Introduction
Visceral artery aneurysms are defined in this
retrospective analysis as a true aneurysm in the celiac trunk (CT),
superior mesenteric artery (SMA), inferior mesenteric artery,
and/or their branches. Visceral artery aneurysms (VAAs) are rare
and mostly asymptomatic., Rapid growth, size >2 cm, and
pregnancy are risk factors associated with rupture. True visceral
aneurysms are aneurysms are the result of weakening and thinning of
the artery wall. Atherosclerosis, connective tissue disorders,
infection (for example pancreatitis) and abdominal surgery are
known risk factors for the development of VAA. Nowadays,
conservative therapy, endovascular, and open surgery are the
treatment options for patients with visceral aneurysms (VAA).
During the last decade, endovascular repair of VAAs has been
increasingly used (1-6).
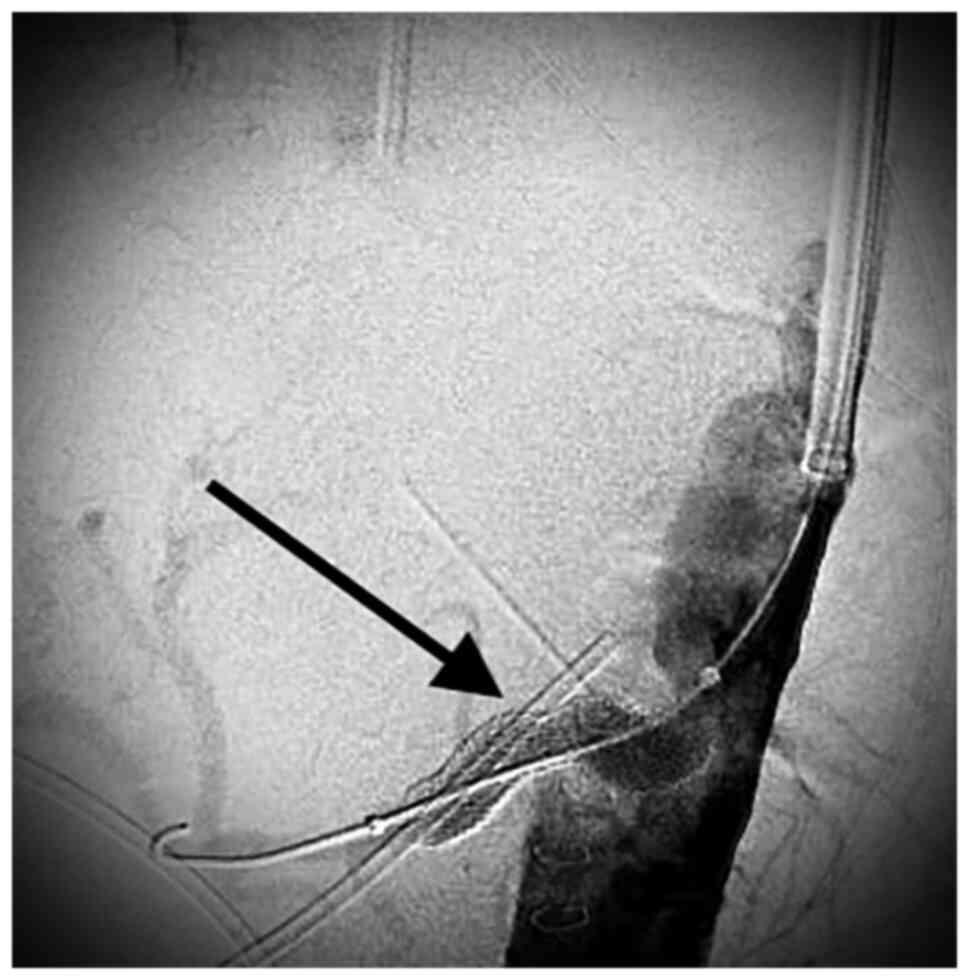
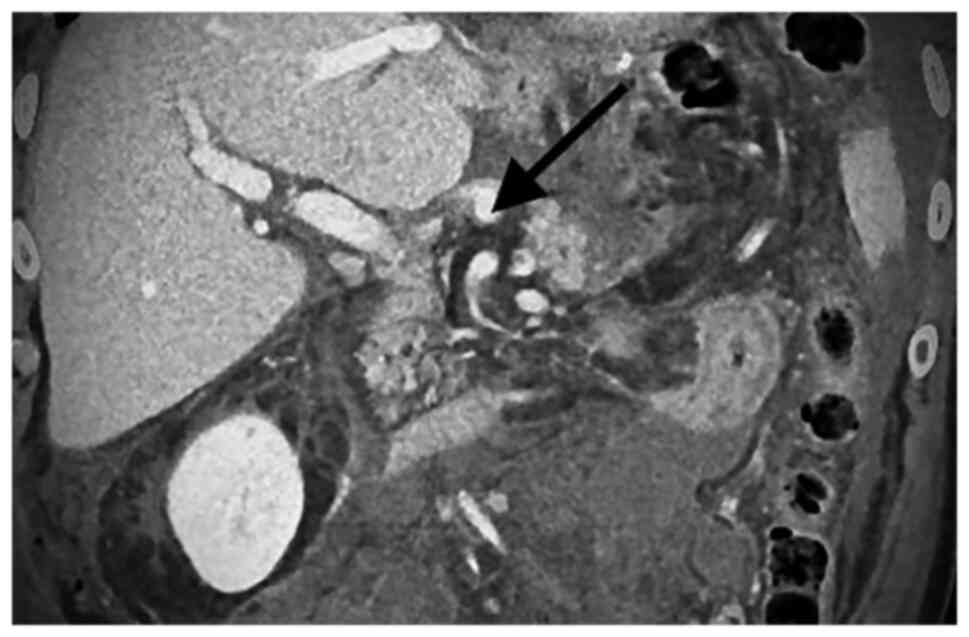
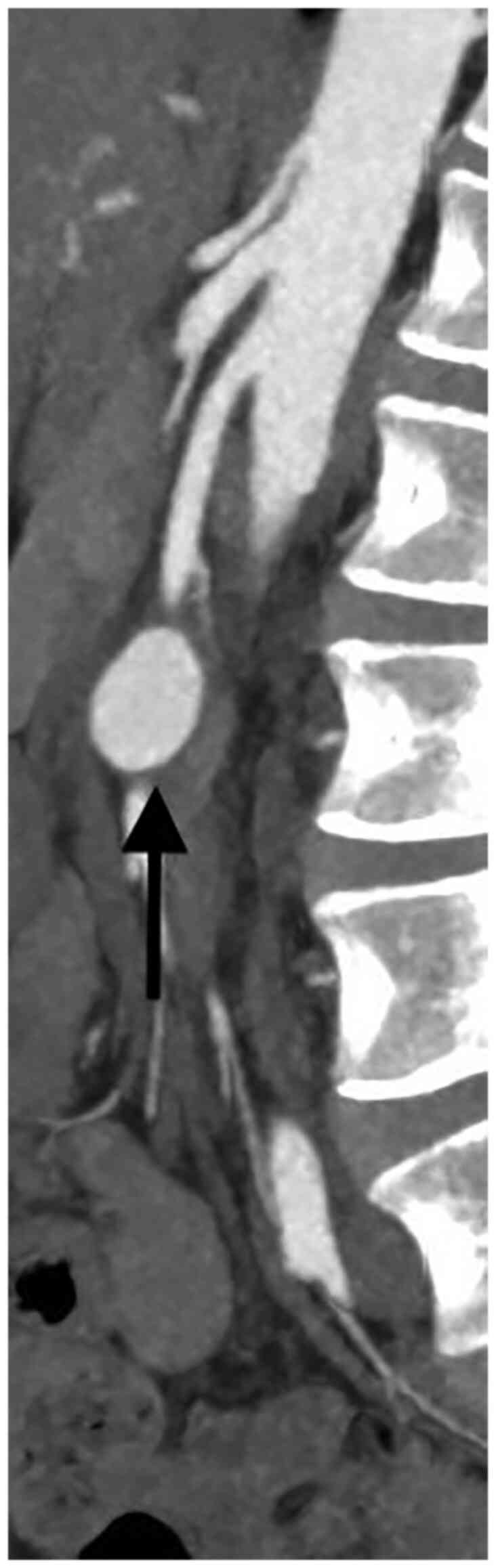
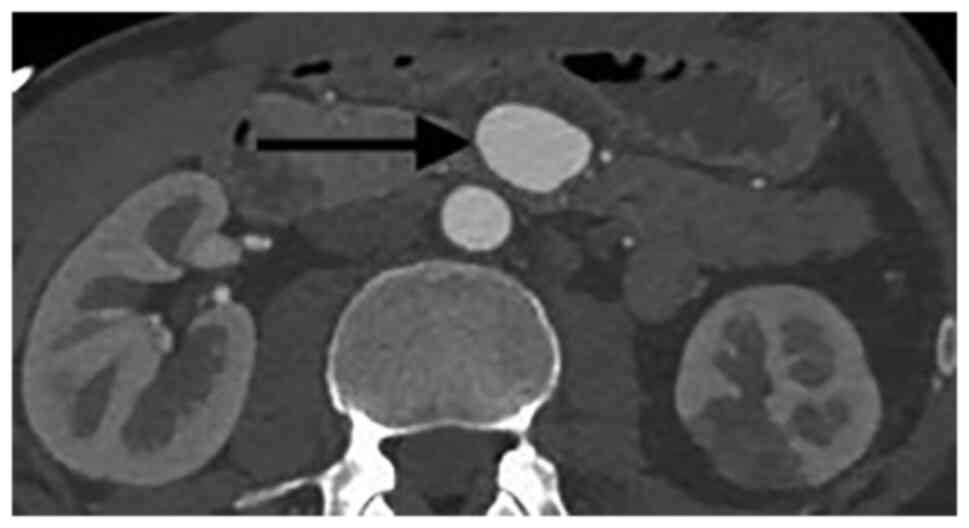
Catheter-based embolization or stent-graft placement are two major
treatment options. Most VAAs originate from the splenic artery (SA)
(60%) (Figs. 1 and 2), followed by the hepatic artery (HA)
(20-50%) (Figs. 3 and 4). An origin from the superior mesenteric
artery (SMA) (6%) (Figs. 5 and
6), the celiac trunk (CT) (4%) or
other, smaller visceral arteries is considerably less common
(7).
Mostly, VAAs are asymptomatic and incidental
findings owing to the evolving and more frequently used imaging
modalities. Risk factors associated with rupture are pancreatitis,
rapid growth, size >2 cm, and pregnancy. The mortality
associated with splenic artery aneurysm rupture has been reported
at around 30%. In pregnancy, these rates are higher. Higher flow
rate through the splenic artery because of distal compression of
the aorta and iliac arteries by the pregnant uterus, portal
congestion, and the progressive weakening of the basic structure of
the arterial media are possible factors that explain this high
mortality (8-16).
The aim of the present study is to compare the
outcomes of patients undergoing open surgery (OS) or endovascular
repair (ER) for the treatment of VAAs. We present our single center
experience on the treatment of VAAs, reporting on 12 patients.
Patiends and methods
All patients 18 years or older at the time of
surgery who were treated for VAAs and underwent endovascular or
open surgery at the Department of Visceral, Vascular and Endocrine
Surgery at the University Hospital Halle (Saale), Germany from 2014
to 2022 were included in the study. The STROBE statement (a
checklist of items that should be addressed in articles reporting
on the three main study designs of analytical epidemiology: cohort,
case-control, and cross-sectional studies) was followed for
reporting on observational data (17).
Anastomotic pseudoaneurysms and aortic aneurysms
involving the visceral arteries were excluded. The decision to
perform an open or endovascular repair was made after discussion in
a multidisciplinary meeting (angiology, radiology and vascular
surgery). All ruptured VAAs underwent intervention. Open repair was
performed in general anesthesia as an aneurysmorrhaphy with or
without vascular reconstruction by (direct end-to- end anastomosis
or using a vein graft interposition). Endovascular treatment was
performed in local anesthesia and consisted either of
coilembolization or covered stent placement. If a stent graft
placement was technically possible it was performed in order to
maintain the vessel patency. If not, a coilembolization was
performed.
Data was extracted and presented in a tabular
fashion. The following descriptive patient and operation
characteristics were documented: sex, age at diagnosis, use of
diagnostic imaging techniques, aneurysm localization, aneurysm size
and symptoms and therapy. The following predefined outcomes were
also extracted: in-hospital mortality, major morbidity (when
defined as Dindo-Clavien >III) (18), length of hospital stay and
technical success (complete aneurysm occlusion in the postoperative
CT-Scan). The Clavien Dindo Classification was used to rank the
severity of surgical complications. This classification consists in
a scale of several grades (Grade I, II, IIIa, IIIb, IV and V).
Grade I complications consists in any deviation from the normal
postoperative course without the need for pharmacological treatment
or surgical, endoscopic, and radiological interventions. Grade II
include complications requiring pharmacological treatment. Grade
III refers to complications requiring surgical, endoscopic or
radiological intervention (IIIa not under general anesthesia and
IIIb under anesthesia). Grade IV regards life-threneting
complications and Grade V represents the death of the patient
(18). Descriptive statistics from
our patient collective are reported as numbers or mean.
Results
From 2014 to 2022, 12 patients with VAAs, 11 females
and one male were treated at the University Hospital Halle
(Saale).
The median age was 59 years (range 40 to 87 years).
Only one patient was male, and all were diagnosed by a CT-scan. The
detailed patient and operative characteristics are given in
Tables I and II.
 | Table IPatients and preoperative
characteristics. |
Table I
Patients and preoperative
characteristics.
| No. | Sex | Age | Year | Imaging | Location | Size, cm | Symptoms related to
the aneurysm | Atherosclerosis | Connective tissue
disorders | Infection | Previous abdominal
surgery | Diabetes Mellitus
Type II | Smoker |
|---|
| 1 | F | 50 | 2019 | CTA | SA | 2.5 | N | N | N | N | N | N | N |
| 2 | F | 69 | 2017 | CTA | SA | 2 | N | N | N | N | N | Y | N |
| 3 | F | 61 | 2014 | CTA | SMA | 5 | N | Y | N | N | Y | N | N |
| 4 | F | 33 | 2021 | CTA | SMA | 2, 5 | N | N | Y | N | N | N | Y |
| 5 | F | 52 | 2020 | CTA | SA | 2 | N | N | N | N | N | N | N |
| 6 | F | 74 | 2021 | CTA | SA | 3.5 | N | N | N | N | N | N | N |
| 7 | M | 67 | 2020 | CTA | HA | 1.5 | Bleeding | N | N | Y | Y | Y | N |
| 8 | F | 64 | 2022 | CTA | CT | 2 | N | Y | N | N | N | N | Y |
| 9 | F | 54 | 2021 | CTA | SA | 2.2 | N | N | N | N | N | N | N |
| 10 | F | 57 | 2021 | CTA | SA | 1.5 | N | N | N | N | N | N | N |
| 11 | F | 53 | 2021 | CTA | SA | 2 | N | N | N | N | N | N | N |
| 12 | F | 87 | 2022 | CTA | SA | 2 | N | N | N | N | N | N | N |
 | Table IISurgical characteristics and
postoperative outcomes. |
Table II
Surgical characteristics and
postoperative outcomes.
| No. | Therapy | Implants | Morbidity
(Dindo-Clavien) | In-Hospital
Mortality | Duration of
postoperative stay (Days) |
|---|
| 1 | OS; aneurysm
resection, direct suture | - | 0 | N | 6 |
| 2 | OS; aneurysm
resection, direct suture | - | 0 | N | 4 |
| 3 | OS; aneurysm
Resection, Vein graft | - | 0 | N | 19 |
| 4 | OS; aneurysm
resection, direct suture | - | 0 | N | 8 |
| 5 | ER; covered
stentgraft | Viabahn 5x50
mm | 0 | N | 1 |
| 6 | ER; covered
stentgraft | Viabahn 8x57
mm | 0 | N | 3 |
| 7 | ER; two covered
stentgrafts | Gore Viabahn 5x50
mm and Bentley Begraft 6x18 mm | 0 | N | 7 |
| 8 | ER; covered
stentgraft | Bentley Begraft
6x27 mm | 0 | N | 3 |
| 9 | ER; covered
stentgraft | Bentley Begraft
6x37 mm | 0 | N | 4 |
| 10 | ER; covered
stentgraft | Bentley Begraft
6x27 mm | 0 | N | 3 |
| 11 | ER; covered
stentgraft | Viabahn 5x50
mm | 0 | N | 2 |
| 12 | ER; coiling | Platinum
embolization coils | 0 | N | 5 |
There were eight patients with an aneurysm of the
SA, two patients with aneurysms of the SMA, one patient with an
aneurysm of the HA and one patient with an aneurysm of the CT. Only
one patient was symptomatic and presented with signs of bleeding.
All patients received a contrast-enhanced CT-scan.
The median aneurysm diameter was 2 cm (range 1.5 cm
to 5 cm) for all aneurysms, 3.75 cm for aneurysms of the SMA, 2 cm
for aneurysms of the SA and for aneurysms of the CT and 1.5 for the
aneurysm of the HA.
Six aneurysms of SA, one aneurysm of the CT and one
aneurysm of the HA were treated with ER (eight patients). Seven
patients were treated with covered stents and one with coiling
embolization. In total eight covered stents were implanted. Two
patients with SA aneurysms and two patients with SMA aneurysms
underwent OS. No allogeneic grafts were required. Three patients
needed direct suture only and one a vein graft.
There was no in-hospital mortality and no major
postoperative complications (Clavien-Dindo grade ≥3). Technical
success was achieved in all patients. The median postoperative stay
was four days for all procedures and significantly longer after OS
when compared with ER (seven days vs. three days).
Discussion
In this retrospective study we reported on our
single center experience on the treatment of VAAs, both with
endovascular and open surgery.
In our small patient collective, no mortality was
observed. This may be due to the almost total absence of emergency
repairs. Considerable mortality is described in the treatment of
these patients in an emergency setting (19). In a retrospective study reporting
on 185 aneurysms, 46% of the patients were symptomatic with
bleeding or rupture. Despite 98% technical success on treating
symptomatic patients, 30-day overall and aneurysm-related mortality
was 6.2 and 3.4%, respectively. On the other hand, no deaths were
observed in patients undergoing elective treatment (20). In another report of 217 splenic
artery aneurysms, operative mortality was 5% in the elective group
and 20% in the emergency group (8). In another study an operative
mortality rate of 37.5% for ruptured superior mesenteric artery
aneurysms was described. Also in this study, no mortality was
observed for elective repair (21). In another large retrospective
study, morbidity (19% vs. 4%; P=.003), 30-day mortality (13% vs. 0%
P=0.001), 1-year (32.5% vs. 4.1%, P<.001), and 3-year mortality
rates (36.4% vs. 8.3%; P<.001) were significantly higher for
ruptured aneurysms than for intact aneurysms. Open surgery had
higher 30-day mortality rates thanendovascular repair (28% vs. 7%;
P= .06) (22). In our
retrospective patient cohort, length of stay was shorter in the ER
group (mean difference -4.25 days, 95% CI [-5.52; -2.98],
P<0.00001; seven vs. four days). Comparable results regarding
the length of stay were reported in a previous meta-analysis
(23). The technical success of
100% when using endovascular stentgrafts or coiling observed in our
patient collective may reflect the bias inherent in the analysis of
a very small patient collective. In a systematic review and
meta-analysis from 2016 comprising 22 studies reporting on
endovascular treatment of VAAs, a 93.2% technical success rate was
reported (24).
This study has limitations. The main limitation is
that it is exclusively based on retrospective data, which could
represent a problem in terms of selection bias. The long inclusion
period does not necessarily reflect contemporary surgical and
endovascular techniques. Another limitation is the small number of
patients. The STROBE guidelines were followed to ensure
transparency and standardized reporting. Nevertheless, the findings
of this work may provide useful information, as it reports a case
series of a rare disease with outcomes on open and endovascular
treatment.
In conclusion, evidence from this retrospective
small case series shows no mortality and a shorter length of stay
for patients undergoing ER for the treatment of VAA. Although the
results are in line with the fact that ER is nowadays considered
the first line treatment for VAA, they may be prone to selection
bias.
Acknowledgements
Not applicable.
Funding
Funding: This work was partially supported by the Advanced
Clinician Scientist Program of the Medical Faculty of the
Martin-Luther University Halle-Wittenberg, Halle (Saale), Germany
(grant no. FKZ ACS23/06).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AR outlined, wrote and drafted the manuscript. AR,
UR, JP, JK, EJ and JU performed analysis or interpretation of data
for the work. All authors critically revised the manuscript and
read and approved the final version of the manuscript. All authors
agree to be accountable for all aspects of the work in ensuring
that questions related to the accuracy or integrity of any part of
the work are appropriately investigated and resolved. AR and JP
confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
A fully anonymized retrospective evaluation of the
study data was conducted, and so the need for an ethical vote and
patient consent was waived, according to section 17 of the Hospital
Act of the Federal State of Saxony-Anhalt and section 15 of the
Saxony-Anhalt Medical Association's professional code of
conduct.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests
References
|
1
|
Iida A, Katayama K and Yamaguchi A:
Laparoscopic resection for splenic artery aneurysm using the
lateral approach: Report of two cases. Asian J Endosc Surg.
6:147–150. 2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kim Y and Johna S: Laparoscopic excision
of splenic artery aneurysm. JSLS. 17:132–134. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Pietrabissa A, Ferrari M, Berchiolli R,
Morelli L, Pugliese L, Ferrari V and Mosca F: Laparoscopic
treatment of splenic artery aneurysms. J Vasc Surg. 50:275–279.
2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tiberio GA, Bonardelli S, Gheza F, Arru L,
Cervi E and Giulini SM: Prospective randomized comparison of open
versus laparoscopic management of splenic artery aneurysms: A
10-year study. Surg Endosc: Jun 30, 2012 (Epub ahead of print).
|
|
5
|
Balderi A, Antonietti A, Ferro L, Peano E,
Pedrazzini F, Fonio P and Grosso M: Trattamento endovascolare di
aneurismi e pseudoaneurismi viscerali: la nostra esperienza.
Radiologia Medica. 117:815–830. 2012.
|
|
6
|
Cappucci M, Zarco F, Orgera G, López-Rueda
A, Moreno J, Laurino F, Barnes D, Tipaldi MA, Gomez F, Macho
Fernandez J and Rossi M: Endovascular treatment of visceral artery
aneurysms and pseudoaneurysms with stent-graft: Analysis of
immediate and long-term results. Cir Esp. 95:283–292.
2017.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
7
|
Meyer A, Uder M, Lang W and Croner R:
Visceral artery aneurysms. Zentralbl Chir. 135:416–420.
2010.PubMed/NCBI View Article : Google Scholar : (Article in
German).
|
|
8
|
Abbas MA, Stone WM, Fowl RJ, Gloviczki P,
Oldenburg WA, Pairolero PC, Hallett JW, Bower TC, Panneton JM and
Cherry KJ: Splenic artery aneurysms: Two decades experience at mayo
clinic. Ann Vasc Surg. 16:442–449. 2002.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Tulsyan N, Kashyap VS, Greenberg RK, Sarac
TP, Clair DG, Pierce G and Ouriel K: The endovascular management of
visceral artery aneurysms and pseudoaneurysms. J Vasc Surg.
45:276–283. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Herbeck M, Horbach T, Putzenlechner C,
Klein P and Lang W: Ruptured splenic artery aneurysm during
pregnancy: A rare case report with both maternal and fetal
survival. Am J Obstet Gynecol. 181:763–764. 1999.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Barrett JM, Van Hooydonk JE and Boehm FH:
Pregnancy related rupture of arterial aneurysms. Obstet Gynecol
Surv. 37:557–566. 1982.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Trastek VF, Pairolero PC and Bernatz PE:
Splenic artery aneurysms. World J Surg. 9:378–383. 1985.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lee PC, Rhee RY, Gordon RY, Fung JJ and
Webster MW: Management of splenic artery aneurysms: The
significance of portal and essential hypertension. J Am Coll Surg.
5:483–490. 1999.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Berceli SA: Hepatic and splenic artery
aneurysms. Semin Vasc Surg. 18:196–201. 2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Moore SW, Guida PM and Schumacher HW:
Splénic artery aneurysm. Bull Soc Int Chir. 29:210–218.
1970.PubMed/NCBI
|
|
16
|
Nanez L, Knowles M, Modrall JG and
Valentine RJ: Ruptured splenic artery aneurysms are exceedingly
rare in pregnant women. J Vasc Surg. 60:1520–1523. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
von Elm E, Altman DG, Egger M, Pocock SJ,
Gøtzsche PC, Vandenbroucke JP and STROBE Initiative: The
strengthening the reporting of observational studies in
epidemiology (STROBE) statement: Guidelines for reporting
observational studies. J Clin Epidemiol. 61:344–349.
2008.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Dindo D, Demartines N and Clavien PA:
Classification of surgical complications: A new proposal with
evaluation in a cohort of 6336 patients and results of a survey.
Ann Surg. 240:205–213. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Roberts KJ, McCulloch N, Forde C, Mahon B,
Mangat K, Olliff SP and Jones RG: Emergency treatment of
haemorrhaging coeliac or mesenteric artery aneurysms and
pseudoaneurysms in the era of endovascular management. Eur J Vasc
Endovasc Surg. 49:382–389. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fankhauser GT, Stone WM, Naidu SG, Oderich
GS, Ricotta JJ, Bjarnason H and Money SR: Mayo Vascular Research
Center Consortium. The minimally invasive management of visceral
artery aneurysms and pseudoaneurysms. J Vasc Surg. 53:966–970.
2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Stone WM, Abbas M, Cherry KJ, Fowl RJ and
Gloviczki P: Superior mesenteric artery aneurysms: Is presence an
indication for intervention? J Vasc Surg. 36:234–237; discussion
237. 2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Shukla AJ, Eid R, Fish L, Avgerinos E,
Marone L, Makaroun M and Chaer RA: Contemporary outcomes of intact
and ruptured visceral artery aneurysms. J Vasc Surg. 61:1442–1447.
2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Barrionuevo P, Malas MB, Nejim B, Haddad
A, Morrow A, Ponce O, Hasan B, Seisa M, Chaer R and Murad MH: A
systematic review and meta-analysis of the management of visceral
artery aneurysms. J Vasc Surg. 72:40S–45S. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kok HK, Asadi H, Sheehan M, Given MF and
Lee MJ: Systematic review and single-center experience for
endovascular management of visceral and renal artery aneurysms. J
Vasc Interv Radiol. 27:1630–1641. 2016.PubMed/NCBI View Article : Google Scholar
|