Introduction
The trachea and bronchus in children are
characterized by narrow lumen and weak tracheal cartilage.
Therefore, influenced by these anatomical and physiological
characteristics, children are susceptible to respiratory infections
(1). General anesthesia is an
essential method used in surgery (2). Children have relatively immature
immune systems and may therefore be more vulnerable to infection
during surgery. The improvement in the safety of anesthesia holds
the potential for clinical significance, which is not only crucial
to the life and health of patients, but also has a positive impact
on all aspects of medical practice, helping to improve the quality
of care, reduce medical risks, and enhance the satisfaction of
patients and medical staff.
As a supraglottic ventilation device, the laryngeal
mask airway offers several advantages, including no requirement for
a laryngoscope to expose the glottis, lack of damage to the airway
and minimal cardiovascular reaction (3). A systematic review demonstrated that
the laryngeal mask airway significantly reduced the incidence of
laryngeal spasms and postoperative hoarseness in adult patients
undergoing general anesthesia (4).
The insertion procedure of the laryngeal mask airway for anesthesia
is simple and easy to secure, minimizing the risk of dislodgment.
Complications, such as laryngeal edema, vocal cord injury and
recurrent laryngeal nerve paralysis are less likely to occur. In
addition, it allows for spontaneous breathing, avoiding adverse
reactions due to the use of muscle relaxants and their antagonists.
The device causes minimal stimulation and secretion, does not
affect the tracheal ciliary activity, aids in sputum clearance and
maintains the self-cleaning effect of the airway. Moreover, it
reduces the occurrence of postoperative cough, atelectasis,
pneumonia and other pulmonary complications. The airway resistance
and patient breathing capacity are minimal and the respiratory
muscle is more resistant to fatigue. The depth of anesthesia
required is shallower than that for endotracheal intubation and the
dosage of anesthesia is reduced (5).
Endotracheal intubation is a more traditional
procedure where a tracheal tube is inserted from the mouth into the
trachea (6). However, excessive or
rough intubation can result in tooth loss, damage to the mucous
membranes of the nose or throat and bleeding. Using a catheter with
a diameter that is too small can increase respiratory resistance,
leading to poor ventilation function, while using a catheter that
is too large and rigid can cause laryngeal edema. If the catheter
inserted is too shallow, it may be removed unexpectedly and
dislodge due to changes in the patient's position. The deep
insertion of the catheter into the bronchus can cause hypoxia and
atelectasis on one side, affecting lung ventilation. In addition,
intubation can stimulate the vagus nerve, which in severe cases may
lead to respiratory and cardiac arrest (7,8).
Endotracheal intubation can stimulate the glottis and airway,
potentially causing damage to the oral mucosa in children, glottic
edema and complications, such as laryngeal spasm and sore throat
(9). The compression of the airway
mucosa by an airbag following the long-term placement of the
endotracheal catheter and the re-stimulation of the glottis and
airway mucosa during extubation can lead to mucosal injury
(10).
The present study performed a meta-analysis to
systematically evaluate the safety and effectiveness of the
laryngeal mask airway and endotracheal intubation in airway
management under general anesthesia in children and aimed to
provide a reference for clinical use.
Materials and methods
Search strategy
The present literature review and meta-analysis was
conducted following the Preferred Reporting Items for Systematic
Reviews (11) and Meta-Analyses
guidelines (12). The keywords
‘laryngeal mask airway’, ‘endotracheal tube’, ‘tracheal tube’,
‘children’, ‘pediatric’, ‘anesthesia’, ‘randomized controlled
trials’ (RCTs) and ‘randomized’ were used for searching the
relevant literature in MEDLINE (https://pubmed.ncbi.nlm.nih.gov/), Embase (https://www.embase.com/), Cochrane Central Register of
Controlled Trials via the Wiley Interface (https://www.cochranelibrary.com/central), Web of
Science Core Collection (https://www.webofscience.com/) and PubMed (https://pubmed.ncbi.nlm.nih.gov/). The search
results were restricted to the records included in the subset ‘as
supplied by publisher’ to identify references that were not yet
indexed in MEDLINE and Google Scholar (https://scholar.google.com/) (13). The search was performed using a
combination of subject terms such as ‘Medical Subject Headings’ and
filters such as ‘RCT’. The references of the included articles were
inspected to identify relevant studies. No language was imposed,
while a time restriction of 1990-2021 was imposed on the search.
The exact date of the database search was September 1, 2021
(Table SI).
Inclusion and exclusion criteria
The following inclusion criteria were used: i) The
study type was RCT and the language of the literature was limited
to English; ii) the study participants were pediatric patients
undergoing general anesthesia; and iii) the experimental group was
treated with a laryngeal mask airway, while the control group was
treated with endotracheal intubation.
Recent upper respiratory tract infections,
significant heart and lung diseases, airway abnormalities and
throat diseases were criteria for exclusion from the present study.
Moreover, studies were excluded when surgery was performed on the
heart, lungs and mediastinum, the relevant data were absent from
the literature, and the authors could not be successfully
contacted.
Study quality
During the literature screening, the titles and
abstracts were initially reviewed, and subsequently, the full text
was read to determine whether the study should be included or not
according to the aforementioned inclusion and exclusion criteria. A
total of two authors, namely WD and WZ, assessed the quality of the
studies based on the domains defined by the Cochrane Collaboration
tool for assessing bias risk (14). WD selected the studies for
full-text review. In cases of disagreement between WD and WZ on a
particular study, the final assessment and decision were provided
by the author JH, who is a senior expert in anesthesiology.
Data extraction
Subsequently to the literature screening, the
following data were extracted: i) Basic characteristics of included
studies, including authors of literature and year of publication;
ii) basic characteristics of the subjects; and iii) specific
details of interventions and clinical outcome measures.
Main comparison and outcomes
The following outcomes were extrapolated from the
selected studies and used in the present meta-analysis: Heart rate
variation, bronchospasm, throat pain, mucosal injury, hypoxemia,
postoperative cough, nausea and vomiting, reflux aspiration and
one-time success rate of implantation.
Bias risk assessment and evidence
quality assessment
The quality of the included studies was assessed
according to the risk of bias assessment criteria established in
the Cochrane Manual (15,16). The evaluation criteria mainly
included the following: Selection bias, performance bias,
measurement bias, follow-up bias, reporting bias and other
biases.
The Grading of Recommendations Assessment,
Development and Evaluation (GRADE) scoring system (17) was used to evaluate the quality of
significant outcome indicators into the four following levels:
High, medium, low and very low.
Statistical analysis
RevMan v5.2 software (https://tech.cochrane.org/revman/download) was used
for statistical analysis. Subgroup analysis was performed on
included data and the c2 test was used to assess
heterogeneity between studies. The significance level was set to
P=0.10. Moreover, I2 statistics were used to analyze the
study heterogeneity quantitatively and the significance level was
set to 50%. For P>0.1 and I2<50%, multiple similar
studies could be considered to be homogenous, and a fixed-effects
model could be used for the meta-analysis. For P≤0.1 and
I2≥50%, significant heterogeneity among studies was
assumed and the random-effects model was selected for the
meta-analysis. The measurement data were expressed as mean
difference and 95% CI, whilst enumeration data were expressed as
relative risk and 95% CI. The µ-test was used to test the null
hypothesis, represented by the Z- and P-values. The significance
level was set to α=0.05. GRADEpro software (5.2; GRADE Working
Group) was used for statistical analysis of the GRADE scores (high,
middle and low). P<0.05 was considered to indicate a
statistically significant difference.
Funnel diagram
Funnel diagrams are used to visualize data
processing, filtering processes or stage transition diagrams. They
often appear in a wide and narrow shape, like a funnel, which may
intuitively illustrate the reduction or transformation of data at
different stages, thereby helping to make decisions or identify
potential problems. Funnel charts are usually created using charts
to annotate data volume or conversion rates at different stages. A
funnel chart usually consists of two main parts: The top and
bottom. The top shows big data, while the bottom shows small data.
A conversion funnel chart may usually be described as a set of data
from four sources: The data displayed at the top is given as a
single value, which typically represents the foundation. Next is a
series of independent target groups, each with an independent
filter, and data values must meet their conditions to enter the
target group. These filters may be stacked, mutually exclusive, or
a process that changes over time.
Results
Research characteristics
A total of 1,021 relevant studies were retrieved,
and following elimination of duplicate studies, 147 were included
in the present analysis. Initially, 67 publications were screened
based on the title and abstract; according to the exclusion
criteria, 80 articles were selected for full-text review. After
reading the complete text, 60 articles were further excluded, of
which 20 were ongoing studies, 14 were conference abstracts, 18
were interventional studies and 8 were reviews. A total of 16 RCTs
were included in the present meta-analysis (Fig. S1 and Table I).
 | Table IBasic characteristics of the included
studies. |
Table I
Basic characteristics of the included
studies.
| First author/s,
year | Sample number
(laryngeal mask airway/endotracheal tube) | Complication
index | (Refs.) |
|---|
| Duman et al,
2001 | 18/20 | 1 | (18) |
| Fan et al,
2017 | 35/41 | 1,3,6,7,8 | (22) |
| Agrawal et
al, 2012 | 30/29 | 1 | (21) |
| Fröhlich et
al, 1997 | 13/12 | 6 | (33) |
| Al-Mazrou et
al, 2010 | 30/30 | 3,4,6 | (25) |
| Lalwani et
al, 2010 | 30/30 | 1,2,3,4,6,8,9 | (20) |
| Patel et al,
2010 | 30/30 | 3,5,6,7,8,9 | (27) |
| Ozdamar et
al, 2010 | 20/20 | 3,6 | (26) |
| Ozden et al,
2016 | 40/80 | 4,5,6,7,8 | (29) |
| Peng et al,
2011 | 60/71 | 5 | (31) |
| Gul et al,
2012 | 38/39 | 2,3,4,6,7,9 | (23) |
| Doksrød et
al, 2010 | 69/62 | 5,6,7 | (30) |
| Sinha et al,
2007 | 30/30 | 1,4,6,8,9 | (19) |
| Splinter et
al, 1994 | 55/57 | 3 | (24) |
| Tian et al,
2017 | 50/50 | 1,3,4,6, 9 | (28) |
| Zhao et al,
2014 | 120/51 | 5 | (32) |
Methodological quality assessment
According to the qualitative analysis of the funnel
plots, the distribution of the included literature was symmetrical
and the publication bias was negligible. Moreover, the majority of
the studies were located at the tip of the funnel plot, indicating
that the confidence interval of the included studies was narrow and
the accuracy was high (Fig. S2).
In addition, in all included studies, a minor risk of bias was
present in the judgement of each risk of bias item, which was
expressed as a percentage (Fig.
S3).
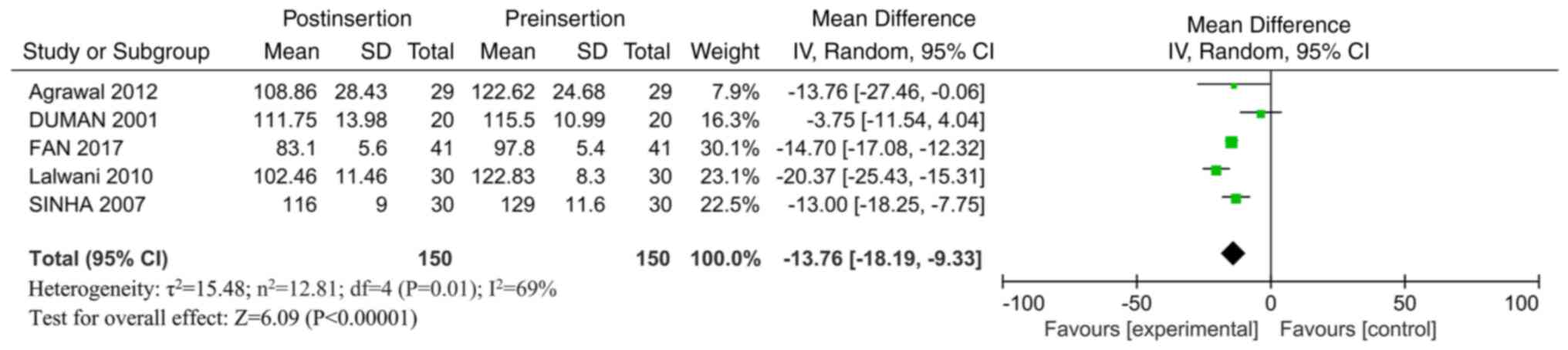
Outcome analysis of heart rate
variability
A total of 5 RCTs (18-22)
reported heart rate variability. The heart rate variability in the
laryngeal mask airway group was significantly lower than that in
the intubation group [mean difference=-13.76; 95% CI,
-18.19-(-9.33); I2=69%; P<0.00001; Fig. 1]. This result indicated that the
laryngeal mask airway could significantly reduce heart rate
variability, thereby promoting a stable heart rate, compared with
endotracheal intubation.
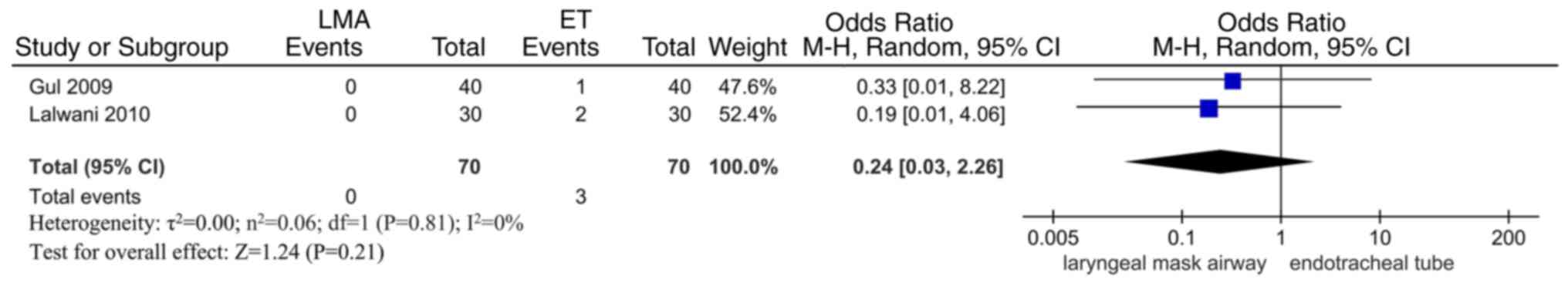
Bronchospasm, sore throat and mucosal
lesions
A total of two RCTs (20,23)
reported bronchospasm. No statistically significant difference was
noted in the bronchospasm incidence between the two groups [odds
ratio (OR)=0.24; 95% CI, 0.03-2.26; I2=0%; P=0.21;
Fig. 2), indicating that
endotracheal intubation may not cause additional damage compared
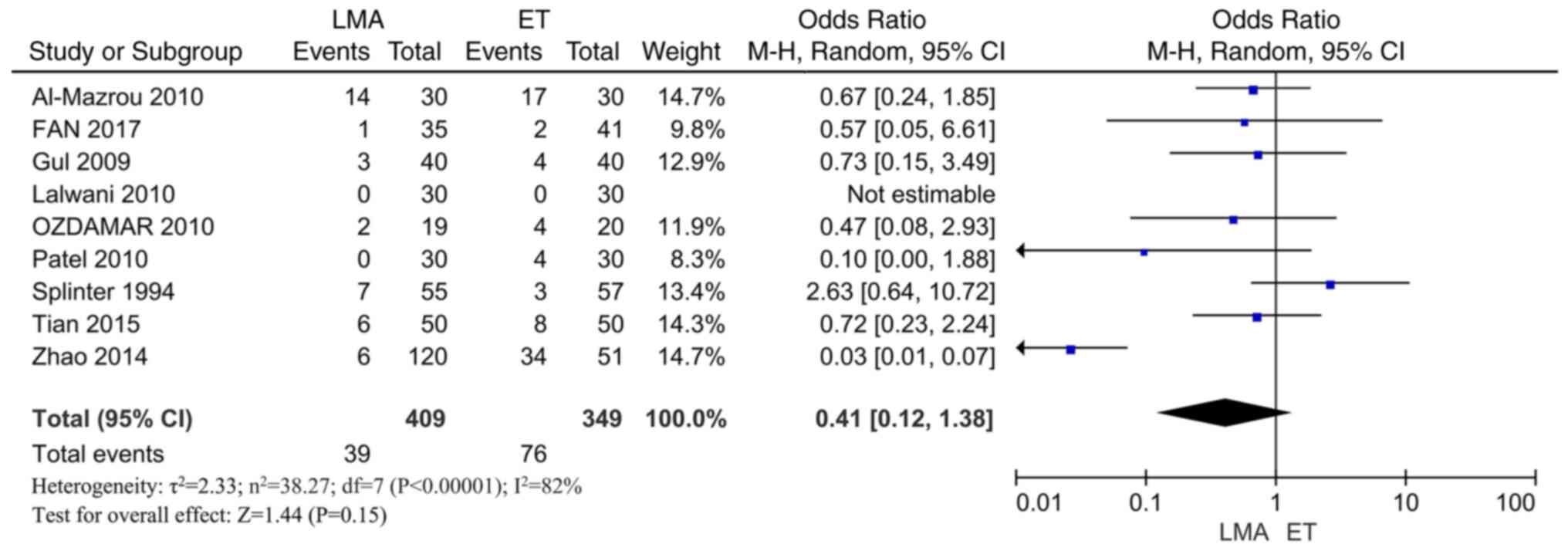
with the laryngeal mask airway. A total of eight RCTs (20,22-28)
reported sore throats. The results indicated no significant
difference in throat pain between the two groups (OR=0.41; 95% CI,
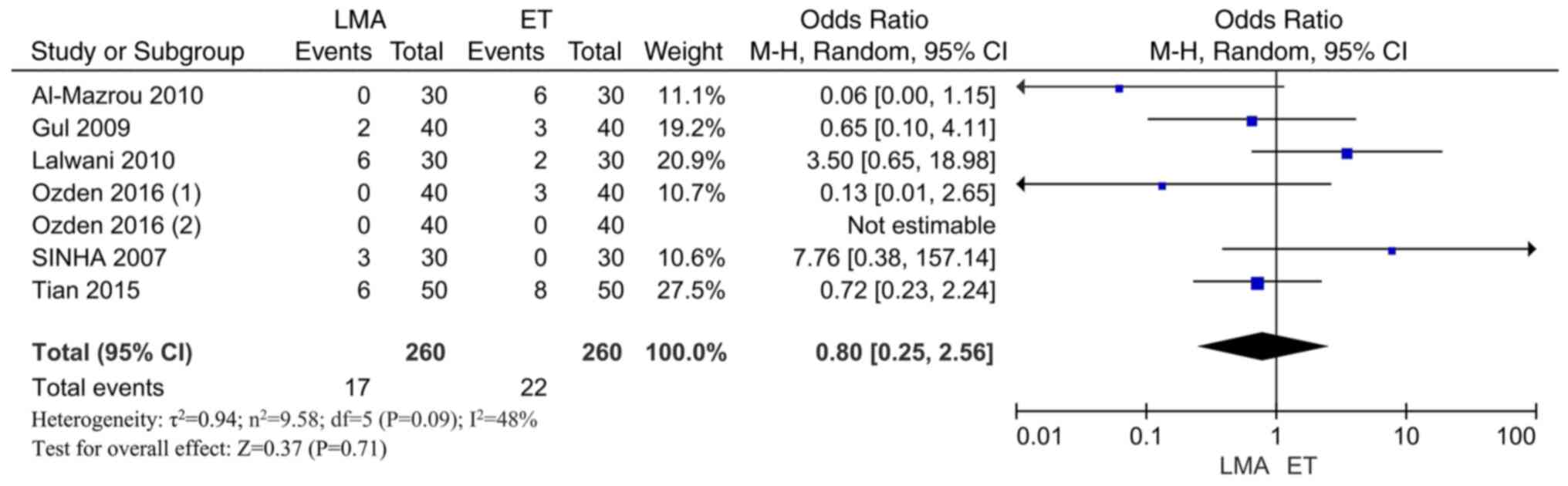
0.12-1.38; I2=82%; P=0.15; Fig. 3). A total of six RCTs (19,20,23,25,28,29)
reported mucosal lesions. The results indicated no significant
difference in mucosal injury between the two groups (OR=0.80; 95%
CI, 0.25-2.56; I2=48%; P=0.71; Fig. 4). Therefore, concerning sore throat
and mucosal lesions, the results indicated that the endotracheal
intubation may not cause additional damage compared with the
laryngeal mask airway.
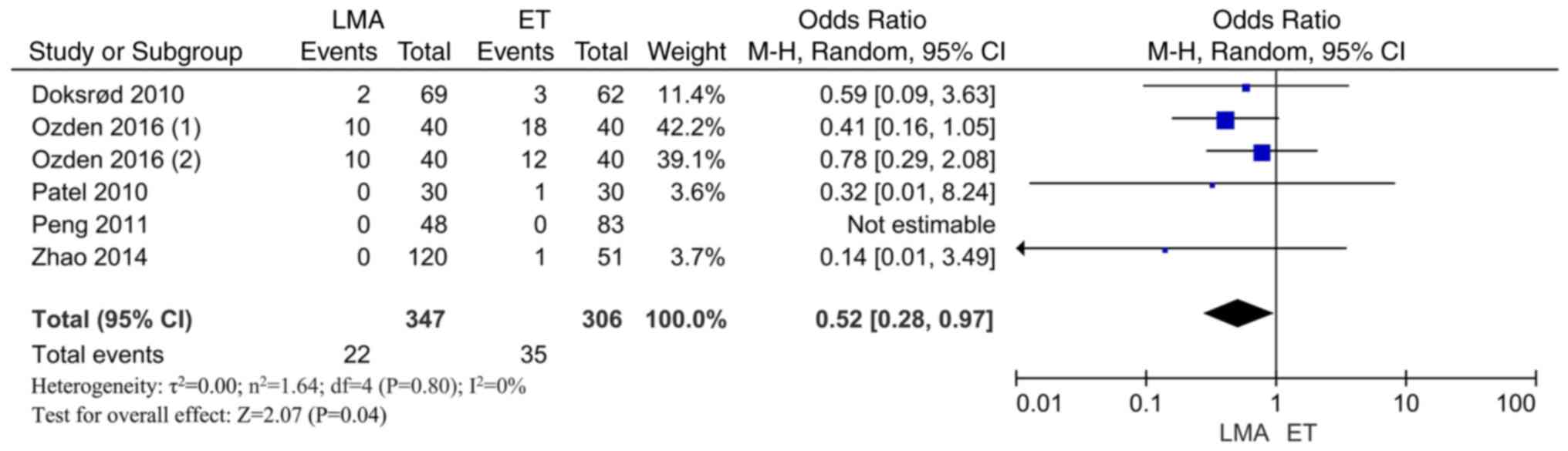
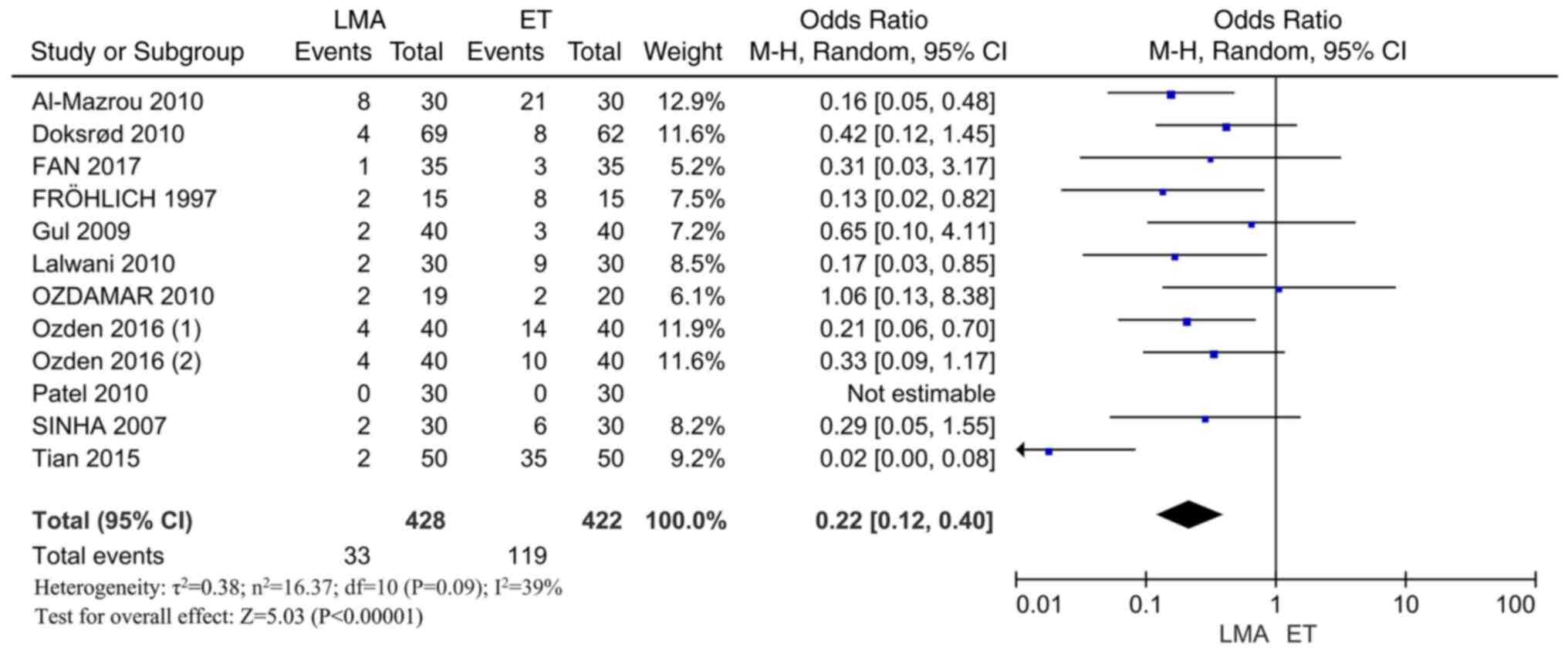
Hypoxemia and postoperative cough
A total of five RCTs (27,29-32)
reported hypoxemia. The results indicated that the incidence of
hypoxemia in the laryngeal mask airway group was significantly
lower than that noted in the endotracheal intubation group
(OR=0.52; 95% CI, 0.28-0.97; I2=0%; P=0.04; Fig. 5). This demonstrated that
endotracheal intubation may accelerate hypoxemia compared with the
laryngeal mask airway. A total of 11 RCTs (19,20,22,23,25-30,33)
reported postoperative cough. The results indicated that the
incidence of postoperative cough in the laryngeal mask airway group
was significantly lower than that noted in the endotracheal
intubation group (OR=0.22; 95% CI, 0.12-0.40; I2=39%;
P<0.00001; Fig. 6). The
laryngeal mask airway could significantly reduce postoperative
cough compared with endotracheal intubation.
Nausea and vomiting and reflux
aspiration
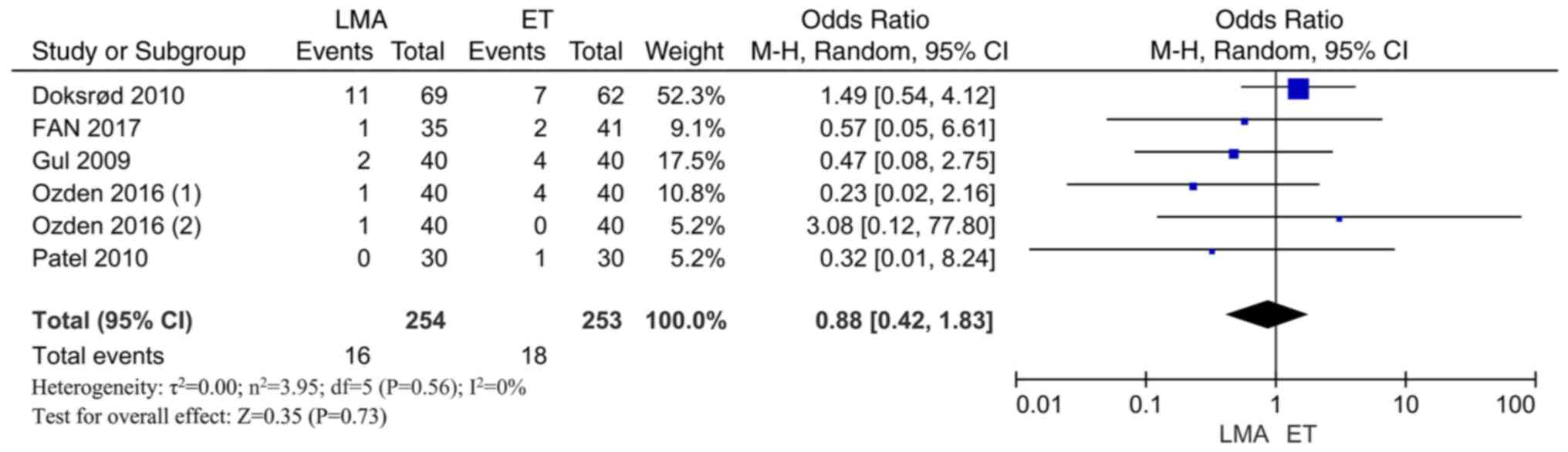
A total of 5 RCTs (22,23,27,29,30)
reported nausea and vomiting. The results indicated a lack of
significant differences in the incidence of nausea and vomiting
between the two groups (OR=0.88; 95% CI, 0.42-1.83;
I2=0%; P=0.73; Fig. 7).
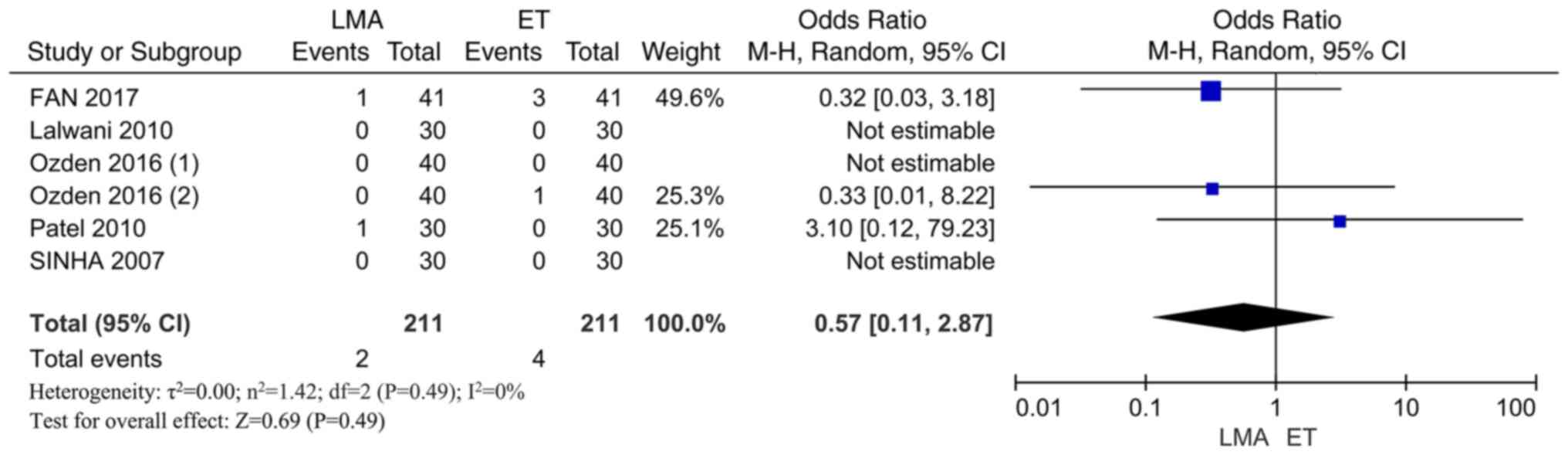
A total of 5 RCTs (19,20,22,27,29)
reported reflux aspiration. The results indicated a lack of
statistical significance between the two groups in reflux
aspiration (OR=0.57; 95% CI, 0.11-2.87; I2=0%; P=0.49;
Fig. 8). Collectively, the results
demonstrated a lack of significant differences in the incidence of
nausea and vomiting and reflux aspiration between the laryngeal
mask airway and the endotracheal intubation groups.
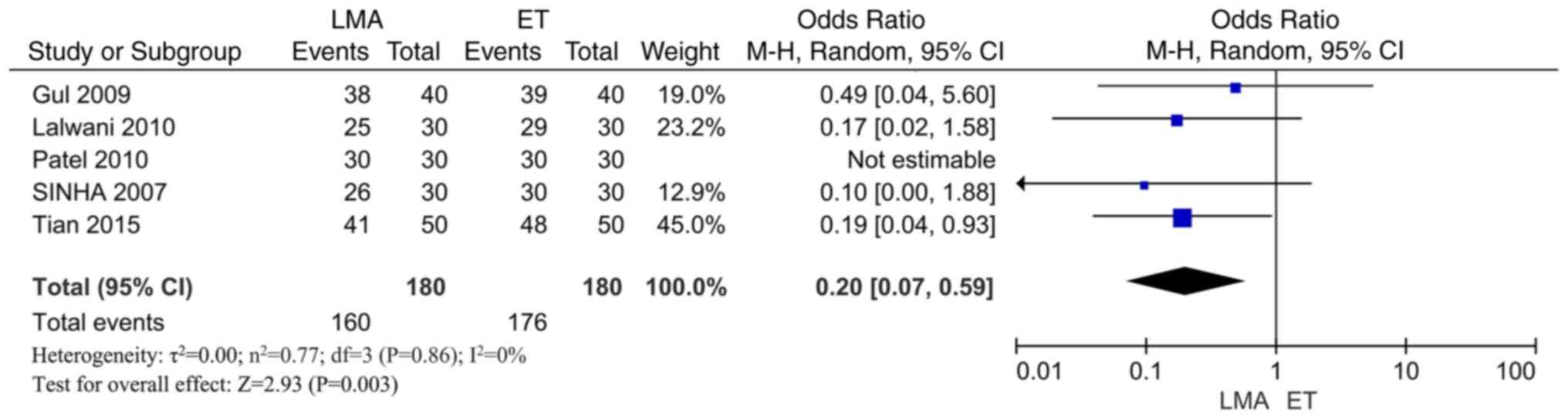
Success rate of single
implantation
A total of 5 RCTs (19,20,23,27,28)
reported the success rate of a single implantation method. The
success rate of primary implantation in the laryngeal mask airway
group was significantly higher than that of the endotracheal
intubation group (OR=0.20; 95% CI: 0.07-0.59; I2=0%;
P=0.003; Fig. 9). These results
indicated that the one-time implantation rate of the laryngeal mask
airway was higher than that of the endotracheal intubation.
Discussion
The present study indicated that laryngeal mask
airway placement during general anesthesia could reduce the
complications of general anesthesia, such as hypoxemia and
postoperative cough; in addition, one-time implantation of the
laryngeal mask airway exhibited a high success rate.
Compared with endotracheal intubation, a laryngeal
mask airway during general anesthesia may reduce hypoxemia
following general anesthesia (34). Hypoxia can be induced by
ventilation and/or ventilation dysfunction due to various causes,
such as central nervous system disorders and bronchial and
pulmonary diseases (29,30). The use of a laryngeal mask airway
can increase the success rate, reduce the difficulty and
complications of the operation, thereby ensuring the effectiveness
of the operation (35). External
chest compressions are not affected during the operation, which can
obtain valuable rescue time for patients with cardiac and
respiratory arrest without exposing the larynx and glottis, thus
reducing the difficulty of the operation (36). The laryngeal mask airway has a
prominent role in opening and clearing the airway, absorbing the
phlegm quickly and preventing air leakage (37).
Compared with endotracheal intubation, laryngeal
mask airway placement during general anesthesia may reduce
post-general anesthesia cough. Laryngeal mask airway placement does
not pass through the glottis and trachea, and the irritation to the
respiratory tract is significantly lower than that of endotracheal
intubation (38). Laryngeal mask
airway ventilation provides stable systemic circulation and
adequate oxygenation, which is improved compared with that of the
endotracheal intubation in reducing the stress response of
intubation and avoiding severe circulation fluctuation caused by
deep anesthesia during endotracheal intubation (39). Laryngeal mask airway ventilation is
easy to use compared with endotracheal intubation, requires no
stimulation of the glottis and trachea and does not affect the
ciliary movement of the tracheal mucosa. Its prominent advantage is
the elimination of mechanical stimulation to the tracheal larynx
(40). In the absence of
stimulation, the occurrence of complications, such as vomiting and
restlessness, is reduced (41).
Compared with endotracheal intubation, single
laryngeal mask airway implantation under general anesthesia
exhibits a higher success rate. Intraoperative hemodynamics are
stable, the fluctuation range of the heart rate and blood pressure
is low, and the physical harm caused to the patient is minor
(39). Endotracheal intubation can
easily cause severe fluctuation of the heart rate and blood
pressure; in addition, the patient's hemodynamics are unstable,
affecting the surgical effect (36). If the laryngeal mask airway can be
used reasonably during the operation, it can decrease the incidence
of complications during the peri-anesthesia period, shorten the
time of resuscitation, and therefore reduce postoperative
complications (42).
Despite the rigorous analysis of the present study,
certain limitations are evident. Firstly, certain included studies
did not describe the random sequence generation, allocation
concealment and blinding method in detail. Therefore, potential for
selection, implementation and measurement bias is present.
Secondly, in the literature studies included in the present report,
the duration of surgery in children was generally low (30-90 min),
which may be conducive to the use of the laryngeal mask airway and
cause bias to the results.
In conclusion, the use of laryngeal mask airway
during general anesthesia can reduce the occurrence of
complications, such as heart rate variability, the incidence of
hypoxemia and postoperative cough, compared with endotracheal
intubation, with a high success rate of one-time implantation.
Supplementary Material
Flow diagram of the research studies
included in the meta-analysis.
Quality assessment. (A) Heart rate
variation. (B) Bronchospasm. (C) Throat pain. (D) Mucosal injury.
(E) Hypoxemia. (F) Postoperative cough. (G) Nausea and vomiting.
(H) Reflux aspiration. (I) One-time implantation success rate.
According to the qualitative analysis of the funnel plot, the
distribution of the included literature was symmetrical, and the
publication bias was small. MD, mean difference; SE, standard
error; OR, odds ratio; SE (log [OR]), SE of the natural logarithm
of the OR.
Risk of bias graph. Percentages across
all included studies.
Literature search tracking
information.
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by the Tianjin Key Medical
Discipline Construction Project (grant no. TJYXZDXK-042A).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
WD contributed to the study conception and design.
WZ acquired the data through the database search. JE contributed to
the statistical analysis of the data. JH and JL analyzed data and
drafted the manuscript. WD and JH confirm the authenticity of all
the raw data. WD and JL revised the main contents of the
manuscript. All authors have read and approved the final version of
the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Stein ML, Park RS and Kovatsis PG:
Emerging trends, techniques, and equipment for airway management in
pediatric patients. Paediatr Anaesth. 30:269–279. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jindal S, Mittal A, Anand LK, Singh M and
Kapoor D: Comparative evaluation of Air-Q blocker and Proseal
laryngeal mask airway in patients undergoing elective surgery under
general anaesthesia: A randomised controlled trial. Indian J
Anaesth. 65 (Suppl 1):S20–S26. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Martínez-de Los Santos CA and Cruz-Cruz
EF: Laryngeal mask in pediatrics. Rev Esp Anestesiol Reanim (Engl
Ed). 69:315–316. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Van Zundert AAJ, Gatt SP, Van Zundert
TCRV, Kumar CM and Pandit JJ: Features of new vision-incorporated
third-generation video laryngeal mask airways. J Clin Monit Comput.
36:921–928. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nishihara F, Ohkawa M, Hiraoka H, Yuki N
and Saito S: Benefits of the laryngeal mask for airway management
during electroconvulsive therapy. J ECT. 19:211–216.
2003.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Okada Y, Nakayama Y, Hashimoto K, Koike K
and Watanabe N: Ramped versus sniffing position for tracheal
intubation: A systematic review and meta-analysis. Am J Emerg Med.
44:250–256. 2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Miller AG, Gentile MA and Coyle JP:
Respiratory therapist endotracheal intubation practices. Respir
Care. 65:954–960. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Butler K and Winters M: The
physiologically difficult intubation. Emerg Med Clin North Am.
40:615–627. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Drake-Brockman TF, Ramgolam A, Zhang G,
Hall GL and von Ungern-Sternberg BS: The effect of endotracheal
tubes versus laryngeal mask airways on perioperative respiratory
adverse events in infants: A randomised controlled trial. Lancet.
389:701–708. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Disma N, Virag K, Riva T, Kaufmann J,
Engelhardt T and Habre W: NECTARINE Group of the European Society
of Anaesthesiology Clinical Trial Network; AUSTRIA (Maria
Vittinghoff); BELGIUM (Francis Veyckemans); CROATIA (Sandra Kralik)
et al. Difficult tracheal intubation in neonates and
infants. NEonate and Children audiT of Anaesthesia pRactice IN
Europe (NECTARINE): A prospective European multicentre
observational study. Br J Anaesth. 126:1173–1181. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zhang X, Tan R, Lam WC, Yao L, Wang X,
Cheng CW, Liu F, Chan JC, Aixinjueluo Q, Lau CT, et al: PRISMA
(Preferred Reporting Items for Systematic Reviews and
Meta-Analyses) Extension for Chinese Herbal Medicines 2020
(PRISMA-CHM 2020). Am J Chin Med. 48:1279–1313. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hernandez AV, Marti KM and Roman YM:
Meta-Analysis. Chest. 158 (1S):S97–S102. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Bramer WM, Rethlefsen ML, Kleijnen J and
Franco OH: Optimal database combinations for literature searches in
systematic reviews: A prospective exploratory study. Syst Rev.
6(245)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Higgins JP, Altman DG, Gøtzsche PC, Jüni
P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L and Sterne JA:
, et al: The Cochrane Collaboration's tool for assessing
risk of bias in randomised trials. BMJ. 343(d5928)2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Martimbianco ALC, Sá KMM, Santos GM,
Santos EM, Pacheco RL and Riera R: Most Cochrane systematic reviews
and protocols did not adhere to the Cochrane's risk of bias 2.0
tool. Rev Assoc Med Bras (1992). 69:469–472. 2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Nass M and Noble JH Jr: Whither Cochrane.
Indian J Med Ethics. 4:1–5. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Riemann D, Baglioni C, Bassetti C,
Bjorvatn B, Dolenc Groselj L, Ellis JG, Espie CA, Garcia-Borreguero
D, Gjerstad M, Gonçalves M, et al: European guideline for the
diagnosis and treatment of insomnia. J Sleep Res. 26:675–700.
2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Duman A, Ogün CO and Okesli S: The effect
on intraocular pressure of tracheal intubation or laryngeal mask
insertion during sevoflurane anaesthesia in children without the
use of muscle relaxants. Paediatr Anaesth. 11:421–424.
2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Sinha A, Sharma B and Sood J: ProSeal as
an alternative to endotracheal intubation in pediatric laparoscopy.
Paediatr Anaesth. 17:327–332. 2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lalwani J, Dubey KP, Sahu BS and Shah PJ:
ProSeal laryngeal mask airway: An alternative to endotracheal
intubation in paediatric patients for short duration surgical
procedures. Indian J Anaesth. 54:541–545. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Agrawal G, Agarwal M and Taneja S: A
randomized comparative study of intraocular pressure and
hemodynamic changes on insertion of proseal laryngeal mask airway
and conventional tracheal intubation in pediatric patients. J
Anaesthesiol Clin Pharmacol. 28:326–329. 2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Fan CH, Peng B and Zhang FC: Influence of
laryngeal mask airway (LMA) insertion anesthesia on cognitive
function after microsurgery in pediatric neurosurgery. Eur Rev Med
Pharmacol Sci. 21 (4 Suppl):S37–S42. 2017.PubMed/NCBI
|
|
23
|
Gul R, Goksu S, Ugur BK, Sahin L, Koruk S,
Okumus S and Erbagci I: Comparison of proseal laryngeal mask and
endotracheal tube for airway safety in pediatric strabismus
surgery. Saudi Med J. 33:388–394. 2012.PubMed/NCBI
|
|
24
|
Splinter WM, Smallman B, Rhine EJ and
Komocar L: Postoperative sore throat in children and the laryngeal
mask airway. Can J Anaesth. 41:1081–1083. 1994.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Al-Mazrou KA, Abdullah KM, ElGammal MS,
Ansari RA, Turkistani A and Abdelmeguid ME: Laryngeal mask airway
vs. uncuffed endotracheal tube for nasal and paranasal sinus
surgery: Paediatric airway protection. Eur J Anaesthesiol.
27:16–19. 2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ozdamar D, Güvenç BH, Toker K, Solak M and
Ekingen G: Comparison of the effect of LMA and ETT on ventilation
and intragastric pressure in pediatric laparoscopic procedures.
Minerva Anestesiol. 76:592–599. 2010.PubMed/NCBI
|
|
27
|
Patel MG, Swadia V and Bansal G:
Prospective randomized comparative study of use of PLMA and ET tube
for airway management in children under general anaesthesia. Indian
J Anaesth. 54:109–115. 2010.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tian Y, Wu XY, Li L, Ma L and Li YF: A
clinical trial evaluating the laryngeal mask airway-Supreme in
obese children during general anesthesia. Arch Med Sci. 13:183–190.
2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ozden ES, Meco BC, Alanoglu Z and Alkıs N:
Comparison of ProSeal laryngeal mask airway (PLMA) with cuffed and
uncuffed endotracheal tubes in infants. Bosn J Basic Med Sci.
16:286–291. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Doksrød S, Løfgren B, Nordhammer A,
Svendsen MV, Gisselsson L and Raeder J: Reinforced laryngeal mask
airway compared with endotracheal tube for adenotonsillectomies.
Eur J Anaesthesiol. 27:941–946. 2010.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Peng A, Dodson KM, Thacker LR, Kierce J,
Shapiro J and Baldassari CM: Use of laryngeal mask airway in
pediatric adenotonsillectomy. Arch Otolaryngol Head Neck Surg.
137:42–46. 2011.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zhao N, Deng F and Yu C: Anesthesia for
pediatric day-case dental surgery: A study comparing the classic
laryngeal mask airway with nasal trachea intubation. J Craniofac
Surg. 25:e245–e248. 2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Fröhlich D, Schwall B, Funk W and Hobbhahn
J: Laryngeal mask airway and uncuffed tracheal tubes are equally
effective for low flow or closed system anaesthesia in children. Br
J Anaesth. 79:289–292. 1997.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Chiumello D and Brioni M: Severe
hypoxemia: Which strategy to choose. Crit Care.
20(132)2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kendall MC: Laryngeal mask airway as a
rescue device for failed endotracheal intubation. Eur J Emerg Med.
26(73)2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Boroda N, Malesinska M, Kars MS and Smith
LP: The use of laryngeal mask airway for adenoidectomy. Int J
Pediatr Otorhinolaryngol. 107:42–44. 2018.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Zaichkin J, McCarney LD and Rhein M: The
laryngeal mask: Empowering nurses to rescue newborns. Adv Neonatal
Care. 23:140–150. 2023.PubMed/NCBI View Article : Google Scholar
|
|
38
|
van Esch BF, Stegeman I and Smit AL:
Comparison of laryngeal mask airway vs tracheal intubation: A
systematic review on airway complications. J Clin Anesth.
36:142–150. 2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Qamarul Hoda M, Samad K and Ullah H:
ProSeal versus Classic laryngeal mask airway (LMA) for positive
pressure ventilation in adults undergoing elective surgery.
Cochrane Database Syst Rev. 7(CD009026)2017.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ozhan MO, Eskin MB, Atik B, Suzer MA and
Capalar CO: Laryngeal mask airway for general anesthesia in
interventional neuroradiology procedures. Saudi Med J. 40:463–468.
2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
de Carvalho ALR, Vital RB, de Lira CCS,
Magro IB, Sato PTS, Lima LHN, Braz LG and Módolo NSP: Laryngeal
mask airway versus other airway devices for anesthesia in children
with an upper respiratory tract infection: A systematic review and
meta-analysis of respiratory complications. Anesth Analg.
127:941–950. 2018.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Simon LV and Torp KD: Laryngeal Mask
Airway. StatPearls. Treasure Island, FL, 2022.
|