Introduction
Ischemic colitis (IC) is an ischemic injury to the
colon caused by an occlusive arterial blood supply, blocked venous
return (1), or by insufficient
blood supply to the colon (2).
Abdominal pain, bloody stools and diarrhea are often the triad of
clinical manifestations (3). It
commonly occurs in older individuals, and the incidence increases
with age (3). IC usually includes
colon ischemia, acute mesenteric ischemia (AMI) and chronic
mesenteric ischemia (CMI) (4).
Ahmed et al (4) reported
that colon ischemia is the most common type followed by AMI and CMI
epidemiologically.
Colon cast (CC) is a rare clinical type of IC that
was first reported by Speakman and Turnbull in 1984(5). Abe et al (6) reported that only 23 cases were
published before 2014.Su et al (7), and Feuerstadt and Brandt (8) also reported a few cases. The main
cause of CC is acute colonic ischemia, and the majority of the
cases are secondary to abdominal aortic aneurysm repairs. Invasive
treatment is required, as it is likely to develop into colonic
stenosis, obstruction and bowel perforation (6). In some cases, the causes include
diabetic ketoacidosis, trauma, pancreatitis, graft-versus-host
disease and ischemic colitis secondary to arteriosclerotic
cardiovascular disease; there are also some cases caused by
ischemic colitis from preceding circulatory disorders (6). The cases that always occur with
severe symptoms and involve the intrinsic muscle layer should be
treated with operations. Only a few cases occur with mild symptoms
and involve infarction limited to the colonic mucosa layer, and
these can be successfully treated by conservative therapies,
including endoscopic dilation (6).
However, there are no such cases of CC reported in mainland China.
To improve our understanding of this disease, the present study
reported a case of CC.
Case presentation
An 80-year-old male patient visited The Affiliated
People's Hospital of Ningbo University (Ningbo, China) due to
abdominal pain and bloody stools for 1 day. The patient had no
significant comorbidities and was not taking any medication. The
patient had no past severe systemic diseases. He had no history of
alcohol consumption or smoking, and he had no family history of
illness. Physical examination suggested tenderness in the left
lower abdomen. Laboratory tests showed positive fecal occult blood.
Routine blood tests, blood coagulation function, D-dimer check and
other tests were all normal. Abdominal computed tomography (CT)
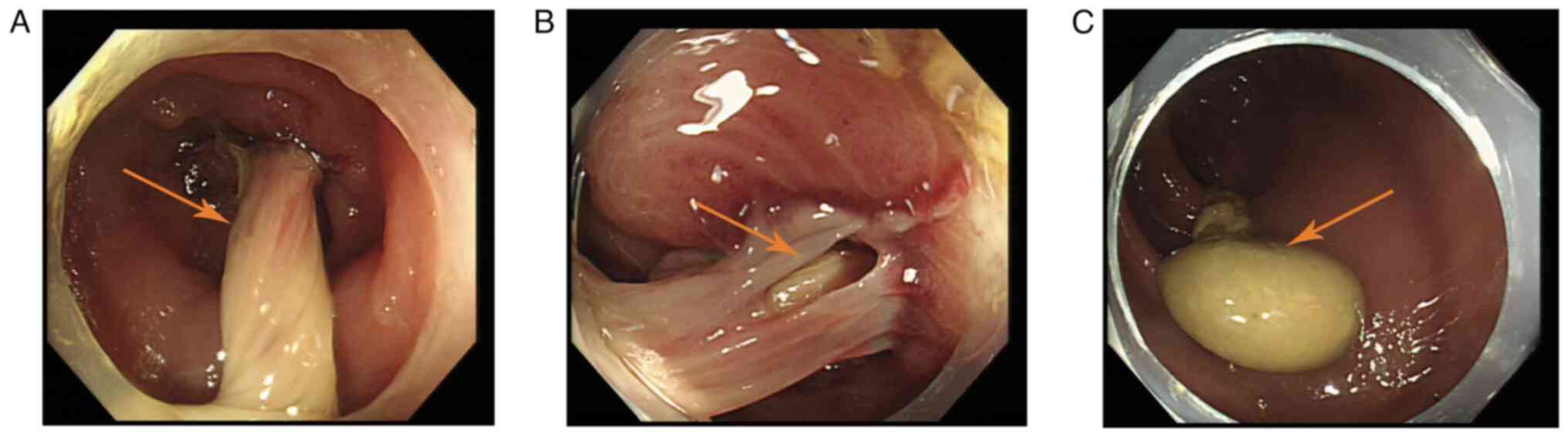
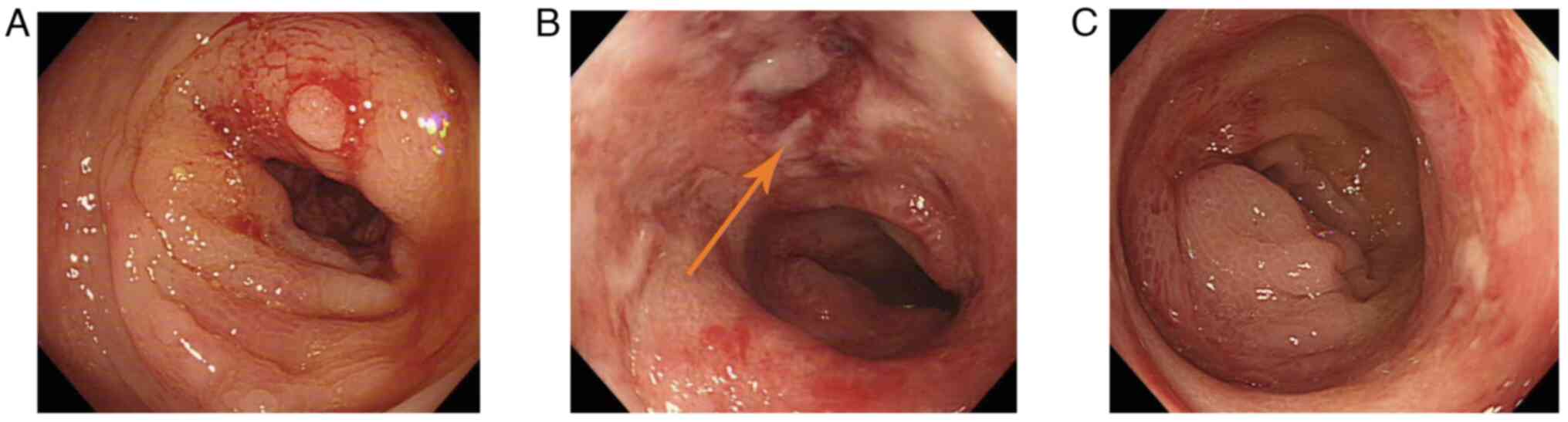
revealed thickening of the sigmoid colon wall. Diagnostic endoscopy
was conducted, which revealed narrowing of the sigmoid colon. There
was a long strip of tissue in the sigmoid cavity with a cystic and
smooth head, and the base of the pedicle was edematous and erosive
(Fig. 1). Further examination by
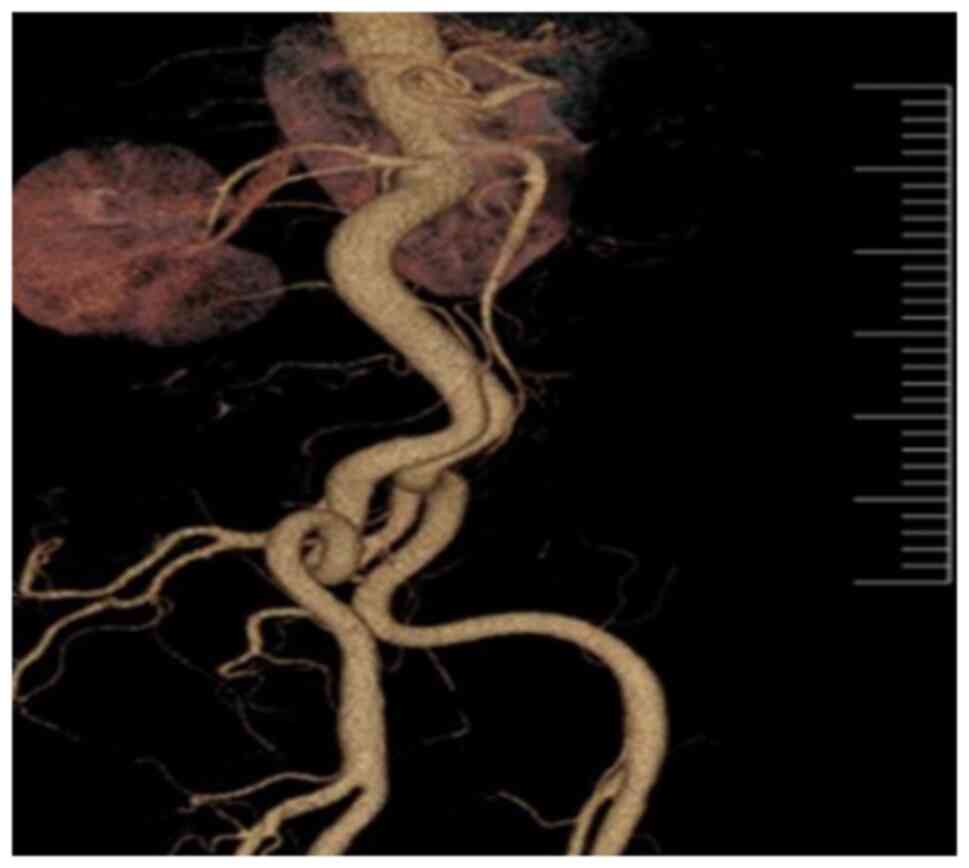
CT angiography revealed thickening of the sigmoid wall and no
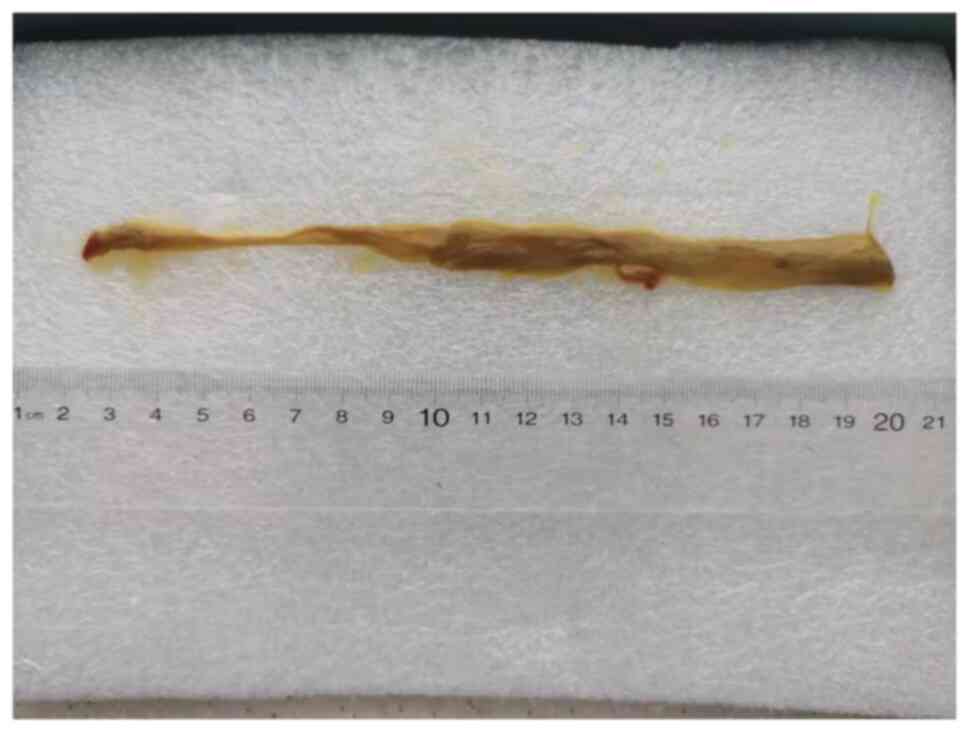
abnormality of the mesenteric artery (Fig. 2). The day after colonoscopy, the
patient expelled a 17-cm strip of tissue that was the eroded
colonic mucosa (Fig. 3) from his
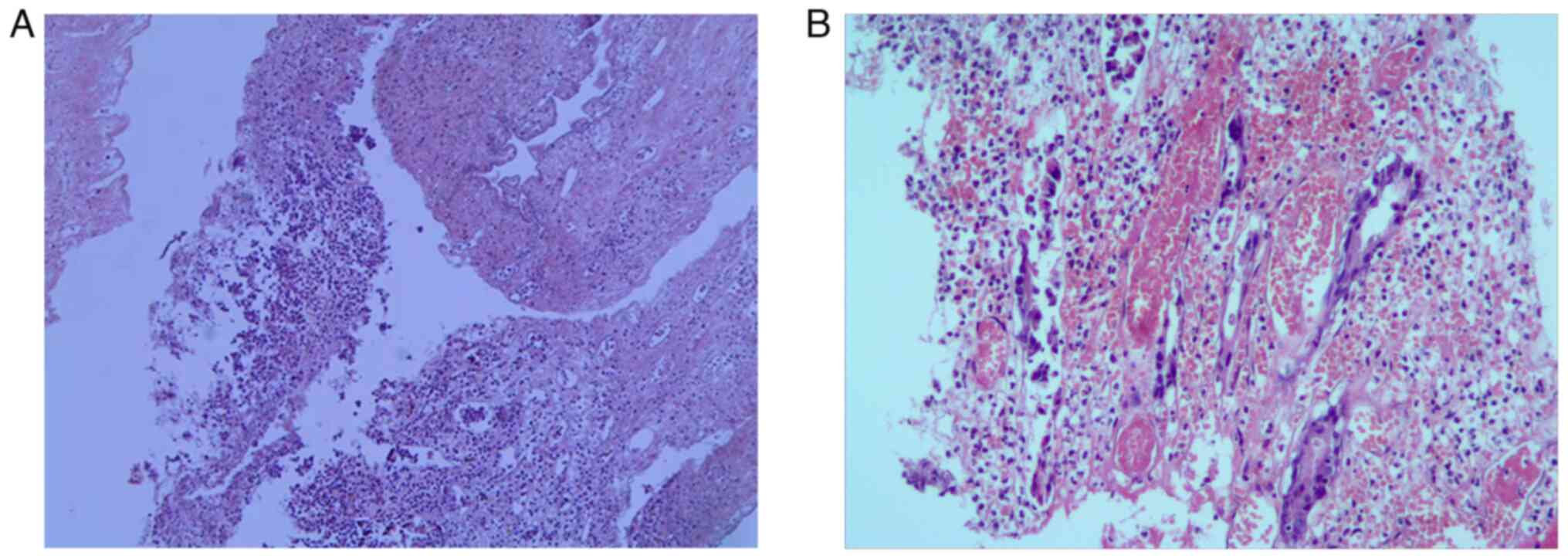
anus and developed fever of 38.5˚C. Pathological examination with
hematoxylin and eosin staining (25˚C, 45 min) revealed an
inflammatory, necrotic colonic mucosa (Fig. 4). After 1 week, re-examination by
colonoscopy revealed that the strip had been shed, the sigmoid
mucosa was edematous and anabrotic, but other intestinal segments
were normal (Fig. 5).
After reviewing the relevant literature, the present
study concluded that this was a rare type of IC called CC. The
patient was treated by fasting for 5 days and anti-inflammatory
medication consisting of cefmetazole (2.0 g twice a day) for 5 days
and low molecular weight heparin (5,000 IU) as anticoagulant
therapy for 1 week. He recovered well and was discharged after
remission. He has been followed up for 1 year without relapse.
Discussion
CC is a rare clinical type of IC. Studies have shown
that colon hypoperfusion and reperfusion injury are involved in the
occurrence of IC (9,10). Colonoscopy combined with
histopathological biopsy is the gold standard for the diagnosis of
IC (11). The endoscopic
manifestations of typical patients with IC are a clear demarcation
between the pathological and normal mucosa, and the common
endoscopic manifestations include congestion, edema, erosion,
intestinal stenosis and hemorrhage (9,12).
The dark blue nodules with dusty background often indicate gangrene
during endoscopic tests (12).
However, CC often confuses the diagnosis because of its non-typical
symptoms (13).
This type of IC presents insidiously, with abdominal
pain, distension, watery bloody stools, fever and elevated white
blood cell count. In addition, erythrocyte sedimentation rate
increases, which peaks after several weeks. The necrotic intestinal
tissue is discharged from the anus. The clinical manifestations,
colonoscopy, blood test and CT angiography results of the current
patient were consistent with those reported in the literature for
CC (14).
At present, the pathogenesis of CC is still not
clear. Most cases have been reported secondary to abdominal aortic
aneurysm or mesenteric thrombosis (6). However, abdominal CT angiography of
the current patient showed no vascular abnormalities; therefore,
the present study hypothesizes that the pathogenesis of CC needs to
be further explored.
According to previous case reports, the lesions of
tubular IC are all located in the left colon; the rectum is often
not involved, and as such IC occurring in the right colon has not
been reported (6,13). The present case is consistent with
the literature. We hypothesize that this may be related to the
characteristics of colorectal vascular anatomy and blood perfusion.
The colon is supplied by the superior mesenteric artery, inferior
mesenteric artery and superior rectal artery. The splenic curvature
of the colon and sigmoid colon are special, because of the limited
collateral circulation in these two regions (15). Therefore, the left colon is the
site most easily involved in IC, while rectal ischemia is less
common, because it has a relatively rich double blood supply
(15). In 2014, Abe et al
(6) reported that the incidence of
IC was 82.6% (19/23) in the left colon. In 2015, Cruz et al
(13) reported that the incidence
of IC was 62.7% (64/102) in the descending colon and 56.9% (58/102)
in the sigmoid colon, and that the splenic curvature was rarely
involved.
The initially reported cases of CC are marked by
prompt interventions following the cast passage, presumably because
of a desire to discover the pathology or fear of missing a lethal
condition (16). The necessity for
surgery is controversial. Foley et al (17) recommends that patients should
undergo conservative treatment for a period of time to rest the
bowel and use broad-spectrum antibiotics to cover the fecal flora
to minimize intestinal ischemia. In the present case, acute
abdominal pain and bloody stools were the main manifestations in
the early stage of the disease, and intestinal obstruction and
fever appeared later. After fasting, anti-inflammatory treatment
with cefmetazole and fluid infusion, the condition of the patient
gradually improved. On the second day after colonoscopy, the
patient discharged the intestinal mucosa from the anus, and the
intestinal obstruction and intestinal infection were gradually
relieved. At 1 week later, colonoscopy showed that the symptoms of
ischemic edema and intestinal stenosis were significantly
improved.
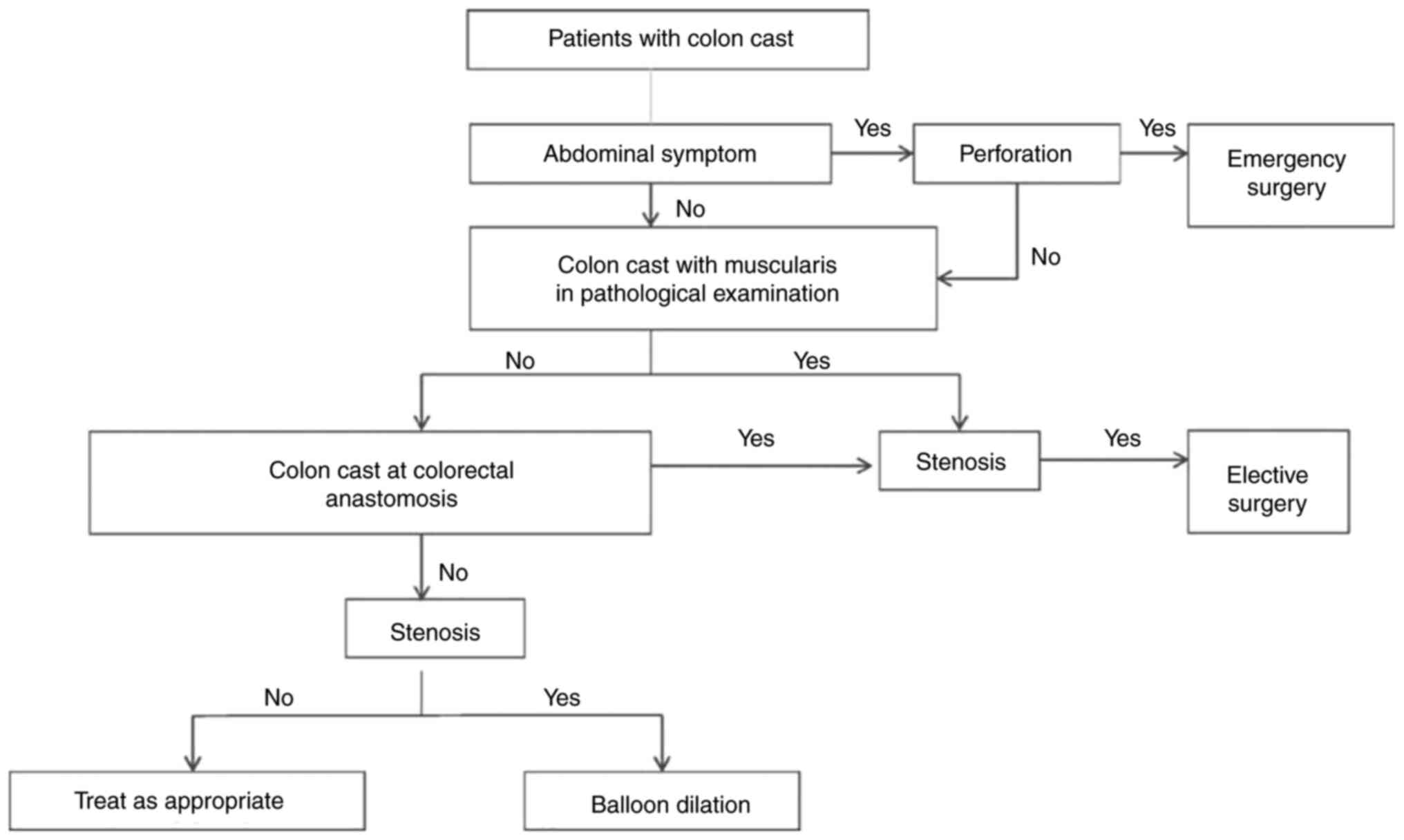
During diagnosis and treatment of the patient, the
present study revealed that the intestinal mucosal lesions of this
type of IC could cause intestinal obstruction after forming tubular
channels, and the CC was discharged from the anus after necrosis
and shedding (14,18). The severity of the colonic mucosal
ischemia determines the treatment (19). If pathological examination suggests
that the lesions only affect the mucosa and submucosa and not the
intrinsic muscle layer, IC including AMI and CMI, as well as CC can
be treated conservatively, including the usage of broad-spectrum
antibiotics, anticoagulants or nutritional supplementation, and the
symptoms will disappear gradually, with no long-term sequelae
(19). These cases are the
so-called mild cases. To the best of our knowledge, such cases have
not been reported before in mainland China. If the lesions affect
deeper than the intrinsic muscle layer, they cause bowel stenosis
or persistent colonic inflammation, which leads to chronic
intestinal obstruction, gangrene and peritonitis. In these cases,
emergency surgery cannot be avoided (19). If the cases have colorectal
anastomosis or the lesion contains muscularis propria, surgical
treatment was also suggested (Fig.
6).
The correct diagnosis and treatment of CC is
important for a favorable outcome. Abe et al (6) reported that the pathologic depth of
the layer of the excreted colon cast may be the key element in
determining the appropriate treatment, if the lesions consisting of
the mucosa/submucosa layer alone, without colorectal anastomosis
might likely be managed by conservative therapy. Although less
severe mild cases may present with similar symptoms, the prognosis
and management are completely different depending on severity of
the colonic mucosal ischemia and they are managed conservatively
rather than surgically (20). In
the present case, no gangrene was found by colonoscopy, and
pathological examination indicated that the ischemia only involved
the mucosal layer; therefore, it was a mild case of CC and could be
cured by conservative medical treatment.
However, there are limitations to the present study,
this was a single rare case, and the diagnostic and therapeutic
experience for CC is limited because of the rarity of the disease.
Therefore, further studies are needed to improve understanding of
the comorbidities, pathology, diagnosis and treatment of CC.
In conclusion, CC is a rare type of IC. The
diagnosis of CC should be based on the clinical presentation and
pathological colonoscopy examination, and the depth of the layer of
CC might be the key element in determining the appropriate
treatment. Conservative therapy is also an effective treatment in
the cases consisting of mucosa/submucosa layer, such as in the
present case. The present case will improve our understanding of
comorbidities, pathology, diagnosis and treatment of CC and IC.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JS performed the colonoscopy, reviewed the
literature, and contributed to manuscript drafting. GC performed
the pathological work. MZ designed the study and was responsible
for manuscript drafting and analysis. JS and MZ confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate.
Not applicable.
Patient consent for publication
The patient provided written informed consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Brandt LJ, Feuerstadt P, Longstreth GF and
Boley SJ: American College of Gastroenterology. ACG clinical
guideline: Epidemiology, risk factors, patterns of presentation,
diagnosis, and management of colon ischemia (CI). Am J
Gastroenterol. 110:18–44. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Rania H, Mériam S, Rym E, Hyafa R, Amine
A, Najet BH, Lassad G and Mohamed TK: Ischemic colitis in five
point: An update 2013. Tunis Med. 92:299–303. 2014.PubMed/NCBI
|
|
3
|
Yngvadottir Y, Karlsdottir BR, Hreinsson
JP, Ragnarsson G, Mitev RUM, Jonasson JG, Möller PH and Björnsson
ES: The incidence and outcome of ischemic colitis in a
population-based setting. Scand J Gastroenterol. 52:704–710.
2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ahmed M: Ischemic bowel disease in 2021.
World J Gastroenterl. 27:4746–4762. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Speakman MJ and Turnbull AR: Passage of a
colon ‘cast’ following resection of an abdominal aortic aneurysm.
Br J Surg. 71(935)1984.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Abe S, Yamaguchi H, Murono K, Kanazawa T,
Ishihara S, Sunami E and Watanabe T: Passage of a sigmoid colon
cast in a patient with ischemic colitis. Int Surg. 99:500–505.
2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Su TH, Liou JM and Wang HP: The passage of
a colonic cast. Lancet. 375(2099)2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Phillips RK and Armitage NC: Colon ‘cast’
in a patient with ischaemic colitis. Br J Surg. 74:759–760.
1987.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Feuerstadt P and Brandt LJ: Update on
colon ischemia: Recent insights and advances. Curr Gastroenterol
Rep. 17(45)2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Feuerstadt P and Brandt LJ: Colon
ischemia: recent insights and advances. Curr Gastroenterol Rep.
12:383–390. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Xu Y, Xiong L, Li Y, Jiang X and Xiong Z:
Diagnostic methods and drug therapies in patients with ischemic
colitis. Int J colorectal Dis. 36:47–56. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Montoro MA, Brandt LJ, Santolaria S,
Gomollon F, Sánchez Puértolas B, Vera J, Bujanda L, Cosme A,
Cabriada JL, Durán M, et al: Clinic patterns and outcomes of
ischaemic colitis: Results of the working group for the study of
ischemic colitis in Spain (CIE study). Scand J Gastroenterol.
46:236–246. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cruz C, Abujudeh HH, Nazarian RM and
Thrall JH: Ischemic colitis: Spectrum of CT findings, sites of
involvement and severity. Emerg Radiol. 22:357–365. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mantas D, Damaskos C, Bamias G and
Dimitroulis D: Colonic casts: Unexpected complications of colonic
ischaemia. Ann R Coll Surg Engl. 98:e109–e110. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Brandt LJ, Feueratadt P and Blaszka MC:
Anatomic patterns, patient characteristics and clinical outcomes in
ischemic colitis: A study of 313 cases supported by histology. Am J
Gastroenterol. 105:2245–2252. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Gregory PJ and Barrett G: Spontaneous
passage of a colon ‘cast’ in a patient with ischemic colitis. Br J
Surg. 74(436)1987.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Foley CL, Taylor CJ, Aslam M, Reddy KP,
Birch HA and Owen ER: Failure of conservative management after the
passage of a distal colonic ‘cast’: Report of a case. Dis Colon
Rectum. 48:1090–1093. 2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Park YM, Lee CK and Kim HJ:
Gastrointestinal: Colon cast with segmental stricture following
colonic ischemia. J Gastroenterol Hepatol. 34:630. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Erguney S, Yavuz N, Ersoy YE, Teksoz S,
Selcuk D, Ogut G, Dogusoy G and Alver O: Passage of ‘Colonic Cast’
after colorectal surgery: Report of four cases and review of the
literature. J Gastrointest Surg. 11:1045–1051. 2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Maimone A, De Ceglie A, Siersema PD, Baron
TH and Conio M: A comprehensive review. Clin Res Hepatol
Gastroenterol. 45(101592)2021.
|