Introduction
Nocardiosis is a rare but severe suppurative
infection, most commonly seen in susceptible patients with
underlying chronic diseases, such as those undergoing tumor
chemotherapy, those suffering from alcoholism, or those with
endogenous or iatrogenic immunosuppression (1,2). It
has been reported that patients with anti-neutrophil cytoplasmic
antibody (ANCA)-associated vasculitis become infected with
Nocardia after immunosuppressive therapy, with high
mortality rates due to ineffective treatment (3-5).
For such patients, it was necessary to control the target organ
damage caused by the primary vasculitis, as well as to actively
treat the opportunistic nocardial abscesses, which makes the
clinical treatment very challenging. In the present study, the case
of an elderly patient presenting with typical multiple large
nocardial abscesses with ANCA-associated vasculitis and renal
insufficiency, who was treated with glucocorticoid and
cyclophosphamide, is reported. After medical and surgical therapy,
the abscesses were completely absorbed, the patient became negative
for ANCA and renal function was completely recovered after 1 year
of follow-up. In addition, the present study reviews the literature
with regard to the age, clinical characteristics, specific
treatment options and treatment outcomes of patients with this rare
infection caused by nephropathy and immunosuppressive therapy, in
order to improve the outcome of this life-threatening
infection.
Case report
A 69-year-old male patient was admitted to the
Department of Geriatrics of the Affiliated Hospital of Nantong
University (Nantong, China) in September 2020 due to recurrent
lower abdominal pain for 1 month. On admission, the patient
presented with persistent dull pain in the lower abdomen
accompanied by poor appetite and fatigue, without any other
complaints of discomfort. The patient was previously healthy.
Physical examination showed that temperature, pulse, respiration
and blood pressure were normal. Emaciation and anemia were also
observed. The breath sounds from both lungs were coarse, but no
rales were detected. The whole abdomen was soft, with mild
tenderness around the umbilicus and lower abdomen, without rebound
pain and muscle tension, and with mild edema in the bilateral lower
extremities. Cardiovascular and nervous systems were normal. Blood
test results after admission showed the following results:
Hemoglobin, 77 g/l (normal range, 120-160 g/l); serum albumin, 28
g/l (normal range, 35-55 g/l); serum creatinine, 242 µmol/l (normal
range, 64-104 µmol/l); erythrocyte sedimentation rate, 108 mm/h
(normal range, 0-10 mm/h); C-reactive protein (CRP), 105 mg/l
(normal range, 0-8 mg/l); and 24-h urine protein, 1.38 g/day
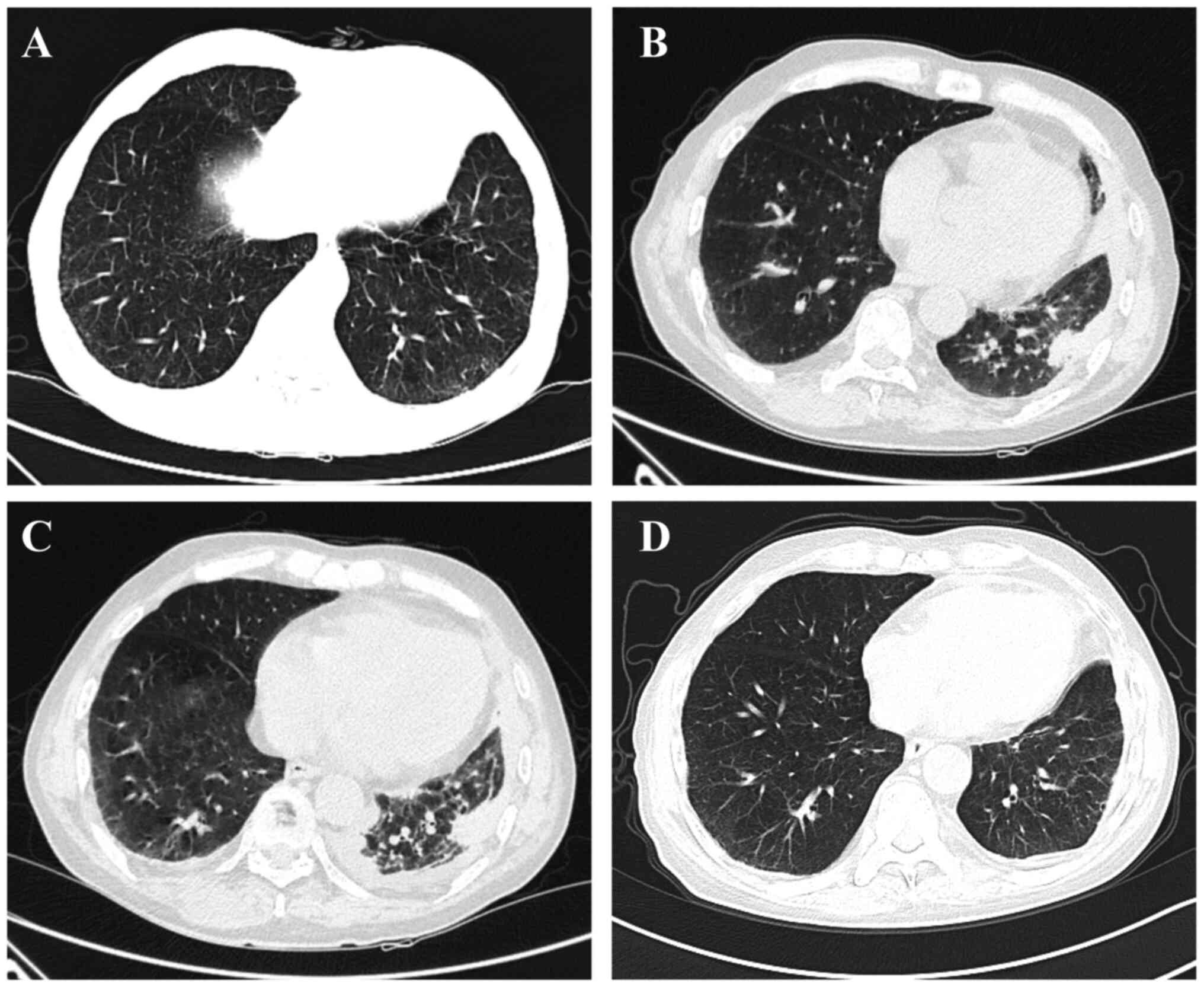
(normal range, 0-0.15 g/day). Chest CT showed interstitial
inflammation in the bilateral inferior lungs (Fig. 1A). The titer of
myeloperoxidase-anti-neutrophil cytoplasmic antibody (MPO-ANCA) was
1,573 AU/ml (normal range, <100 AU/ml) using the AtheNA
Multi-Lyte® Autoimmune Vasculitis Plus Test System (cat.
no. 22020054; Zeus Scientific, Inc.). Thereafter, the patient was
transferred to the Department of Nephrology. The patient refused a
renal biopsy, and the diagnosis was ANCA-associated vasculitis,
renal insufficiency, interstitial pneumonia and moderate anemia.
After 5 days of an intravenous infusion of 40 mg
methylprednisolone, the treatment was changed to oral prednisone
acetate (15 mg three times a day), and 0.6 g cyclophosphamide (CTX)
was intravenously administered once. The patient was discharged at
16 days post-admission, and instead was prescribed oral prednisone
and monthly intravenous CTX medication, and the dose of
corticosteroid was gradually tapered. After 6 months of treatment,
the dosage of prednisone acetate was tapered to 25 mg once a day,
and the total CTX dosage in 7 months was 4.2 g.
In April 2021, the patient developed swelling and
pain in the left hip. After 6 days, the patient was readmitted to
the Affiliated Hospital of Nantong University. The vital signs of
the patient were stable and normal, but there was a 15x10-cm mass
on the left hip. The local skin temperature was increased, with
tenderness and swelling, but there was no obvious redness. There
was moderate edema in the bilateral lower extremities. A routine
blood test showed the following results: White blood cell count,
8.0x109/l (4.0-10.0x109/l); neutrophils,
79.8% (40-75%); hemoglobin, 82 g/l; urine protein, negative; plasma
albumin, 28.8 g/l; serum creatinine, 76 µmol/l; MPO, negative; and
serum hypersensitive CRP, 27.5 mg/l. Serum markers of HIV, syphilis
and hepatitis were negative. The tuberculin test was also negative.
A chest CT scan revealed new left encapsulated pleural effusion and
new anterior mediastinal nodules (Fig.
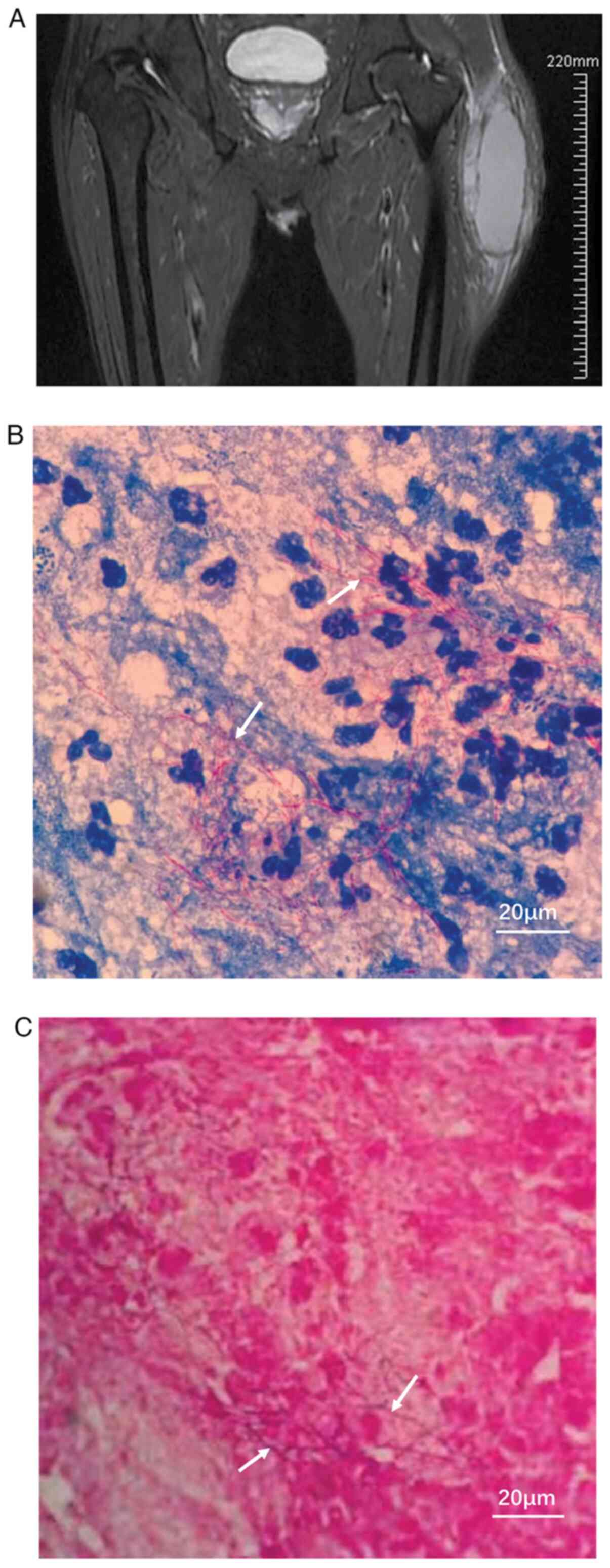
1B). Magnetic resonance imaging (MRI) of the left femur
indicated encapsulated fluid signals in the proximal subcutaneous
part of the left thigh. The mass measured 132x77x44 mm, with
internal separation, peripheral soft-tissue swelling and edema, and
was considered to be an infectious lesion accompanied by abscess
formation (Fig. 2A). After
admission, moxifloxacin sodium chloride (0.4 g/day) was
intravenously administered for anti-infection purposes, while the
dose of oral prednisone acetate was reduced to 10 mg per day and
CTX treatment was discontinued. The patient initially refused
surgery and asked for conservative treatment. Therefore, under the
guidance of ultrasound, 30 ml was extracted from the subcutaneous
abscess at the lateral edge of the left thigh, and the puncture pus
was collected for bacterial culture and drug sensitivity testing. A
metronidazole sodium chloride injection (5 mg/ml) was applied
locally for repeated washing. In addition, 10 g of human albumin
was intravenously provided on a daily basis as supportive care.
After 5 days of treatment, the mass of the left hip did not
improve, the discomfort worsened and the patient agreed to surgical
intervention. A local subcutaneous abscess incision and aspiration
were performed after orthopedic consultation. During the operation,
subcutaneous tissue necrosis and a large amount of pus were
observed and removed. Furthermore, closed negative pressure
drainage was performed on the wound surface after surgery. Weak
acid-fast staining (Fig. 2B) and
Gram-positive staining (Fig. 2C)
(performed at room temperature for ~20 min) of the aspirated pus
showed filamentous Nocardia using a light microscope
(Olympus Corporation). Accordingly, the antibiotic was adjusted to
linezolid glucose injection, 0.6 g by intravenous drip, twice a
day. After 12 days, a repeated chest CT scan revealed a small
amount of bilateral pleural effusion, and the left region was
encapsulated slightly more than before. The anterior mediastinal
nodules were similar to 12 days ago (Fig. 1C). The adjustment of the antibiotic
to linezolid glucose injection was not observed to be associated
with increased pleural effusion of polyserositis. Based on these
results, ultrasound-guided puncture and drainage was performed in
the left pleural cavity, which extracted 15 ml of pus, and then a
metronidazole sodium chloride injection (5 mg/ml) was applied
locally for repeated washing. At 2 days after the drainage
procedure (April 2021), the patient insisted on being discharged
from the hospital due to financial reasons. After discharge, the
patient was provided with linezolid tablets (0.6 g orally, every 12
h) and compound trimethoprim-sulfamethoxazole (TMP-SMX) tablets
(0.48 g orally, twice a day) for continuous anti-bacterial
treatment, as well as prednisone (10 mg daily) orally for
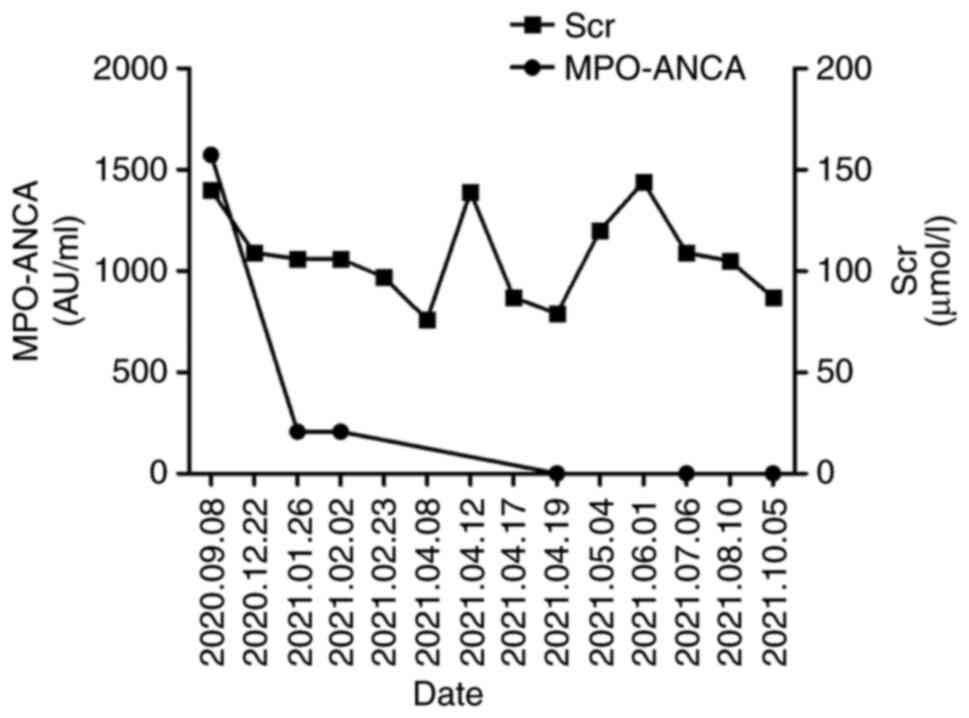
maintenance therapy. Subsequent outpatient review of renal function
showed a creatinine level of 120 µmol/l, while there was a negative
result for MPO and a repeated chest CT scan indicated that the lung
abscess had completely disappeared 11 days after discharge
(Fig. 1D). No MRI was performed
after discharge due to financial reasons. Thereafter, all
antibiotics were discontinued, and prednisone was discontinued
after 6 months. The condition of the patient was stable during the
1 year of follow-up after discharge, with MPO results remaining
negative and renal function still normal (serum creatinine, 87
µmol/l) (Fig. 3). The patient will
have a good prognosis and will be followed up for the next 2
years.
Discussion
Nocardia is an aerobic gram-positive
bacterium, belonging to Mycobacteriaceae family, which can infect
humans through skin trauma or respiratory inhalation (6). In different types of immunosuppressed
populations, the overall incidence of Nocardiosis has been reported
as ≤3.6%, while the associated mortality is as high as 77%
(7-9).
To the best of our knowledge, very few cases of Nocardia
infection in elderly patients with ANCA-associated vasculitis have
been reported as successfully treated in a short period of time
(3-5).
The most common site of Nocardia infection is the lung,
followed by the skin and the brain (10). Nocardia infection is usually
seen in susceptible patients with chronic diseases, or endogenous
or iatrogenic immunosuppression (11). In a review of the literature, 15
published cases of Nocardia infection worldwide from the
last two decades in patients with underlying renal diseases, such
as systemic lupus erythematosus, membranous proliferative
glomerulonephritis, nephrotic syndrome or kidney transplantation,
were found (3-5,12-23;
Table I). Among them, 3 cases were
ANCA-associated vasculitis, and only 1 case was reported in China,
but 1 case in Japan was successfully treated. The current study is
the first case of successful treatment of Nocardia secondary
infection with linezolid in an elderly patient with ANCA-associated
vasculitis in China. In the present case, the patient was an
immunosuppressed elderly male who received glucocorticoid therapy
for ANCA-associated vasculitis. Renal insufficiency might also
impair normal immune function (24). The risk of Nocardia
infection may therefore be higher in older patients with renal
insufficiency who are receiving immunosuppressive therapy. The
reported patient had the three of the aforementioned risk factors
for Nocardia infection. The lungs and skin were
simultaneously involved, and the condition manifested as multiple
sites of suppurative necrosis and abscess formation, which are
typical characteristics of nocardiosis. However, clinical recovery
was finally achieved after comprehensive treatment.
 | Table IReported cases of Nocardia
infection with underlying renal disease and receiving
immunosuppressive therapy. |
Table I
Reported cases of Nocardia
infection with underlying renal disease and receiving
immunosuppressive therapy.
| First author,
year | Country | Age, years | Sex | Type of kidney
disease | Clinical
syndrome | Immunosuppressive
agents | Treatment | Outcome | (Refs.) |
|---|
| McNab et al,
2000 | Chile | 24 | F | Lupus nephritis | Pleuropneumonia and
occipital abscess | Cyclophosphamide and
prednisone | Cotrimoxazole and
cefixime | Deceased | (12) |
| Lee et al,
2002 | South Korea | 37 | F | Lupus nephritis | Pleural effusion | Methylprednisolone
and cyclophosphamide | TMP-SMX | Cured | (13) |
| Pottumarthy et
al, 2003 | USA | 43 | F | SLE | Pulmonary
infection | Cyclosporine and
prednisone | TMP-SMX | Cured | (14) |
| Sonesson et
al, 2004 | Sweden | 60 | M | ANCA-associated
vasculitis | Pulmonary infection
and brain abscess | Methylprednisolone
and cyclophosphamide | Meropenem | Deceased | (3) |
| Elmaci et al,
2007 | Turkey | 49 | M | Nephrotic
syndrome | Mass lesion in the
left lower extremity and brain abscess | Prednisone and
cyclophosphamide | TMP-SMX | Cured | (15) |
| Tilak et al,
2012 | India | 50 | M | Renal transplant | Brain abscess | Cyclosporine,
azathioprine and prednisolone | TMP-SMX | Cured | (16) |
| Lee et al,
2012 | South Korea | 64 | M | Membranous
glomerulopathy | Pulmonary infections
and mass in the right upper arm | Prednisolone | TMP-SMX | Cured | (17) |
| Ates et al,
2013 | Turkey | 40 | F | Lupus nephritis | Subcutaneous and
brain abscesses | Azathioprine and
prednisolone | TMP-SMX and
ceftriaxone | Cured | (18) |
| Patel et al,
2013 | India | 50 | M | Renal transplant | Pulmonary
infection | Prednisolone, MMF and
cyclosporine | Ceftriaxone and
minocycline | Cured | (19) |
| Weerakkody et
al, 2015 | Sri Lanka | 38 | M | Renal transplant | Brain abscess | Tacrolimus and
MMF | Imipenem and
levofloxacin | Cured | (20) |
| Grahammer and
Fischer, 2015 | Germany | 71 | M | Membranous
glomerulonephritis | Pulmonary and i
ntramuscular abscesses | Prednisone and
MMF | Imipenem,
levofloxacin TMP- SMX and linezolid | Cured | (21) |
| Poisnel et al,
2015 | France | 51 | M | Peritoneal
dialysis | Pulmonary and
urinary tract infections |
Methylprednisolone | TMP-SMX | Deceased | (22) |
| Hirayama et
al, 2016 | Japan | 68 | M | ANCA-associated
vasculitis | Pulmonary
infection | Cyclophosphamide
and prednisolone | TMP-SMX | Cured | (4) |
| Zhu et al,
2017 | China | 60 | M | Nephrotic
syndrome | Pulmonary and
cutaneous infections | Cyclophosphamide
and methylprednisolone | TMP-SMX and
ceftriaxone | Cured | (23) |
| Wang et al,
2019 | China | 53 | F | ANCA-associated
renal vasculitis | Brain abscess |
Methylprednisolone | Meropenem +
voriconazole → piperacillin sodium/tazobactam → sodium +
voriconazole cefoperazone/ sulbactam + micafungin | Deceased | (5) |
| Present study | China | 69 | M | ANCA-associated
vasculitis | Pulmonary and
intramuscular abscesses | Cyclophosphamide
and prednisone | Linezolid and
TMP-SMX | Cured | - |
Linezolid is a synthetic antibacterial agent of the
novel antibiotic oxazolidinone, which is active against most
Gram-positive bacteria (25).
Linezolid has been reported as a novel second-line drug for
Nocardia infection, and is generally well tolerated
(26). In the present case, the
patient was clinically cured after receiving linezolid treatment
for 2 weeks, and no serious adverse drug reactions, such as
hematological side effects, lactic acidosis or peripheral
neuropathy, were observed, possibly due to the short-term nature of
the treatment. Despite the development of various new drugs,
including linezolid, in recent decades, sulfonamides remain the
first-line therapy against Nocardia infection (27,28),
the most representative drug being TMP-SMX; however,
drug-resistance has increased over time (29). In the present case, the renal
function of the patient was impaired at the time of admission.
After treatment of the primary disease with immunosuppressants, and
anti-infection treatment with linezolid during hospitalization, the
renal function of the patient returned to normal. A therapeutic
dose (0.48 g, twice a day) of oral TMP-SMX was added after
discharge. During the follow-up, renal function fluctuated in a
short period of time, but returned to normal after the TMP-SMX was
discontinued. During a year of follow-up, the laboratory test
results of the patient were normal.
The present typical case and the related published
literature indicate that rare opportunistic infections are not
entirely uncommon in immunocompromised patients. Clinicians should
be aware of possible Nocardia infection and its tendency to
spread when patients present with clinical manifestations of
systemic dissemination or locally encapsulated effusion (pus). An
early diagnosis of Nocardia infection, and the precise and
rational use of sensitive antibiotics can significantly improve the
prognosis of this high mortality-associated infection.
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by the Nantong Science and
Technology Project (grant nos. JCZ20060 and MS12021038).
Availability of data and materials
All data generated and/or analyzed during this study
are included in this published article.
Authors' contributions
XC and YZ contributed to the conceptualization and
design of the study, the collection of clinical information and the
drafting of the manuscript. YF analyzed medical images (MRI and CT
scans) and patient data, and advised on patient treatment. YF and
YZ contributed to critical revisions of the intellectual content
and confirm the authenticity of all the raw data. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki and approved by the Ethics Committee
of Affiliated Hospital of Nantong University (Nantong, China;
approval no. #2020-K029).
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the data and images included in the
present case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fernández LR, Guerra JM and González IZ:
Bacteremia by Nocardia farcinica. Med Clin (Barc). 154:520–521.
2020.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
2
|
Ambrosioni J, Lew D and Garbino J:
Nocardiosis: Updated clinical review and experience at a tertiary
center. Infection. 38:89–97. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sonesson A, Oqvist B, Hagstam P,
Björkman-Burtscher IM, Miörner H and Petersson AC: An
immunosuppressed patient with systemic vasculitis suffering from
cerebral abscesses due to Nocardia farcinica identified by 16S rRNA
gene universal PCR. Nephrol Dial Transplant. 19:2896–2900.
2004.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hirayama T, Takazono T, Horai Y, Tashiro
M, Saijo T, Kosai K, Morinaga Y, Kurihara S, Nakamura S, Imamura Y,
et al: Pulmonary nocardiosis caused by nocardia concava with a
literature review. Intern Med. 55:1213–1217. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wang T, Jia Y, Chu B, Liu H, Dong X and
Zhang Y: Nocardiosis in kidney disease patients under
immunosuppressive therapy: Case report and literature review. Int J
Med Sci. 16:838–844. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Brown-Elliott BA, Brown JM, Conville PS
and Wallace RJ Jr: Clinical and laboratory features of the Nocardia
spp. Based on current molecular taxonomy. Clin Microbiol Rev.
19:259–282. 2006.PubMed/NCBI View Article : Google Scholar
|
|
7
|
You Y, Chen W, Zhong B, Song Z and Yang X:
Disseminated nocardiosis caused by Nocardia elegans: A case report
and review of the literature. Infection. 46:705–710.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Salinas-Carmona MC: Nocardia brasiliensis:
From microbe to human and experimental infections. Microbes Infect.
2:1373–1381. 2000.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Husain S, McCurry K, Dauber J, Singh N and
Kusne S: Nocardia infection in lung transplant recipients. J Heart
Lung Transplant. 21:354–359. 2002.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Saubolle MA and Sussland D: Nocardiosis:
Review of clinical and laboratory experience. J Clin Microbiol.
41:4497–4501. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Salazar MN, Wray D, Denlinger C, Srinivas
T, Thomas B and Posadas A: Mediastinal mass and pericardial
tamponade in a renal transplant recipient: A rare case of nocardia
infection. Am J Case Rep. 14:295–299. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mc-Nab P, Fuentealba C, Ballesteros F,
Pacheco D, Alvarez M, Dabanch J and Cona E: Nocardia asteroides
infection in a patient with systemic lupus erythematosus. Rev Med
Chil. 128:526–528. 2000.PubMed/NCBI(In Spanish).
|
|
13
|
Lee JS, Lee YH, Cho SJ, Ji JD and Song GG:
A nocardial infection in a patient with systemic lupus
erythematosus. Korean J Med. 62:100–103. 2002.(In Korean).
|
|
14
|
Pottumarthy S, Limaye AP, Prentice JL,
Houze YB, Swanzy SR and Cookson BT: Nocardia veterana, a new
emerging pathogen. J Clin Microbiol. 41:1705–1709. 2003.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Elmaci I, Senday D, Silav G, Ekenel F,
Balak N, Ayan E, Akinci M, Isik N and Yazici S: Nocardial cerebral
abscess associated with mycetoma, pneumonia, and
membranoproliferative glomerulonephritis. J Clin Microbiol.
45:2072–2074. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tilak R, Achra A and Tilak V: Primary
cerebral nocardiosis in a renal transplant recipient: A case
report. J Clin Diagn Res. 6:1417–1418. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lee SH, Sung H, Lee SO, Choi SH, Kim YS,
Woo JH and Kim SH: The first report of disseminated Nocardia
concava infection, in an immunocompromised patient, in South Korea.
J Infect Chemother. 18:764–766. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ates Ö, Cilan H, Oymak S, Yildiz O and
Oymak O: Multidrug-resistant disseminated nocardia farcinica
infection in a systemic lupus erythematosus patient. Turk J
Rheumatol. 28:278–281. 2013.
|
|
19
|
Patel MP, Kute VB, Gumber MR, Shah PR,
Patel HV, Dhananjay KL, Jain SH, Trivedi HL and Vanikar AV:
Successful treatment of Nocardia pneumonia with cytomegalovirus
retinitis coinfection in a renal transplant recipient. Int Urol
Nephrol. 45:581–585. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Weerakkody RM, Palangasinghe DR, Wadanambi
S and Wijewikrama ES: ‘Primary’ nocardial brain abscess in a renal
transplant patient. BMC Res Notes. 8(701)2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Grahammer F and Fischer KG: Pulmonary
infiltrate and painful nodular leg lesions in a patient with
membranous glomerulonephritis. BMJ Case Rep.
28(bcr2015210032)2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Poisnel E, Roseau JB, Landais C,
Rodriguez-Nava V, Bussy E and Gaillard T: Nocardia veterana:
Disseminated infection with urinary tract infection. Braz J Infect
Dis. 19:216–219. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zhu N, Zhu Y, Wang Y and Dong S: Pulmonary
and cutaneous infection caused by Nocardia farcinica in a patient
with nephrotic syndrome: A case report. Medicine. (Baltimore).
96(e7211)2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Gandhi BV, Bahadur MM, Dodeja H, Aggrwal
V, Thamba A and Mali M: Systemic fungal infections in renal
diseases. J Postgrad Med. 51 (Suppl 1):S30–S36. 2005.PubMed/NCBI
|
|
25
|
Diekema DJ and Jones RN: Oxazolidinone
antibiotics. Lancet. 358:1975–1982. 2001.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Moylett EH, Pacheco SE, Brown-Elliott BA,
Perry TR, Buescher ES, Birmingham MC, Schentag JJ, Gimbel JF,
Apodaca A, Schwartz MA, et al: Clinical experience with linezolid
for the treatment of nocardia infection. Clin Infect Dis.
36:313–318. 2003.PubMed/NCBI View
Article : Google Scholar
|
|
27
|
Margalit I, Lebeaux D, Tishler O, Goldberg
E, Bishara J, Yahav D and Coussement J: How do I manage
nocardiosis? Clin Microbiol Infect. 27:550–558. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Hemmersbach-Miller M, Stout JE, Woodworth
MH, Cox GM and Saullo JL: Nocardia infections in the transplanted
host. Transpl Infect Dis. 20(e12902)2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Matchett C, Djamali A, Mandelbrot D,
Saddler C and Parajuli S: Nocardia infection in kidney transplant
recipients: A single-center experience. Transpl Infect Dis.
21(e13192)2019.PubMed/NCBI View Article : Google Scholar
|