Introduction
Antibody-associated vasculitis (AAV) is a rare
autoimmune disease of unknown cause (1). The incidence of AAV among
hospitalized patients in China is 0.25%, with the North exhibiting
a higher incidence than the South (2). A review of AAV has highlighted that
it is associated with combined interaction of infection, genetics
and environmental factors, manifests with a variety of non-specific
symptoms and usually affects the respiratory and renal systems
(3). In addition, AAV is
characterized by the inflammation and destruction of small and
medium-sized blood vessels and the presence of circulating ANCA
(4). It is also distinguished by
the pathophysiological production of proteins directed against the
neutrophilic protein proteinase 3 (PR3-ANCA) or MPO-ANCA. It is
often diagnosed in middle-aged and older adults and is uncommon in
young people (5). Dysfunction of
the immune system is also speculated to be induced by AAV, for
which long-term immunosuppressive therapy is usually administered.
Notably, various infections have become the primary cause of death
when the disease activity is controlled, particularly during the
induction-remission phase of the disease (6). Moreover, infections have been
reported to be the main trigger of AAV, the main mechanisms of
which include B and T cell activation, direct endothelial injury,
immune complex-mediated vascular injury and cell-mediated type IV
hypersensitivity-responsive vascular injury (7). Furthermore, patients with AAV may be
greatly affected by adverse events associated with its treatment
during the first year of diagnosis rather than the active
vasculitis itself. Additionally, infections are the most common
cause of patient death during follow-up, particularly in
individuals undergoing immunosuppressive therapy. Notably, the
mortality rate is reported to be higher in China than in Western
countries (8,9). OMSI is a general term for potential
interstitial septic inflammation of the maxillofacial region, the
floor of the mouth and the soft tissues of the neck. The most
common causes of OMSI are odontogenic infections, dental caries,
periapical periodontitis and pericoronitis (10). However, although the combination of
AAV with OMSI is rare in clinical practice, it is important for
medical professionals to be aware of.
Antineutrophil cytoplasmic antibody
(ANCA)-associated vasculitis (AAV) is a group of autoimmune
diseases characterized by systemic small vessel inflammation and
necrosis. ANCA is an important serum marker for AAV (11). However, the etiology and
pathogenesis of AAV remain unclear, and epidemiological studies
focusing on AAV are scarce in China. The incidence rate of AAV in
other countries is also low (12).
Oral and maxillofacial space infection (OMSI) is a bacterial
infection in the subfascial space of the oral, maxillofacial and
neck regions (13). OMSI can lead
to serious and even life-threatening complications if undetected or
left untreated. OMSI has a fatality rate of between 10 and 40%
(14). In the present case report,
a rare case of AAV combined with OMSI is described. To the best of
our knowledge, this is the first case of AAV combined with OMSI to
be reported.
Case report
A 33-year-old female who presented with swelling and
pain in the left side of the mouth that had persisted for 5 days
was admitted to Baoding No. 1 Central Hospital of Hebei Medical
University (Baoding, China) in June 2022. A year previously, the
patient sought medical care due to poor appetite and fatigue, for
which the following test results were obtained: Urinary protein
(+++), occult blood (++), blood creatinine (180 µmol/l; normal
range, 34.2-75.6 µmol/l), hemoglobin (89 g/l; normal range, 110-150
g/l) and myeloperoxidase (MPO)-ANCA titer [120 relative units
(RU)/ml; normal range, 0-20 RU/ml]. At that time, a renal biopsy
was also performed which led to a diagnosis of ANCA-related small
vessel renal damage (necrotizing vasculitis). Prednisone acetate
tablets (60 mg once daily) and cyclophosphamide (50 mg twice daily)
were prescribed. The cumulative dose of cyclophosphamide reached 8
g, after which the oral administration of 0.75 g of mycophenolate
mofetil twice daily was initiated. In the following year, 5 days
prior to her admission to hospital, the patient developed oral
ulcers with swelling and pain in the oral mucosa and swelling in
the left cheek. Furthermore, 3 days prior to admission, the patient
developed a fever (39.3˚C). Subsequently, she was admitted to the
Department of Nephrology for treatment. The patient had developed a
full and rounded face. This may have been due to Cushing's syndrome
induced by treatment with high doses of prednisone. due to the high
doses of prednisone received during the previous year for Cushing's
syndrome. However, the patient's face was asymmetrical with
pronounced swelling of the left cheek, indicating the occurrence of
OMSI (Fig. 1). The physical
examination results on admission were as follows: Temperature,
38.3˚C; blood pressure, 150/80 mmHg; body weight, 58 kg; BMI, 25.7;
rounded face; swelling of the left cheek; moderate hardness when
palpated without obvious fluid fluctuation; pressure pain (+);
maximum mouth opening (MMO) approximately two transverse fingers;
intraoral examination suggestive of 38 (Lower left 8th permanent
tooth) pericoronal redness and tenderness (+); and buccal mucosal
fistula with purulent fluid effusion. The results of the laboratory
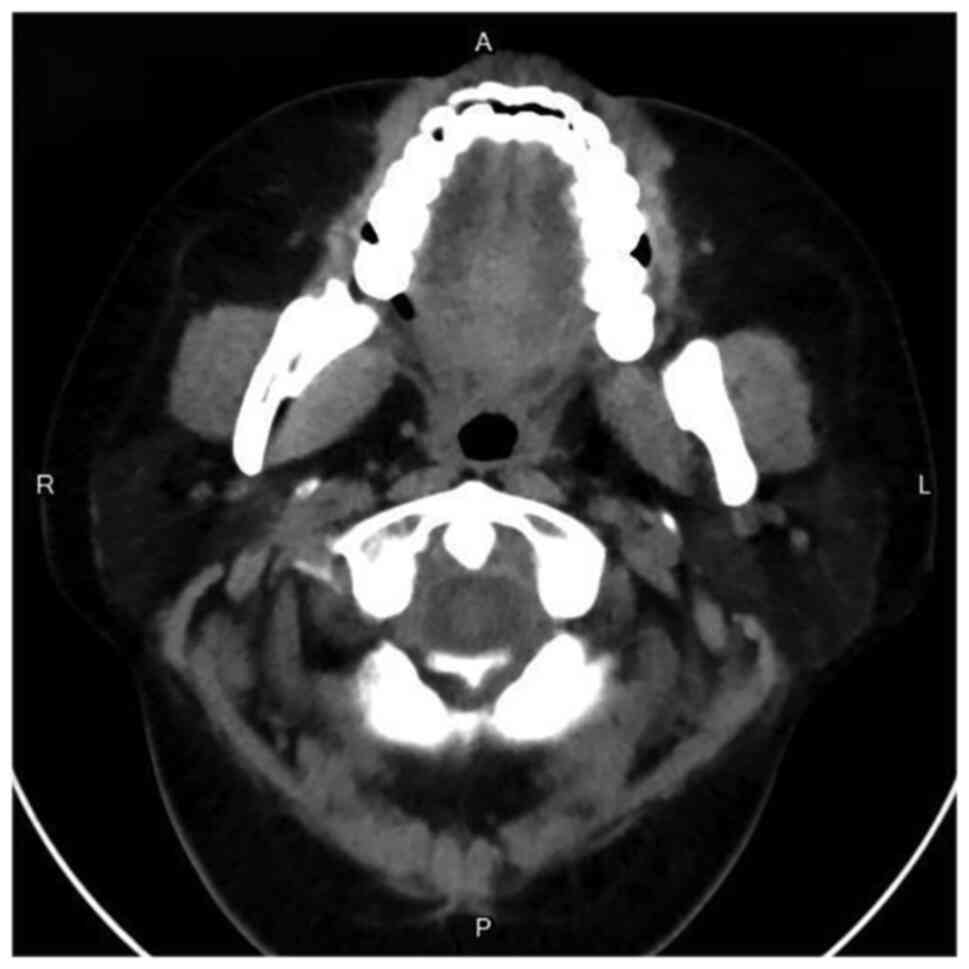
tests performed after admission are presented in Table I. Additionally, chest computed
tomography (CT) revealed no abnormalities. However, CT of the jaws
on admission showed swelling of the soft tissues around the
mandible with abnormal density on the left side, suggesting
infectious lesions and abscess formation (Fig. 2). After consultation with the
Department of Stomatology, the patient was diagnosed with OMSI
combined with abscess formation. Therefore, drainage channels were
established at two locations in the buccal mucosa for the treatment
of the patient. After repeatedly flushing with saline and diluted
hydrogen peroxide solution, yellow pus flowed out of the channels.
Thereafter, drainage strips were placed at the drainage sites and
changed daily, and the affected locations were adequately flushed
locally. On the day of admission, mycophenolate mofetil was
discontinued, and the dose of prednisone was reduced to 30 mg once
daily. In addition, intravenous antibiotic treatment was
administered, comprising oxacillin sodium 2 g twice a day and
ornidazole 0.25 g twice a day.
 | Table ILaboratory results obtained for the
patient. |
Table I
Laboratory results obtained for the
patient.
| Investigation | Normal range | Day 1 | Day 7 |
|---|
| WBC
(x109/l) | 4.00-10.00 | 10.90 | 8.50 |
| Hb (g/l) | 110.00-150.00 | 115.20 | 117.60 |
| Lymphocyte
(x109/l) | 1.20-4.80 | 0.70 | 1.23 |
| Alb (g/l) | 40.00-55.00 | 38.50 | 39.20 |
| 24-h Upro (g) | 0.00-0.15 | 0.60 | 0.40 |
| Urea (mmol/l) | 2.60-7.50 | 15.90 | 12.40 |
| Creatinine
(µmol/l) | 41.00-73.00 | 240.00 | 185.20 |
| Potassium
(mmol/l) | 3.50-5.30 | 3.80 | 4.30 |
| CRP (mg/l) | <8.00 | 129.50 | 7.20 |
| PCT (ng/ml) | <0.25 | 3.30 | 0.30 |
| MPO-ANCA (RU/ml) | <20.00 | 53.30 | 28.40 |
| PR3-ANCA (RU/ml) | <20.00 | 4.60 | 3.80 |
| C3 (g/l) | 0.79-1.52 | 0.90 | 1.30 |
| C4 (g/l) | 0.16-0.38 | 0.20 | 0.30 |
| IgA (g/l) | 1.00-4.20 | 0.45 | 0.78 |
| IgG (g/l) | 8.60-17.40 | 3.74 | 6.51 |
| IgM (g/l) | 0.50-2.80 | 0.38 | 0.46 |
Following these treatments, the left maxillofacial
swelling and pain were gradually alleviated and the temperature of
the patient returned to normal. One week later, CT imaging of the
jaw revealed marked alleviation (Fig.
3). At 1 week later, the general condition of the patient
improved and she was discharged from the hospital. The patient was
recommended to take antibiotics orally at home for 1 week (cefaclor
0.25 g twice daily). Furthermore, during an outpatient follow-up 2
weeks later, mycophenolate mofetil (0.5 g twice daily) was
prescribed. The condition of the patient remained stable during the
monthly follow-up examinations for half a year as an outpatient at
the Department of Nephrology.
Discussion
The present case report describes a young female
patient with a 1-year history of AAV. The pathological findings of
the renal biopsy performed 1 year prior to admission revealed
AAV-associated glomerular nephritis, which was treated with
long-term oral glucocorticoids and immunosuppressive drugs.
Laboratory tests on admission suggested a small amount of
proteinuria, abnormal renal function and a mildly elevated MPO-ANCA
titer. According to the Birmingham vasculitis activity scoring
system (15), the active stage of
vasculitis is defined as a score of >15 points. The score of the
present patient was 10 points, indicating that the patient did not
have active AAV. Additionally, the urine output of the patient was
also normal, suggesting that the AAV was stable. However, the
number of lymphocytes was lower than the normal range and the IgA,
IgG and IgM levels were also downregulated, indicating a poor
immune function.
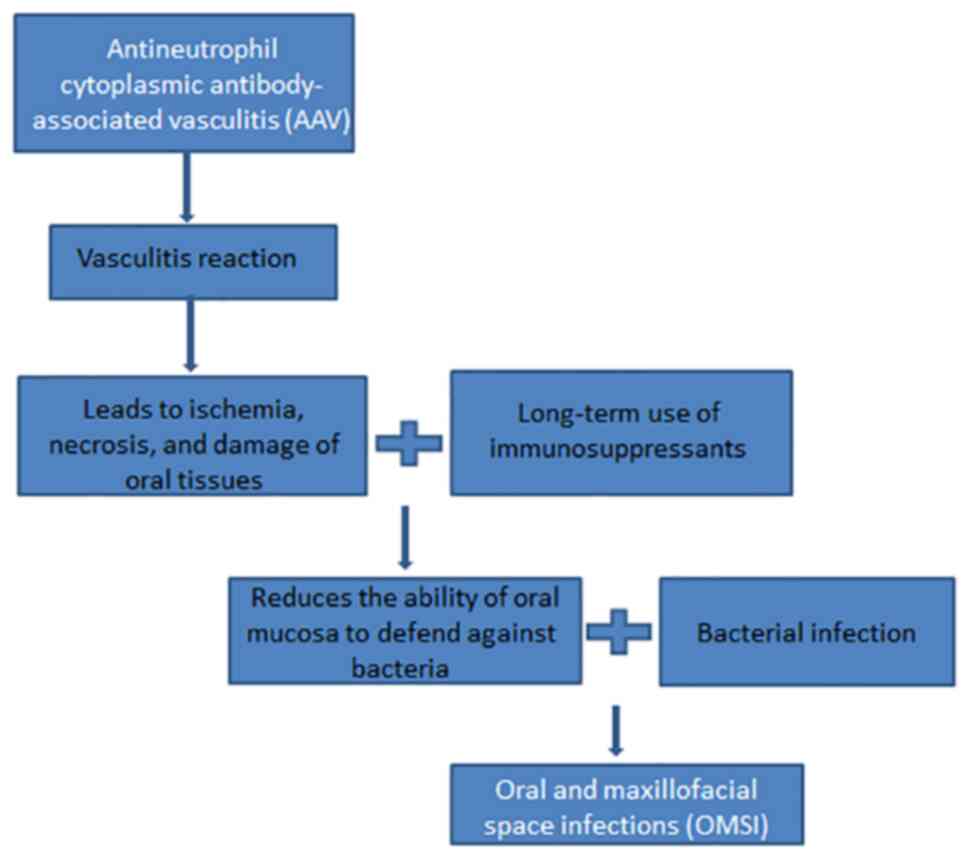
The clinical pathogenesis of AAV combined with OMSI
is relatively complex as it is often challenging to distinguish
whether it is caused by active vasculitis and/or the administration
of immunosuppressive drugs. Clinicians are required to determine
the cause based on the condition of the patient and clinical
examination findings (Fig. 4). The
patient reported in the present study presented with fever and soft
tissue swelling on the left cheek. Additionally, specialized
examination suggested that the left side of the face was more
swollen compared with the right side. In addition, the facial skin
was red in color with a high temperature, and palpable pressure was
evident in the left cheek. No dental caries or periapical infection
were observed in the oral cavity, and the bilateral lower wisdom
teeth had distal mesial gingival coverage. Moreover, CT of the jaws
indicated swelling of the soft tissues around the mandible, mainly
in the left side, suggesting infectious lesions and abscess
formation. Iwanaga et al (16) injected compressed air into the
pterygomandibular space of freshly frozen cadavers to simulate
mandibular infection that had spread to the occlusal space.
Subsequently, significant air diffusion into the parapharyngeal,
parotid, buccal, sublingual and submandibular spaces was observed.
These findings suggest that inflammation spreads easily in the
maxillofacial region, which has abundant branch-linked spaces and
lax connective tissue. The route of infection in the present case
was determined to be the acute phase of pericoronitis in the left
lower wisdom tooth, which had spread to the occlusal space, invaded
the left buccal space, and eventually formed an oral space
infection. Moreover, the present patient was young, which is
consistent with the finding of a study that young patients are the
most affected population (17).
Additionally, disease onset in the present case occurred in the
summer, which concurs with a previous study that reported a high
incidence of AAV in the summer (13).
In addition to the timely surgical management of the
local abscess, the discontinuation of immunosuppressive drugs and
reduction of glucocorticoids were crucial in restoring the immune
functions of the patient. Additionally, the routine intravenous
administration of broad-spectrum antibiotics was crucial for the
complete control of OMSI in the patient. The patient received
regular follow-ups from the hospital, and her conditions have
remained stable to date. Patients with AAV are prone to
co-infection, which is closely associated with the disease state,
individual constitution and the type, dose and duration of
immunosuppressive drugs. Immunosuppressive drugs often cause
secondary immune deficiency in patients, which can lead to certain
rare or uncommon infections and, in severe cases, death (18). Thus, aggressive infection control
can not only ameliorate the activity of AAV but also effectively
improve the long-term survival of the patient (19).
There are some limitations in the present case.
Firstly, the patient refused to be photographed during the surgery,
so photographs that could provide an improved representation of the
disease status and the outcome of the surgery are not available.
Secondly, no photographs of the pus samples collected for
laboratory tests and of the affected area at the time of discharge
are available to demonstrate the severity of the infection and the
outcome of treatment more visually. However, after timely and
precise treatment, the patient recovered and was discharged. Future
studies are required to present more evidence to validate the
current treatment regimen for AAV combined with OMSI.
In conclusion, glucocorticoids and immunosuppressive
drugs are effectively able to control the activity and recurrence
of AAV, but secondary infections commonly occur. Infections can
impede subsequent treatment of the disease and require careful
consideration by clinicians. Therefore, based on the successful
treatment experience of the present case, the following
recommendations for the prevention and control of AAV infection are
proposed. Firstly, the rational use of glucocorticoids and
immunosuppressive agents is recommended, with minimal drug doses to
control the disease. Current treatment guidelines may be used as a
reference in clinical practice, and it is worth noting that
personalized treatment regimens are also essential. Secondly, close
follow-up is required to regularly monitor the blood and lymphocyte
subsets of the patient, allowing early detection and timely
intervention. Thirdly, prompt adjustment of the treatment regimens,
particularly medication modifications and the initiation of
anti-infective treatment should be performed in a timely manner if
the patient shows signs of infection. Therefore, specialized
surgical management should be promptly considered for infections
that meet the conditions for surgery.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZQ contributed to conceptualization and design of
the study, analyzed and interpreted the data, and was a major
contributor in drafting the manuscript. XL was responsible for
study design and manuscript revision. SL and HZ collected clinical
information, designed the study and assisted with the drafting of
the manuscript. XL and ZQ confirm the authenticity of all the raw
data. All authors critically revised the manuscript for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of the data and images in this case
report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Deng X, Gao J and Zhao F: Identification
of differentially expressed genes and pathways in kidney of
ANCA-associated vasculitis by integrated bioinformatics analysis.
Ren Fail. 44:204–216. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Li J, Cui Z, Long JY, Huang W, Wang JW,
Wang H, Zhang L, Chen M and Zhao MH: The frequency of
ANCA-associated vasculitis in a national database of hospitalized
patients in China. Arthritis Res Ther. 20(226)2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Salvador F: ANCA associated vasculitis.
Eur J Intern Med. 74:18–28. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Geetha D and Jefferson JA: ANCA-associated
vasculitis: Core curriculum 2020. Am J Kidney Dis. 75:124–137.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kitching AR, Anders HJ, Basu N, Brouwer E,
Gordon J, Jayne DR, Kullman J, Lyons PA, Merkel PA, Savage COS, et
al: ANCA-associated vasculitis. Nat Rev Dis Primers.
6(71)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Xiao Y, Guyatt G, Zeng L, Rw Jayne D, A
Merkel P, Ac Siemieniuk R, Dookie JE, A Buchan T, Ahmed MM, J
Couban R, et al: Comparative efficacy and safety of alternative
glucocorticoids regimens in patients with ANCA-associated
vasculitis: A systematic review. BMJ Open.
12(e050507)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Theofilis P, Vordoni A, Koukoulaki M,
Vlachopanos G and Kalaitzidis RG: Overview of infections as an
etiologic factor and complication in patients with vasculitides.
Rheumatol Int. 42:759–770. 2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
King C, Harper L and Little M: The
complications of vasculitis and its treatment. Best Pract Res Clin
Rheumatol. 32:125–136. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lionaki S and Boletis JN: The prevalence
and management of pauci-immune glomerulonephritis and vasculitis in
Western countries. Kidney Dis (Basel). 1:224–234. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kamat RD, Dhupar V, Akkara F and Shetye O:
A comparative analysis of odontogenic maxillofacial infections in
diabetic and nondiabetic patients: An institutional study. J Korean
Assoc Oral Maxillofac Surg. 41:176–180. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Nakazawa D, Masuda S, Tomaru U and Ishizu
A: Pathogenesis and therapeutic interventions for ANCA-associated
vasculitis. Nat Rev Rheumatol. 15:91–101. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mohammad AJ: An update on the epidemiology
of ANCA-associated vasculitis. Rheumatology (Oxford). 59
(Suppl3):iii42–iii50. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Han X, An J, Zhang Y, Gong X and He Y:
Risk factors for life-threatening complications of maxillofacial
space infection. J Craniofac Surg. 27:385–390. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Al-Sebaei MO and Jan AM: A survey to
assess knowledge, practice, and attitude of dentists in the Western
region of Saudi Arabia. Saudi Med J. 37:440–445. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Mukhtyar C, Lee R, Brown D, Carruthers D,
Dasgupta B, Dubey S, Flossmann O, Hall C, Hollywood J, Jayne D, et
al: Modification and validation of the Birmingham vasculitis
activity score (version 3). Ann Rheum Dis. 68:1827–1832.
2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Iwanaga J, Watanabe K, Anand MK and Tubbs
RS: Air dissection of the spaces of the head and neck: A new
teaching and dissection method. Clin Anat. 33:207–213.
2020.PubMed/NCBI View
Article : Google Scholar
|
|
17
|
Khawaja NA, Khalil H, Parveen K, Al-Mutiri
A, Al-Mutiri S and Al-Saawi A: A retrospective radiographic survey
of pathology associated with impacted third molars among patients
seen in oral & maxillofacial surgery clinic of college of
dentistry, riyadh. J Int Oral Health. 7:13–17. 2015.PubMed/NCBI
|
|
18
|
Arman F, Barsoum M, Selamet U, Shakeri H,
Wassef O, Mikhail M, Rastogi A and Hanna RM: Antineutrophil
cytoplasmic antibody-associated vasculitis, update on molecular
pathogenesis, diagnosis, and treatment. Int J Nephrol Renovasc Dis.
11:313–319. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kakoullis L, Parperis K, Papachristodoulou
E and Panos G: Infection-induced myeloperoxidase specific
antineutrophil cytoplasmic antibody (MPO-ANCA) associated
vasculitis: A systematic review. Clin Immunol.
220(108595)2020.PubMed/NCBI View Article : Google Scholar
|