Introduction
Esophageal foreign body impaction is a common
emergency of the digestive system, with >150,000 reports to
American Poison Centers every year (1). The condition most frequently occurs
at three physiological strictures (including the level of the
cricopharyngeus muscle, the aortic arch/left mainstem bronchus and
the esophageal hiatus of the diaphragm) (2) due to the ingestion of fish bones,
toys and missing dentures by mistake. The main clinical
manifestations are esophageal foreign body sensation, difficulty
swallowing and pain behind the sternum (3). In severe cases, patients may
experience perforation, obstruction, formation of an
aorto-esophageal and/or tracheoesophageal fistula (4). The foreign body may also pierce large
blood vessels and lead to mortality (5).
Vascular damage adjacent to the foreign object is
one of the most serious complications reported. In 2019, Zhao et
al (6) reported that a
53-year-old female patient succumbed to hemorrhagic shock due to a
fish bone penetrating the left subclavian artery. In another case
in 2021, a 40-year-old male patient experienced hemorrhagic shock,
aortoesophageal fistula and thoracic aorta pseudoneurysm (7). It was caused by a fish bone that was
2.5-cm long near the sixth thoracic vertebra (7). Therefore, esophageal foreign body
objects can present a danger to the lives of patients. It is
important to find suitable methods for removing fish bones as soon
as possible.
To the best of our knowledge, in the previous
reports (8-10)
on the removal of esophageal foreign bodies, fibro-bronchoscopy was
not used in conjunction with gastroscopy, as it is mainly used in
the airways. The aim of the present case was to document a case of
a patient with a fish bone trapped in the esophagus, which lied
adjacent to the thoracic aorta and was at high-risk of puncturing
it. It was finally removed using the combination of gastroscopy and
fibro-bronchoscopy.
Case report
A 22-year-old female patient was admitted to Chengdu
First People's Hospital (Chengdu, China) in January 2023 due to a
foreign body sensation in the throat 6 h after eating fish.
Discomfort in the pharynx and sternum were the main symptoms,
without other obvious symptoms. There were no significant findings
from the physical examination. The patient did not receive any
other treatments before being admitted to the hospital.
No significant abnormalities were revealed from the
results of the laboratory tests, including routine blood, liver
function, kidney function, electrolytes and coagulation tests
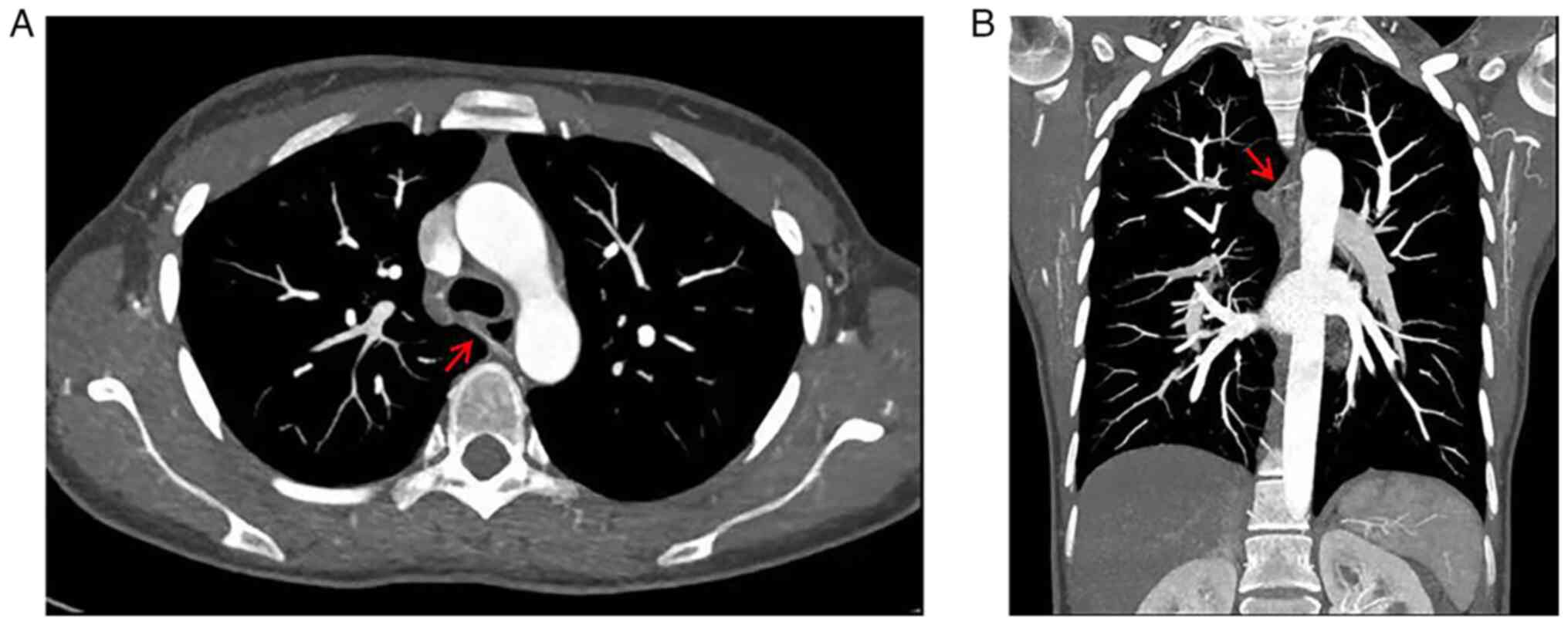
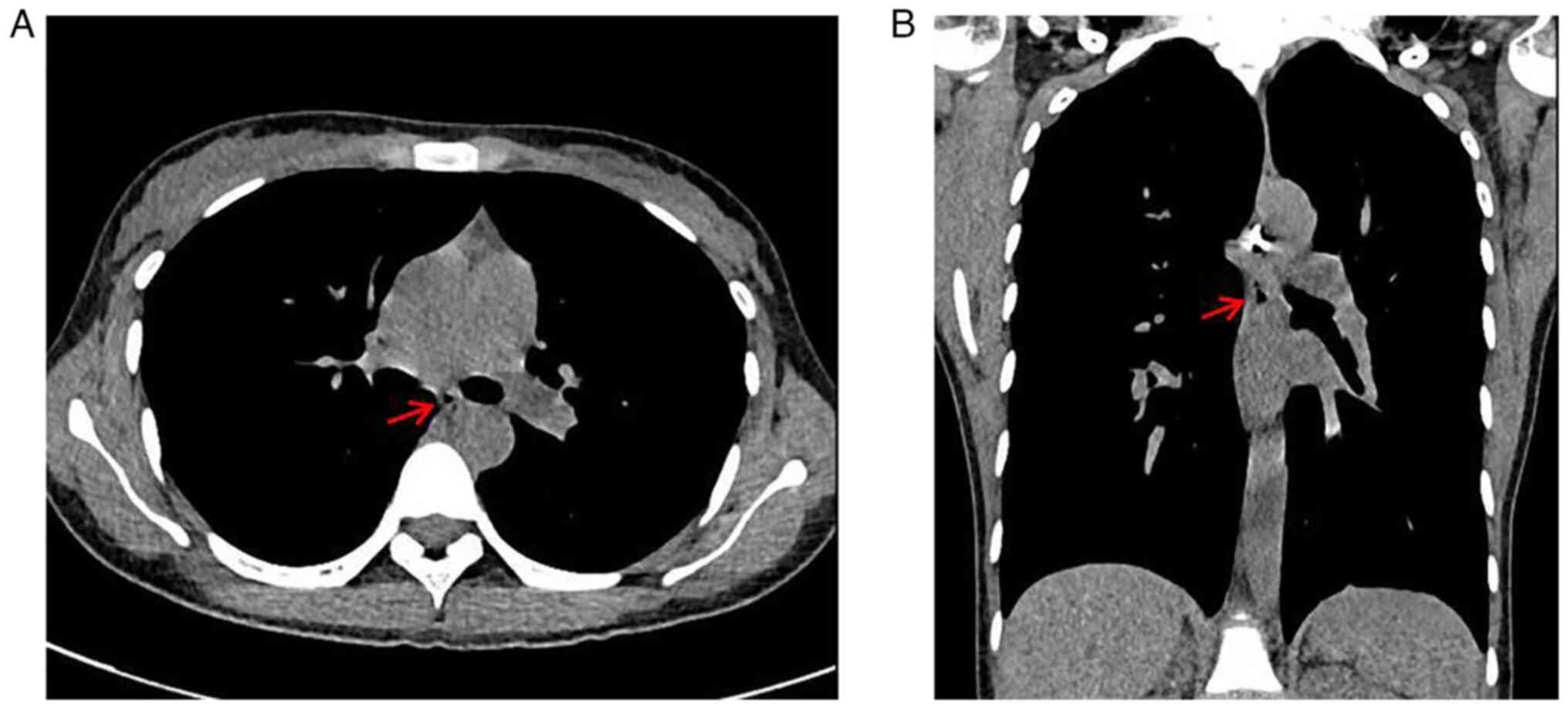
(Table I). Thoracic CT and
thoracic-aorta CT angiography scanning indicated a foreign body in
the middle third of the esophagus. The length of esophageal foreign
body was ~3.0 cm. The right end of the foreign body had pierced the
esophageal wall and reached the tracheal carina, where the distance
between the left end of the foreign body and the aortic wall was
<0.1 cm (Fig. 1). Therefore,
the patient was diagnosed with esophageal foreign body
impaction.
 | Table IMain indicators from routine blood,
liver function, renal function, electrolyte and coagulation
laboratory tests. |
Table I
Main indicators from routine blood,
liver function, renal function, electrolyte and coagulation
laboratory tests.
| Indicators | Results | Sign | Normal range |
|---|
| Red blood cell,
x1012/l | 4.62 | - | 3.80-5.10 |
| White blood cell,
x109/l | 8.88 | - | 3.50-9.50 |
| Neutrophil, % | 80.80 | Up | 50.00-70.00 |
| Platelets,
x109/l | 189.00 | - | 100.00-300.00 |
| High-sensitivity
C-reactive protein, mg/l | 0 | - | 0-10.00 |
| Total bilirubin,
µmol/l | 10.30 | - | 1.70-28.00 |
| Albumin, g/l | 43.20 | - | 35.00-55.00 |
| Alanine
aminotransferase, U/l | 10.00 | - | 0-50.00 |
| Aspartate
aminotransferase, U/l | 19.00 | - | 0-50.00 |
| Creatinine,
µmol/l | 52.00 | - | 45.00-84.00 |
| Ca2+,
mmol/l | 2.19 | - | 2.09-2.54 |
| K+,
mmol/l | 3.70 | - | 3.50-5.30 |
| Na+,
mmol/l | 134.00 | Down | 135.00-145.00 |
| Prothrombin time,
sec | 10.40 | - | 9.00-14.00 |
| Activated partial
thromboplastin time, sec | 27.90 | - | 20.00-40.00 |
Specifically, one end of the esophageal foreign body
was close to the thoracic aorta and there was high risk of it
puncturing the aorta. After multidisciplinary consultation, it was
considered that the first step was to perform endoscopic foreign
body removal; if this failed, thoracoscopy or thoracotomy would be
required. To ensure the right of the patient to life and health,
the patient and their family was informed regarding the treatment
plan and the risks involved, before subsequently consent was
obtained. After completing preoperative preparation, the surgery to
remove the foreign body was performed under general anesthesia and
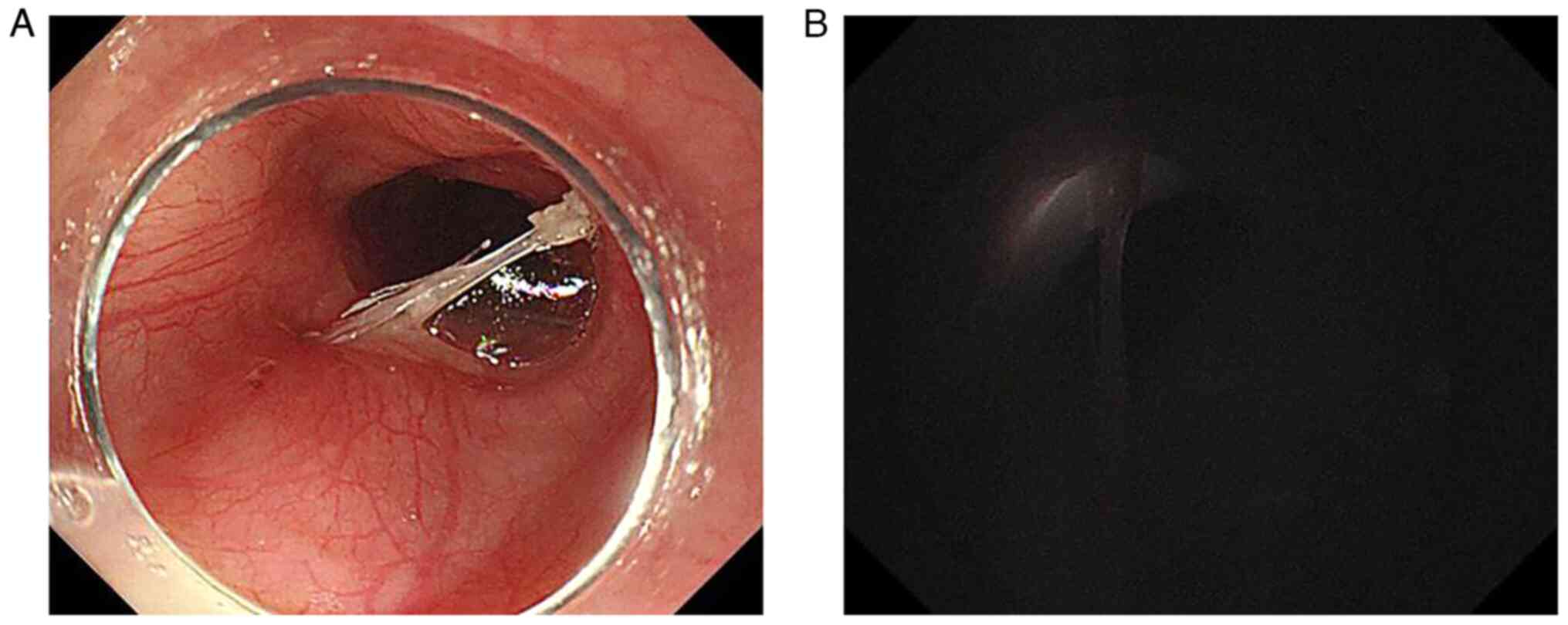
gastroscopy. During the operation, a white strip of fish bone was
revealed to be embedded on both sides of the esophageal wall ~25 cm
from the incisor teeth under gastroscopy (Fig. 2A). One end of the fish bone had
become fan-shaped with burrs, whilst the other end penetrated the
esophageal wall in a complete strip shape.
To maximize the safety of the patient and verify the
locations of the two ends of the fish bone under gastroscopy,
fibro-bronchoscopy was performed during the operation. Under
fibro-bronchoscopy, it was revealed that the fish bone had pierced
the bronchus. In addition, when the light source of the gastroscope
was turned off, the light source of the fiberoptic-bronchoscope
could be observed through the bronchial and esophageal walls
(Fig. 2B). Subsequently, the
fiberoptic bronchoscope was removed and the light source of
gastroscope was turned on. Due to limitations in available tools,
the fish bone could not be cut in half. Biopsy forceps were used to
clamp the left end of the fish bone under gastroscopy, repeatedly
pulling it towards the right end to free the left end of the fish
bone. During this process, the left end was fixed as much as
possible to reduce movement and risk. Immediately, biopsy forceps
were used to keep clamping the left free end of the fish bone, and
successfully remove the right end of the fish bone outside the
body.
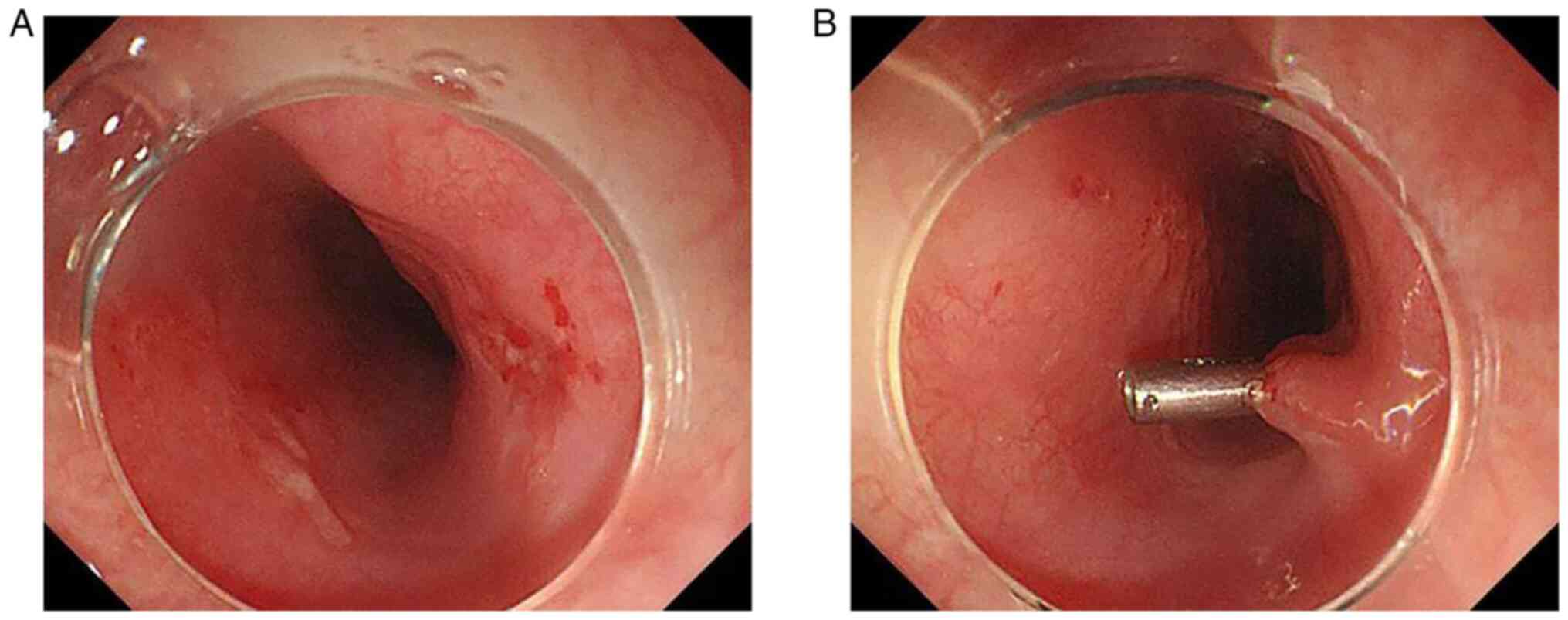
It was observed that the mucosa of the left
esophageal wall in contact with the foreign body was congested and
eroded under the endoscope, but no exact fistula formation was
observed. By contrast, the mucosa of the right esophageal wall in
contact with the foreign body was more eroded and congested with
edematous compared with that of the left wall, but no obvious
fistula opening could be observed either (Fig. 3). Finally, the right wound was
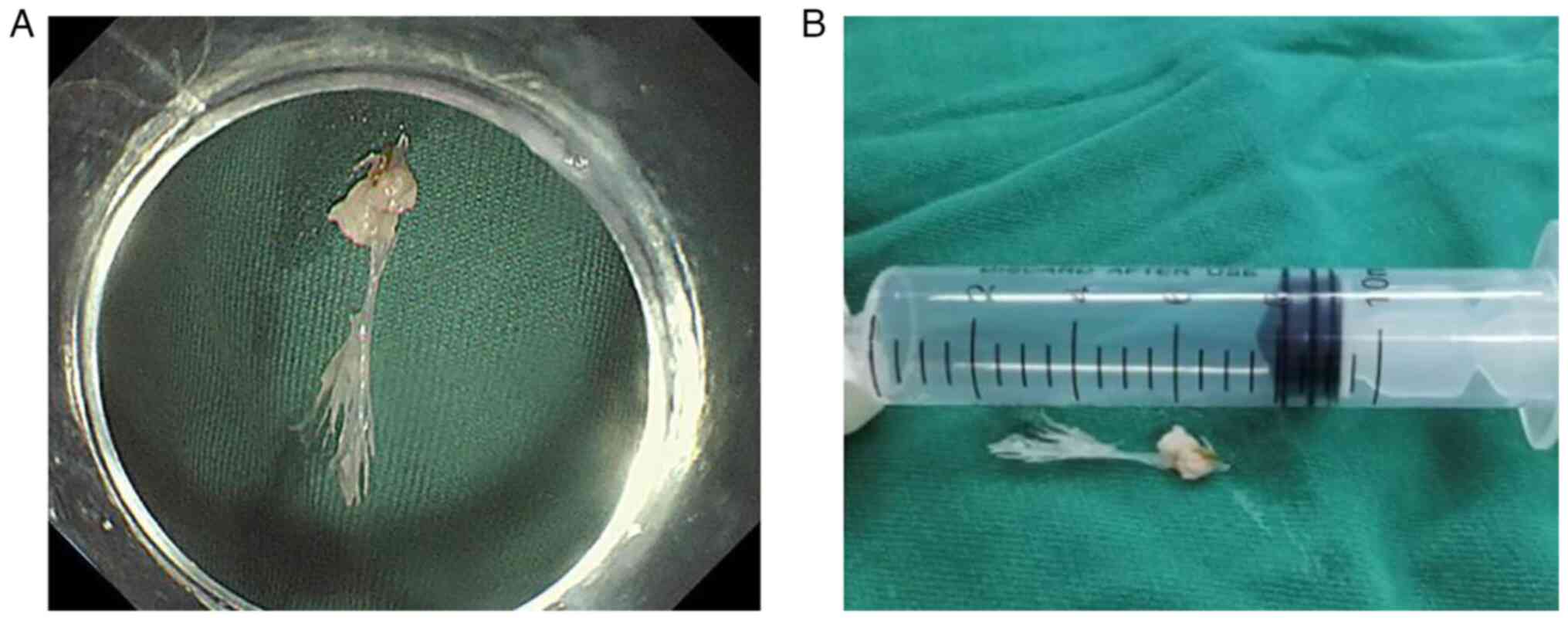
closed with a titanium clip. The ~2.7 cm foreign body was
completely removed (Fig. 4) and
the injury of thoracic aorta was avoided.
Postoperative gastrointestinal decompression was
performed, followed by prohibition of food and drink for 48 h.
However, the patient received a 250-ml compound amino acid
injection (18AA) via an intravenous drip twice a day, a 250-ml
medium/long chain fat emulsion injection via an intravenous drip
once a day, fluid infusion (400 ml 10% glucose injection, 100 ml
50% glucose injection and 15 ml 10% potassium chloride injection)
via an intravenous drip once a day, acid-suppression (250 ml 5%
glucose injection and Famotidine 20 mg) via an intravenous drip
twice a day and anti-infection (Ceftazidime 1 g and 100 ml 0.9%
sodium chloride) injection via an intravenous drip three times a
day. Subsequently, the patient had a fluid diet without any signs
of discomfort, such as difficulty swallowing, swallowing
obstruction, chest pain or fever. After a total of 5 days of
standard care, the thoracic CT showed that there was a 2.3x5.6-mm
bubble shadow in the posterior mediastinum (Fig. 5). This was a normal postoperative
phenomenon that is usually absorbed in a short period of time. The
patient was discharged with no obvious discomfort. All of the
treatments followed the standardized management procedures
(Management of foreign bodies in the airway and oesophagus) for
removing esophageal foreign bodies under endoscopy (11,12).
Through four telephone follow-up surveys conducted at 1 week, 1
month, 3 months and 5 months after discharge, the condition of the
patient was recorded as stable.
Discussion
Ingestion of foreign bodies by mistake is a common
clinical issue worldwide. Children make up ~80% of patients, and
the annual incidence for adults reaches 13.0 per 100,000
individuals (13). The majority of
ingested foreign bodies will pass through the digestive system
spontaneously (14). However,
10-20% cases of ingested foreign bodies do require
endoscopy-assisted removal and 1% will require surgery for foreign
body extraction or treatment of complications (15). In the majority of cases,
endoscopy-assisted removal of foreign bodies is safe and has risk
of minor complications when performed by an experienced endoscopist
(14,16). However, there is a risk of fatality
if foreign bodies are not removed in a prompt and correct manner. A
previous study (17) reported the
case of a 3-year-old child who had a prolonged presence of disc
batteries in the esophagus, resulting in an aorto-esophageal
fistula and subsequently fatal hemorrhage.
The European Society of Gastrointestinal Endoscopy
clinical guidelines (14)
recommend emergency endoscopy for sharp-pointed objects in the
esophagus within 24 h. The previous study by Zhang et al
(18) demonstrated that the
incidence of complications, including ulcers, laceration,
perforation and perforation with mediastinitis or mediastinal
abscesses, were more frequent in the >24 h compared with that in
the ≤24 h group. Effective treatment within 24 h resulted in less
complications and shorter postoperative hospitalization stays
(18). In the present case, the
patient came to the hospital in a timely manner, 6 h after
ingesting the fish bone. Even with the addition of preoperative
preparation and operating time, the fish bone was successfully
removed within a total of 12 h. This most likely aided the recovery
of the patient.
The present case was a high-risk esophageal foreign
body due to its proximity to the thoracic aorta. It is important to
conduct a meticulous anamnesis, adequate imaging and urgent
gastroscopy for patients with esophageal fish bone impaction before
treatment (19). Due to several
factors, such as changes in the position of the patient and
endoscopic techniques, it was necessary to reposition the two ends
of the fish bone. Since one end was inserted into the bronchus, it
was not only a foreign body in the esophagus, but also seemed to be
a part of the airway. The present case revealed that the light
source of the fiberoptic bronchoscope could serve an auxiliary
role. During the operation, the combination of fibro-bronchoscopy
and gastroscopy was used to eliminate the possibility of
misjudgment and reduce the severity of organ injury, where the
foreign body was safely removed.
Endoscopic removal remains to be the gold standard
of treatment and surgical removal is the last resort (11,12).
Bae and Cho (20) previously
reported the case of a 57-year-old male patient complaining of a
sore throat, odynophagia pain and chest pain behind the sternum
after eating a fish. It was then revealed using a chest CT scan
that a sharp fish bone was located between the aortic arch and the
right subclavian artery. Considering the difficulties and dangers,
thoracotomy was adopted to remove the esophageal foreign body.
Despite its success, the majority of patients may not be as willing
to experience such an invasive surgical procedure due to the
advantages of endoscopy, which is minimally invasive, more
economical and convenient (21,22).
In the present case, the successful removal of the foreign object
using endoscopy was performed, avoiding further trauma.
The present case reports a rare occasion of foreign
body removal using upper gastrointestinal endoscopy and
fibro-bronchoscopy. Without the assistance of fibro-bronchoscopy,
it may have resulted in an incorrect direction of dissociation and
endangered the patient's life. This suggested that
fibro-bronchoscopy may exhibit a good auxiliary effect on the
removal of esophageal foreign bodies in special cases. It may
improve the success rate of one endoscopic procedure whilst
avoiding further surgical procedures for patients. In such cases,
they not only need to be diagnosed and treated in a timely manner,
but it is also necessary to apply multiple strategies according to
the type and location of the foreign body.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YM and XX contributed to the conception of the
study. YM and YT wrote the manuscript. YM, YT and XX analyzed and
interpreted the imaging findings. YC, TP and HR obtained and
analyzed the endoscopic images. TP and XX edited and reviewed the
prepublication version of the manuscript. YM, YT and XX confirm the
authenticity of all the raw data. All authors read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
The Ethics Committee of Chengdu First People's
Hospital exempted this case study from the ethical review approval
due to the management mode of emergency procedures.
Patient consent for publication
Written informed consent for the publication of the
patient's clinical information and images was obtained from the
patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Crosby JC: Emergency department management
of gastrointestinal foreign body ingestion. Emerg Med Pract.
25:1–28. 2023.PubMed/NCBI
|
|
2
|
Rosen RD and Winters R: Physiology, lower
esophageal sphincter. Treasure Island (FL): StatPearls Publishing,
2023.
|
|
3
|
Athanassiadi K, Gerazounis M, Metaxas E
and Kalantzi N: Management of esophageal foreign bodies: A
retrospective review of 400 cases. Eur J Cardiothorac Surg.
21:653–656. 2002.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Boo SJ and Kim HU: Esophageal foreign
body: Treatment and complications. Korean J Gastroenterol. 72:1–5.
2018.PubMed/NCBI View Article : Google Scholar : (In Korean).
|
|
5
|
Kozlov LD and P'Ianov RP: Perforation of
the esophageal wall and aorta by a foreign body. Vestn
Otorinolaringol. 90–91. 1978.PubMed/NCBI(In Russian).
|
|
6
|
Zhao S, Tinzin L, Deng W, Tong F, Shi Q
and Zhou Y: Sudden unexpected death due to left subclavian
artery-esophageal fistula caused by fish bone. J Forensic Sci.
64:1926–1928. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yang S, Chen G, Liang M, Yang M and Wu Z:
Hemorrhagic shock, aorto-esophageal fistula, and thoracic aorta
pseudoaneurysm caused by fish bone. Circ Cardiovasc Imaging.
14(e11476)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wang HC, Hu SW, Lin KJ and Chen AC: A
novel approach to button battery removal in a two-and-half year-old
patient's esophagus after ingestion: A case report. BMC Pediatr.
22(96)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yonemoto S, Uesato M, Aoyama H, Maruyama
T, Urahama R, Suito H, Yamaguchi Y, Kato M and Matsubara H: A
double-scope technique enabled a patient with an esophageal plastic
fork foreign body to avoid surgery: A case report and review of the
literature. Clin J Gastroenterol. 15:66–70. 2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lee JS, Chun HJ, Lee JM, Hwang YJ, Kim SH,
Kim ES, Jeen YT and Lee HJ: Salvage technique for endoscopic
removal of a sharp fish bone impacted in the esophagus using a
transparent cap and detachable snares. Korean J Gastroenterol.
61:215–218. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Togo S, Ouattara MA, Li X, Yang SW and
Koumaré S: Management for esophageal foreign bodies: About 36
cases. Pan Afr Med J. 27(207)2017.PubMed/NCBI View Article : Google Scholar : (In French).
|
|
12
|
Rodríguez H, Passali GC, Gregori D,
Chinski A, Tiscornia C, Botto H, Nieto M, Zanetta A, Passali D and
Cuestas G: Management of foreign bodies in the airway and
oesophagus. Int J Pediatr Otorhinolaryngol. 76 (Suppl 1):S84–S91.
2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Schaefer TJ and Trocinski D: Esophageal
foreign body. In: StatPearls. Treasure Island (FL): StatPearls
Publishing; January 30, 2023.
|
|
14
|
Yadollahi S, Buchannan R, Tehami N, Stacey
B, Rahman I, Boger P and Wright M: Endoscopic management of
intentional foreign body ingestion: Experience from a UK centre.
Frontline Gastroenterol. 13:98–103. 2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Birk M, Bauerfeind P, Deprez PH, Häfner M,
Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L and Meining A:
Removal of foreign bodies in the upper gastrointestinal tract in
adults: European society of gastrointestinal endoscopy (ESGE)
clinical guideline. Endoscopy. 48:489–496. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Marashi Nia SF, Aghaie Meybodi M, Sutton
R, Bansal A, Olyaee M and Hejazi R: Outcome, complication and
follow-up of patients with esophageal foreign body impaction: An
academic institute's 15 years of experience. Dis Esophagus.
33(doz103)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kozhevnikov EM, Polovinkin AR, Vorobyev VG
and Edelev NS: The case of the death of a child due to perforation
of the walls of the esophagus and aorta caused by a foreign body-an
electric battery. Sud Med Ekspert. 65:51–53. 2022.PubMed/NCBI View Article : Google Scholar : (In Russian).
|
|
18
|
Zhang X, Jiang Y, Fu T, Zhang X, Li N and
Tu C: Esophageal foreign bodies in adults with different durations
of time from ingestion to effective treatment. J Int Med Res.
45:1386–1393. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Conthe A, Payeras Otero I, Pérez Gavín LA,
Baines García A, Usón Peiron C, Villaseca Gómez C, Herrera Fajes JL
and Nogales Ó: Esophageal fish bone impaction: The importance of
early diagnosis and treatment to avoid severe complications. Rev
Esp Enferm Dig. 114:660–662. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bae CH and Cho JW: Esophageal foreign body
removal by thoracotomy in a patient with aberrant right subclavian
artery. Kardiochir Torakochirurgia Pol. 17:212–213. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhai YQ, Chai NL, Zhang WG, Li HK, Lu ZS,
Feng XX, Liu SZ and Linghu EQ: Endoscopic versus surgical resection
in the management of gastric schwannomas. Surg Endosc.
35:6132–6138. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Liu Q, Ding L, Qiu X and Meng F: Updated
evaluation of endoscopic submucosal dissection versus surgery for
early gastric cancer: A systematic review and meta-analysis. Int J
Surg. 73:28–41. 2020.PubMed/NCBI View Article : Google Scholar
|