetes Complications. 27:41–43.
2013.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Murtha MJ, Eichler T, Bender K, Metheny J,
Li B, Schwaderer AL, Mosquera C, James C, Schwartz L, Becknell B
and Spencer JD: Insulin receptor signaling regulates renal
collecting duct and intercalated cell antibacterial defenses. J
Clin Invest. 128:5634–5646. 2018.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Giubilato S, Liuzzo G, Brugaletta S,
Pitocco D, Graziani F, Smaldone C, Montone RA, Pazzano V, Pedicino
D, Biasucci LM, et al: Expansion of CD4+CD28null T-lymphocytes in
diabetic patients: exploring new pathogenetic mechanisms of
increased cardiovascular risk in diabetes mellitus. Eur Heart J.
32:1214–1226. 2011.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Geerlings SE and Hoepelman AI: Immune
dysfunction in patients with diabetes mellitus (DM). FEMS Immunol
Med Microbiol. 26:259–265. 1999.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Liang T, Zhao C, Wu G, Tang B, Luo X, Lu
S, Dong Y and Yang H: Multi-tract percutaneous nephrolithotomy
combined with EMS lithotripsy for bilateral complex renal stones:
Our experience. BMC Urol. 17(15)2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Rashid AO, Mahmood SN, Amin AK, Bapir R
and Buchholz N: Multitract percutaneous nephrolithotomy in the
management of staghorn stones. Afr J Urol. 26(74)2020.
|
|
48
|
Desai M, Jain P, Ganpule A, Sabnis R,
Patel S and Shrivastav P: Developments in technique and technology:
The effect on the results of percutaneous nephrolithotomy for
staghorn calculi. BJU Int. 104:542–548. 2009.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Schnabel MJ, Rosenhammer B, Steckermeier
M, Fritsche HM, Burger M and Spachmann PJ: Miniaturized
percutaneous nephrolithotomy without antibiotic prophylaxis: A
single institution experience. Int Urol Nephrol. 53:1551–1556.
2021.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Xu P, Zhang S, Zhang Y, Zeng T, Chen D and
Wu W, Tiselius HG, Li S, Huang J, Zeng G and Wu W: Enhanced
antibiotic treatment based on positive urine dipstick infection
test before percutaneous nephrolithotomy did not prevent
postoperative infection in patients with negative urine culture. J
Endourol. 35:1743–1749. 2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
European Association of Urology (EAU):
Guideline on urolithiasis. EAU, Arnhem, 2022. https://uroweb.org/guidelines/urolithiasis. Accessed
December 20, 2022.
|
|
52
|
Pearle MS, Goldfarb DS, Assimos DG, Curhan
G, Denu-Ciocca CJ, Matlaga BR, Monga M, Penniston KL, Preminger GM,
Turk TM, et al: Medical management of kidney stones: AUA guideline.
J Urol. 192:316–324. 2014.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Zhang S, Li G, Qiao L, Lai D, He Z, An L,
Xu P, Tiselius HG, Zeng G, Zheng J and Wu W: The antibiotic
strategies during percutaneous nephrolithotomy in China revealed
the gap between the reality and the urological guidelines. BMC
Urol. 22(136)2022.PubMed/NCBI View Article : Google Scholar
|
|
54
|
He C, Chen H, Li Y, Zeng F, Cui Y and Chen
Z: Antibiotic administration for negative midstream urine culture
patients before percutaneous nephrolithotomy. Urolithiasis.
49:505–512. 2021.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Puia D, Radavoi GD, Proca TM, Puia A,
Jinga V and Pricop C: Urinary tract infections in complicated
kidney stones: Can they be correlated with Guy's stone score? J Pak
Med Assoc. 72:1721–1725. 2022.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Akman T, Binbay M, Akcay M, Tekinarslan E,
Kezer C, Ozgor F, Seyrek M and Muslumanoglu AY: Variables that
influence operative time during percutaneous nephrolithotomy: An
analysis of 1897 cases. J Endourol. 25:1269–1273. 2011.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Jiao B, Luo Z, Huang T, Zhang G and Yu J:
A systematic review and meta-analysis of minimally invasive vs
standard percutaneous nephrolithotomy in the surgical management of
renal stones. Exp Ther Med. 21(213)2021.PubMed/NCBI View Article : Google Scholar
|