Introduction
Reflux esophagitis (RE) is classified as an upper
gastrointestinal disease that is characterized by symptoms of
regurgitation, heartburn and esophageal mucosal injury. Most of
these symptoms are caused by regurgitation of gastric or duodenal
contents into the esophagus. RE is a type of gastroesophageal
reflux disease (GERD) with high incidence and recurrence rates. The
occurrence of RE is attributed to the interaction of multiple
factors, including the impaired anti-reflux function of the
gastroesophageal junction (GEJ), low motility state of the stomach
and esophagus, and decreased clearing ability of the
extra-esophageal organs to regurgitation. Among these factors,
damage to the anatomical structure of the GEJ is the most critical
causative factor for the occurrence of RE (1). Gastroscopy is the preferred
examination in the diagnosis and treatment of GERD. Abnormalities
of the GEJ, including the severity of the esophageal mucosa injury,
axial length of the hiatal hernia (HH), degree of relaxation of the
cardia, and morphological changes in the gastroesophageal flap
valve (GEFV), can be observed directly through gastroscopy. Reflux
symptoms can recur or persist in patients with GERD and an abnormal
anatomical morphology of the GEJ (2,3). A
previous review showed that 17 to 45% of 21,736 patients still
experienced reflux symptoms after treatment with proton-pump
inhibitors (PPIs) (4).
The GERD clinical guidelines of numerous countries
point out that the objective of GERD treatment should primarily
consider cost-effectiveness (5,6). The
initial evaluation methods of GERD include a PPI test,
questionnaire and gastroscopy evaluation. When further diagnosis
and treatment are required, including clarifying the degree and
nature of regurgitation, endoscopic treatment and preoperative
evaluation, objective examinations including multichannel
intraluminal impedance-pH testing (MII-pH), high-resolution
esophageal manometry (HRM) are needed.
Numerous studies have analyzed the risk factors for
RE. However, only a few studies have examined the predictive
factors for reflux recurrence by observing the structural
abnormalities of the GEJ during endoscopy. In the present study,
reflux recurrence and the efficacy of PPI treatment were evaluated
through a Reflux Disease Questionnaire (RDQ) and collected data on
gastroscopic findings and general information of patients with
different degrees of reflux symptom recurrence. The prediction
model and receiver operating characteristic (ROC) curves were
constructed to evaluate the clinical predictive values of reflux
recurrence.
Materials and methods
Patients
An analysis was performed on patients who were
treated in four hospitals from September 2020 to December 2021 for
RE with structural abnormalities of the GEJ and reflux symptoms
including regurgitation, heartburn, noncardiogenic chest pain, and
food reflux. The present study protocol was approved (approval no.
T20211223001) by the Ethics Committee of Linfen People's Hospital
affiliated to Shanxi Medical University (Taiyuan, China). Inclusion
criteria: Patients who were diagnosed using painless gastroscopy
and responded to a 6-week treatment of esomeprazole were included
in the study. Exclusion criteria were as follows: i) Patients
diagnosed with other digestive system diseases, including achalasia
of the cardia, esophageal cardia laceration, nodular gastritis,
bile reflux gastritis, peptic ulcer, Zollinger-Ellison syndrome,
refractory RE, secondary RE, gastroesophageal varices,
gastroesophageal carcinoma, upper gastrointestinal surgery history,
and digestive tract malformation; ii) those with non-digestive
system diseases, such as depression and other psychiatric
illnesses, severe dysfunction of important organs; iii) those with
other conditions that required drug intake that affect the
gastrointestinal function during treatment, including non-steroidal
anti-inflammatory drugs, hormonal drugs, calcium antagonists, and
other drugs. Patients who did not receive the standard treatment or
had incomplete case information were also excluded from the study.
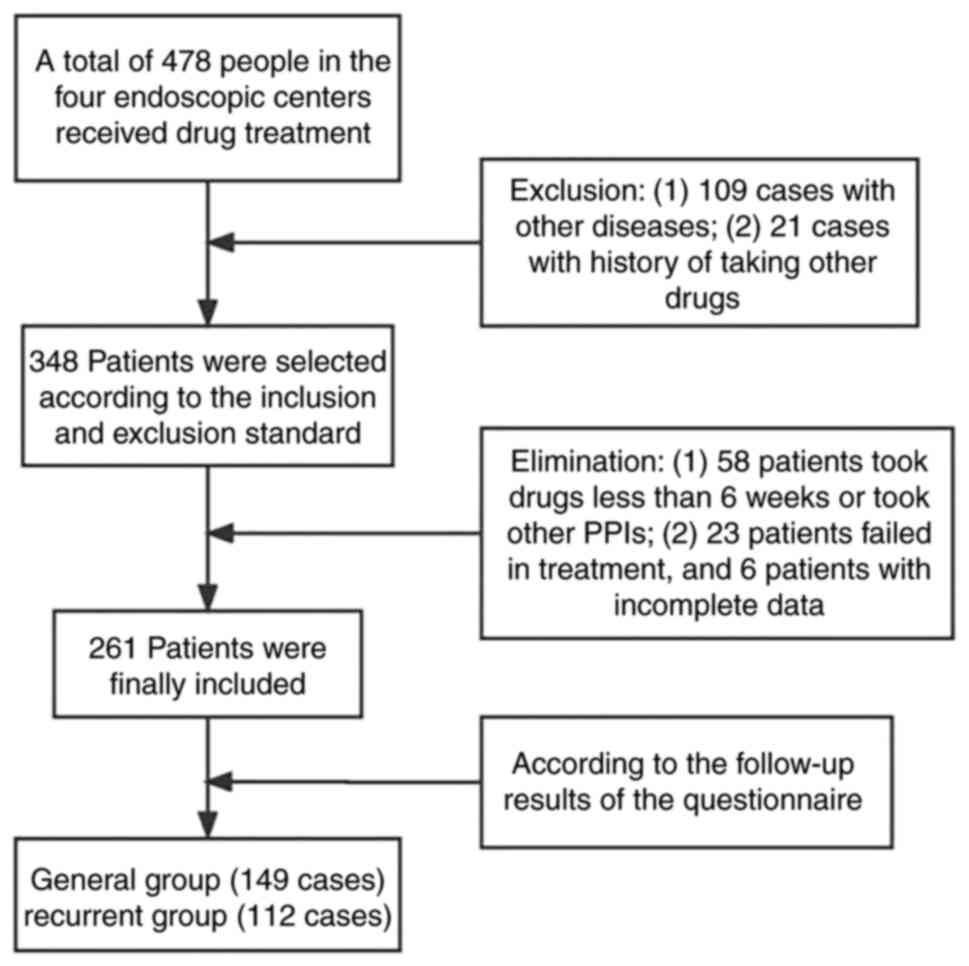
The screening process is illustrated in Fig. 1. Among all the patients (n=261)
participating in this study, there were 158 men and 103 women,
ranging in age from 21 to 83 years old.
Treatment and grouping criteria
The treatment administered was in accordance with
the Chinese GERD guidelines (7).
Esomeprazole (20 mg) was administered twice daily (i.e., 30 min
before breakfast and before bedtime) for 6 weeks as the initial
treatment, and the maintenance treatment was esomeprazole 20 mg
administered once, if necessary. Patients were evaluated using the
RDQ before the initial treatment and at the first and third months
after the initial treatment to determine whether the initial
treatment was effective or if the symptoms recurred (Table SI) (8). Effective treatment or no recurrence
was defined as a decrease in RDQ score of ≥50% before the initial
treatment; otherwise, the treatment was considered invalid or
recurrent (9,10). Patients who responded to the
initial treatment were screened and divided into general and
recurrent groups according to the RDQ score and GERD guidelines. On
the third month after the initial treatment, patients with severity
and frequency scores of ≤2 points for any reflux symptoms were
assigned to the general group while patients who met one of the
following conditions were assigned to the recurrent group: i) the
frequency score was >2 points regardless of the severity of
reflux symptoms; ii) severity score was >2 points. The follow-up
time for all patients is regular, so there is no difference in the
follow-up time between the two groups of patients. During the
follow-up, no patients in the General group needed maintenance
treatment. By contrast, 67 patients in the recurrent group reported
receiving maintenance therapy with Esomeprazole 20 mg once a day
for 1 to 10 days after the initial treatment, while 19 patients
remained on Esomeprazole.
Data collection
The general information of the patients, including
sex, age, body mass index (BMI), Helicobacter pylori (H.
pylori) infection, smoking and drinking history, was collected
during the follow-up. Gastroscopic findings include RE grade, GEFV
grade, axial length of HH, esophageal hiatus diameter, chronic
superficial gastritis and chronic atrophic gastritis (CAG).
RE grade was assigned based on the Los Angeles
classification (11), GEVF was
evaluated using the Hill classification, CAG was graded based on
the Kimura-Takemoto classification (12) and H. pylori infection was
diagnosed by the urea breath test. The distance from the
diaphragmatic hiatus to the incisors subtracted by the distance
from the dentate line to the incisors was defined as the axial
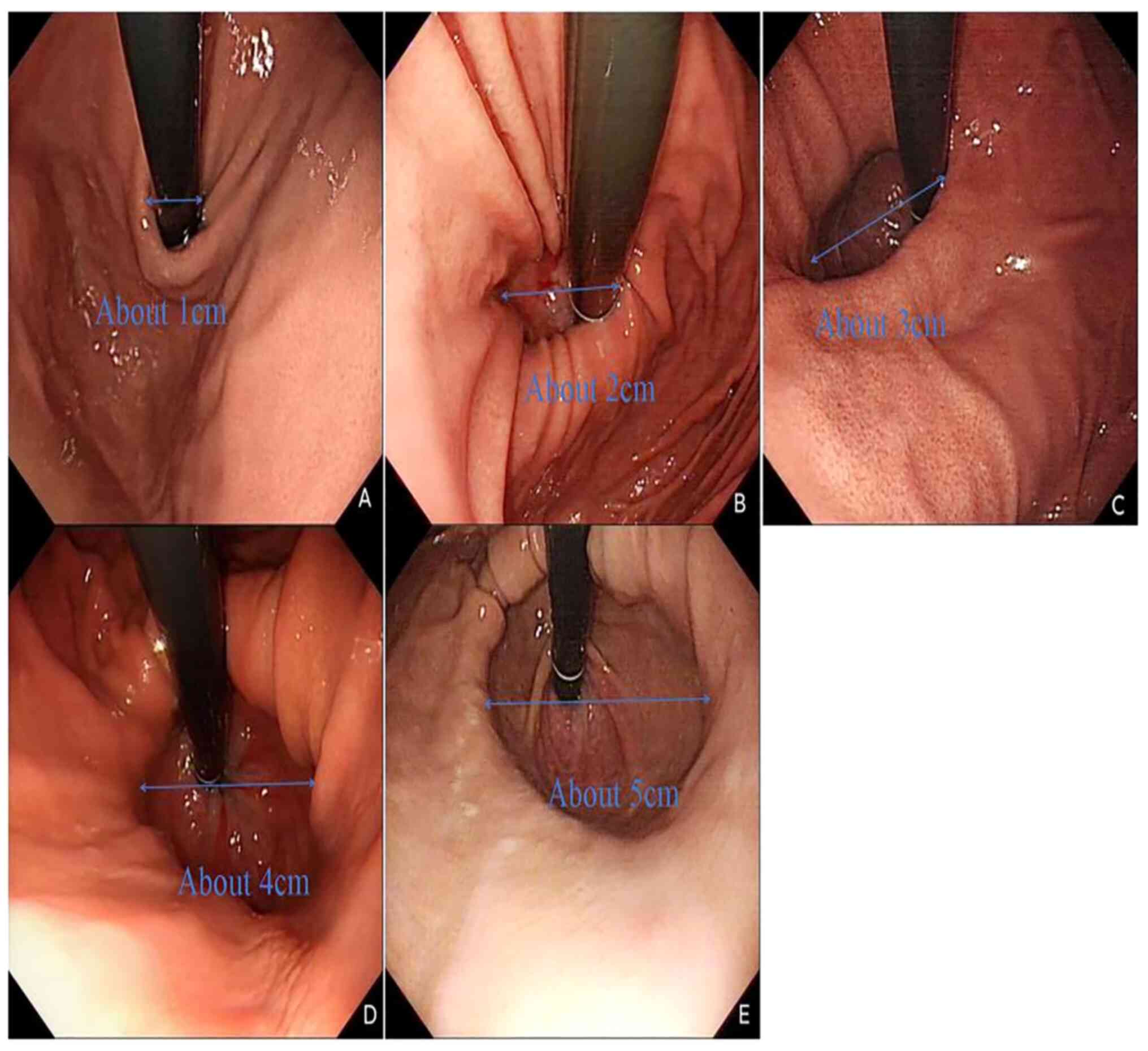
length of the HH (13,14). During gastroscopy, images were
captured after observing the morphology of GEFV for at least 30 sec
and the diameter of the esophageal hiatus was assessed on these
images. Using the endoscope shaft (~1 cm) as the reference, the
algebraic multiple relationship between the esophageal hiatus
diameter and endoscope shaft was measured (15). The diameters of the esophageal
hiatus of all patients were evaluated and recorded by the same
researcher. Since the diameter of the esophageal hiatus cannot be
measured directly, a scoring system was used to represent the range
of esophageal hiatus diameters for statistical analysis. Based on
the measurement results, 1 cm ≤ diameter <2 cm was defined as 1
point, 2 cm ≤ diameter <3 cm was defined as 2 points, 3 cm ≤
diameter <4 cm was defined as 3 points, 4 cm ≤ diameter <5 cm
was defined as 4 points and diameter ≥5 cm was defined as 5 points.
The endoscopic images of each score are shown in Fig. 2. Two types of gastroscope
(GIF-H290, Olympus Corporation; and EG760, FUJIFILM Wako Pure
Chemical Corporation) were used in these assessments.
Statistical analysis
Data were analyzed using SPSS V25.0 (IBM Corp.). All
the quantitative data were normally distributed. Quantitative data
were expressed as the mean ± standard error and independent samples
t-test was used for comparison. Qualitative data were expressed as
rate (%) and chi-square test was used for comparison. Correlations
between the continuous variables (i.e., axial length of the HH) and
ordinal categorical variables (i.e., RE grade and recurrence) were
analyzed using the Kendall correlation coefficients. The factors
with P<0.2 in the univariate analysis were included in the
logistic regression analysis. The ROC curves and nomogram were
built using R version 4.2.2 (www.r-project.org). P<0.05 was considered to
indicate a statistically significant difference.
Results
Sex, BMI, axial length of HH, esophageal hiatus
diameter score, RE classification, Hill classification, smoking
history, and drinking history between the two groups were
significantly different. The results of univariate analysis are
shown in Table I. Univariate
analysis revealed that sex, smoking and alcohol consumption were
closely associated with reflux symptom recurrence (P<0.001);
however, these three factors were not independent risk factors for
reflux recurrence after excluding the interaction among the factors
through logistic regression analysis.
 | Table IThe factors included in the present
study and the results of univariate analysis. |
Table I
The factors included in the present
study and the results of univariate analysis.
| Factors | General group
(n=149) | Recurrent group
(n=112) | t-value | P-value |
|---|
| Sex | | | 11.41 | 0.001 |
|
Female
(%) | 72 (48.3%) | 31 (27.7%) | | |
|
Male
(%) | 77 (51.7%) | 81 (72.3%) | | |
| Age (years) | 55.2±12.2 | 56.7±10.3 | -0.24 | 0.275 |
| Body mass index
(kg/m2) | 24.4±2.3 | 25.6±2.2 | -3.83 | <0.001 |
| Reflux
esophagitis | | | | |
|
Grade A
(%) | 78 (52.2%) | 42 (37.5%) | | |
|
Grade B
(%) | 57 (38.3%) | 45 (40.2%) | | |
|
Grade C
(%) | 12 (8.1%) | 15 (13.4%) | | |
|
Grade D
(%) | 2 (1.3%) | 10 (8.9%) | | |
| Hill | | | | |
|
Grade III
(%) | 107 (71.8%) | 41 (36.6%) | 32.28 | <0.001 |
|
Grade IV
(%) | 42 (28.1%) | 71 (63.3%) | | |
| The axial length of
hiatal hernia (cm) | 1.97±0.51 | 2.40±0.54 | -6.09 | <0.001 |
| Esophageal hiatus
diameter score | 2.48±0.62 | 3.07±0.62 | -6.74 | <0.001 |
| Superficial
gastritis | | | | |
|
No | 60 (40.2%) | 50 (44.5%) | 0.50 | 0.479 |
|
Yes | 89 (59.7%) | 62 (55.4%) | | |
| Atrophic
gastritis | | | | |
|
No (%) | 89 (59.7%) | 62 (55.4%) | 5.06 | 0.080 |
|
C1/C2
(%) | 50 (33.6%) | 48 (42.9%) | | |
|
C3/O1
(%) | 10 (6.7%) | 2 (1.8%) | | |
| Drinking | | | | |
|
No | 122 (81.8%) | 78 (69.6%) | 5.35 | 0.021 |
|
Yes | 27 (18.1%) | 34 (30.4%) | | |
| Smoking | | | | |
|
No | | | | |
|
Yes | | | | |
| Helicobacter
Pylori infection | | | | |
|
No | 123 (82.6%) | 99 (88.4%) | 1.72 | 0.190 |
|
Yes | 26 (17.4%) | 13 (11.6%) | | |
The factors with P<0.2 in the univariate analysis
were included in the logistic regression analysis. Axial length of
HH, esophageal hiatus diameter score, Hill classification, and BMI
were independent risk factors for reflux recurrence. The results
are shown in Table II. A total of
148 patients were classified as grade III, including 41 (27.7%)
cases in the recurrent group and 107 (72.2%) cases in the general
group; 113 patients were classified as grade IV, including 71
(62.8%) patients in the recurrent group and 42 (37.1%) cases in the
general group. The average BMI of the general and recurrent groups
were 24.4±2.3 and 25.6±2.2 kg/m2, respectively.
 | Table IIResults of Logistic regression
analysis and risk factors for reflux symptoms recurrence. |
Table II
Results of Logistic regression
analysis and risk factors for reflux symptoms recurrence.
| Risk factors | β | SE | Wald | P-value | OR (95% confidence
interval) |
|---|
| Sex (man) | 0.548 | 0.354 | 2.394 | 0.122 | 1.730
(0.864~3.462) |
| Hill grade IV | 0.875 | 0.366 | 5.722 | 0.017 | 2.399
(1.171~4.912) |
| Reflux esophagitis
classification | | | 3.716 | 0.294 | |
| Grade B | -0.564 | 0.920 | 0.376 | 0.852 | 0.829
(0.114~6.014) |
| Grade C | -0.945 | 0.892 | 1.122 | 0.540 | 0.569
(0.094~3.451) |
| Grade D | -1.436 | 0.959 | 2.242 | 0.134 | 0.238
(0.036~1.559) |
| Chronic atrophic
gastritis | | | 0.356 | 0.837 | |
| C1/C2 | 0.079 | 0.952 | 0.007 | 0.934 | 1.083
(0.168~6.991) |
| C3/O1 | 0.265 | 0.957 | 0.076 | 0.782 | 1.303
(0.200~8.504) |
| The axial length of
hiatal hernia | 0.970 | 0.347 | 7.810 | 0.005 | 2.638
(1.336~5.207) |
| Esophageal hiatus
diameter score | 0.984 | 0.293 | 11.264 | 0.001 | 3.676
(1.506~4.754) |
| Body mass
index | 0.160 | 0.069 | 5.402 | 0.020 | 1.173
(1.025~1.342) |
| Helicobacter
Pylori infection (Yes) | -0.906 | 0.486 | 3.474 | 0.062 | 0.404
(0.156~1.048) |
| Drinking | 0.409 | 0.443 | 0.852 | 0.356 | 1.505
(0.632~3.584) |
| Smoking | 0.210 | 0.502 | 0.175 | 0.676 | 1.234
(0.461~3.300) |
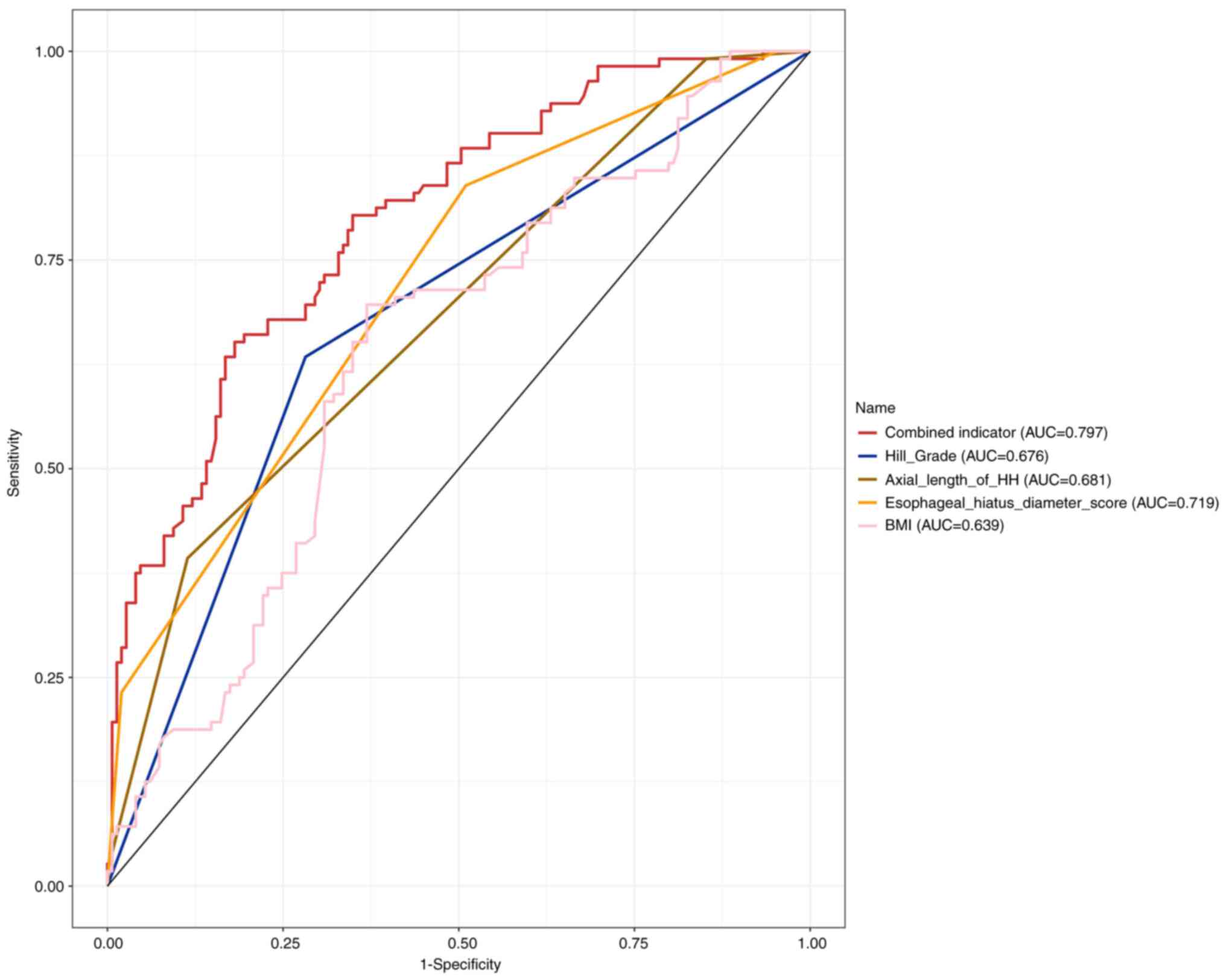
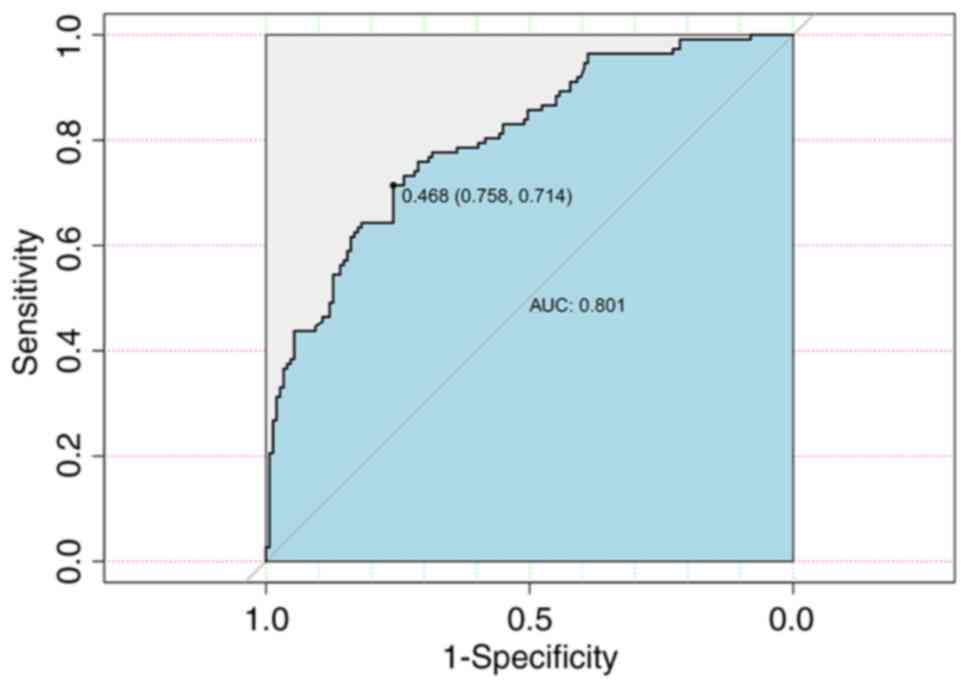
The axial length of the HH, esophageal hiatus
diameter score, Hill classification, and BMI were used as test
variables, and recurrence was used as a classification variable to
construct the ROC curves (Fig. 3).
In Table III, the AUC values of
each factor are summarized. The cut-off value of the esophageal
hiatus diameter score was >2 points, corresponding to the
esophageal hiatus diameter of ≥3 cm. The differences in the AUC
between the prediction model and each factor were statistically
significant (P<0.000). The prediction model showed a higher
accuracy in predicting reflux recurrence than each factor
alone.
 | Table IIIThe prediction model for predicting
reflux symptom recurrence. |
Table III
The prediction model for predicting
reflux symptom recurrence.
| Predictors | AUC | 95% CI | Cut-off value | Sensitivity
(%) | Specificity
(%) | P-value |
|---|
| The axial length of
HH (cm) | 0.681 | 0.630~0.733 | >2 | 39.29 | 88.59 |
P1<0.000 |
| Esophageal hiatus
diameter score | 0.719 | 0.665~0.773 | >2 | 83.93 | 48.99 |
P2<0.000 |
| Hill
classification | 0.676 | 0.618~0.734 | > grade III | 63.39 | 71.81 |
P3<0.000 |
| BMI
(kg/m2) | 0.639 | 0.571~0.706 | >25.1 | 69.64 | 63.09 |
P4<0.000 |
| Prediction
model | 0.797 | 0.734~0.851 | >0.539 | 65.18 | 81.88 | |
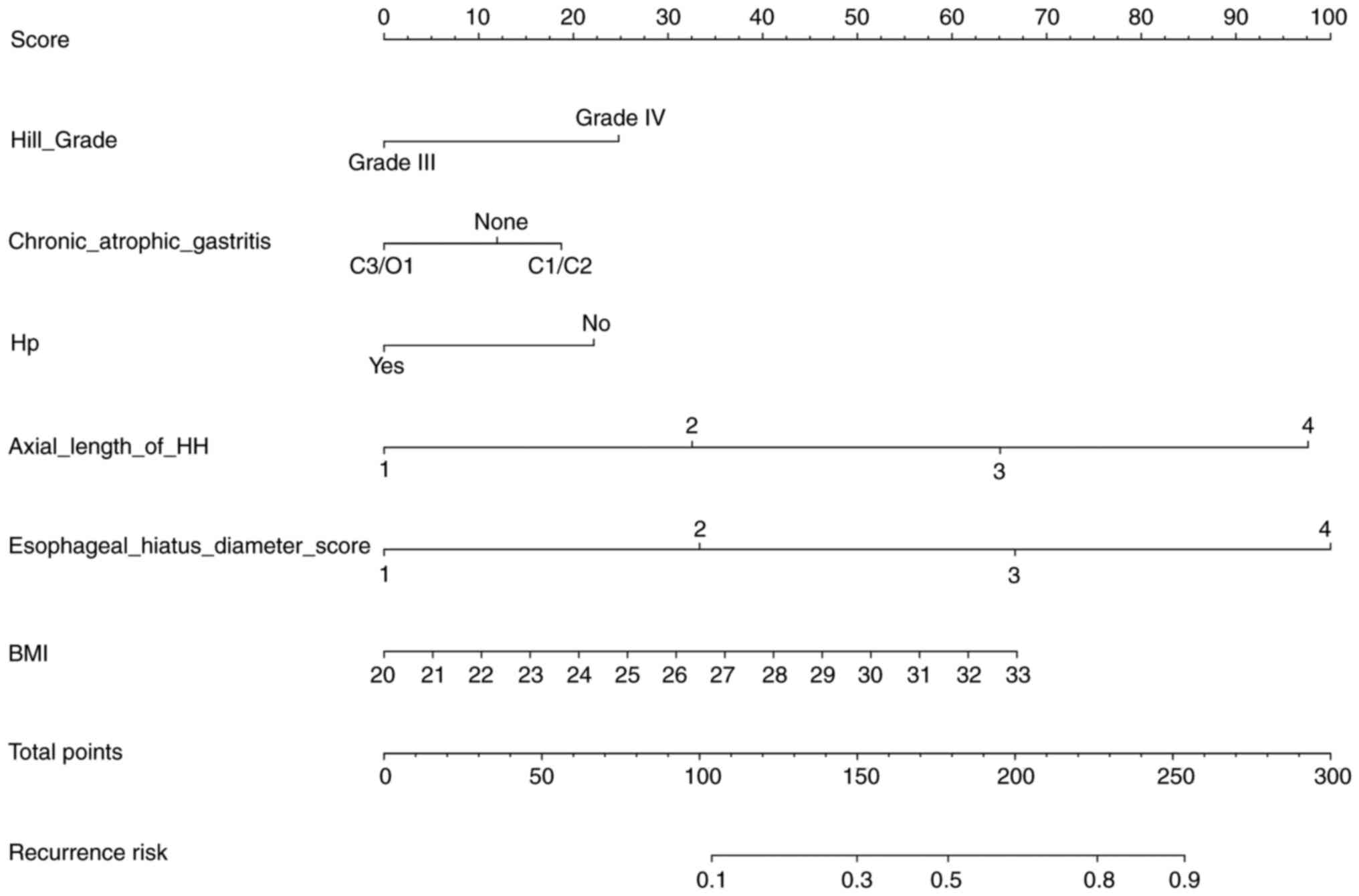
The nomogram was developed based on clinical
experience and a literature review using the four independent risk
factors, CAG and H. pylori infection (Fig. 4). The higher total point value for
the six indicators, the greater the probability of reflux
recurrence. In multivariate prediction model, the reflux recurrence
score of 0.468 showed the most accurate prediction. The cut-off
value of 46.8 revealed accuracy, sensitivity, specificity, positive
predictive value and negative predictive value of 74.0, 71.4, 75.8,
69.0 and 77.9%, respectively (Table
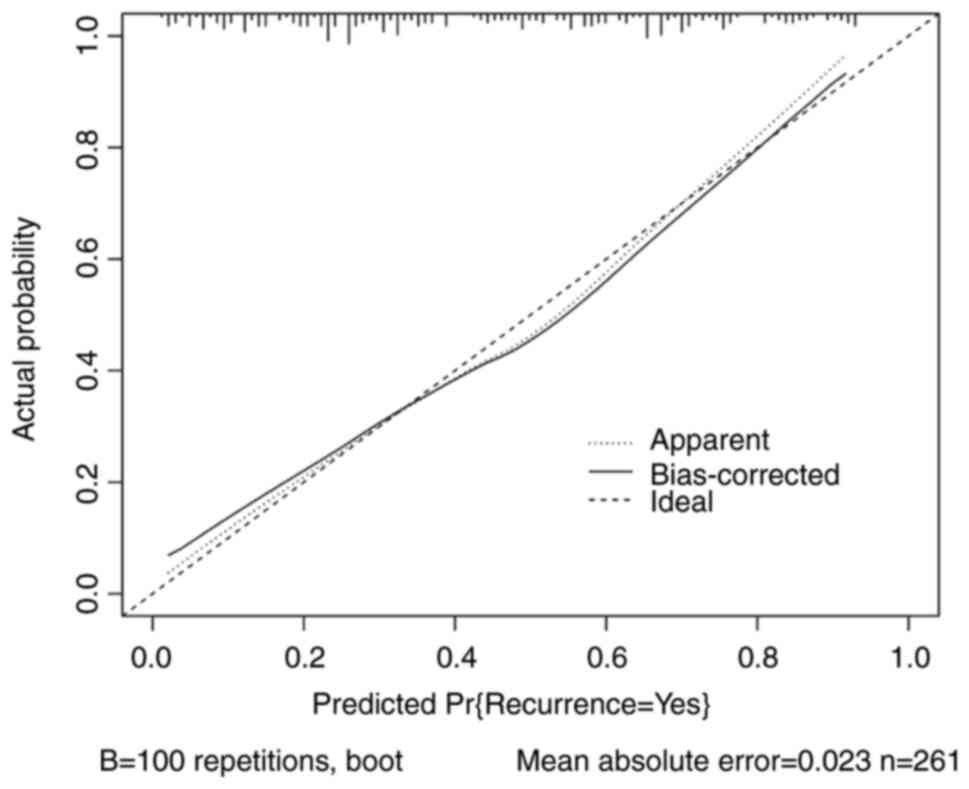
IV). The multivariate prediction model for reflux recurrence
was established using the data from all patients and showed a ROC
of 0.801 (95% confidence interval: 0.748-0.854) (Fig. 5). In addition, the AUC of the two
prediction models was not significantly different (P=0.552). The
calibration curve revealed favorable predictive accuracy between
the predicted and actual reflux recurrence (mean absolute
error=0.023) (Fig. 6).
 | Table IVThe efficacy of the multivariate
prediction model in predicting reflux recurrence. |
Table IV
The efficacy of the multivariate
prediction model in predicting reflux recurrence.
| Cutoff | Accuracy | Sensitivity | Specificity | Positive predictive
value | Negative predictive
value | Positive by
prediction model |
|---|
| 63.8 | 0.709 | 0.482 | 0.879 | 0.750 | 0.693 | 72 (0.276) |
| 56.1 | 0.743 | 0.616 | 0.839 | 0.742 | 0.744 | 93 (0.356) |
| 46.8 | 0.740 | 0.714 | 0.758 | 0.690 | 0.779 | 116 (0.444) |
| 39.1 | 0.732 | 0.759 | 0.711 | 0.664 | 0.797 | 128 (0.490) |
| 26.9 | 0.648 | 0.839 | 0.503 | 0.560 | 0.807 | 168 (0.644) |
| 26.4 | 0.655 | 0.857 | 0.503 | 0.565 | 0.824 | 170 (0.651) |
| 15.1 | 0.579 | 0.964 | 0.289 | 0.505 | 0.915 | 214 (0.820) |
| 12.0 | 0.548 | 0.973 | 0.228 | 0.487 | 0.919 | 224 (0.858) |
| 10.3 | 0.540 | 0.991 | 0.201 | 0.483 | 0.968 | 230 (0.881) |
| 7.2 | 0.494 | 0.991 | 0.121 | 0.459 | 0.947 | 242 (0.927) |
| 6.3 | 0.475 | 0.991 | 0.087 | 0.449 | 0.929 | 247 (0.946) |
| 4.2 | 0.464 | 1.000 | 0.060 | 0.444 | 1.000 | 252 (0.966) |
| 2.4 | 0.448 | 1.000 | 0.034 | 0.438 | 1.000 | 256 (0.981) |
Discussion
The occurrence of RE is attributed to the
interaction of multiple factors. The abnormal anatomical morphology
of the GEJ weakens the anti-reflux function and the low motility
state decreases the clearance ability of the esophagus and prolongs
acid exposure time, which not only aggravate regurgitation, but
also affects the efficacy of PPI treatment (6). Reflux symptoms can recur or persist
in patients with GERD and an abnormal anatomical morphology of the
GEJ (2). In the present study, the
anatomical morphology of the GEJ of patients with different
severity of regurgitation was analyzed. Previous studies have
indicated that factors, including HH and abnormal GEFV affect the
efficacy of PPI treatment for GERD (16,17),
but BMI does not (18). In the
present study, it appeared that patients with axial length HH >2
cm, esophageal hiatus diameter ≥3 cm, Hill grade IV, and BMI
>25.1 kg/m2 at the same time are vulnerable to severe
regurgitation and may require long-term maintenance treatment.
In the current study, the optimal cut-off value of
BMI was >25.1 kg/m2 and patients with recurrent
regurgitation accounted for 58.2% (78/134). Pandolfino et al
(19) analyzed the relationship
between obesity and pressure of the EGJ; it was revealed that
patients with BMI >25 kg/m2 had significantly higher
intragastric pressure than those with BMI <25 kg/m2.
This finding indicated that the gastroesophageal pressure in the
GEJ increases with BMI, causing the anti-reflux function to become
unstable. Furthermore, patients with a BMI >30 kg/m2
were more likely to develop HH and GERD, further supporting the
results of the present study.
The morphology of the gastric mucosal fold and its
fit with the endoscopic shaft reflects the anti-reflux function of
the GEJ. Hill et al classified GEFV into four grades based
on the appearance of the GEJ; grades I and II were normal, while
grades III and IV were abnormal (20). In a meta-analysis examining the
predictive value of the Hill classification on GERD (21), 3,914 patients were included in
seven studies, and the sensitivity and specificity of abnormal GEFV
in the diagnosis of RE were 54.8 and 75.7%, respectively. The Hill
classification provides diagnostic information on the morphology of
the EGJ and quantifies the severity of GERD, which facilitates the
selection of a therapeutic regimen and observation of
prognosis.
The endoscopic evaluation of sliding HH includes the
axial length of the HH and esophageal hiatus diameter; however,
presently, there is no unified standard for its endoscopic
diagnosis and classification (2,22).
Schlottmann et al (23)
measured the axial length of HH using barium radiography and
divided the study population into three groups: HH <3, 3-5, and
>5 cm. Regurgitation occurred more frequently and esophagitis
and reflux symptoms were more severe in patients with longer axial
length of HH; in the current study, the average axial lengths of HH
in the general and recurrent groups were 1.97±0.51 and 2.40±0.54
cm, respectively. Additionally, the Kendall tau-β correlation
coefficients between the axial length of HH and RE classification
and recurrence were 0.198 and 0.366, respectively (P<0.001),
which were similar to the study conducted by Schlottmann et
al.
A previous research showed that the average axial
length of HH and Hill classification in patients with GERD were
greater than those in non-GERD patients (1.9 and 2.7 cm vs. 1.6 and
2.2 cm). There was no statistical difference between the Hill
classification and axial length of HH; however, in clinical
practice, the Hill classification was more accurate in measurement
than that of axial length of HH (24). In the present study, there was no
statistical significance in the AUC between the Hill classification
and axial length of HH (P=0.880), which indicates that the Hill
classification was not superior to axial length of HH in predicting
reflux symptom recurrence. The combination of the axial length of
HH, esophageal hiatus diameter, Hill classification, and BMI showed
a higher accuracy in predicting reflux symptom recurrence than that
of each individual factor (P<0.001).
The relationship between H. pylori infection
and GERD has not yet been resolved (25). Gastric atrophy and hyposecretion of
gastric acid often occur in patients with H. pylori
infection. Therefore, it is mostly considered believe that H.
pylori infection is negatively correlated with RE, which may
protect vulnerable individuals from GERD (26). Similarly, the effect of CAG on
gastric mucosa is analogous to that of H. pylori infection
(27). To construct a reasonable
and complete prediction model, combined with the authors' clinical
experience and literature review, atrophic gastritis and H.
pylori infection were included in the multivariate prediction
model, even if they are not independent risk factors for reflux
recurrence. Specifically, the results may be more definitive when
the sample size increases. In a similar study, a prediction model
with a sample size of 494 patients showed improved discriminative
power (28).
Actually, MII-pH or HRM have not yet been
popularized in all medical institutions of developing countries
including China, but patients with GERD are very common (5,29).
Without complicated symptoms, outpatients or physical examination
patients with GERD alone, usually do not require to be subjected to
other examinations than endoscopy from a cost-effective
perspective. There were several limitations to the present study.
Given the patients' condition in the present study, the data were
measured using RDQ and gastroscopy without other objective
examination, including MII-pH or HRM. The esophageal hiatus
diameter was indirectly measured by directly comparing the
esophageal hiatus diameter and endoscope shaft, scores were used to
reflect the range of the esophageal hiatus diameter and perform
statistical analysis. The sample size may not be sufficient due to
the exclusion criteria and patient compliance. Certain patients
discontinued their treatment voluntarily after a slight improvement
in symptoms. Further study with a larger sample size and more
objective examination is required to confirm the efficacy of the
prediction model in the present study.
This prediction model is more suitable for primary
clinical evaluation without imposing additional burdens on
outpatients. Patients with an axial length of HH >2 cm,
esophageal hiatus diameter ≥3 cm, Hill grade >III, and BMI
>25.1 kg/m2 are prone to have reflux recurrence or
require PPI maintenance treatment. In clinical practice, patients
who present with H. pylori infection and CAG are relatively
less likely to develop reflux recurrence. However, this feature was
not represented in the prediction model of the present study.
Meanwhile, a reference was provided for diagnosing refractory RE
and screening high-risk populations with poor drug efficacy or
recurrent reflux.
Supplementary Material
The scoring criteria of Reflux Disease
Questionnaire.
Acknowledgements
The authors would like to thank Dr Chaoxi Liu and Dr
Xuchun Wang (Department of Public Health, Shanxi Medical
University) for guiding the statistical analysis of the present
study.
Funding
Funding: The present study was partially supported (grant no.
201903D321140) by Key Research and Development (R&D) Projects
of Shanxi (China).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XC, QW and JL conceived and designed the study. JL
performed statistical analysis. QW and JL analyzed the data. QW,
YS, JF, JR and ZW performed data collection. QW and JL confirm the
authenticity of all the raw data. All authors contributed to the
writing of the manuscript and reviewed, read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was conducted in accordance with
the tenets of the Declaration of Helsinki. The present study
protocol was approved (approval no. T20211223001) by the Ethics
Committee of Linfen People's Hospital affiliated to Shanxi Medical
University (Taiyuan, China). According to the Shanxi Medical
University Ethics Committee, the study patients were notified of
the study and permitted the opportunity to refuse participation in
the study.
Patient consent for publication
With regard to the informed consent of participants,
the Ethics Committee of Linfen People's Hospital affiliated to
Shanxi Medical University made a decision based on the Ethical
Guidelines for Medical and Health Research Involving Human
Subjects, which states that non-intervention studies are deemed
exempt from patients' consent and, instead, researchers must notify
the study subjects about the information regarding study contents
on a home page, and guarantee an opportunity when the study
subjects could refuse consent. All patients participating in the
present study received written informed consent.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fuchs KH, DeMeester TR, Otte F, Broderick
RC, Breithaupt W, Varga G and Musial F: Severity of GERD and
disease progression. Dis Esophagus. 34(doab006)2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Li L, Gao H, Zhang C, Tu J, Geng X, Wang
J, Zhou X, Pan W and Jing J: Diagnostic value of X-ray, endoscopy,
and high-resolution manometry for hiatal hernia: A systematic
review and meta-analysis. J Gastroenterol Hepatol. 35:13–18.
2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Asaoka D, Takeda T, Sasaki H, Shimada Y,
Matsumoto K, Ueyama H, Matsumoto K, Izumi K, Komori H, Akazawa Y,
et al: Evaluation of symptomatic reflux esophagitis in proton pump
inhibitor users. Biomed Rep. 10:277–282. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
El-Serag H, Becher A and Jones R:
Systematic review: Persistent reflux symptoms on proton pump
inhibitor therapy in primary care and community studies. Aliment
Pharmacol Ther. 32:720–737. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Katz PO, Dunbar KB, Schnoll-Sussman FH,
Greer KB, Yadlapati R and Spechler SJ: ACG clinical guideline for
the diagnosis and management of gastroesophageal reflux disease. Am
J Gastroenterol. 117:27–56. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gyawali CP, Kahrilas PJ, Savarino E,
Zerbib F, Mion F, Smout AJPM, Vaezi M, Sifrim D, Fox MR, Vela MF,
et al: Modern diagnosis of GERD: The Lyon Consensus. Gut.
67:1351–1362. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Multidisciplinary Branch of
Gastroesophageal Reflux of China International Exchange and
Promotion Association for Medical and Healthcare. Consensus on
multidisciplinary diagnosis and treatment of gastroesophageal
reflux disease in China. Chin J Gastroesophagol Reflux Dis
(Electronic Edition). 7:1–28. 2020.(In Chinese).
|
|
8
|
Dent J, Vakil N, Jones R, Bytzer P,
Schöning U, Halling K, Junghard O and Lind T: Accuracy of the
diagnosis of GORD by questionnaire, physicians and a trial of
proton pump inhibitor treatment: The Diamond Study. Gut.
59:714–721. 2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Value of reflux diagnostic questionnaire
in the diagnosis of gastroesophageal reflux disease. Chin J Dig
Dis. 5:51–55. 2004.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Shaw MJ, Talley NJ, Beebe TJ, Rockwood T,
Carlsson R, Adlis S, Fendrick AM, Jones R, Dent J and Bytzer P:
Initial validation of a diagnostic questionnaire for
gastroesophageal reflux disease. Am J Gastroenterol. 96:52–57.
2001.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lundell LR, Dent J, Bennett JR, Blum AL,
Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler
SJ, et al: Endoscopic assessment of oesophagitis: Clinical and
functional correlates and further validation of the Los Angeles
classification. Gut. 45:172–180. 1999.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Quach DT and Hiyama T: Assessment of
endoscopic gastric atrophy according to the kimura-takemoto
classification and its potential application in daily practice.
Clin Endosc. 52:321–327. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sgouros SN, Mpakos D, Rodias M,
Vassiliades K, Karakoidas C, Andrikopoulos E, Stefanidis G and
Mantides A: Prevalence and axial length of hiatus hernia in
patients, with nonerosive reflux disease: A prospective study. J
Clin Gastroenterol. 41:814–818. 2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wallner B, Björ O, Andreasson A, Hellström
PM, Forsberg AM, Talley NJ and Agreus L: Identifying clinically
relevant sliding hiatal hernias: A population-based endoscopy
study. Scand J Gastroenterol. 53:657–660. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kaneyama H, Kaise M, Arakawa H, Arai Y,
Kanazawa K and Tajiri H: Gastroesophageal flap valve status
distinguishes clinical phenotypes of large hiatal hernia. World J
Gastroenterol. 16:6010–6015. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Peng S, Xiao YL, Cui Y, Lin JK, Zhang N,
Hu PJ and Chen MH: High-dose esomeprazole is required for
intraesophageal acid control in gastroesophageal reflux disease
patients with hiatus hernia. J Gastroenterol Hepatol. 27:893–898.
2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cheong JH, Kim GH, Lee BE, Choi MK, Moon
JY, Ryu DY, Kim DU and Song GA: Endoscopic grading of
gastroesophageal flap valve helps predict proton pump inhibitor
response in patients with gastroesophageal reflux disease. Scand J
Gastroenterol. 46:789–796. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Watanabe A, Iwakiri R, Yamaguchi D,
Higuchi T, Tsuruoka N, Miyahara K, Akutagawa K, Sakata Y, Fujise T,
Oda Y, et al: Risk factors for resistance to proton pump inhibitor
maintenance therapy for reflux esophagitis in Japanese women over
60 years. Digestion. 86:323–331. 2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Pandolfino JE, El-Serag HB, Zhang Q, Shah
N, Ghosh SK and Kahrilas PJ: Obesity: A challenge to
esophagogastric junction integrity. Gastroenterology. 130:639–649.
2006.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Hill LD, Kozarek RA, Kraemer SJ, Aye RW,
Mercer CD, Low DE and Pope CE II: The gastroesophageal flap valve:
In vitro and in vivo observations. Gastrointest Endosc. 44:541–547.
1996.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Osman A, Albashir MM, Nandipati K, Walters
RW and Chandra S: Esophagogastric junction morphology on Hill's
classification predicts gastroesophageal reflux with good accuracy
and consistency. Dig Dis Sci. 66:151–159. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Duranceau A: Massive hiatal hernia: A
review. Dis Esophagus. 29:350–366. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Schlottmann F, Andolfi C, Herbella FA,
Rebecchi F, Allaix ME and Patti MG: GERD: Presence and size of
hiatal hernia influence clinical presentation, esophageal function,
reflux profile, and degree of mucosal injury. Am Surg. 84:978–982.
2018.PubMed/NCBI
|
|
24
|
Hansdotter I, Björ O, Andreasson A, Agreus
L, Hellström P, Forsberg A, Talley NJ, Vieth M and Wallner B: Hill
classification is superior to the axial length of a hiatal hernia
for assessment of the mechanical anti-reflux barrier at the
gastroesophageal junction. Endosc Int Open. 4:E311–E317.
2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Richter JE and Rubenstein JH: Presentation
and epidemiology of gastroesophageal reflux disease.
Gastroenterology. 154:267–276. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Eusebi LH, Ratnakumaran R, Yuan Y,
Solaymani-Dodaran M, Bazzoli F and Ford AC: Global prevalence of,
and risk factors for, gastro-oesophageal reflux symptoms: A
meta-analysis. Gut. 67:430–440. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Han YM, Chung SJ, Yoo S, Yang JI, Choi JM,
Lee J and Kim JS: Inverse correlation between gastroesophageal
reflux disease and atrophic gastritis assessed by endoscopy and
serology. World J Gastroenterol. 28:853–867. 2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kim JY, Shin IS, Min YW, Kim K, Lee H, Min
BH, Lee JH, Kim JJ and Rhee PL: Endoscopic prediction for acid
reflux in patients without Hiatus Hernia. Korean J Gastroenterol.
76:134–141. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Xiao YL, Zhou LY, Hou XH, Li YQ, Zou DW
and Chen MH: Chinese Society of Gastroenterology. Chinese expert
consensus on gastroesophageal reflux disease in 2020. J Dig Dis.
22:376–389. 2021.PubMed/NCBI View Article : Google Scholar
|