|
1
|
Lee GY, Cho BO, Shin JY, Jang SI, Cho IS,
Kim HY, Park JS, Cho CW, Kang JS, Kim JH and Kim YH: Tyrosinase
inhibitory components from the seeds of Cassia tora. Arch Pharm
Res. 41:490–496. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Luo H, Wu H, Wang L, Xiao S, Lu Y, Liu C,
Yu X, Zhang X, Wang Z and Tang L: Hepatoprotective effects of
Cassiae Semen on mice with non-alcoholic fatty liver disease based
on gut microbiota. Commun Biol. 4(1357)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kim YJ, Lee S, Jin J, Woo H, Choi YK and
Park KG: Cassiaside C Inhibits M1 polarization of macrophages by
downregulating glycolysis. Int J Mol Sci. 23(1696)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Yang B, Xie L, Peng S, Sun K, Jin J, Zhen
Y, Qin K and Cai B: Nine components pharmacokinetic study of rat
plasma after oral administration raw and prepared Semen Cassiae in
normal and acute liver injury rats. J Sep Sci. 42:2341–2350.
2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Xu L, Li J, Tang X, Wang Y, Ma Z and Gao
Y: Metabolomics of aurantio-obtusin-induced hepatotoxicity in rats
for discovery of potential biomarkers. Molecules.
24(3452)2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mugas ML, Calvo G, Marioni J, Céspedes M,
Martinez F, Vanzulli S, Sáenz D, Di Venosa G, Nuñez Montoya S and
Casas A: Photosensitization of a subcutaneous tumour by the natural
anthraquinone parietin and blue light. Sci Rep.
11(23820)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zou Y, Cao Z, Wang J, Chen X, Chen YQ, Li
Y, Liu J, Zhao Y, Wang A and He B: A Series of Novel HDAC
inhibitors with anthraquinone as a cap group. Chem Pharm Bull
(Tokyo). 68:613–617. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Watroly MN, Sekar M, Fuloria S, Gan SH,
Jeyabalan S, Wu YS, Subramaniyan V, Sathasivam KV, Ravi S, Mat Rani
NNI, et al: Chemistry, biosynthesis, physicochemical and biological
properties of rubiadin: A promising natural anthraquinone for new
drug discovery and development. Drug Des Devel Ther. 15:4527–4549.
2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li Y, Guo F, Guan Y, Chen T, Ma K, Zhang
L, Wang Z, Su Q, Feng L, Liu Y and Zhou Y: Novel anthraquinone
compounds inhibit colon cancer cell proliferation via the reactive
oxygen Species/JNK Pathway. Molecules. 25(1672)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Szymańska M and Majerz I: Effect of
substitution of hydrogen atoms in the molecules of anthrone and
anthraquinone. Molecules. 26(502)2021.PubMed/NCBI View Article : Google Scholar
|
|
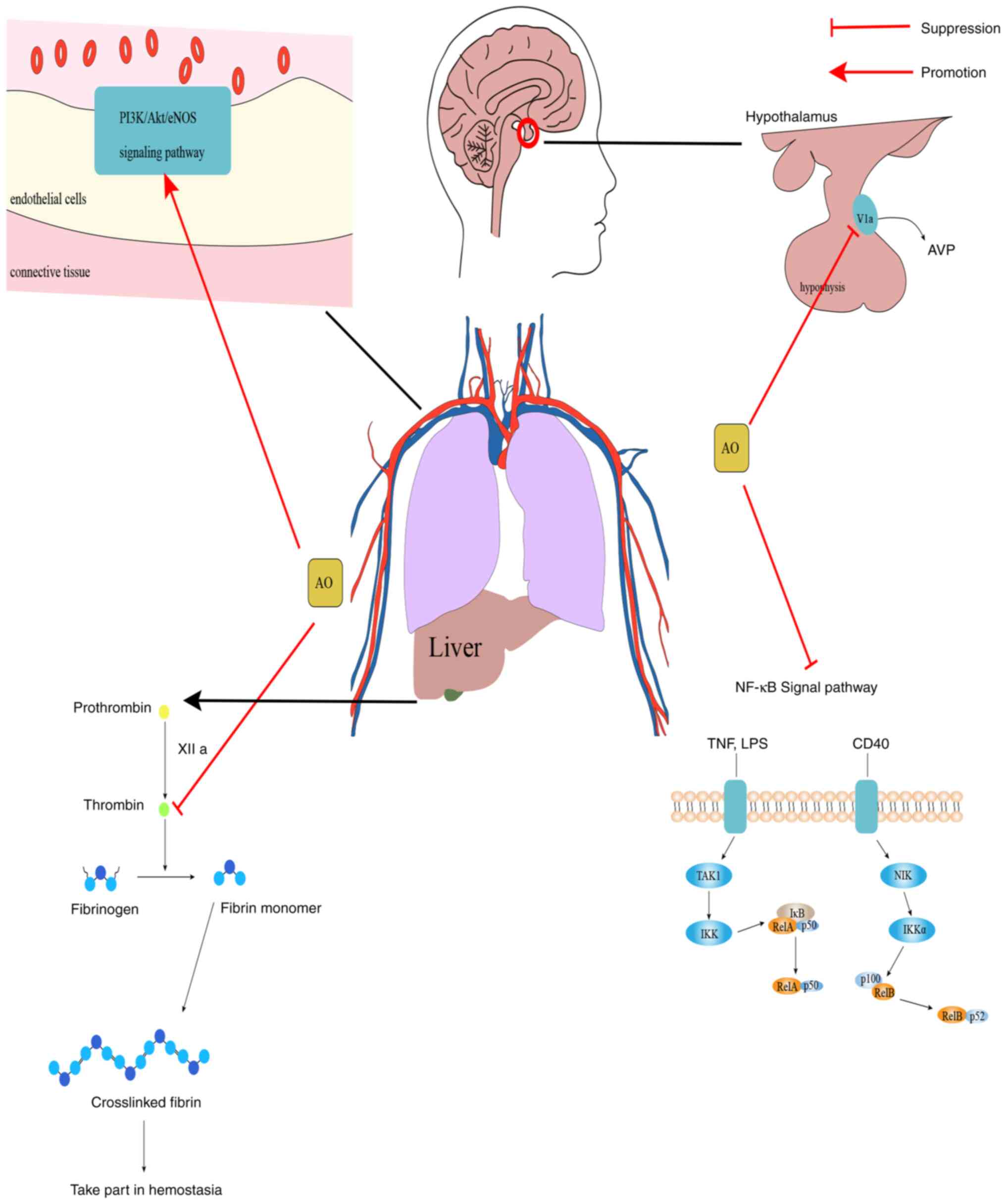
11
|
Panigrahi GK, Verma N, Singh N, Asthana S,
Gupta SK, Tripathi A and Das M: Interaction of anthraquinones of
Cassia occidentalis seeds with DNA and Glutathione. Toxicol Rep.
5:164–172. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhang N, Dong N, Pang L, Xu H and Ji H:
Quantitative determination and pharmacokinetic study of
aurantio-obtusin in rat plasma by liquid chromatography-mass
spectrometry. J Chromatogr Sci. 52:1059–1064. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nie C, Zhang F, Ma X, Guo R, Zhou S, Zhao
L, Xu H, Xiao X and Wang Z: Determination of quality markers of
Xuezhiling tablet for hyperlipidemia treatment. Phytomedicine.
44:231–238. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kwon KS, Lee JH, So KS, Park BK, Lim H,
Choi JS and Kim HP: Aurantio-obtusin, an anthraquinone from cassiae
semen, ameliorates lung inflammatory responses. Phytother Res.
32:1537–1545. 2018.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
He YQ, Zhou CC, Yu LY, Wang L, Deng JL,
Tao YL, Zhang F and Chen WS: Natural product derived phytochemicals
in managing acute lung injury by multiple mechanisms. Pharmacol
Res. 163(105224)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ahmed B, Sultana R and Greene MW: Adipose
tissue and insulin resistance in obese. Biomed Pharmacother.
137(111315)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Munafò A, Frara S, Perico N, Di Mauro R,
Cortinovis M, Burgaletto C, Cantarella G, Remuzzi G, Giustina A and
Bernardini R: In search of an ideal drug for safer treatment of
obesity: The false promise of pseudoephedrine. Rev Endocr Metab
Disord. 22:1013–1025. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Stadler JT and Marsche G: Obesity-Related
changes in high-density lipoprotein metabolism and function. Int J
Mol Sci. 21(8985)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mongioì LM, La Vignera S, Cannarella R,
Cimino L, Compagnone M, Condorelli RA and Calogero AE: The role of
resveratrol administration in human obesity. Int J Mol Sci.
22(4362)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Mayoral LP, Andrade GM, Mayoral EP, Huerta
TH, Canseco SP, Rodal Canales FJ, Cabrera-Fuentes HA, Cruz MM,
Pérez Santiago AD, Alpuche JJ, et al: Obesity subtypes, related
biomarkers & heterogeneity. Indian J Med Res. 151:11–21.
2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kuder MM and Nyenhuis SM: Optimizing
lifestyle interventions in adult patients with comorbid asthma and
obesity. Ther Adv Respir Dis. 14(1753466620906323)2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Purdy JC and Shatzel JJ: The hematologic
consequences of obesity. Eur J Haematol. 106:306–319.
2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ganesan SM, Vazana S and Stuhr S:
Waistline to the gumline: Relationship between obesity and
periodontal disease-biological and management considerations.
Periodontol 2000. 87:299–314. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Landecho MF, Marin-Oto M, Recalde-Zamacona
B, Bilbao I and Frühbeck G: Obesity as an adipose tissue
dysfunction disease and a risk factor for infections-Covid-19 as a
case study. Eur J Intern Med. 91:3–9. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Gammone MA and D'Orazio N: COVID-19 and
Obesity: Overlapping of two pandemics. Obes Facts. 14:579–585.
2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Guo CY, Liao WT, Qiu RJ, Zhou DS, Ni WJ,
Yu CP and Zeng Y: Aurantio-obtusin improves obesity and insulin
resistance induced by high-fat diet in obese mice. Phytother Res.
35:346–360. 2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yamashita S, Masuda D and Matsuzawa Y:
Pemafibrate, a new selective PPARα modulator: Drug concept and its
clinical applications for dyslipidemia and metabolic diseases. Curr
Atheroscler Rep. 22(5)2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Ciavarella C, Motta I, Valente S and
Pasquinelli G: Pharmacological (or Synthetic) and nutritional
agonists of PPAR-γ as candidates for cytokine storm modulation in
COVID-19 disease. Molecules. 25(2076)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Prabhakar PK: Pathophysiology of diabetic
secondary complication and their management. Curr Diabetes Rev.
17:395–396. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wang Z, Shen S, Cui Z, Nie H, Han D and
Yan H: Screening and isolating major aldose reductase inhibitors
from the seeds of evening primrose (Oenothera biennis). Molecules.
24(2709)2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Julius A, Renuka RR, Hopper W, Babu Raghu
P, Rajendran S, Srinivasan S, Dharmalingam K, Alanazi AM,
Arokiyaraj S and Prasath S: Inhibition of aldose reductase by novel
phytocompounds: A heuristic approach to treating diabetic
retinopathy. Evid Based Complement Alternat Med.
2022(9624118)2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Thakur S, Gupta SK, Ali V, Singh P and
Verma M: Aldose Reductase: A cause and a potential target for the
treatment of diabetic complications. Arch Pharm Res. 44:655–667.
2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Zhou Y, Chi J, Lv W and Wang Y: Obesity
and diabetes as high-risk factors for severe coronavirus disease
2019 (Covid-19). Diabetes Metab Res Rev. 37(e3377)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Dodda D, Rama Rao A and Veeresham C: In
vitro and in vivo evaluation of pterostilbene for the management of
diabetic complications. J Ayurveda Integr Med. 11:369–375.
2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Jang DS, Lee GY, Kim YS, Lee YM, Kim CS,
Yoo JL and Kim JS: Anthraquinones from the seeds of Cassia tora
with inhibitory activity on protein glycation and aldose reductase.
Biol Pharm Bull. 30:2207–2210. 2007.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Younossi ZM, Marchesini G, Pinto-Cortez H
and Petta S: Epidemiology of nonalcoholic fatty liver disease and
nonalcoholic steatohepatitis: Implications for liver
transplantation. Transplantation. 103:22–27. 2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Arrese M, Arab JP, Barrera F, Kaufmann B,
Valenti L and Feldstein AE: Insights into nonalcoholic fatty-liver
disease heterogeneity. Semin Liver Dis. 41:421–434. 2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
American Family Physician: Nonalcoholic
Fatty Liver Disease. https://www.aafp.org/pubs/afp/issues/2020/1115/p603-s1.html.
Accessed April 2, 2023.
|
|
39
|
Makri E, Goulas A and Polyzos SA:
Epidemiology, pathogenesis, diagnosis and emerging treatment of
nonalcoholic fatty liver disease. Arch Med Res. 52:25–37.
2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Friedman SL, Neuschwander-Tetri BA,
Rinella M and Sanyal AJ: Mechanisms of NAFLD development and
therapeutic strategies. Nat Med. 24:908–922. 2018.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Zhou F, Ding M, Gu Y, Fan G, Liu C, Li Y,
Sun R, Wu J, Li J, Xue X, et al: Aurantio-Obtusin attenuates
non-alcoholic fatty liver disease through AMPK-Mediated autophagy
and fatty acid oxidation pathways. Front Pharmacol.
12(826628)2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Galli SJ, Tsai M and Piliponsky AM: The
development of allergic inflammation. Nature. 454:445–454.
2008.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Hu T, Dong Y, Yang C, Zhao M and He Q:
Pathogenesis of children's allergic diseases: Refocusing the role
of the gut microbiota. Front Physiol. 12(749544)2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Yao Y, Chen CL, Yu D and Liu Z: Roles of
follicular helper and regulatory T cells in allergic diseases and
allergen immunotherapy. Allergy. 76:456–470. 2021.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Nguyen SMT, Rupprecht CP, Haque A,
Pattanaik D, Yusin J and Krishnaswamy G: Mechanisms governing
anaphylaxis: Inflammatory cells, mediators, endothelial gap
junctions and beyond. Int J Mol Sci. 22(7785)2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Xu-De Z, Bei-Bei G, Xi-Juan W, Hai-Bo L,
Li-Li Z and Feng-Xia L: Serum IgE Predicts difference of population
and allergens in allergic diseases: Data from Weifang City, China.
Mediators Inflamm. 2021(6627087)2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Zellweger F and Eggel A: IgE-associated
allergic disorders: Recent advances in etiology, diagnosis, and
treatment. Allergy. 71:1652–1661. 2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Kim M, Lim SJ, Lee HJ and Nho CW: Cassia
tora seed extract and its active compound aurantio-obtusin inhibit
allergic responses in IgE-Mediated mast cells and anaphylactic
models. J Agric Food Chem. 63:9037–9046. 2015.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Hou J, Gu Y, Zhao S, Huo M, Wang S, Zhang
Y, Qiao Y and Li X: Anti-Inflammatory effects of aurantio-obtusin
from seed of cassia obtusifolia L. through Modulation of the NF-κB
pathway. Molecules. 23(3093)2018.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Song JY, Casanova-Nakayama A, Möller AM,
Kitamura SI, Nakayama K and Segner H: Aryl hydrocarbon receptor
signaling is functional in immune cells of rainbow trout
(Oncorhynchus mykiss). Int J Mol Sci. 21(6323)2020.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Disner GR, Lopes-Ferreira M and Lima C:
Where the Aryl hydrocarbon receptor meets the microRNAs: Literature
review of the last 10 years. Front Mol Biosci.
8(725044)2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Yamashita N, Kanno Y, Yoshikawa M, Ozawa
M, Sanada N, Nemoto K and Kizu R: Polycyclic aromatic hydrocarbons
induce CYP3A5 gene expression via aryl hydrocarbon receptor in
HepG2 cells. J Toxicol Sci. 46:25–29. 2021.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Vogel CFA, Van Winkle LS, Esser C and
Haarmann-Stemmann T: The aryl hydrocarbon receptor as a target of
environmental stressors-Implications for pollution mediated stress
and inflammatory responses. Redox Biol. 34(101530)2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Amakura Y, Yoshimura M, Takaoka M, Toda H,
Tsutsumi T, Matsuda R, Teshima R, Nakamura M, Handa H and Yoshida
T: Characterization of natural aryl hydrocarbon receptor agonists
from cassia seed and rosemary. Molecules. 19:4956–4966.
2014.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Xu H, Bin NR and Sugita S: Diverse
exocytic pathways for mast cell mediators. Biochem Soc Trans.
46:235–247. 2018.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Lee EK, Song J, Seo Y, Koh EM, Kim SH and
Jung KJ: Inhibitory Effects of AF-343, a Mixture of Cassia tora L.,
Ulmus pumila L., and Taraxacum officinale, on Compound
48/80-Mediated Allergic Responses in RBL-2H3 Cells. Molecules.
25(2434)2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
WHO: Global health estimates:leading
causes of death. Cause specific mortality 2000-2019. WHO, Genova,
Switzerland, 2019.
|
|
58
|
Dumitrache MD, Jieanu AS, Scheau C,
Badarau IA, Popescu GDA, Caruntu A, Costache DO, Costache RS,
Constantin C, Neagu M and Caruntu C: Comparative effects of
capsaicin in chronic obstructive pulmonary disease and asthma
(Review). Exp Ther Med. 22(917)2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Chen YY, Yu MF, Zhao XX, Shen J, Peng YB,
Zhao P, Xue L, Chen W, Ma LQ, Qin G, et al: Paracetamol inhibits
Ca2+ permeant ion channels and Ca(2+) sensitization
resulting in relaxation of precontracted airway smooth muscle. J
Pharmacol Sci. 142:60–68. 2020.PubMed/NCBI View Article : Google Scholar
|
|
60
|
She YS, Ma LQ, Liu BB, Zhang WJ, Qiu JY,
Chen YY, Li MY, Xue L, Luo X, Wang Q, et al: Semen cassiae extract
inhibits contraction of airway smooth muscle. Front Pharmacol.
9(1389)2018.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Duong V, Lambrechts L, Paul RE, Ly S, Lay
RS, Long KC, Huy R, Tarantola A, Scott TW, Sakuntabhai A and Buchy
P: Asymptomatic humans transmit dengue virus to mosquitoes. Proc
Natl Acad Sci USA. 112:14688–14693. 2015.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Lee H, Halverson S and Ezinwa N:
Mosquito-Borne Diseases. Prim Care. 45:393–407. 2018.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Gan SJ, Leong YQ, Bin Barhanuddin MFH,
Wong ST, Wong SF, Mak JW and Ahmad RB: Dengue fever and insecticide
resistance in Aedes mosquitoes in Southeast Asia: A review. Parasit
Vectors. 14(315)2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Fillinger U and Lindsay SW: Larval source
management for malaria control in Africa: Myths and reality. Malar
J. 10(353)2011.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Raman Ibrahim NBB, Puchooa D,
Govinden-Soulange J and Facknath S: Cassia species: a potential
source of biopesticides. Journal of Plant Diseases and Protection.
128:339–351. 2021.
|
|
66
|
Mbatchou VC, Tchouassi DP, Dickson RA,
Annan K, Mensah AY, Amponsah IK, Jacob JW, Cheseto X, Habtemariam S
and Torto B: Mosquito larvicidal activity of Cassia tora seed
extract and its key anthraquinones aurantio-obtusin and obtusin.
Parasit Vectors. 10(562)2017.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Mbatchou VC, Dickson RA, Amponsah IK,
Mensah AY and Habtemariam S: Protection effect of the
anthraquinones, cassiatorin and aurantio-obtusin from seeds of
Senna tora against cowpea weevil attack. Asian Pac J Trop Biomed.
8:98–105. 2018.
|
|
68
|
Piplani M, Bhagwat DP, Singhvi G,
Sankaranarayanan M, Balana-Fouce R, Vats T and Chander S:
Plant-based larvicidal agents: An overview from 2000 to 2018. Exp
Parasitol. 199:92–103. 2019.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Lim H, Park BK, Shin SY, Kwon YS and Kim
HP: Methyl caffeate and some plant constituents inhibit age-related
inflammation: Effects on senescence-associated secretory phenotype
(SASP) formation. Arch Pharm Res. 40:524–535. 2017.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Birch J and Gil J: Senescence and the
SASP: Many therapeutic avenues. Genes Dev. 34:1565–1576.
2020.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Ohtani N: The roles and mechanisms of
senescence-associated secretory phenotype (SASP): Can it be
controlled by senolysis? Inflamm Regen. 42(11)2022.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Scheltens P, De trooper B, Kivipelto M,
Holstege H, Chételat G, Teunissen CE, Cummings J and van der Flier
WM: Alzheimer's disease. Lancet. 397:1577–1590. 2021.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Jung HA, Ali MY, Jung HJ, Jeong HO, Chung
HY and Choi JS: Inhibitory activities of major anthraquinones and
other constituents from Cassia obtusifolia against β-secretase and
cholinesterases. J Ethnopharmacol. 191:152–160. 2016.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Török B, Fazekas CL, Szabó A and Zelena D:
Epigenetic modulation of vasopressin expression in health and
disease. Int J Mol Sci. 22(9415)2021.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Watanabe J, Takayanagi Y, Yoshida M,
Hattori T, Saito M, Kohno K, Kobayashi E and Onaka T: Conditional
ablation of vasopressin-synthesizing neurons in transgenic rats. J
Neuroendocrinol. 33(e13057)2021.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Glavaš M, Gitlin-Domagalska A, Dębowski D,
Ptaszyńska N, Łęgowska A and Rolka K: Vasopressin and its
analogues: From natural hormones to multitasking peptides. Int J
Mol Sci. 23(3068)2022.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Al-Kuraishy HM, Al-Gareeb AI, Qusti S,
Alshammari EM, Atanu FO and Batiha GE: Arginine vasopressin and
pathophysiology of COVID-19: An innovative perspective. Biomed
Pharmacother. 143(112193)2021.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Mondritzki T, Mai TA, Vogel J, Pook E,
Wasnaire P, Schmeck C, Hüser J, Dinh W, Truebel H and Kolkhof P:
Cardiac output improvement by pecavaptan: A novel dual-acting
vasopressin V1a/V2 receptor antagonist in experimental heart
failure. Eur J Heart Fail. 23:743–750. 2021.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Szczepanska-Sadowska E, Wsol A,
Cudnoch-Jedrzejewska A and Żera T: Complementary role of oxytocin
and vasopressin in cardiovascular regulation. Int J Mol Sci.
22(11465)2021.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Che K, Muttenthaler M and Kurzbach D:
Conformational selection of vasopressin upon V1a
receptor binding. Comput Struct Biotechnol J. 19:5826–5833.
2021.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Sparapani S, Millet-Boureima C, Oliver J,
Mu K, Hadavi P, Kalostian T, Ali N, Avelar CM, Bardies M, Barrow B,
et al: The biology of vasopressin. Biomedicines.
9(89)2021.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Lago TR, Brownstein MJ, Page E, Beydler E,
Manbeck A, Beale A, Roberts C, Balderston N, Damiano E, Pineles SL,
et al: The novel vasopressin receptor (V1aR) antagonist SRX246
reduces anxiety in an experimental model in humans: A randomized
proof-of-concept study. Psychopharmacology (Berl). 238:2393–2403.
2021.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Paudel P, Kim DH, Jeon J, Park SE, Seong
SH, Jung HA and Choi JS: Neuroprotective effect of
aurantio-obtusin, a putative vasopressin V(1A) receptor antagonist,
on transient forebrain ischemia mice model. Int J Mol Sci.
22(3335)2021.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Lemmens-Gruber R and Kamyar M: Vasopressin
antagonists. Cell Mol Life Sci. 63:1766–1779. 2006.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Lemmens-Gruber R and Kamyar M:
Pharmacology and clinical relevance of vasopressin antagonists.
Internist (Berl). 49:628. 629–630, 632-4. 2008.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Ripoll GV, Pifano M, Garona J and Alonso
DF: Commentary: Arginine vasopressin receptor 1a is a therapeutic
target for castration-resistant prostate cancer. Front Oncol.
9(1490)2020.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Hu Y, Tao R, Chen L, Xiong Y, Xue H, Hu L,
Yan C, Xie X, Lin Z, Panayi AC, et al: Exosomes derived from
pioglitazone-pretreated MSCs accelerate diabetic wound healing
through enhancing angiogenesis. J Nanobiotechnology.
19(150)2021.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Li S, Wang Y, Wang Z, Chen L, Zuo B, Liu C
and Sun D: Enhanced renoprotective effect of GDNF-modified
adipose-derived mesenchymal stem cells on renal interstitial
fibrosis. Stem Cell Res Ther. 12(27)2021.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Chen C, Sun L, Zhang W, Tang Y, Li X, Jing
R and Liu T: Limb ischemic preconditioning ameliorates renal
microcirculation through activation of PI3K/Akt/eNOS signaling
pathway after acute kidney injury. Eur J Med Res.
25(10)2020.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Chen J, Huang Y, Hu X, Bian X and Nian S:
Gastrodin prevents homocysteine-induced human umbilical vein
endothelial cells injury via PI3K/Akt/eNOS and Nrf2/ARE pathway. J
Cell Mol Med. 25:345–357. 2021.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Xue X, Ling X, Xi W, Wang P, Sun J, Yang Q
and Xiao J: Exogenous hydrogen sulfide reduces atrial remodeling
and atrial fibrillation induced by diabetes mellitus via activation
of the PI3K/Akt/eNOS pathway. Mol Med Rep. 22:1759–1766.
2020.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Song W, Liang Q, Cai M and Tian Z:
HIF-1α-induced up-regulation of microRNA-126 contributes to the
effectiveness of exercise training on myocardial angiogenesis in
myocardial infarction rats. J Cell Mol Med. 24:12970–12979.
2020.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Li S, Li Q, Lv X, Liao L, Yang W, Li S, Lu
P and Zhu D: Aurantio-obtusin relaxes systemic arteries through
endothelial PI3K/AKT/eNOS-dependent signaling pathway in rats. J
Pharmacol Sci. 128:108–115. 2015.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Yu X, Wei LH, Zhang JK, Chen TR, Jin Q,
Wang YN, Zhang SJ, Dou TY, Cao YF, Guo WZ, et al: Anthraquinones
from Cassiae semen as thrombin inhibitors: In vitro and in silico
studies. Phytochemistry. 165(112025)2019.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Tarandovskiy ID, Artemenko EO, Panteleev
MA, Sinauridze EI and Ataullakhanov FI: Antiplatelet agents can
promote two-peaked thrombin generation in platelet rich plasma:
Mechanism and possible applications. PLoS One.
8(e55688)2013.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Varghese R, George Priya Doss C, Kumar RS,
Almansour AI, Arumugam N, Efferth T and Ramamoorthy S:
Cardioprotective effects of phytopigments via multiple signaling
pathways. Phytomedicine. 95(153859)2022.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Alkarithi G, Duval C, Shi Y, Macrae FL and
Ariëns RAS: Thrombus structural composition in cardiovascular
disease. Arterioscler Thromb Vasc Biol. 41:2370–2383.
2021.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Wu H, Wang Y, Zhang Y, Xu F, Chen J, Duan
L, Zhang T, Wang J and Zhang F: Breaking the vicious loop between
inflammation, oxidative stress and coagulation, a novel
anti-thrombus insight of nattokinase by inhibiting LPS-induced
inflammation and oxidative stress. Redox Biol.
32(101500)2020.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Zhao Y, Xie R, Yodsanit N, Ye M, Wang Y,
Wang B, Guo LW, Kent KC and Gong S: Hydrogen peroxide-responsive
platelet membrane-coated nanoparticles for thrombus therapy.
Biomater Sci. 9:2696–2708. 2021.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Williams LM and Gilmore TD: Looking Down
on NF-κB. Mol Cell Biol. 40:e00104–20. 2020.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Harrold AP, Cleary MM, Bharathy N, Lathara
M, Berlow NE, Foreman NK, Donson AM, Amani V, Zuercher WJ and
Keller C: In vitro benchmarking of NF-κB inhibitors. Eur J
Pharmacol. 873(172981)2020.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Son M, Wang AG, Tu HL, Metzig MO, Patel P,
Husain K, Lin J, Murugan A, Hoffmann A and Tay S: NF-κB responds to
absolute differences in cytokine concentrations. Sci Signal.
14(eaaz4382)2021.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Yang B, Xie Y, Guo M, Rosner MH, Yang H
and Ronco C: Nephrotoxicity and Chinese Herbal Medicine. Clin J Am
Soc Nephrol. 13:1605–1611. 2018.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Liu Y, Mapa MST and Sprando RL: Liver
toxicity of anthraquinones: A combined in vitro cytotoxicity and in
silico reverse dosimetry evaluation. Food Chem Toxicol.
140(111313)2020.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Yang J, Zhu A, Xiao S, Zhang T, Wang L,
Wang Q and Han L: Anthraquinones in the aqueous extract of Cassiae
semen cause liver injury in rats through lipid metabolism disorder.
Phytomedicine. 64(153059)2019.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Hu M, Lin L, Liu J, Zhong Y, Liang B,
Huang Y, Li Z, Lin X, Wang B, Zhang B, et al: Aurantio-obtusin
induces hepatotoxicity through activation of NLRP3 inflammasome
signaling. Toxicol Lett. 354:1–13. 2022.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Wang J, Zhao Y, Xiao X, Li H, Zhao H,
Zhang P and Jin C: Assessment of the renal protection and
hepatotoxicity of rhubarb extract in rats. J Ethnopharmacol.
124:18–25. 2009.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Yu J, Han JC and Gao YJ: Biotransformation
of glucoaurantio-obtusin towards aurantio-obtusin increases the
toxicity of irinotecan through increased inhibition towards SN-38
glucuronidation. Phytother Res. 28:1577–1580. 2014.PubMed/NCBI View Article : Google Scholar
|