Introduction
A hernia is a common condition that can be treated
with surgery, with inguinal hernias being more common in men, with
a prevalence of 25% (1). The
Retzius space is an anatomical space between the bladder and pubic
symphysis, which is located extraperitoneally (2). Lipomas are composed of mature fat
cells and can develop in any part of the body where fatty tissue is
located, particularly the shoulders, back, neck, breast, abdomen
and proximal extremities (3).
Pathologically, lipomas are categorized into spindle cell lipoma,
fibrolipoma, myxolipoma, myenteric lipoma, angiolipoma,
osteolipoma, pleomorphic lipoma and chondrolipoma (4). In 2009, Okuda et al (5) reported a case of spindle cell lipoma
occurring in the Retzius space where a malignant tumor or
preoperative gastric cancer metastasis was originally suspected.
The tumor size was 3.0x3.0x3.5 cm. Laparotomy was performed under
direct vision, the tumor was resected and the postoperative
histopathological report showed that the tumor was composed of
spindle cells and abundant mature adipose tissue.
Immunohistochemical staining results were CD34 (+); S-100 protein
(-); desmin (-); CD31 (-); and α-smooth muscle actin (-) and the
diagnosis was spindle cell lipoma. The aforementioned case study
could serve as a foundation for the treatment of interstitial
lipoma in the Retzius space. In the past 15 years, a small number
cases of lipomas in the Retzius space have been reported,
particularly without the use of laparoscopic surgery for giant
lipomas in the Retzius space (5).
The present study reports the case of a giant lipoma in the Retzius
space, measuring 25x20 cm, that was completely resected under
laparoscopy. The relevant treatment regime is also summarized.
Case report
Medical history
In October 2022, a 61-year-old male presented at the
Department of Urology in Beijing Yanhua Hospital (Beijing, China)
with frequent urination. Routine urine tests demonstrated mild
hematuria and proteinuria. Based on the initial suspicion of a
urinary tumor, CT scan of the lower abdomen was performed. The CT
images showed an indirect inguinal hernia and lipoma. The patient
was referred to the Department of General Surgery for further
treatment. The patient reported no symptoms, such as abdominal
pain, nausea, vomiting, change in bowel habits or cough. Medical
history included left indirect inguinal hernia for 3 months and
benign prostatic hyperplasia. Physical examination showed a flat
abdomen, without a mass or bulge, varicose veins in the abdominal
wall, intestinal pattern or peristaltic waves. On palpation, the
abdomen was soft, without abdominal mass and with normal bowel
sounds. To clarify the presence or absence of ascites, the patient
was examined for shifting dullness, which was negative. Plain
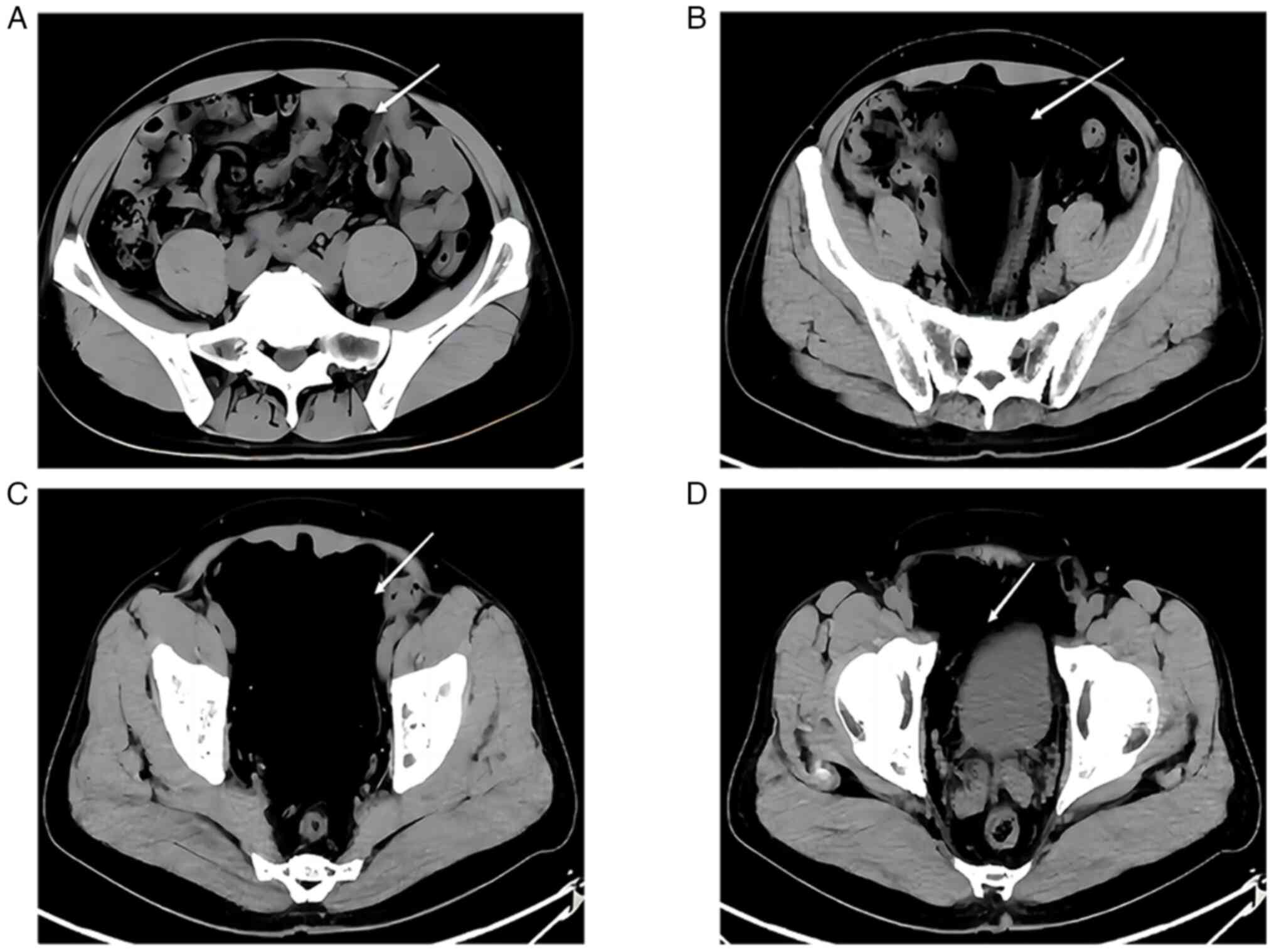
abdominal CT scan images demonstrated a cystic lesion measuring
~12x12x9 cm and a CT value of -110 HU. The boundary of the lesion
with the surrounding tissue was unclear (Fig. 1) However, tumor markers such as
CEA, AFP, CA125 and CA19-9, were within the expected ranges. CT
findings were consistent with a pelvic mass and indirect inguinal
hernia, therefore, an ultrasound was not performed.
The patient provided written informed consent for
publication of the present case report.
Surgical procedure and clinical
course
Based on a multidisciplinary consultation, in
October 2022, the patient was scheduled for laparoscopic pelvic
tumor resection with high ligation of inguinal hernia. Although the
tumor was located in the Retzius space, it was too large to be
operated on extraperitoneally. It was difficult to remove the tumor
intact, as it was too large. At the same time, preoperative CT
could not distinguish whether the tumor was intraperitoneal or
extraperitoneal, and an extraperitoneal surgical approach is
difficult for larger tumors; therefore, intraperitoneal surgery was
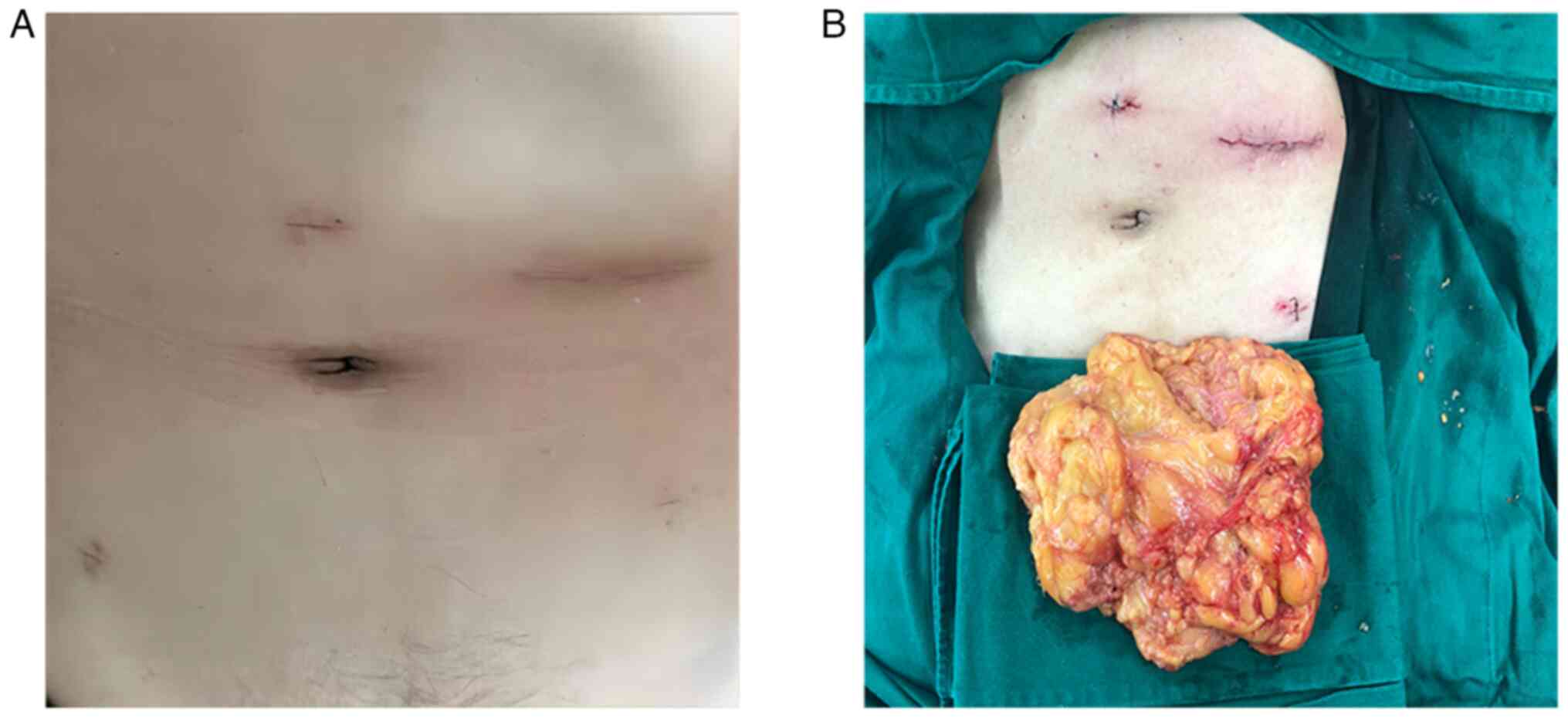
performed. A 10 mm trocar was placed in the umbilicus as
observation port ‘A’, a 12 mm trocar was placed in the left upper
abdomen as the main operation port ‘B’ and 5 mm trocars were placed
in the upper umbilicus, left lower abdomen and right lower abdomen
as auxiliary operation ports ‘C’, ‘D’ and ‘E’, respectively. The
pneumoperitoneum was initially maintained with a pneumoperitoneal
pressure of 15 mmHg to fully expose the field of vision. After
entering the abdominal cavity, the hernia sac lateral to the
inferior epigastric artery confirmed a diagnosis of inguinal
hernia. A large mass with a diameter ~25 cm was located in the
Retzius space and descended to the bladder. The mass was yellow,
fat-like and lobulated, with an insufflation pressure of 12 mmHg.
The tumor had no pedicle. Although the mass stemmed from the
bladder, it had entered into the Retzius space; therefore, it was
classified as a Retzius space tumor. The peritoneum was incised
above the tumor with an ultrasonic scalpel and separated along the
tumor border. The root of the tumor was located on the bladder wall
and was fully freed. Subsequently, the muscular layer of the
bladder wall and the incised peritoneum were sutured continuously
in layers with absorbable barbed sutures and the left inguinal
hernia was ligated at a high position. An incision ~5 cm was made
in the B trocar, the incision protective sleeve was placed and an
attempt was made to remove the tumor. Based on the patient medical
history and preoperative examination findings, the tumor was
initially thought to be benign. Therefore, a 5 cm incision
protective sleeve was used. However, removal of the tumor was not
smooth. Therefore, the incision was enlarged to ~8 cm and the tumor
was removed smoothly. The intraoperative blood loss volume was ~20
ml. The entire procedure was performed in ~70 min; the mass was
freed in ~50 min and was removed from the intraperitoneal region in
~20 min. The tumor measured ~25x20 cm and was lobulated (Fig. 2). The postoperative
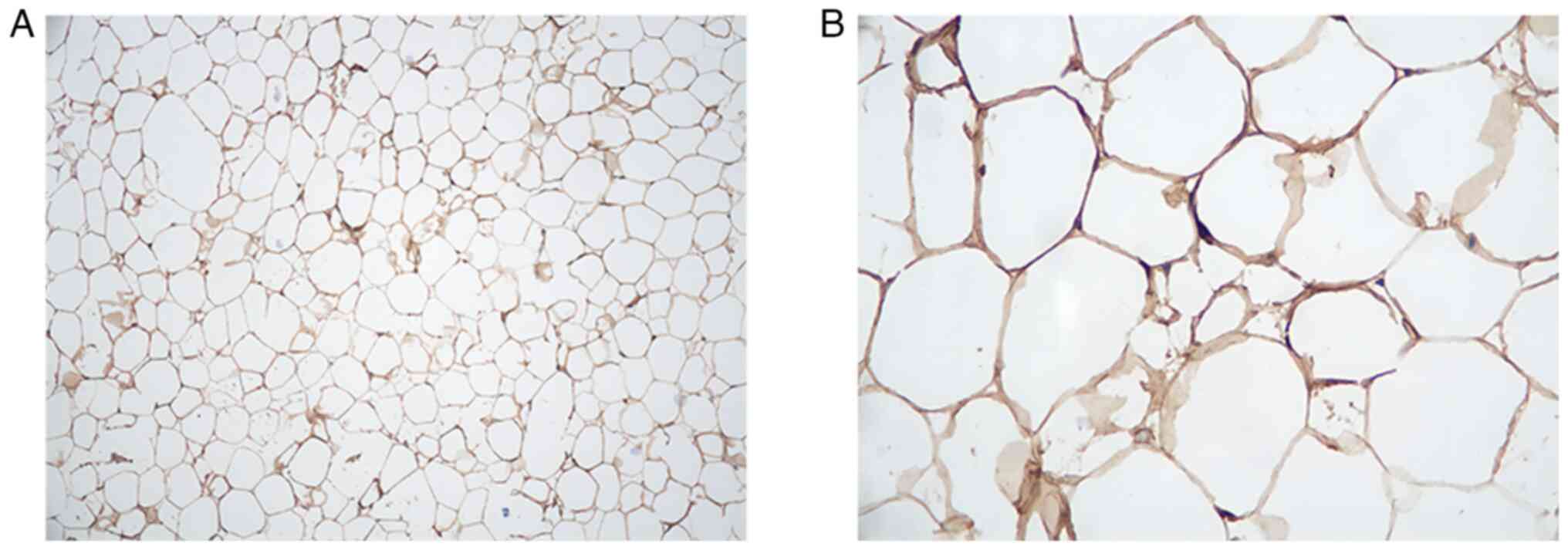
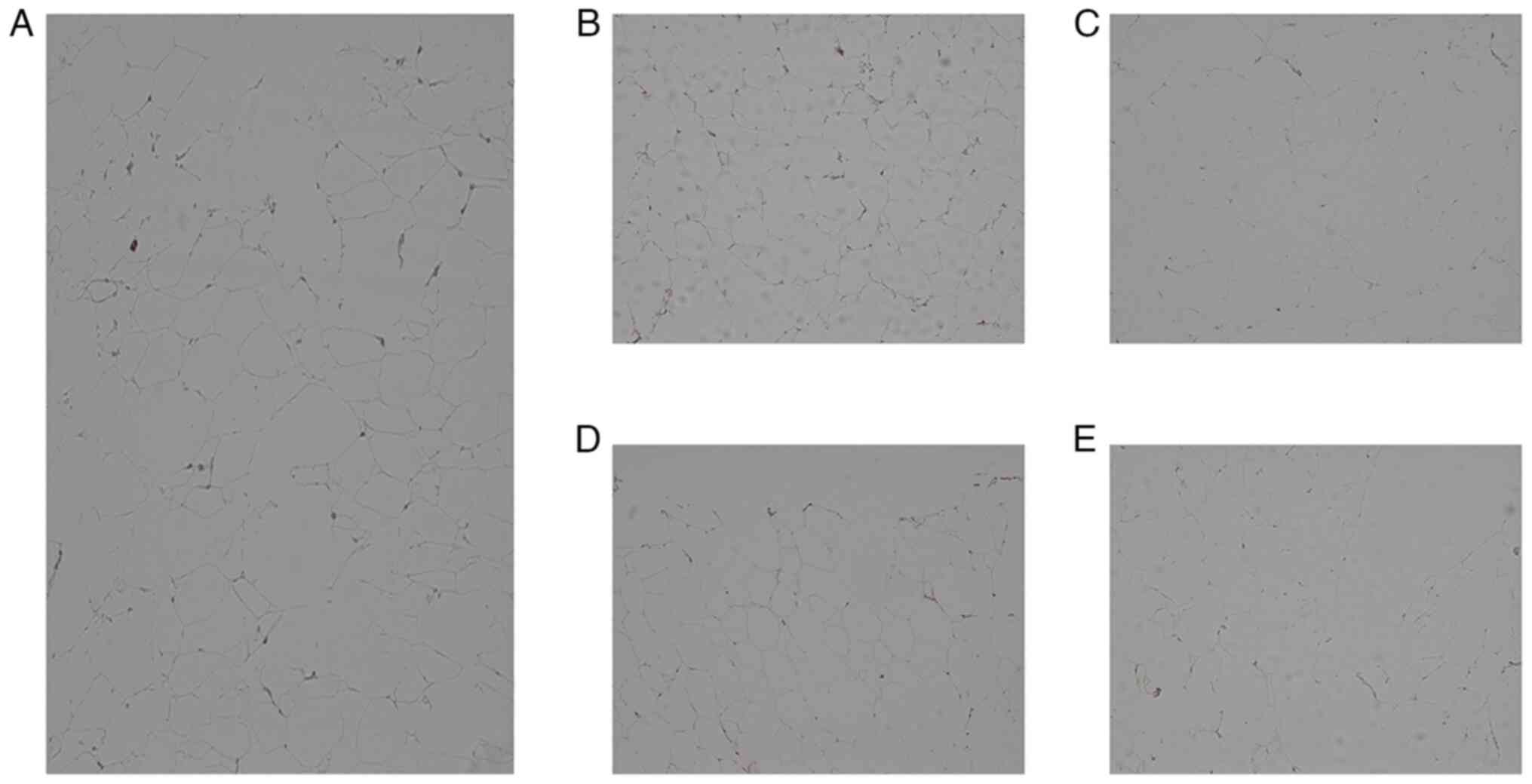
histopathological diagnosis was lipoma. Immunohistochemical
staining demonstrated that the mass was S100(+), CD34(-),
desmin(-), CDK4(-), MDM2(-) and Ki67(-) (Figs. 3 and 4).
Immunohistochemistry method
Tissue samples were placed in Eppendorf tubes and
fixed 4% polyformin for 24 h at room temperature. The tissues were
dehydrated using graded ethanol (70, 80, 95 and 100%), placed in
xylene for transparency and then embedded in paraffin wax in order
to cut them into thin slices (5 µm). Subsequently, paraffin slices
were placed on polylysine slides in a water bath at 45˚C and dried
for 2 h in a 60˚C drying oven.
Paraffin removal was performed with xylene for 10
min (2 times), followed by dehydration with 100, 95, 90, 80 and 70%
ethanol (5 min each). The sections were soaked in PBS for 5
min.
For diaminobenzidine staining (Beijing Zhongsan
Jinqiao Biotechnology Co.), the sections were treated with citrate
buffer with microwave heating for antigen repair, then washed with
PBS 3 times for 5 min each. The sections were then incubated with
3% H2O2 for 10 min at room temperature in
order to block endogenous peroxidase and washed in PBS 3 times for
5 min each. An immunohistochemistry pen was used to draw a circle
around the tissue to prevent the staining solution from flowing
away. Primary antibody was added in a dropwise manner and placed at
room temperature for 1 h, then left overnight at 4˚C. The next day,
the sections were taken out and shaken slowly at low speed on a
room temperature shaker for 1 h, before being allowed to rise to
room temperature and washed three times with PBS for 5 min each
time. Enzyme-labelled sheep anti-mouse/rabbit IgG polymer was added
in a dropwise manner and incubated for 20 min at room temperature,
before washing with PBS 3 times for 3 min each. Finally, the
sections were incubated with DAB for 5 min at room temperature and
washed with PBS 3 times for 2 min each. Staining with hematoxylin
was performed for 3 min, before washing with tap water. Hematoxylin
differentiation solution was used for a few seconds, before washing
with tap water, then returned to blue with hematoxylin and washed
with running water. Sections were then dehydrated in gradient
ethanol (70, 80, 95 and 100%), made transparent with xylene and
sealed with neutral gum. All images were taken using an optical
microscope (Nikon ECLIPSE CI-S; Nikon Coporation) with an image
analysis system (Nikon DS-U3; Nikon Coporation).
Primary antibodies used were as follows: S-100
(ready-to-use solution; cat. no. ZA-0225; rabbit anti-human
antibody; Beijing Zhongsan Jinqiao Biotechnology Co.), CD34
(ready-to-use solution; cat. no. ZM-0046; mouse anti-human
antibody; Beijing Zhongsan Jinqiao Biotechnology Co.), Desmin
(ready-to-use solution; cat. no. ZA-0610; rabbit anti-human
antibody; Beijing Zhongsan Jinqiao Biotechnology Co.), CDK4
(ready-to-use solution; cat. no. ZA-0614; rabbit anti-human
antibody; Beijing Zhongsan Jinqiao Biotechnology Co.), MDM2
(ready-to-use solution; cat. no. ZM-0425; mouse anti-human
antibody; Beijing Zhongsan Jinqiao Biotechnology Co.) and Ki-67
(ready-to-use solution; cat. no. ZM-0166; mouse anti-human
antibody; (Beijing Zhongsan Jinqiao Biotechnology Co.). The
secondary antibody was an anti-mouse/rabbit IgG (ready-to-use
solution; cat. no. UM-9002; Beijing Zhongsan Jinqiao Biotechnology
Co.).
Postoperative situation
On postoperative day 4, the urinary catheter was
removed as the patient had no discomfort. Subsequently, the patient
was discharged. At the time of writing the present report at the
1-month follow-up, the wound had healed well.
Discussion
Compared with giant lipomas of the body surface,
giant lipomas in the Retzius space are rare (5). The present case may provide a
reference for diagnosis and treatment of this condition in the
future.
The present patient had a left inguinal hernia,
which is usually associated with increased intra-abdominal
pressure. Common causes of increased intra-abdominal pressure are
cigarette smoking, chronic cough, obesity and poor urination
(1). However, the intra-abdominal
pressure was likely increased in the present patient because of the
presence of a large pelvic mass. The left inguinal hernia may have
developed secondary to the mass. The present case report suggested
that clinicians should consider the possibility of a pelvic mass in
patients with inguinal hernia.
Large pelvic masses usually raise the abdomen and
can be palpated. However, in the present case, physical examination
showed no abdominal swelling on inspection and no mass on
palpation. Abdominal CT demonstrated a large pelvic mass,
considered to be a lipoma. When no mass is palpable on abdominal
examination, the possibility of a large pelvic mass cannot be ruled
out and abdominal CT should be performed to confirm the diagnosis.
Here, no pelvic mass was found on physical examination because the
patient had a benign soft tissue mass in the retroperitoneal
position. The Retzius space is large and a soft tissue mass can
grow until it fills the entire space (6). As the peritoneum covering the tumor
exerts pressure on the tumor, the tumor is more likely to compress
loose connective tissue in the pelvic cavity, rather than push the
peritoneum up, thus manifesting as a pelvic mass (7). In summary, a large benign soft tissue
mass in the pelvic cavity may manifest as a flat abdomen and no
mass on palpation and this diagnosis could be confirmed by imaging
findings. For patients clinically considered to have a pelvic mass,
abdominal CT is helpful in confirming the diagnosis (8).
For large intra-abdominal masses, laparotomy is the
treatment of choice (9). Since the
1980s, minimally invasive laparoscopic surgery has been developed
and is widely used in many fields, such as general surgery,
gynecology and urology (10).
Previous clinical studies have reported that compared with open
surgery, minimally invasive laparoscopic surgery is less traumatic
to patients, causes significantly less pain and leads to
significantly faster postoperative recovery (11,12).
In addition, laparoscopic surgery can aid in evaluating the
association between the tumor and surrounding organs
intraoperatively and can be used to identify the blood vessels of
the tumor (13). However, only a
few cases of large intra-abdominal tumors treated with laparoscopic
resection have been reported and clinical experience with the
distribution of the trocar, the position of the operator and the
manner in which the procedure is performed remains insufficient
(14-17).
In 2009, Shiroshita et al (13) performed laparoscopic resection of a
giant lipoma in the omentum of a 71-year-old male. Abdominal
ultrasonography demonstrated a hyperechoic mass in the abdominal
cavity and preoperative CT scan led to a preliminary diagnosis of
lipoma. Considering that the tumor originated from the omentum, a
transperitoneal approach was undertaken. The tumor was resected
endoscopically and 10 mm trocars were placed on, above and below
the umbilicus. Intraoperatively, the tumor measured ~29x19x3 cm and
postoperative histopathology confirmed that the tumor was a lipoma.
Using laparoscopy, Choi et al (18) resected a large abdominal lipoma
with a diameter of ~20 cm in a 36-year-old male. The chief
complaint of the patient was frequent urination, and a physical
examination showed no abdominal mass. Urinalysis results were
within the healthy expected ranges. CT scan showed a mass of ~20x11
cm, located between the abdominal wall muscles and compressed
bladder, within the peritoneum. The postoperative histopathological
diagnosis was benign lipoma.
In the present case, preoperative abdominal CT
indicated that the pelvic mass was likely benign, soft and with a
clear boundary with the surrounding tissues. Therefore, complete
laparoscopic resection of the large pelvic mass was attempted.
Intraoperatively, because the D trocar was located
in the left lower abdomen, when separating the left side of the
tumor, the tumor could not initially be removed because the
distance between the B and D trocars was too small. Separation on
the left border of the mass was difficult. Adhesion between the
tumor and surrounding tissue could not be ruled out preoperatively,
nor could the requirement of adhesion release be ruled out
intraoperatively. Therefore, based on the findings during the
operation, the trocar position A was better for observation. The
positions of the A and B trocars remained unchanged. The C trocar
was inserted at the junction of the left midclavicular line and a
line drawn 2 cm above the navel. The D and E trocars were inserted
at the junction of lines 2 cm lateral to the left and right
midclavicular lines with a line 2 cm below the navel, respectively.
The navel functioned as an auxiliary hole.
When resecting the specimen, considering that the
tumor was soft and benign, a small incision was made measuring ~5
cm. However, the tumor could not be removed smoothly. Therefore,
the opening was enlarged to ~8 cm. Subsequently, removal of the
mass was successful but partial tearing of the specimen occurred.
Therefore, for such tumors, to ensure integrity of the specimen,
small incisions should not be excessively manipulated and the
incision should be directly extended to an appropriate length.
Iatrogenic bladder injury is a relatively common
complication of pelvic surgery, with an incidence reaching 4.5%
(19,20). In the present case, the pelvic
lipoma adhered tightly to the bladder wall and surgical treatment
risked damaging the bladder wall. To avoid damaging the bladder
wall during surgery, the bladder should be fully emptied by
inserting a urinary catheter preoperatively. In addition, when the
boundary of the bladder cannot be clearly defined intraoperatively,
fluid or CO2 can be injected into the bladder to clarify
the boundary (19,21). If bladder injury is suspected
intraoperatively, cystoscopy can be performed to confirm injury
(22,23). In the present case, preoperative CT
indicated that the tumor was close to the bladder and the
possibility that the tumor originated from the bladder could not be
ruled out.
In conclusion, the present study is a preliminary
report of the successful diagnosis and treatment of a giant lipoma
in the Retzius space.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Beijing
Municipal Science & Technology Commission (grant no.
Z221100007422005).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LW and NWZ made contributions to the study
conception and design. CXT, CYY, BA and JW contributed to the
acquisition of data. WJC and MYS contributed to the analysis and
interpretation of data. NWZ, GZX, DBL and TXL performed the
surgery. LXT, ZW and DXD performed the imaging. MYS, LXT and JW
advised on patient treatment. TXL and JW confirm the authenticity
of all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient consented to the use of their clinical
information/data and images for the purpose of research and their
publication. The patient provided written informed consent.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hewitt DB: Groin Hernia. JAMA.
317(2560)2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wagaskar VG, Mittal A, Sobotka S, Ratnani
P, Lantz A, Falagario UG, Martini A, Dovey Z, Treacy PJ, Pathak P,
et al: Hood technique for robotic radical prostatectomy-preserving
periurethral anatomical structures in the space of retzius and
sparing the pouch of douglas, enabling early return of continence
without compromising surgical margin rates. Eur Urol. 80:213–221.
2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Jóźwik M, Kołodziejczak M,
Klonowska-Dziatkiewicz E and Jóźwik M: Giant vulvar lipoma in an
adolescent girl: A case study and literature review. J Pediatr
Adolesc Gynecol. 27:e117–e119. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sergey K and Svetlana VB: Nasopharyngeal
Lipoma: Clinical Case. Laryngoscope. 131:E1099–E1102.
2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Okuda H: Spindle cell lipoma in Retzius'
space. Int J Urol. 16:218–219. 2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Asakage N: Paradigm shift regarding the
transversalis fascia, preperitoneal space, and Retzius' space.
Hernia. 22:499–506. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chen X, Kang C and Zhang M: Imaging
features of urachal cancer: A case report. Front Oncol.
9(1274)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Bebobru M, Nasri FA, Niculescu-Valaenu M
and Friedhoff K: Retrorectal teratoma (dermoid cyst) of an
adult-Diagnosis and treatment based on an example of a case report.
Dtsch Med Wochenschr. 146:104–107. 2021.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
9
|
Koehne EL, Bajic P and Gupta GN:
Robotic-assisted laparoscopic retroperitoneal adrenalectomy. Surg
Oncol. 31(7)2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Vecchio R, MacFayden BV and Palazzo F:
History of laparoscopic surgery. Panminerva Med. 42:87–90.
2000.PubMed/NCBI
|
|
11
|
Kapritsou M, Korkolis DP and Konstantinou
EA: Open or laparoscopic surgery for colorectal cancer: A
retrospective comparative study. Gastroenterol Nurs. 36:37–41.
2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Cha JM, Lee JI, Joo KR, Choe JW, Jung SW,
Shin HP, Kim HC, Lee SH and Lim SJ: Giant mesenteric lipoma as an
unusual cause of abdominal pain: A case report and a review of the
literature. J Korean Med Sci. 24:333–336. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Shiroshita H, Komori Y, Tajima M, Bandoh
T, Arita T, Shiraishi N and Kitano S: Laparoscopic examination and
resection for giant lipoma of the omentum: A case report and review
of related literature. Surg Laparosc Endosc Percutan Tech.
19:e217–e220. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Jiang L, Zhao X, Han Y, Liu K and Meng X:
Giant ovarian cysts treated by single-port laparoscopic surgery: A
case series. Front Oncol. 11(796330)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Dolan MS, Boulanger SC and Salameh JR:
Laparoscopic management of giant ovarian cyst. JSLS. 10:254–256.
2006.PubMed/NCBI
|
|
16
|
Postma VA, Wegdam JA and Janssen IM:
Laparoscopic extirpation of a giant ovarian cyst. Surg Endosc.
16(361)2002.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bhandarkar D, Ghuge A, Kadakia G and Shah
R: Laparoscopic excision of an omental leiomyoma with a giant
cystic component. JSLS. 15:409–411. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Choi H, Ryu D, Choi JW, Xu Y and Kim Y: A
giant lipoma of the parietal peritoneum: Laparoscopic excision with
the parietal peritoneum preserving procedure-a case report with
literature review. BMC Surg. 18(49)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Saaqib S, Iqbal A, Naheed M, Saeed T and
Khalid M: A randomized controlled trial of cystoinflation to
prevent bladder injury in the adhesive disease of multiple
caesarean sections. Sci Rep. 10(15297)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Vorobev V, Beloborodov V, Golub I, Frolov
A, Kelchevskaya E, Tsoktoev D and Maksikova T: Urinary system
iatrogenic injuries: Problem review. Urol Int. 105:460–469.
2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Findley AD and Solnik MJ: Prevention and
management of urologic injury during gynecologic laparoscopy. Curr
Opin Obstet Gynecol. 28:323–328. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Rao D, Yu H, Zhu H and Duan P: The
diagnosis and treatment of iatrogenic ureteral and bladder injury
caused by traditional gynaecology and obstetrics operation. Arch
Gynecol Obstet. 285:763–765. 2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Vakili B, Chesson RR, Kyle BL, Shobeiri
SA, Echols KT, Gist R, Zheng YT and Nolan TE: The incidence of
urinary tract injury during hysterectomy: A prospective analysis
based on universal cystoscopy. Am J Obstet Gynecol. 192:1599–1604.
2005.PubMed/NCBI View Article : Google Scholar
|