Introduction
Genitourinary syndrome of menopause (GSM) is
prevalent in post-menopausal women and is associated with vaginal
itching, burning, dryness, dyspareunia and urinary tract
dysfunction (1). GSM affects ~50%
of women after menopause and leads to reduced sexual function and
poor quality of life (2). GSM
results from the reduction in estrogen and subsequent anatomical
and functional changes in the urogenital tissues, such as reduction
in vaginal blood flow, increase in pH, altered expression levels of
elastin and collagen, reduction in secretions and thinning of the
epithelium (1). The resulting
symptoms of vaginal itching, burning, dryness, dyspareunia, painful
sexual activity and urinary tract dysfunction of varying
intensities are associated with a reduced quality of life (2,3).
Guidelines from the North American Menopause Society
state that the initial management protocol of GSM includes vaginal
moisturizers, lubricants and continuation of sexual activity
(4). Lubricants are a temporary
solution that are used during sexual activity to reduce tissue
irritation; however, moisturizers are longer acting and aim to
reduce dryness and vaginal pH thereby reducing GSM. Additionally,
local estrogen therapies are also effective in managing moderate to
severe cases of GSM as they specifically target the underlying
pathology, namely the hypoestrogenic vaginal tissue (5). Nevertheless, local estrogen therapies
have relatively low compliance (6). Topical estrogens often lead to
incomplete relief of symptoms, and their effect stops with
discontinuation of treatment. Therefore, other modes of therapy for
this condition are needed (6).
In the past decade, laser therapy using a general
fractionated CO2 laser has, anecdotally, become
increasingly utilized in the management of GSM. CO2
laser therapy utilizes a gaseous medium to deliver a laser at
10,600 nm which is rapidly absorbed by water molecules to penetrate
the vulvovaginal tissues (7). In a
systematic review and meta-analysis of 25 studies, Filippini et
al (8) reported that
CO2 laser therapy was effective in alleviating GSM.
However, the quality of evidence, assessed using risk of bias
tools, was low to very low, as most studies were observational
without any randomization. GSM is characterized by symptoms that
are mainly subjective, such as itching, burning and dryness;
therefore it is important that a placebo effect is negated during
the assessment of the efficacy of any treatment. Therefore, the
present systematic review and meta-analysis evaluated
sham-controlled trials to assess the efficacy of CO2
laser therapy for the management of GSM.
Materials and methods
Search source and strategy
The present review was registered on PROSPERO (ID
no. CRD42023432973). A systematic search of the literature for
studies that were published from inception to June 30, 2023 was
performed by two reviewers, separately. The databases examined were
as follows: PubMed, Embase, Web of Science, CENTRAL and Scopus.
Google Scholar was also searched for gray literature.
The inclusion of studies was based on the following
Population, Intervention, Comparison, Outcome and Study type
(PICOS) criteria: P, menopausal women with GSM; I, use of
CO2 laser therapy; C, sham laser therapy; O, GSM
evaluated by any standardized scale; and S, randomized controlled
trials (RCTs). Non-randomized studies, studies using active
treatment modality in the control group, editorials, theses,
non-peer-reviewed studies and animal studies were excluded.
The search for studies was based on the following
keywords: ‘menopause’; ‘genitourinary’; ‘vulvovaginal atrophy’;
‘carbon dioxide’; ‘CO2’; ‘laser’; and ‘randomized’.
Different search strings were generated using ‘AND’ and ‘OR’. The
search strings were similar across databases. Search details are
listed in Table SI.
Study selection
Two reviewers independently evaluated all the search
results. First, the retrieved data was collated and deduplicated
electronically using Mendeley (version 1.19.8, Elsevier). The
titles and abstracts of all articles were screened to identify
relevant studies based on the aforementioned inclusion criteria.
The selected studies underwent full-text analysis. The reviewers
screened these studies based on the eligibility criteria for
further inclusion. Any disagreements were solved by discussion and
consensus between the reviewers. The reference lists of the
included studies were also examined to identify any other relevant
articles.
Extracted data and outcomes
The following data were extracted from the selected
articles by two reviewers independently: First author; year of
publication; study location; inclusion criteria; laser type; laser
energy settings; number of laser sessions; sample size; participant
age; years since menopause; study outcomes; and follow-up period.
Study details extracted by the two reviewers were then
cross-matched and any discrepancies were resolved.
Risk of bias analysis
Risk of Bias 2 tool (The Cochrane Collaboration,
release date 22 August 2019) was used for quality assessment
(9). For each domain of the
assessment tool, studies were marked as having a low or high risk
of bias, or as having some concerns. The different domains of the
tool included: randomization process; deviation from intended
intervention; missing outcome data; measurement of outcomes;
selection of reported results; and overall risk of bias.
Statistical analysis
The present review was performed according to the
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
guidelines (10). Statistical
analysis was performed using Review Manager (RevMan; version 5.3;
The Cochrane Collaboration). The outcomes for meta-analysis were
selected based on the availability of data from ≥3 studies. Data
were combined to generate a mean difference (MD) with 95%
confidence intervals (CI). Results are presented in the form of
forest plots. The meta-analysis was conducted using the
random-effects model. Funnel plots were not generated due to a low
number of studies included in the meta-analysis. Inter-study
heterogeneity analysis was performed, yielding an I2
value, <50% suggested low heterogeneity and >50% suggested
substantial heterogeneity between studies.
Results
Search results
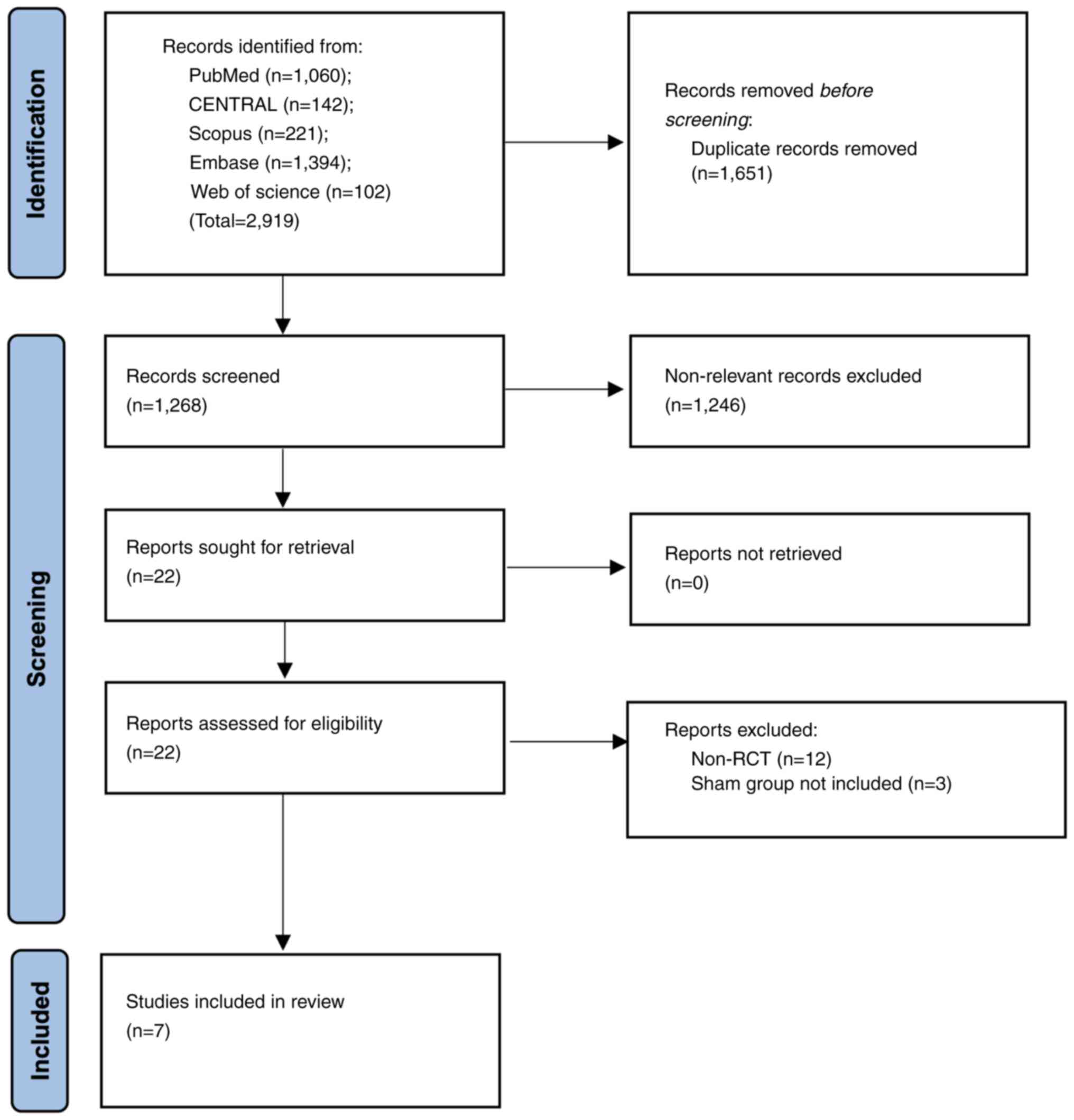
A total of 2,919 articles were initially retrieved.
Duplicate articles were excluded and further screening was
performed on 1,268 records, of which 22 studies were found to be
suitable for full-text analysis. Finally, seven articles were
selected for the final review and meta-analysis (11-17).
The search strategy is presented in Fig. 1.
Study details
Details of included studies are listed in Table I. All RCTs were published in the
past three years and were from Thailand, Italy, Greece, United
States of America, Belgium, Spain and Australia. The participants
of two RCTs included only gynecological or breast cancer survivors
with GSM. The remaining RCTs did not have restrictive inclusion
criteria. The same fractionated CO2 laser equipment was
used in all trials, whilst the energy output used was either 30 or
40 W. In the control groups, the same laser equipment was used as
in the treatment groups, but without any laser emitted. A total of
three sessions of laser therapy were used in 6/7 studies, performed
4-8 weeks apart. Only one trial used five sessions of laser
therapy. There were 8-44 patients per group and follow-up was 3-6
months. The risk of bias of each study, assessed using risk of bias
analysis, is presented in Table
II. All included studies were determined to be high-quality
RCTs with a low risk of bias.
 | Table ICharacteristics of the randomized
control trials included in the review and meta-analysis. |
Table I
Characteristics of the randomized
control trials included in the review and meta-analysis.
| First author/s,
year | Country | Inclusion
criteria | CO2
laser | No. of laser
sessions | Control | Groups | Sample size | Age, years mean ±
standard deviation or median (range) | Post-menopause,
years | Follow-up,
months | (Refs.) |
|---|
| Mension et al,
2023 | Spain | Breast cancer
survivors >30 years receiving aromatase inhibitors; menopause,
signs or symptoms of GSM with dyspareunia, and vaginal pH ≥5; and
sexually active | SmartXide2 V2LR
Monalisa Touch; 40 W power, 1,000 µs dwell time | 5, 1 month apart | Sham laser | Laser | 35 | 52.3±8.3a | NR | 6 | (14) |
| | | | | | | Control | 37 | | | | |
| Page et al,
2022 | Belgium | Moderate to severe
symptoms of GSM (namely. vaginal dryness, vaginal itching, vaginal
burning, dyspareunia and dysuria) shown by an MBS score of ≥2 | SmartXide2 V2LR
Monalisa Touch; 30 W power, 1,000 µs dwell time | 3, 4 weeks
apart | Sham laser | Laser | 29 | 57.4±7.1 | 7.3±5.2 | 3 | (12) |
| | | | | | | Control | 29 | 56.2±6.3 | 6.4±5.6 | | |
| Quick et al,
2021 | USA | Gynecologic cancer
survivors with GSM | SmartXide2 V2LR
Monalisa Touch; 30 W power, 1,000 µs dwell time | 3, 1 month
apart | Sham laser | Laser | 10 | 56.0±11.2 | NR | 4 | (11) |
| | | | | | | Control | 8 | 56.8±6.0 | | | |
| Li et al,
2021 | Australia | Symptomatic
amenorrheic for ≥12 months | SmartXide2 V2LR
Monalisa Touch; 40 W power, 1,000 µs dwell time | 3, 4-8 weeks
apart | Sham laser | Laser | 43 | 55±7 | 8 (4-14) | 6 | (13) |
| | | | | | | Control | 42 | 58±8 | 6 (3-9) | | |
| Cruff and
Khandwala, 2021 | USA | Menopausal women
(or status-post bilateral oophorectomy) with dyspareunia or vaginal
dryness rated as moderate-severe, who were desirous of sexual
function | SmartXide2 V2LR
Monalisa Touch; 30W power, 1,000 µs dwell time | 3, 6 weeks
apart | Sham laser | Laser | 16 | 61 (54-66) | 14 (5-24) | 6 | (15) |
| | | | | | | Control | 14 | 59 (56-65) | 10 (4-15) | | |
| Salvatore et
al, 2020 | Greece, Italy | Postmenopausal
women with GSM diagnosis according to the International Society for
the Study of Women's Sexual Health and The North American Menopause
Society definitions | SmartXide2 V2LR
Monalisa Touch; 30 W power, 1,000 µs dwell time | 3, 1 month
apart | Sham laser | Laser | 28 | 57.0±6.9 | 8.2±4.9 | 4 | (16) |
| | | | | | | Control | 30 | 58.4±6.0 | 8.7±4.9 | | |
| Ruanphoo and
Bunyavejchevin, 2020 | Thailand | Postmenopausal
women with moderate to severe intensity of any vaginal atrophy
symptom | SmartXide2 V2LR
Monalisa Touch; 40 W power, 1,000 µs dwell time | 3, 4 weeks
apart | Sham laser | Laser | 44 | 48.9±3.0 | NR | 3 | (17) |
| | | | | | | Control | 44 | 49.5±3.9 | | | |
 | Table IIRisk of bias analysis of the
randomized control trials included in the review and
meta-analysis. |
Table II
Risk of bias analysis of the
randomized control trials included in the review and
meta-analysis.
| | Risk | |
|---|
| First author/s,
year | Randomization
process | Deviation from
intended intervention | Missing outcome
data | Measurement of
outcomes | Selection of
reported results | Overall risk of
bias | (Refs.) |
|---|
| Mension et
al, 2023 | Low | Low | Low | Low | Low | Low | (14) |
| Page et al,
2022 | Low | Low | Low | Low | Low | Low | (12) |
| Quick et al,
2021 | Low | Low | Low | Low | Low | Low | (11) |
| Li et al,
2021 | Low | Low | Low | Low | Low | Low | (13) |
| Cruff and
Khandwala, 2021 | Low | Low | Low | Low | Low | Low | (15) |
| Salvatore et
al, 2020 | Low | Low | Low | Low | Low | Low | (16) |
| Ruanphoo and
Bunyavejchevin, 2020 | Low | Low | Low | Low | Low | Low | (17) |
Meta-analysis
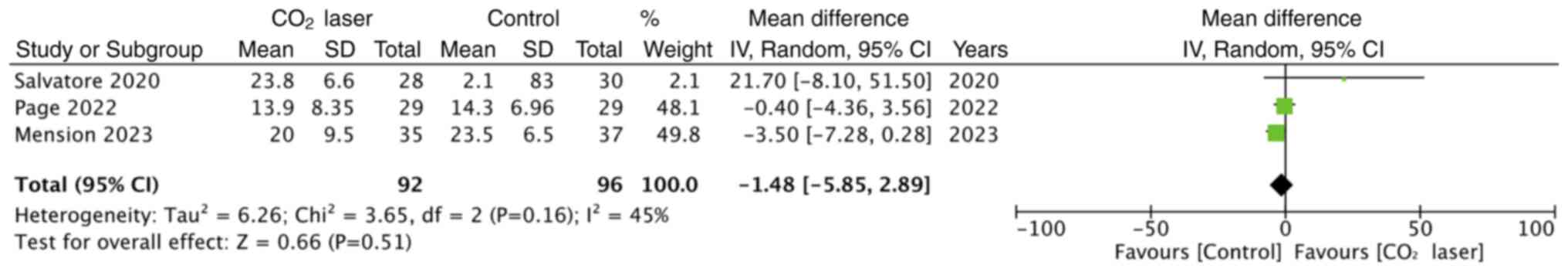
The study outcomes selected for quantitative
analysis, based on the availability of data, were Female Sexual
Function Index (FSFI), Vaginal Health Index (VHI) and visual analog
scale (VAS) for dyspareunia, dryness, burning, itching and dysuria.
A total of three studies reported a final FSFI score at follow-up.
Meta-analysis demonstrated there was no statistically significant
difference in FSFI scores between laser and control groups
(Fig. 2). Additionally, two
studies only reported changes in FSFI scores and therefore, their
results were not included in the meta-analysis. Quick et al
(11) reported significantly
improved FSFI scores in the laser group compared with the control
group (P=0.02), whilst Cruff and Khandwala (15) reported no significant difference in
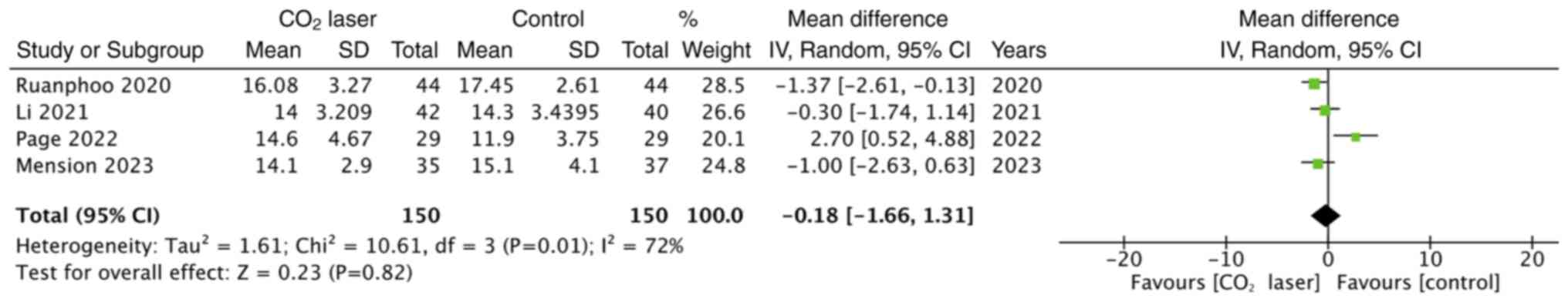
FSFI score changes between the two groups (P=0.77). A total of four
studies reported data on VHI, however the pooled analysis
demonstrated no statistically significant difference in VHI scores
between laser and sham groups (Fig.
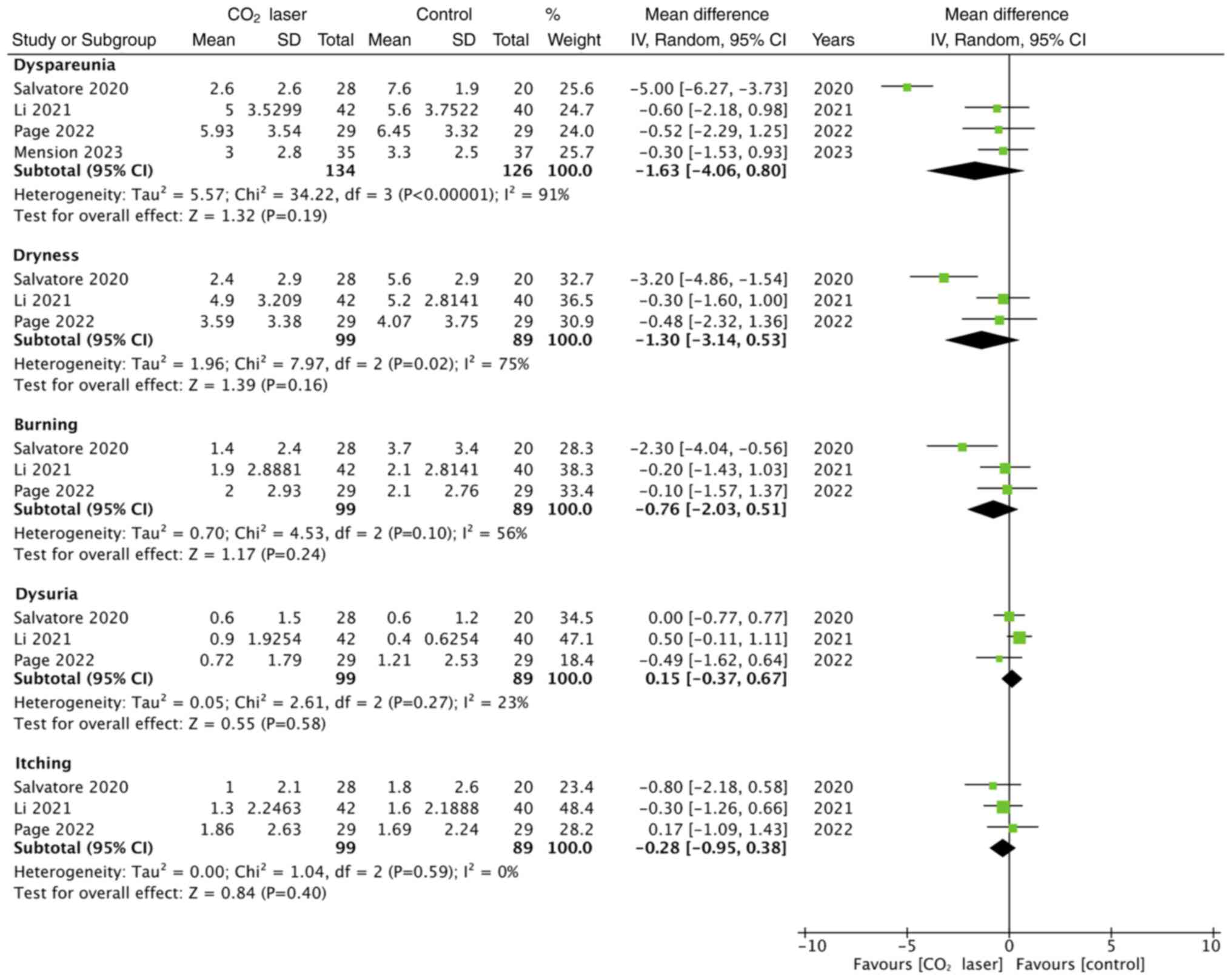
3). The meta-analysis also demonstrated no statistically
significant difference in VAS scores for dyspareunia (n=4), dryness
(n=3), burning (n=3), itching (n=3) and dysuria (n=3) between the
laser and control groups (Fig.
4).
Discussion
In 2013, the North American Menopause Society
(18) recommended the
administration of systemic estrogen or local low-dose estrogen for
the management of moderate-to-severe or mild-unresponsive GSM.
Nevertheless, certain women with GSM decline the use of these
therapies due to fear of side effects (such as stress
incontinence), compliance issues, inadequate efficacy and
contraindications (19). In the
past decade, traditional therapies for GSM such as topical
estrogens have begun to be substituted with innovations such as
CO2 laser therapy which was first introduced in
2014(7). Previous studies reported
that CO2 laser treatment was associated with certain
histological changes in the vulvovaginal tissues which could
potentially alter the severity of GSM (20). Zerbinati et al (21) reported that CO2 laser
therapy restored the thick vaginal epithelial lining, increased
collagen and ground substance in the lamina propria and increased
the vascular supply of the tissue. The fractional CO2
laser mode of action is based on the production of heat by
vaporization of water present in the cells of deeper lamina
propria. The energy of the laser is precisely directed to avoid
damage to the surrounding tissues. As a result of this
hyper-regulated injury, there is neoangiogenesis and
neocollagenesis which could improve the vaginal environment and GSM
symptoms (22).
CO2 laser therapy has been used for GSM
(8), however there is still a lack
of high-quality evidence to guide clinical practice. In 2018, the
United States Food and Drug Administration stated that there was
inadequate data to recommend laser therapies for the optimization
of sexual function and reduction of symptoms of GSM (23). Most of the data for the use of
CO2 laser therapy is from observational studies which
have a high risk of bias (8). A
large meta-analysis of 25 such studies (8) reported that CO2 laser
therapy significantly reduced symptoms of dryness (MD, -5.15; 95%
CI, -5.72, -4.58), dyspareunia (MD, -5.27; 95% CI, -5.93, -4.62),
itching (MD, -2.75; 95% CI, -4.0, -1.51), burning (MD, -2.66; 95%
CI, -3.75, -1.57) and dysuria (MD, -2.14; 95% CI, -3.41, -0.87) in
patients with GSM. Moreover, the FSFI score was significantly
improved. However, the non-randomization of study participants and
lack of blinding of participants and outcome assessors generated
bias which hampered the interpretation and acceptance of such
results (24). Another recent
narrative review by D'Oria et al (25) reported that CO2 laser
therapy was an effective and safe therapeutic option for treatment
of vulvovaginal atrophy in gynecological cancer survivors. However,
only nine studies were evaluated and quantitative synthesis was not
performed. Furthermore, Khamis et al (26) pooled data from three
sham-controlled trials and reported that CO2 laser
therapy resulted in significant improvements in VAS score, FSFI and
patient satisfaction in patients with GSM. The low number of trials
included failed to generate adequate outcome data and provide high
quality evidence, despite only evaluating RCTs.
Therefore, the present review provided higher
quality evidence for the efficacy of CO2 laser therapy
in the management of GSM. As, to the best of our knowledge, this is
the first review that has assessed the efficacy of CO2
laser for GSM by using pooled analysis of only high-quality
sham-controlled RCTs. The present study did not include trials that
used an active comparator or placebo, namely no laser in the
control group. All patients in control groups were blinded and the
same laser equipment with no energy settings was applied for the
same duration for all participants. Thus, the placebo effect was
well-controlled in these trials (24). Additionally, all trials were
blinded for outcome assessment to reduce bias in the results.
Scores reported by ≥3 studies in a meta-analysis were combined to
evaluate the efficacy of CO2 laser therapy, from which
it was demonstrated that this treatment modality did not result in
any significant differences in outcomes in patients with GSM. There
was no statistically significant difference in total FSFI, VHI and
VAS scores for dyspareunia, dryness, burning, itching and
dysuria.
However, the participants of two of the included
trials included only cancer survivors with GSM. Endocrine therapies
used for the treatment of breast and gynecological cancer often
result in adverse events including sexual dysfunction. Patients
report problems with sexual desire, interest, arousal, orgasm and
genitopelvic pain, and these symptoms are often underdiagnosed and
undertreated (27). Patients are
often treated using vaginal lubricants, moisturizers, estrogen,
dehydroepiandrosterone, ospemifene and counseling, but with limited
effects. It has been previously reported that combination therapies
may be more beneficial in this subgroup of patients (28). Moreover, given the scarce evidence
for CO2 laser therapy for the management of GSM in
cancer survivors, there is a need for further trials focused
specifically on this cohort (27,28).
The trials included in the present review did not
report any major adverse events associated with the use of
CO2 lasers. A previous study also reported that
CO2 lasers are safe and are associated with minimal
complications (29). The
Manufacturer and User Facility Device Experience database, which
monitors laser-based adverse events for vaginal rejuvenation,
reported that pain, numbing and burning are the most common adverse
effects of CO2 laser therapy (30). Nevertheless, in certain patients,
CO2 laser therapy can cause serious complications, such
as fibrosis, scarring, agglutination and penetrating injury. These
outcomes need to be assessed in future trials (29).
There are certain limitations to the present review
and meta-analysis. The number of RCTs included (n=7) was low with
variations in the outcome scores and only three or four studies
included in each meta-analysis. Additionally, the heterogeneity in
four of the meta-analyses was high. This could be due to variations
in the severity of baseline patient symptoms, differences in
patient inclusion criteria and the protocol of CO2 laser
sessions. However, due to the small number of studies in the
meta-analysis, the source of the heterogeneity could not be
evaluated using subgroup or meta-regression analysis. Moreover, all
trials reported only short-term follow-up data (<1 year). The
potential long-term benefits of CO2 laser therapy for
the management of GSM are still unknown.
In conclusion, the present meta-analysis of
high-quality sham-controlled randomized trials demonstrated that
CO2 laser treatment may not have any beneficial effect
on GSM. The present meta-analysis and qualitative analysis failed
to demonstrate any significant effect of CO2 laser
therapy on GSM, with no significant difference in FSFI, VHI and VAS
scores for dyspareunia, dryness, burning, itching and dysuria with
the use of a CO2 laser. The limited data and high
heterogeneity in meta-analyses in this area of research are
important limitations that need to be addressed by future RCTs.
Supplementary Material
Key words and search strings used in
the search for studies.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YN conceived and designed the study. YN and JL
collected the data and reviewed the literature. YN wrote the
manuscript. YN and JL have read and approved the final manuscript.
YN and JL confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gandhi J, Chen A, Dagur G, Suh Y, Smith N,
Cali B and Khan SA: Genitourinary syndrome of menopause: An
overview of clinical manifestations, pathophysiology, etiology,
evaluation, and management. Am J Obstet Gynecol. 215:704–711.
2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Parish SJ, Nappi RE, Krychman ML,
Kellogg-Spadt S, Simon JA, Goldstein JA and Kingsberg SA: Impact of
vulvovaginal health on postmenopausal women: A review of surveys on
symptoms of vulvovaginal atrophy. Int J Womens Health. 5:437–447.
2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mac Bride MB, Rhodes DJ and Shuster LT:
Vulvovaginal atrophy. Mayo Clin Proc. 85:87–94. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
North American Menopause Society. The role
of local vaginal estrogen for treatment of vaginal atrophy in
postmenopausal women: 2007 position statement of The North American
Menopause Society. Menopause. 14:357–369. 2007.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Benini V, Ruffolo AF, Casiraghi A,
Degliuomini RS, Frigerio M, Braga A, Serati M, Torella M, Candiani
M and Salvatore S: New innovations for the treatment of
vulvovaginal atrophy: An up-to-date review. Medicina (Kaunas).
58(770)2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Radnia N, Hosseini S, Vafaei S, Pirdehghan
A and Mehrabadi N: The effect of conjugated estrogens vaginal cream
and a combined vaginal cream of vitamins D and E in the treatment
of genitourinary syndrome. J Fam Med Prim Care.
12(507)2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Rabley A, O'Shea T, Terry R, Byun S and
Louis Moy M: Laser therapy for genitourinary syndrome of menopause.
Curr Urol Rep. 19(83)2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Filippini M, Porcari I, Ruffolo AF,
Casiraghi A, Farinelli M, Uccella S, Franchi M, Candiani M and
Salvatore S: CO2-Laser therapy and genitourinary
syndrome of menopause: A systematic review and meta-analysis. J Sex
Med. 19:452–470. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Higgins J, Thomas J, Chandler J, Cumpston
M, Li T, Page MJ and Welch VA (eds): Cochrane Handbook for
Systematic Reviews of Interventions. 2nd edition. John Wiley &
Sons, Chichester, UK, 2019.
|
|
10
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. Int J Surg. 88(105906)2021.PubMed/NCBI View
Article : Google Scholar
|
|
11
|
Quick AM, Dockter T, Le-Rademacher J,
Salani R, Hudson C, Hundley A, Terstriep S, Streicher L, Faubion S,
Loprinzi CL, et al: Pilot study of fractional CO2 laser
therapy for genitourinary syndrome of menopause in gynecologic
cancer survivors. Maturitas. 144:37–44. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Page AS, Verbakel JY, Verhaeghe J, Latul
YP, Housmans S and Deprest J: Laser versus sham for genitourinary
syndrome of menopause: A randomised controlled trial. BJOG.
130:312–319. 2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Li FG, Maheux-Lacroix S, Deans R,
Nesbitt-Hawes E, Budden A, Nguyen K, Lim CY, Song S, McCormack L,
Lyons SD, et al: Effect of fractional carbon dioxide laser vs. sham
treatment on symptom severity in women with postmenopausal vaginal
symptoms: A randomized clinical trial. JAMA. 326:1381–1389.
2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mension E, Alonso I, Anglès-Acedo S, Ros
C, Otero J, Villarino Á, Farré R, Saco A, Vega N, Castrejón N, et
al: Effect of fractional carbon dioxide vs. sham laser on sexual
function in survivors of breast cancer receiving aromatase
inhibitors for genitourinary syndrome of menopause: The LIGHT
randomized clinical trial. JAMA Netw Open.
6(E2255697)2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Cruff J and Khandwala S: A double-blind
randomized sham-controlled trial to evaluate the efficacy of
fractional carbon dioxide laser therapy on genitourinary syndrome
of menopause. J Sex Med. 18:761–769. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Salvatore S, Pitsouni E, Grigoriadis T,
Zacharakis D, Pantaleo G, Candiani M and Athanasiou S:
CO2 laser and the genitourinary syndrome of menopause: A
randomized sham-controlled trial. Climacteric. 24:187–193.
2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ruanphoo P and Bunyavejchevin S: Treatment
for vaginal atrophy using microablative fractional CO2
laser: A randomized double-blinded sham-controlled trial.
Menopause. 27:858–863. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Management of symptomatic vulvovaginal
atrophy: 2013 position statement of The North American Menopause
Society. Menopause. 20:888–902. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kingsberg SA and Krychman ML: Resistance
and barriers to local estrogen therapy in women with atrophic
vaginitis. J Sex Med. 10:1567–1574. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Salvatore S, Maggiore ULR, Athanasiou S,
Origoni M, Candiani M, Calligaro A and Zerbinati N: Histological
study on the effects of microablative fractional CO2
laser on atrophic vaginal tissue: An ex vivo study. Menopause.
22:845–849. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zerbinati N, Serati M, Origoni M, Candiani
M, Iannitti T, Salvatore S, Marotta F and Calligaro A: Microscopic
and ultrastructural modifications of postmenopausal atrophic
vaginal mucosa after fractional carbon dioxide laser treatment.
Lasers Med Sci. 30:429–436. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Perino A, Calligaro A, Forlani F, Tiberio
C, Cucinella G, Svelato A, Saitta S and Calagna G: Vulvo-vaginal
atrophy: A new treatment modality using thermo-ablative fractional
CO2 laser. Maturitas. 80:296–301. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
U.S. Food and Drug Administration:
Statement from FDA Commissioner Scott Gottlieb, M.D., on efforts to
safeguard women's health from deceptive health claims and
significant risks related to devices marketed for use in medical
procedures for ‘vaginal rejuvenation’. https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottlieb-md-efforts-safeguard-womens-health-deceptive-health-claims#:~:text=We%20are%20deeply%20concerned%20women,as%20condylomas%20(genital%20warts).
Accessed June 30, 2023.
|
|
24
|
Gorayeb RP, Forjaz MJ, Ferreira AG and
Ferreira JJ: Use of sham interventions in randomized controlled
trials in neurosurgery. J Neurol Surg A Cent Eur Neurosurg.
81:456–462. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
D'Oria O, Giannini A, Buzzaccarini G,
Tinelli A, Corrado G, Frega A, Vizza E and Caserta D: Fractional
CO2 laser for vulvo-vaginal atrophy in gynecologic
cancer patients: A valid therapeutic choice? A systematic review.
Eur J Obstet Gynecol Reprod Biol. 277:84–89. 2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Khamis Y, Abdelhakim AM, Labib K, Islam
BA, Nassar SA, Motaal AOA, Saleh DM, Abdou H, Abbas AM and Mojahed
EM: Vaginal CO2 laser therapy versus sham for
genitourinary syndrome of menopause management: A systematic review
and meta-analysis of randomized controlled trials. Menopause.
28:1316–1322. 2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Seav SM, Dominick SA, Stepanyuk B, Gorman
JR, Chingos DT, Ehren JL, Krychman ML and Su HI: Management of
sexual dysfunction in breast cancer survivors: A systematic review.
Womens Midlife Health. 1(9)2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Vizza R, Capomolla EM, Tosetto L, Corrado
G, Bruno V, Chiofalo B, Di Lisa FS, Filomeno L, Pizzuti L, Krasniqi
E, et al: Sexual dysfunctions in breast cancer patients: Evidence
in context. Sex Med Rev. 11:179–195. 2023.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Gordon C, Gonzales S and Krychman ML:
Rethinking the techno vagina: A case series of patient
complications following vaginal laser treatment for atrophy.
Menopause. 26:423–427. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ahluwalia J, Avram MM and Ortiz AE: Lasers
and energy-based devices marketed for vaginal rejuvenation: A
cross-sectional analysis of the MAUDE database. Lasers Surg Med.
51:671–677. 2019.PubMed/NCBI View Article : Google Scholar
|