Introduction
Fetus in fetu (FIF) is a very rare congenital
anomaly where a malformed fetus is enclosed within the body of a
twin fetus, with an incidence of 1 in 500,000 live births (1). FIF mainly occurs in the
retroperitoneal region but has also been reported in other
locations, such as the cranial cavity and the scrotum (2). The FIF has the same blood type, sex
chromosome, protein polymorphism and DNA as the host fetus
(3). The exact pathogenesis of FIF
remains to be elucidated. One hypothesis suggests that FIF arises
from an abnormal division of monochorionic monozygotic twins during
early embryogenesis (3). Another
hypothesis suggests that FIF and teratoma are two related
congenital manifestations with the same pathogenesis (4).
Imaging modalities, including ultrasonography (US)
and magnetic resonance imaging (MRI), have an important role in the
early diagnosis and management of FIF. Since US is the most common
choice/imaging in the prenatal examination, obstetricians must
become familiar with the ultrasound findings suggestive of FIF. The
present study reported a single case of a retroperitoneal FIF
diagnosed by prenatal US.
Case presentation
A 45-year-old woman (gravida 2, para 1) was admitted
at 37+4 gestational weeks to the Ultrasonography
Department of Huidong People's Hospital, the People's Government of
Liangshan Yi Autonomous Prefecture, Sichuan, with an obstetric US
diagnosis of a teratoma. The initial US at 37+3 weeks of
gestation showed a fetal-like echo in the thoracic cavity of the
fetus. After admission, a repeat ultrasound examination revealed a
live third-trimester singleton fetus in a cephalic presentation
with a retroperitoneal mass of mixed echogenicity. One fetus had a
weak heartbeat and the other was acardiac. The woman and her
husband were both healthy. Her first child had no congenital
abnormalities; the husband was not the father of her first child.
There was no history of twin gestation or newborns with
deformities.
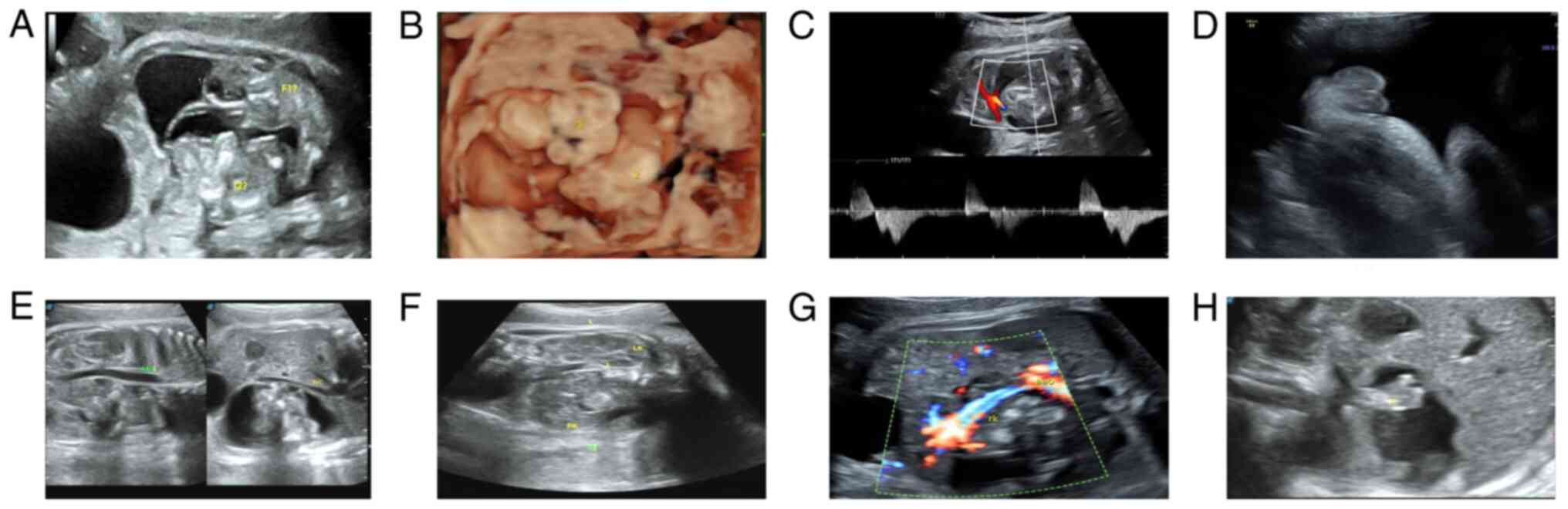
Obstetric US revealed a mixed cystic-solid mass at
the right retroperitoneal space of the host fetus. There were two
parallel fetal-like signals in the upper and lower ends of the
mass. The fetal-like echoes were parallel to the sagittal plane of
the fetal spine (Fig. 1A and
B) and closer to the ventral side
of the host fetus. The fetal-like tissue, 4.7x2.1 cm in size,
showed mixed echogenicity and intra-cyst septation that closely
adhered to the cyst wall. Furthermore, multi-sectional and
multimodal scanning of the fetal-like tissue showed an irregular
morphology and outline, with no fetal head, spine, upper limb, or
heart echoes. The abdominal and thoracic cavities were not
distinguishable. However, continuous sagittal and transverse
scanning showed that one limb was continuous. The limb was covered
with skin and had a long bone, a distal footpad and toe-like
echoes, with a stiff morphology (Fig.
1C and D). In addition, an
umbilical cord-like vascular echo was also found connected to the
fetal-like mass, but no blood flow signal was found by color
Doppler scan. At its rear side, another fetal sonogram with a size
of about 3.9x2.1 cm could be seen. Multi-sectional and multimodal
scanning showed the following: Irregular shape and contour, no
fetal head, spine, or upper limb; the thorax and abdominal cavity
could not be distinguished. However, continuous sagittal and
transverse sections revealed the buttock-like contour at the
posterior part of the body; the fetal limb was seen at the far end,
similar to femoral echo; plantar echo was seen at the far end; long
bone echo was seen in the proximal limb and the limb was covered
with skin. A faint fetal heartbeat was seen in the chest cavity.
Color doppler flow image showed blood flow signal. Pulsed wave
Doppler showed a positive and negative two-way arterial spectrum.
The fetal movement was continuously observed. The FIF compressed
the host fetus's inferior vena cava and abdominal aorta, which
showed arch-shaped shifting. The intestine of the host fetus was
also compressed and shifted to the left; the right kidney was
compressed and displaced into the pelvic cavity. The blood flow to
the two kidneys of the FIF was from the abdominal aorta of the host
fetus (Fig. 1E-H). Finally, an
ultrasound diagnosis of a retroperitoneal FIF was made (Video S1 and S2).
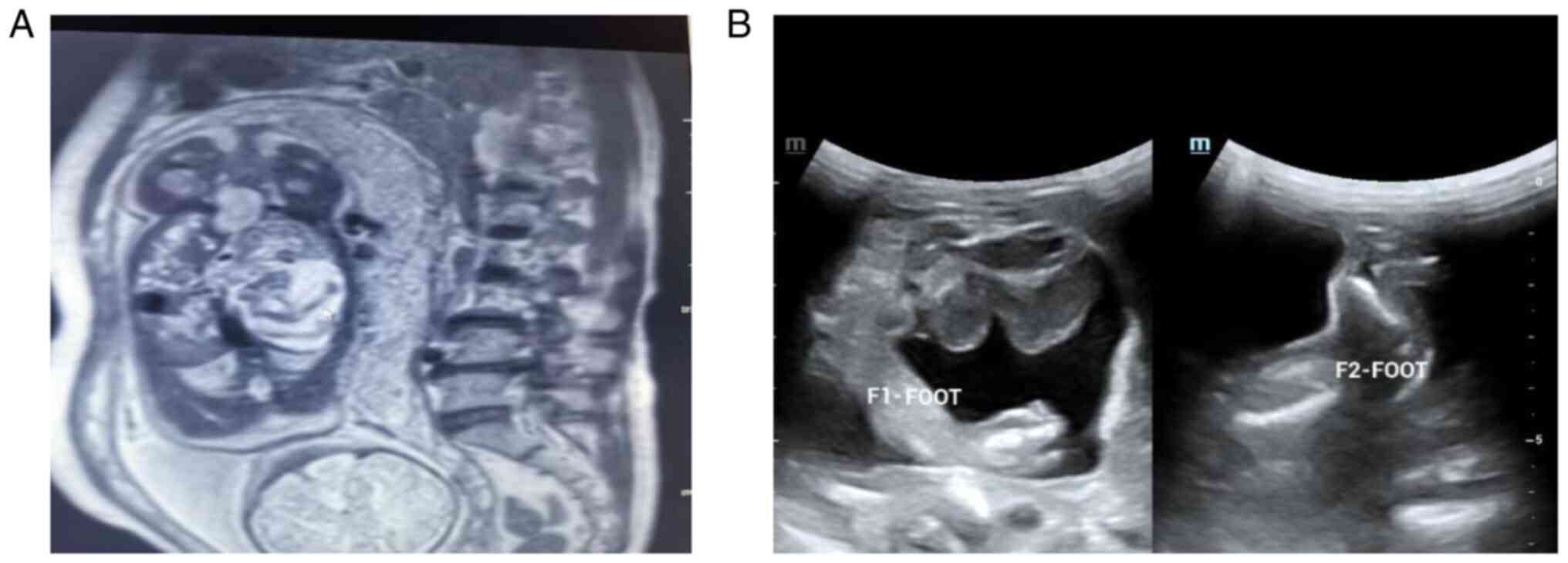
An abdominopelvic MRI at 37+5 weeks of
gestation showed a cystic space-occupying lesion at the right
epigastric region of the fetus, suggesting a FIF with developmental
deformity (Fig. 2A). The US
performed on the newborn suggested a retroperitoneal twin FIF
(Fig. 2B). A computed tomography
examination in the newborn showed a gigantic space-occupying lesion
at the right retroperitoneal region containing adipose tissue, long
bone and axial skeleton-like structures, which wrapped the right
renal artery and vein and compressed the pancreas, liver, intestine
and surrounding blood vessels. The findings highly suggested
FIF.
At 20 days after the child's birth, the patient was
admitted to the Department of critical care medicine of West China
Hospital of Sichuan University. He was diagnosed with FIF and
underwent surgery on December 21, 2021. During the operation, a
15x13x14 cm mass was resected from the retroperitoneum and the
final diagnosis was of a right retroperitoneal giant tumor
(teratoma) following the surgery.
Pathological examination revealed a mass with a
bunch of hand- and foot-shaped teratoma-like masses on gross
inspection, with an approximate overall size of 13.5x7.8x4.6 cm;
microscopy showed immature teratoma-like characteristics.
At the time of writing, the child is 1 year and 8
months old, 80 cm tall and 10 kg in weight and in good health.
Discussion
The present study presented a case of
retroperitoneal FIF in a live intrauterine fetus diagnosed by US at
37 weeks of gestation. One fetus had weak cardiac activity, while
the other had no heartbeat. The FIF fed on the host blood supply
and compressed adjacent organs. This case represents a prenatal
diagnosis of FIF, demonstrating the critical role of the US in FIF
diagnosis.
FIF can be single or multiple (5) and while most FIFs reported in the
literature showed no cardiac activity, the present case had FIF in
which one was acardiac and the other demonstrated weak cardiac
activity and visible fetal motion. The FIF had limbs, digital pads
and skin. Doppler scan showed that renal blood flow of the live FIF
originated from the host's abdominal aorta. A recent study also
reported a viable FIF with recognizable cardiac chambers using a
prenatal Doppler ultrasound (6).
US has an important role in diagnosing FIF,
particularly during prenatal life. The key to diagnosing FIF in
utero is detecting fetal structure formation in the host fetus.
Moreover, Spencer et al (3)
suggest looking for certain characteristics in the mass of the host
fetus to increase suspicion of FIF. Identifying these
characteristics in the prenatal US would assist in early diagnosis
and informed decision-making. Consequently, the case in the present
report demonstrated ultrasound characteristics similar to previous
reports (6-8),
including a retroperitoneal cystic-solid mass with a thin wall
(representing the amniotic membrane) and clear boundaries; the
solid components enlarged with gestational age, gradually showing
fetal morphology surrounded by echo-free region (representing the
amniotic fluid). Additionally, the mass contained an umbilical
cord-like vascular pedicle in which a Doppler scan revealed a
parallel artery and vein connected to the host fetus's artery and
vein, respectively. Finally, the mass compressed the surrounding
tissues of the host fetus without infiltration.
Some important clinical entities need to be
distinguished from FIF. Teratoma is the most common differential
diagnosis of FIF (9). However,
teratoma is sporadic bone mass or calcification without vertebral
bones, limbs, or viscera. Neuroblastoma is another congenital
anomaly that may resemble FIF but is primarily characterized by a
solid mass with no bones or other viscera. Last, meconium
peritonitis can manifest as an abdominal mass devoid of fetal-like
structures.
In conclusion, when cystic and solid masses are
found in ultrasound examination during pregnancy, especially in the
middle axis of the fetus, the diagnosis of an endoparasitic fetus
should be considered and it should be carefully observed whether
the mass contains the spinal axis, long bone, or organ structure.
In addition, prenatal ultrasound diagnosis based on the spinal
axis, long bone structure, skin and vascular pedicle has a high
coincidence rate. Otherwise, teratoma should be considered.
Supplementary Material
37 week pregnant women prenatal
ultrasound examination.
Postnatal ultrasound examination.
Supplementary Data
Supplementary Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
The conception of the present study was by WTP, who
was also responsible for methodology. WTP and SQZ were responsible
for validation. WTP and MD preformed formal analysis. WTP and MD
were responsible for resources. WTP and SQZ were responsible for
data curation. WTP and MD wrote the original draft of the
manuscript and WTP and SQZ reviewed and edited the manuscript. WTP
supervised the present study. WTP was also responsible for project
administration. WTP and SQZ confirm the authenticity of all the raw
data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was a simple single case with no
patient-identifiable information and therefore did not require
ethical approval.
Patient consent for publication
At the time of writing, as the patient is a minor,
the present study obtained the informed consent of the parents of
the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hoeffel CC, Nguyen KQ, Phan HT, Truong NH,
Nguyen TS, Tran TT and Fornes P: Fetus in fetu: A case report and
literature review. Pediatrics. 105:1335–1344. 2000.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lu T, Ma J and Yang X: A rare case of
fetus in fetu in the sacrococcygeal region: CT and MRI findings.
BMC Pediatr. 21(575)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Spencer R: Parasitic conjoined twins:
External, internal (fetuses in fetu and teratomas) and detached
(acardiacs). Clin Anat. 14:428–444. 2001.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Basu A, Jagdish S, Iyengar KR and Basu D:
Fetus in fetu or differentiated teratomas? Indian J Pathol
Microbiol. 49:563–565. 2006.PubMed/NCBI
|
|
5
|
Gerber RE, Kamaya A, Miller SS, Madan A,
Cronin DM, Dwyer B, Chueh J, Conner KE and Barth RA: Fetus in fetu:
11 fetoid forms in a single fetus: Review of the literature and
imaging. J Ultrasound Med. 27:1381–1387. 2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wang L, Long B, Zhou Q and Zeng S:
Prenatal diagnosis of a ‘living’ oropharyngeal fetus in fetu: A
case report. BMC Pregnancy Childbirth. 19(453)2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Xia B, Li DD, Wei HX, Zhang XX, Li RM and
Chen J: Retroperitoneal parasitic fetus: A case report. World J
Clin Cases. 9:11482–11486. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ruffo G, Di Meglio L, Di Meglio L, Sica C,
Resta A and Cicatiello R: Fetus-in-fetu: Two case reports. J Matern
Fetal Neonatal Med. 32:2812–2819. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mohta A and Khurana N: Fetus-in-fetu or
well-differentiated teratoma- a continued controversy. Indian J
Surg. 73:372–374. 2011.PubMed/NCBI View Article : Google Scholar
|