Introduction
The prevalence of type 2 diabetes imposes notable
social and economic burdens globally (1). Before onset of type 2 diabetes,
individuals can live in a high-risk state of prediabetes, defined
as impaired fasting glucose or impaired glucose tolerance (IGT)
(2). IGT is an intermediate
category between normal glucose tolerance and overt diabetes
(3), which can be identified using
an oral glucose tolerance test. The number of individuals with IGT
has been increasing for decades with an estimated 374 million
individuals in 2017, equal to 7.7% of the worldwide population aged
18-99 years (1). Individuals with
IGT are at high risk of progression to type 2 diabetes (4), cardiovascular disease (5) and mortality (6).
Previous clinical trials have suggested that
lifestyle interventions, including diet and exercise, can
effectively slow the progression from IGT to type 2 diabetes
(7-9).
However, not all individuals with prediabetes achieve the
recommended lifestyle modifications and may instead need
pharmacotherapy. Antidiabetic drugs, such as metformin, acarbose,
rosiglitazone, pioglitazone and liraglutide, have proven beneficial
for the prevention of diabetes and underlying prediabetes (8,10-13).
Liraglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist
that stimulates insulin (INS) secretion, inhibits glucagon
secretion and lowers plasma glucose levels after binding to the
GLP-1 receptor (14). Liraglutide
not only protects and restores pancreatic β-cell activity but is
also involved in atherosclerosis prevention in patients with
diabetes (15-17).
For individuals with IGT, preclinical studies have demonstrated
that liraglutide may have beneficial effects on atherosclerosis and
potentially reduce the risk for cardiovascular disease (18,19).
However, to the best of our knowledge, little conclusive evidence
from clinical trials has been shown. The present study was
therefore performed to evaluate the efficacy and safety of
liraglutide for prevention of atherosclerosis progression in
patients with IGT.
Materials and methods
Participants
The study protocol was approved by the Institutional
Review Board of the Chengyang People's Hospital in Qingdao (China;
approval no. CYQRMYY2019-09-11) and performed following the 1964
Declaration of Helsinki and its later amendments. All study
participants provided written informed consent. A total of 39
patients (26 female and 13 male) aged 20-75 years who were
overweight or obese (BMI, 27-40 kg/m2) and diagnosed
with IGT from October 2019 to September 2021 in Chengyang People's
Hospital were included in the present study. Glucose tolerance
status was defined using an oral glucose tolerance test (OGTT)
according to the World Health Organization criteria (20). The exclusion criteria were as
follows: i) Type 1 or 2 diabetes; ii) lower limb ischemia; iii)
treatment with hypoglycemic drugs or angiotensin-converting enzyme
inhibitor/angiotensin II receptor antagonist during the trial; iv)
chronic disease or health conditions; v) acute illness (such as
infection) and vi) pregnancy or lactation.
The patient baseline clinical characteristics,
including age, sex, height, weight, BMI, waist circumference (WC),
hip circumference (HC), systolic blood pressure (SBP) and diastolic
blood pressure (DBP), were recorded.
Study design
The study period was October 2009 to September 2021.
Participants were randomized to receive either liraglutide (n=17)
or lifestyle interventions (n=22) for 6 months. Liraglutide was
injected subcutaneously daily before breakfast. The dose was
escalated weekly from 0.6 to 1.2 mg (increments, 0.1 mg per week).
Lifestyle interventions included dietary intervention and physical
activity. The dietary intervention involved advice and counseling
to develop an individual plan for behavioral change aiming to
achieve the following: Total dietary energy intake >50% from
carbohydrates; decreased total and saturated fat intake with
<30% total dietary energy from fat intake; increased fiber
intake and weight loss to achieve BMI <25 kg/m2
(21,22). The physical activity intervention
was designed to encourage participation in increased physical
activity equivalent to 30 min of moderate aerobic physical
activity/day. Both participants and study administrators
(physicians, nurses, dietitians and coordinators) were blinded to
the treatment assignment.
OGTT
Following 14 h of overnight fasting, all subjects
were admitted to the Chengyang People's Hospital in Qingdao (China)
between 8:00 and 9:00 a.m. After resting for 30 min, venous blood
(2 ml) was drawn to measure fasting glucose and INS levels. A 75-g
oral glucose load was administered over a 1 min period. Blood draws
for glucose and analysis of INS levels were performed 60 and 120
min after administration of the glucose load. Serum INS was
measured using the Mercodia Insulin ELISA kit (cat. no. 10-1113-01;
Mercodia AB) (23).
Biochemical analysis
Blood samples were collected after 14 h overnight
fasting at baseline and after 4 months of each treatment. Serum
levels of triglyceride (TG) and total cholesterol (TC) were
measured using an enzymatic method (Roche Diagnostics). The
phosphotungstic acid-Mg2+ method was used to determine
high-density lipoprotein (HDL) concentrations. Low-density
lipoprotein (LDL) was estimated in samples with a triglyceride
level <400 mg/dl, using the modified Friedewald formula
(24).
The glycosylated hemoglobin (HbA1c) levels were
measured through boronate-affinity high-performance liquid
chromatography (Premier Hb9210™; Trinity Biotech, Inc.). The
analytical column contains aminophenylboronic acid bonded to a
porous polymer support (gel) and pumps transfer reagents and
patient samples through the analytical column. Modules of the
instruments are as follows: SPD 20A UV detector, DGU-20A5 degasser,
SIL-20A HT autosampler, LC-20AT pump (liquid chromatograph) and
CTO-IOAS column oven. Briefly, to a 5 µl sample, a 1,250 µl
hemolysis reagent was added and the mixture was left for 30 min at
37˚C. The precipitated protein was removed by centrifugation at
10,000 x g at 4˚C for 2 min. A total of 20 µl of the supernatant
was injected into the chromatographic system. Separation of HbA1c
was achieved with a 35x4.6 mm cation exchanger column (ImmuChrom
GmbH) with a particle size of 3 µm at a flow rate of 1.5 ml/min.
The areas of peaks detected by UV detector (415 nm) were used for
quantification. HbA1c levels were expressed as %. To minimize
inter-batch analytical variation, all samples from any given
volunteer were assayed in a single batch. Each sample from one
subject was assayed in duplicate, using the analytical system in
accordance with the manufacturer's instructions. The same lots of
calibrators, reagent lot and quality-control materials were used
throughout, and analyses were performed by a single analyst.
C-reactive protein (CRP) levels were measured using
the immunoturbidimetric method (CRPL3 assay; Roche Diagnostics) on
a Cobas 702 module (Roche Diagnostics). TNF-α (cat. no.
YSRIBIO-3736), IL-1β (cat. no. YSRIBIO-3292), IL-2α (cat. no.
YSRIBIO-4666) and IL-6 (cat. no. YSRIBIO-4610) levels were measured
using ELISA kits obtained from Shanghai Yansheng Biochemical
Reagents Co., Ltd. The ELISA procedure was performed according to
the manufacturer' instructions. White blood cell (WBC) count
analysis was performed using using the Sysmex XE 2100 automated
hematology system (Sysmex Corporation) (25).
Ultrasonography of carotid
intima-media thickness (CIMT)
B-mode real-time ultrasound was performed at
baseline and after 4 months of treatment to evaluate arterial wall
thickness in the carotid arteries as a surrogate marker of
subclinical atherosclerosis (26).
All examinations were performed by a single examiner in a blinded
manner using the same ultrasound machine (Acuson Antares™
ultrasound system, premium edition; Siemens Healthineers), without
access to previous scans when follow-up studies were performed. The
ultrasound examination was performed in a standardized manner and
specific sonographic images were obtained for comparison.
Patients were examined in the supine position and
each carotid wall or segment was evaluated to identify IMT, as
previously reported (27). Each
scan of the common carotid artery began just above the clavicle and
the transducer was moved to the carotid bifurcation and along the
internal carotid artery. In total, three segments were identified
and measured in anterior and posterior planes on each side: i)
Distal 1.0 cm of the common carotid artery proximal to the
bifurcation; ii) the bifurcation and iii) proximal 1.0 cm of the
internal carotid artery. At each of these sites, IMT was
determined, defined as the distance between the echogenic line
representing the intimal blood interface and the outer echogenic
line representing the adventitial junction. IMT <0.9 mm was
defined as normal; 0.9 mm≤ IMT <1.3 mm was defined as intimal
medial thickness; and IMT ≥1.3 mm was defined as plaque. In
addition, electrocardiogram revealed the general condition of the
coronary arteries. ST segment or T wave change on electrocardiogram
was considered as myocardial ischemia.
Follow-up
The primary endpoint was occurrence of
atherosclerosis in macrovasculature, as well as in peripheral and
visceral vessels. Patients were followed up once every 3 months,
with a total follow-up duration of 6 months. The patient clinical
profile and laboratory measurements were recorded at each visit.
The side effects during the intervention were monitored to assess
the tolerance and safety of each treatment.
Statistical analysis
Statistical analysis was performed using SPSS
version 22.0 (IBM Corp.). The normality of distribution of the
variables data was assessed using Shapiro-Wilk test. Data normally
distributed are presented as mean ± standard deviation and tested
using Student's t test. If the data were skewed, the Wilcoxon rank
sum test was used to assess differences in changes before and after
treatment between the two groups. Categorical data was compared
using χ2 test or Fisher's exact probability method.
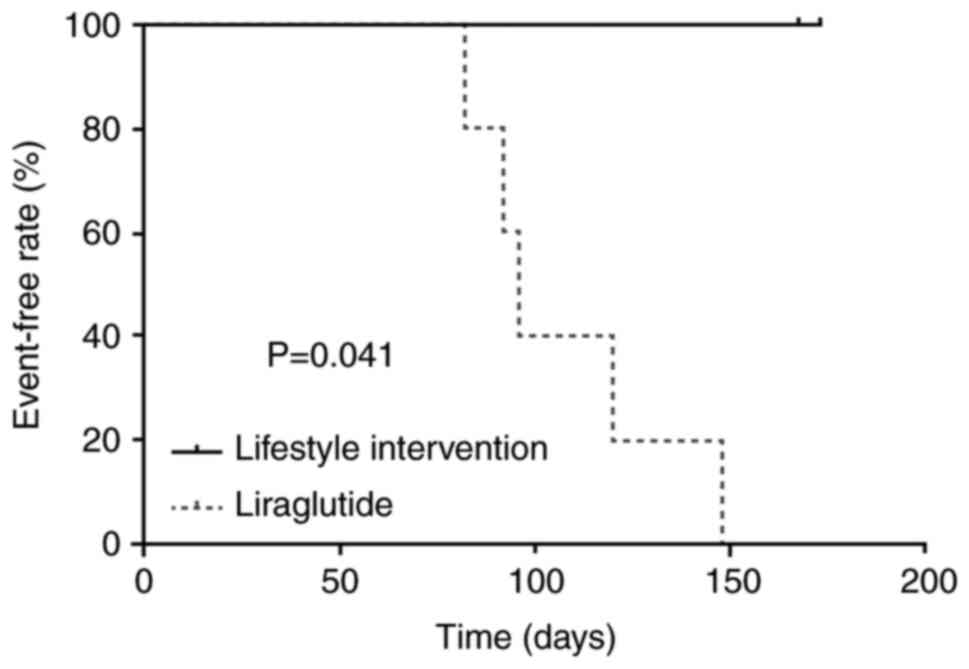
Kaplan-Meier survival analysis and a log-rank test were used to
compare the risk of vascular disease following treatment between
the two groups. A two-tailed P<0.05 was considered to indicate a
statistically significant difference.
Results
Clinical characteristics of enrolled
patients
Individuals randomized to receive liraglutide or
lifestyle intervention had similar baseline characteristics
including sex (P=0.819), age (P=0.322), BMI (P=0.596), WC
(P=0.734), HC (P=0.292), DBP (P=0.795) and SBP (P=0.547) (Table I). BMI, WC and HC after liraglutide
treatment were lower than those after lifestyle intervention (all
P<0.001). DBP and SBP levels did not show any
statistically significant difference between the treatment arms
(all P>0.05).
 | Table IClinical characteristics of
participants before and after treatment. |
Table I
Clinical characteristics of
participants before and after treatment.
| | Lifestyle
intervention (n=22) | Liraglutide
(n=17) | |
|---|
| Characteristic | Pre-treatment | Post-treatment | Δ change | Pre-treatment | Post-treatment | Δ change |
P-valuea |
P-valueb |
|---|
| Sex, female, n
(%) | 15 (68.18) | 15 (68.18) | NA | 11 (64.71) | 11 (64.71) | NA | 0.819 | NA |
| Mean age,
years | 48.91±10.12 | 49.27±10.01 | 0.41±0.50 | 44.92±14.69 | 45.35±14.75 | 0.41±0.51 | 0.322 | 1.000 |
| BMI,
kg/m2 | 26.21±4.33 | 26.15±3.21 | -0.06±0.08 | 26.84±2.47 | 23.38±3.71 | -3.46±0.67 | 0.596 | <0.001 |
| Waist
circumference, cm | 87.12±5.74 | 86.47±5.36 | -0.65±0.28 | 86.52±4.98 | 82.31±5.48 | -4.21±0.75 | 0.734 | <0.001 |
| Hip circumference,
cm | 102.86±5.88 | 99.98±5.49 | -2.88±0.41 | 101.02±4.51 | 90.03±4.07 | -10.99±1.42 | 0.292 | <0.001 |
| Diastolic blood
pressure, mmHg | 120.52±18.39 | 119.01±17.16 | -1.51±0.74 | 118.86±21.13 | 117.26±20.19 | -1.60±0.55 | 0.795 | 0.677 |
| Systolic blood
pressure, mmHg | 69.47±11.13 | 69.22±11.64 | -0.25±0.22 | 67.33±10.57 | 67.02±11.16 | -0.31±0.34 | 0.547 | 0.508 |
Side effects in liraglutide treatment
group and lifestyle intervention group
Treatment-associated side effects are shown in
Table SI. The most common side
effect of liraglutide was nausea (n=4; 23.5%). There was no
significant difference in side effects between liraglutide
treatment and lifestyle intervention.
Effect of liraglutide treatment on
serum glucose and INS levels
Liraglutide treatment could induce a greater
reduction in HbA1c compared with lifestyle intervention
(P<0.001; Table II).
Similar trends were also observed for fasting blood glucose,
fasting INS, 2 h postprandial blood glucose and 2 h postprandial
INS between liraglutide treatment and lifestyle intervention (all
P<0.001; Table II).
 | Table IIDynamic changes of serum HbA1c,
glucose and insulin before and after treatment. |
Table II
Dynamic changes of serum HbA1c,
glucose and insulin before and after treatment.
| | Lifestyle
intervention (n=22) | Liraglutide
(n=17) | |
|---|
| Parameter | Pre-treatment | Post-treatment | Δ change | Pre-treatment | Post-treatment | Δ change |
P-valuea |
|---|
| HbA1c, % | 5.91±0.33 | 5.89±0.29 | -0.02±0.02 | 5.98±0.42 | 5.16±0.39 | -0.82±0.07 | <0.001 |
| Fasting blood
glucose, mmol/l | 6.02±1.48 | 6.04±1.85 | 0.01±0.02 | 5.97±1.28 | 5.75±1.21 | -0.22±0.06 | <0.001 |
| Fasting insulin,
mu/l | 15. 42±3.57 | 14. 94±4.39 | -0.48±0.06 | 15.77±2.94 | 8.86±3.36 | -6.91±0.42 | <0.001 |
| 2 h postprandial
blood glucose, mmol/l | 9.26±1.19 | 8.72±1.60 | -0.54±0.04 | 9.33±1.46 | 6.84±1.19 | -2.49±0.27 | <0.001 |
| 2 h insulin,
mU/l | 92.48±21.02 | 90.7±26.89 | -1.78±0.83 | 91.38±14.68 | 47.94±19.98 | -43.44±5.36 | <0.001 |
Effect of liraglutide treatment on
lipid profile
Liraglutide treatment significantly decreased TC and
LDL levels compared with lifestyle intervention (all
P<0.001; Table III).
However, no changes in TG and HDL were observed.
 | Table IIIDynamic changes of lipid profile
before and after treatment. |
Table III
Dynamic changes of lipid profile
before and after treatment.
| | Lifestyle
intervention (n=22) | Liraglutide
(n=17) | |
|---|
| Parameter | Pre-treatment | Post-treatment | Δ change | Pre-treatment | Post-treatment | Δ change |
P-valuea |
|---|
| Triglyceride,
mmol/l | 1.29±0.88 | 1.24±0.45 | -0.05±0.04 | 1.27±0.53 | 1.21±0.36 | -0.06±0.06 | 0.537 |
| Total cholesterol,
mmol/l | 5.59±1.04 | 5.51±1.14 | -0.07±0.08 | 5.53±0.98 | 4.42±0.95 | -1.11±0.19 | <0.001 |
| High-density
lipoprotein, mmol/l | 1.50±0.18 | 1.48±0.28 | -0.02±0.03 | 1.48±0.26 | 1.45±0.34 | -0.03±0.05 | 0.443 |
| Low-density
lipoprotein, mmol/l | 2.76±1.19 | 2.68±1.58 | -0.08±0.24 | 9.32±1.46 | 6.84±1.19 | -2.49±0.51 | <0.001 |
Effect of liraglutide treatment on
inflammatory markers
Liraglutide treatment significantly decreased levels
of WBC, CRP, TNF-α, IL-1β, IL-2α and IL-6 compared with lifestyle
intervention (all P<0.001; Table
IV).
 | Table IVDynamic changes of inflammatory
markers before and after treatment. |
Table IV
Dynamic changes of inflammatory
markers before and after treatment.
| | Lifestyle
intervention (n=22) | Liraglutide
(n=17) | |
|---|
| Parameter | Pre-treatment | Post-treatment | Δ change | Pre-treatment | Post-treatment | Δ change |
P-valuea |
|---|
| White blood cell,
x109/l | 6.94±0.54 | 6.95±0.38 | 0.01±0.01 | 6.94±0.55 | 5.17±0.39 | -1.77±0.21 | <0.001 |
| C-reactive protein,
mg/l | 5.39±1.05 | 5.43±0.81 | 0.04±0.03 | 5.38±0.97 | 2.41±0.51 | -2.97±0.35 | <0.001 |
| TNF-α, ng/l | 25.65±3.86 | 24.18±5.25 | -1.47±0.42 | 26.53±3.57 | 14.01±3.97 | -12.53±0.73 | <0.001 |
| IL-1β, ng/l | 54.56±7.78 | 51.97±12.03 | -2.59±4.68 | 54.14±6.29 | 30.84±7.41 | -23.29±8.71 | <0.001 |
| IL-2α, ng/l | 2.89±0.30 | 2.78±0.54 | -0.11±0.07 | 2.82±0.36 | 0.87±0.24 | -1.96±0.42 | <0.001 |
| IL-6, ng/l | 15.37±2.49 | 15.13±2.91 | -0.24±0.22 | 15.69±2.24 | 6.65±1.51 | -9.04±0.72 | <0.001 |
Effect of liraglutide treatment on the
development of atherosclerosis
The levels of CIMT decreased significantly in
patients treated with liraglutide compared with lifestyle
intervention (P<0.001; Table
V). Although the lifestyle intervention group exhibited a
higher incidence of atherosclerosis in coronary and peripheral
arteries compared with that in the liraglutide treatment group, no
significant difference was observed (all P>0.05; Table SII). Based on the Kaplan-Meier
analysis, the incidence of vascular disease in the liraglutide
group was significantly lower than that in the lifestyle
intervention group (log-rank test P=0.041; Fig. 1).
 | Table VDynamic changes of CIMT before and
after treatment. |
Table V
Dynamic changes of CIMT before and
after treatment.
| | Lifestyle
intervention (n=22) | Liraglutide
(n=17) | |
|---|
| Parameter | Pre-treatment | Post-treatment | Δ change | Pre-treatment | Post-treatment | Δ change |
P-valuea |
|---|
| CIMT, mm | 0.91±0.23 | 0.92±0.18 | 0.01±0.01 | 0.91±0.25 | 0.70±0.16 | -0.21±0.07 | <0.001 |
Discussion
In the present study, the efficacy and safety of
liraglutide were evaluated for prevention of atherosclerotic
development in patients with IGT. A greater decrease in CIMT was
observed in patients treated with liraglutide compared with those
who received lifestyle interventions. Furthermore, hematological
and biochemical examination indicated that liraglutide treatment
ameliorated the lipid profile and inflammation in patients with
IGT.
Cardiovascular disease causes disability and death
in patients with diabetes. La Sala et al (28) highlighted in a review that the
appearance of atherosclerosis may start as early as the onset of
diabetes. Moreover, a systematic review and meta-analysis
highlighted a series of large-scale epidemiological studies that
showed that early manifestation of diabetes, especially IGT,
aggravates atherosclerosis and increase the risk of developing
cardiovascular diseases (5,29-31).
IGT represents an intermediate metabolic state between normal
glucose homeostasis and hyperglycemia, which has been suggested as
a strong predictor of type 2 diabetes and macrovascular disease
(4,5). Therefore, interventions should be
performed during the early stage of diabetes to decrease the
occurrence of cardiac complications.
IGT has an insidious onset and its non-specific
clinical findings may not be instantly discernible. With the effect
of behavior and lifestyle on blood glucose levels, 30% of patients
with IGT eventually develop diabetes (4). The Da Qing Diabetes Prevention
Outcome Study was the first global study to report that lifestyle
changes could reduce the risk of cardiovascular events in patients
with IGT (32). However, changing
lifestyle required long-term adherence and patients often exhibit
poor compliance (33). Therefore,
for those who cannot adhere to a healthy lifestyle for a long
period or have a poor response to lifestyle interventions,
therapeutic interventions should be considered. At present,
disputes remain regarding the optimum regimens for pre-diabetes.
The DPP (metformin) (8), DREAM
(INS sensitizer) (11) and
STOP-NIDDM (acarbose) (34)
studies have shown that medications notably decrease the risk of
diabetes and cardiovascular disease.
An ideal option for IGT treatment may be a drug that
can lower the postprandial blood glucose levels and restore the
first phase of INS secretion with no serious side effects (such as
gastrointestinal reaction, weight gain and hypoglycemia). With the
gradual application of novel hypoglycemic drugs (such as GLP-1
receptor agonists) in clinical practice, liraglutide has also
attracted attention (35-37).
Liraglutide has 97% amino acid sequence homologous to native human
GLP-1, which preserves the biological activity of native GLP-1 and
is resistant to degradation (37).
Furthermore, liraglutide activates the GLP-1 receptor on the
surface of pancreatic cells, increases cyclic adenosine
monophosphate in the cells, promotes INS release, inhibits glucagon
secretion and improves the sensitivity of peripheral tissue to INS
(38,39).
By binding to the GLP-1 receptor in the
gastrointestinal tract, liraglutide could directly inhibit gastric
emptying, slowing gastrointestinal peristalsis and gastric juice
secretion (37). It may also
interfere with absorption of nutrients and enable weight loss
(40). In vivo studies have
showed that the GLP-1 receptor agonist liraglutide could improve
the cell ultrastructure in IGT rats, inhibit excessive
proliferation of α islet cells, decrease the excessive synthesis of
glucagon, improve the structure of pancreatic islets, alleviate INS
resistance and delay the development of glucose metabolism disorder
(18,41). In the present study, metabolic
markers such as TC and LDL for patients with IGT were significantly
improved following treatment with liraglutide, suggesting that
liraglutide may serve as a therapeutic strategy for IGT
management.
Previous studies have found that the levels of CIMT
are significantly increased in the early stages of IGT (42,43).
IGT is a risk factor for carotid atherosclerosis (44,45).
The European Society of Cardiology and the European Society of
Hypertension guidelines recommend CIMT >0.9 mm as a marker of
target organ injury in atherosclerosis (46). Preclinical studies have shown that
the gradual emergence of atherosclerotic plaques is associated with
oxidative stress injury, macrophage-mediated phagocytosis and
formation of foam cells (47,48).
Furthermore, exacerbated INS resistance and production of
proinflammatory cytokines also promote development of
atherosclerosis. Existing evidence suggests that liraglutide may
inhibit activation of NF-κB, which serves as an essential
inflammatory biomarker for regulating the balance of the
proinflammatory-anti-inflammatory system (49,50).
Zhang et al (51)
demonstrated that liraglutide protects cardiomyocytes from
IL-1β-induced metabolic disturbance and mitochondrial dysfunction.
The present study showed that inflammatory indicators and CIMT were
significantly decreased following treatment with liraglutide,
suggesting that GLP-1 receptor agonist improved the inflammatory
response in patients with IGT and slowed the occurrence of
atherosclerosis.
The present study has certain limitations. First,
the sample size was relatively small. Therefore, a larger
prospective study is required to verify the results. Secondly, the
diet type and schedule were not controlled for lifestyle
interventions, which may have led to differences in outcomes
between patients. Thirdly, the follow-up duration was short. Since
vascular disease has a slow and insidious onset, statistical
significance may have been achieved for several outcomes with a
longer follow-up period and more events. In addition, only blood
tests and CIMT were performed to evaluate atherosclerotic
development. Although several indices (such as aortic plaque
burden) have also been considered as key indicators of
atherosclerosis in preclinical research (52), their diagnostic value remains to be
validated in clinical studies. Other indices, such as
ankle-brachial index (53) and
arterial pulse wave velocity (54), are also key indicators of
atherosclerotic progression. However, these indices were not
employed in the present study due to low patient compliance. These
indices should be included in a future prospective study.
In conclusion, GLP-1 receptor agonist liraglutide
may slow atherosclerosis development and improve the inflammatory
status and intimal function in patients with IGT with few side
effects.
Supplementary Material
Side effects.
Location of atherosclerosis.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Qingdao Medical
Research Guidance Plan (grant no. 2015-WJZD142).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XR conceived and designed the study and revised the
manuscript. LS contributed to data collection and analysis and
drafted the manuscript. YY and YL performed data analysis and
manuscript revision. XR and LS confirmed the authenticity of all
the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
All procedures performed in studies involving human
participants were performed following the ethical standards of the
institutional and/or national research committee, as well as the
1964 Helsinki Declaration and its later amendments or comparable
ethical standards. All procedures were approved by the
Institutional Review Board of the Chengyang People's Hospital in
Qingdao (approval no. CYQRMYY2019-09-11). Written informed consent
was obtained from all participants included in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Saeedi P, Petersohn I, Salpea P, Malanda
B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA,
Ogurtsova K, et al: Global and regional diabetes prevalence
estimates for 2019 and projections for 2030 and 2045: Results from
the International Diabetes Federation Diabetes Atlas,
9th edition. Diabetes Res Clin Pract.
157(107843)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
de Vegt F, Dekker JM, Jager A, Hienkens E,
Kostense PJ, Stehouwer CDA, Nijpels G, Bouter LM and Heine RJ:
Relation of impaired fasting and postload glucose with incident
type 2 diabetes in a Dutch population: The Hoorn Study. JAMA.
285:2109–2113. 2001.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Harris MI: Impaired glucose tolerance in
the U.S. population. Diabetes Care. 12:464–474. 1989.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Edelstein SL, Knowler WC, Bain RP, Andres
R, Barrett-Connor EL, Dowse GK, Haffner SM, Pettitt DJ, Sorkin JD,
Muller DC, et al: Predictors of progression from impaired glucose
tolerance to NIDDM: An analysis of six prospective studies.
Diabetes. 46:701–710. 1997.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Huang Y, Cai X, Mai W, Li M and Hu Y:
Association between prediabetes and risk of cardiovascular disease
and all cause mortality: Systematic review and meta-analysis. BMJ.
355(i5953)2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gong Q, Zhang P, Wang J, An Y, Gregg EW,
Li H, Zhang B, Shuai Y, Yang W, Chen Y, et al: Changes in mortality
in people with IGT before and after the onset of diabetes during
the 23-year follow-up of the Da Qing Diabetes Prevention Study.
Diabetes Care. 39:1550–1555. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Tuomilehto J, Lindström J, Eriksson JG,
Valle TT, Hämäläinen H, Ilanne-Parikka P, Keinänen-Kiukaanniemi S,
Laakso M, Louheranta A, Rastas M, et al: Prevention of type 2
diabetes mellitus by changes in lifestyle among subjects with
impaired glucose tolerance. N Engl J Med. 344:1343–1350.
2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Knowler WC, Barrett-Connor E, Fowler SE,
Hamman RF, Lachin JM, Walker EA and Nathan DM: Diabetes Prevention
Program Research Group. Reduction in the incidence of type 2
diabetes with lifestyle intervention or metformin. N Engl J Med.
346:393–403. 2002.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ramachandran A, Snehalatha C, Mary S,
Mukesh B, Bhaskar AD and Vijay V: Indian Diabetes Prevention
Programme (IDPP). The Indian Diabetes Prevention Programme shows
that lifestyle modification and metformin prevent type 2 diabetes
in Asian Indian subjects with impaired glucose tolerance (IDPP-1).
Diabetologia. 49:289–297. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Holman RR, Coleman RL, Chan JCN, Chiasson
JL, Feng H, Ge J, Gerstein HC, Gray R, Huo Y, Lang Z, et al:
Effects of acarbose on cardiovascular and diabetes outcomes in
patients with coronary heart disease and impaired glucose tolerance
(ACE): A randomised, double-blind, placebo-controlled trial. Lancet
Diabetes Endocrinol. 5:877–886. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
DREAM (Diabetes REduction Assessment with
ramipril and rosiglitazone Medication) Trial Investigators.
Gerstein HC, Yusuf S, Bosch J, Pogue J, Sheridan P, Dinccag N,
Hanefeld M, Hoogwerf B, Laakso M, et al: Effect of rosiglitazone on
the frequency of diabetes in patients with impaired glucose
tolerance or impaired fasting glucose: A randomised controlled
trial. Lancet. 368:1096–1105. 2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
DeFronzo RA, Tripathy D, Schwenke DC,
Banerji M, Bray GA, Buchanan TA, Clement SC, Henry RR, Hodis HN,
Kitabchi AE, et al: Pioglitazone for diabetes prevention in
impaired glucose tolerance. N Engl J Med. 364:1104–1115.
2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Pi-Sunyer X, Astrup A, Fujioka K, Greenway
F, Halpern A, Krempf M, Lau DC, le Roux CW, Violante Ortiz R,
Jensen CB, et al: A randomized, controlled trial of 3.0 mg of
liraglutide in weight management. N Engl J Med. 373:11–22.
2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Blonde L and Russell-Jones D: The safety
and efficacy of liraglutide with or without oral antidiabetic drug
therapy in type 2 diabetes: An overview of the LEAD 1-5 studies.
Diabetes Obes Metab. 11 (Suppl 3):S26–S34. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Rizzo M, Nikolic D, Patti AM, Mannina C,
Montalto G, McAdams BS, Rizvi AA and Cosentino F: GLP-1 receptor
agonists and reduction of cardiometabolic risk: Potential
underlying mechanisms. Biochim Biophys Acta Mol Basis Dis.
1864:2814–2821. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Vergès B and Charbonnel B: After the
LEADER trial and SUSTAIN-6, how do we explain the cardiovascular
benefits of some GLP-1 receptor agonists? Diabetes Metab. 43 (Suppl
1):2S3–2S12. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Nauck MA, Quast DR, Wefers J and Meier JJ:
GLP-1 receptor agonists in the treatment of type 2
diabetes-state-of-the-art. Mol Metab. 46(101102)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Noyan-Ashraf MH, Shikatani EA, Schuiki I,
Mukovozov I, Wu J, Li RK, Volchuk A, Robinson LA, Billia F, Drucker
DJ and Husain M: A glucagon-like peptide-1 analog reverses the
molecular pathology and cardiac dysfunction of a mouse model of
obesity. Circulation. 127:74–85. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Simanenkova A, Minasian S, Karonova T,
Vlasov T, Timkina N, Shpilevaya O, Khalzova A, Shimshilashvili A,
Timofeeva V, Samsonov D, et al: Comparative evaluation of metformin
and liraglutide cardioprotective effect in rats with impaired
glucose tolerance. Sci Rep. 11(6700)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Shareef M, Saleh L, van den Meiracker AH
and Visser W: The impact of implementing the WHO-2013 criteria for
gestational diabetes mellitus on its prevalence and pregnancy
outcomes: A comparison of the WHO-1999 and WHO-2013 diagnostic
thresholds. Eur J Obstet Gynecol Reprod Biol. 246:14–18.
2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Penn L, White M, Oldroyd J, Walker M,
Alberti KG and Mathers JC: Prevention of type 2 diabetes in adults
with impaired glucose tolerance: The European Diabetes Prevention
RCT in Newcastle upon Tyne, UK. BMC Public Health.
9(342)2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Mann J, Lean M, Toeller M, Slama G,
Uusitupa M and Vessby B: Recommendations for the nutritional
management of patients with diabetes mellitus. Eur J Clin Nutr.
54:353–355. 2000.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lee MY, Fraser JD, Chapman MJ,
Sundararajan K, Umapathysivam MM, Summers MJ, Zaknic AV, Rayner CK,
Meier JJ, Horowitz M and Deane AM: The effect of exogenous
glucose-dependent insulinotropic polypeptide in combination with
glucagon-like peptide-1 on glycemia in the critically ill. Diabetes
Care. 36:3333–3336. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
DeLong DM, DeLong ER, Wood PD, Lippel K
and Rifkind BM: A comparison of methods for the estimation of
plasma low- and very low-density lipoprotein cholesterol: The Lipid
Research Clinics Prevalence Study. JAMA. 256:2372–2377.
1986.PubMed/NCBI
|
|
25
|
Ruzicka K, Veitl M, Thalhammer-Scherrer R
and Schwarzinger I: The new hematology analyzer Sysmex XE-2100:
Performance evaluation of a novel white blood cell differential
technology. Arch Pathol Lab Med. 125:391–396. 2001.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Rizzo M, Chandalia M, Patti AM, Di Bartolo
V, Rizvi AA, Montalto G and Abate N: Liraglutide decreases carotid
intima-media thickness in patients with type 2 diabetes: 8-month
prospective pilot study. Cardiovasc Diabetol. 13(49)2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Corrado E, Rizzo M, Tantillo R, Muratori
I, Bonura F, Vitale G and Novo S: Markers of inflammation and
infection influence the outcome of patients with baseline
asymptomatic carotid lesions: A 5-year follow-up study. Stroke.
37:482–486. 2006.PubMed/NCBI View Article : Google Scholar
|
|
28
|
La Sala L, Prattichizzo F and Ceriello A:
The link between diabetes and atherosclerosis. Eur J Prev Cardiol.
26:15–24. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Pankow JS, Kwan DK, Duncan BB, Schmidt MI,
Couper DJ, Golden S and Ballantyne CM: Cardiometabolic risk in
impaired fasting glucose and impaired glucose tolerance: The
Atherosclerosis Risk in Communities Study. Diabetes Care.
30:325–331. 2007.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Magliano DJ, Soderberg S, Zimmet PZ,
Cartensen B, Balkau B, Pauvaday V, Kowlessur S, Tuomilehto J,
Alberti KG and Shaw JE: Mortality, all-cause and cardiovascular
disease, over 15 years in multiethnic mauritius: Impact of diabetes
and intermediate forms of glucose tolerance. Diabetes Care.
33:1983–1989. 2010.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Barr EL, Zimmet PZ, Welborn TA, Jolley D,
Magliano DJ, Dunstan DW, Cameron AJ, Dwyer T, Taylor HR, Tonkin AM,
et al: Risk of cardiovascular and all-cause mortality in
individuals with diabetes mellitus, impaired fasting glucose, and
impaired glucose tolerance: The Australian Diabetes, Obesity, and
Lifestyle Study (AusDiab). Circulation. 116:151–157.
2007.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Gong Q, Zhang P, Wang J, Ma J, An Y, Chen
Y, Zhang B, Feng X, Li H, Chen X, et al: Morbidity and mortality
after lifestyle intervention for people with impaired glucose
tolerance: 30-year results of the Da Qing Diabetes Prevention
Outcome Study. Lancet Diabetes Endocrinol. 7:452–461.
2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Schuler G, Adams V and Goto Y: Role of
exercise in the prevention of cardiovascular disease: Results,
mechanisms, and new perspectives. Eur Heart J. 34:1790–1799.
2013.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Chiasson JL, Josse RG, Gomis R, Hanefeld
M, Karasik A and Laakso M: Acarbose for prevention of type 2
diabetes mellitus: The STOP-NIDDM randomised trial. Lancet.
359:2072–2077. 2002.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Frías JP, Davies MJ, Rosenstock J, Pérez
Manghi FC, Fernández Landó L, Bergman BK, Liu B, Cui X and Brown K:
SURPASS-2 Investigators. Tirzepatide versus semaglutide once weekly
in patients with type 2 diabetes. N Engl J Med. 385:503–515.
2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
GRADE Study Research Group. Nathan DM,
Lachin JM, Bebu I, Burch HB, Buse JB, Cherrington AL, Fortmann SP,
Green JB, Kahn SE, et al: Glycemia reduction in type 2 diabetes
microvascular and cardiovascular outcomes. N Engl J Med.
387:1075–1088. 2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Sisson EM: Liraglutide: Clinical
pharmacology and considerations for therapy. Pharmacotherapy.
31:896–911. 2011.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Knudsen LB and Lau J: The discovery and
development of liraglutide and semaglutide. Front Endocrinol
(Lausanne). 10(155)2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Gallwitz B: Glucagon-like peptide-1
analogues for type 2 diabetes mellitus. Drugs. 71:1675–1688.
2011.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Lazzaroni E, Ben Nasr M, Loretelli C,
Pastore I, Plebani L, Lunati ME, Vallone L, Bolla AM, Rossi A,
Montefusco L, et al: Anti-diabetic drugs and weight loss in
patients with type 2 diabetes. Pharmacol Res.
171(105782)2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Schwasinger-Schmidt T, Robbins DC,
Williams SJ, Novikova L and Stehno-Bittel L: Long-term liraglutide
treatment is associated with increased insulin content and
secretion in beta-cells, and a loss of alpha-cells in ZDF rats.
Pharmacol Res. 76:58–66. 2013.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Brohall G, Oden A and Fagerberg B: Carotid
artery intima-media thickness in patients with Type 2 diabetes
mellitus and impaired glucose tolerance: A systematic review.
Diabet Med. 23:609–616. 2006.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Henry RMA, Kostense PJ, Dekker JM, Nijpels
G, Heine RJ, Kamp O, Bouter LM and Stehouwer CDA: Carotid arterial
remodeling: A maladaptive phenomenon in type 2 diabetes but not in
impaired glucose metabolism: The Hoorn study. Stroke. 35:671–676.
2004.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Henry RMA, Kostense PJ, Spijkerman AMW,
Dekker JM, Nijpels G, Heine RJ, Kamp O, Westerhof N, Bouter LM and
Stehouwer CD: Hoorn Study. Arterial stiffness increases with
deteriorating glucose tolerance status. Circulation. 107:2089–2095.
2003.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Bonora E, Kiechl S, Oberhollenzer F, Egger
G, Bonadonna RC, Muggeo M and Willeit J: Impaired glucose
tolerance, Type II diabetes mellitus and carotid atherosclerosis:
Prospective results from the Bruneck Study. Diabetologia.
43:156–164. 2000.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Williams B, Mancia G, Spiering W, Agabiti
Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G,
Dominiczak A, et al: 2018 ESC/ESH Guidelines for the management of
arterial hypertension. Eur Heart J. 39:3021–3104. 2018.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Munzel T, Gori T, Bruno RM and Taddei S:
Is oxidative stress a therapeutic target in cardiovascular disease?
Eur Heart J. 31:2741–2748. 2010.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Tabas I and Bornfeldt KE: Macrophage
phenotype and function in different stages of atherosclerosis. Circ
Res. 118:653–667. 2016.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Hattori Y, Jojima T, Tomizawa A, Satoh H,
Hattori S, Kasai K and Hayashi T: A glucagon-like peptide-1 (GLP-1)
analogue, liraglutide, upregulates nitric oxide production and
exerts anti-inflammatory action in endothelial cells. Diabetologia.
53:2256–2263. 2010.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Shiraki A, Oyama J, Komoda H, Asaka M,
Komatsu A, Sakuma M, Kodama K, Sakamoto Y, Kotooka N, Hirase T and
Node K: The glucagon-like peptide 1 analog liraglutide reduces
TNF-α-induced oxidative stress and inflammation in endothelial
cells. Atherosclerosis. 221:375–382. 2012.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Zhang L, Tian J, Diao S, Zhang G, Xiao M
and Chang D: GLP-1 receptor agonist liraglutide protects
cardiomyocytes from IL-1β-induced metabolic disturbance and
mitochondrial dysfunction. Chem Biol Interact.
332(109252)2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Chow BS, Koulis C, Krishnaswamy P,
Steckelings UM, Unger T, Cooper ME, Jandeleit-Dahm KA and Allen TJ:
The angiotensin II type 2 receptor agonist Compound 21 is
protective in experimental diabetes-associated atherosclerosis.
Diabetologia. 59:1778–1790. 2016.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Yeboah J, Young R, McClelland RL, Delaney
JC, Polonsky TS, Dawood FZ, Blaha MJ, Miedema MD, Sibley CT, Carr
JJ, et al: Utility of nontraditional risk markers in
atherosclerotic cardiovascular disease risk assessment. J Am Coll
Cardiol. 67:139–147. 2016.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Aatola H, Hutri-Kahonen N, Juonala M,
Viikari JS, Hulkkonen J, Laitinen T, Taittonen L, Lehtimaki T,
Raitakari OT and Kahonen M: Lifetime risk factors and arterial
pulse wave velocity in adulthood: the cardiovascular risk in young
Finns study. Hypertension. 55:806–811. 2010.PubMed/NCBI View Article : Google Scholar
|