Introduction
Sagittal split ramus osteotomy (SSRO) is a widely
used orthognathic surgery, and complications such as accidental
intraoperative fracture, nerve damage, and heavy intraoperative
bleeding can be encountered (1,2).
Among the complications of SSRO, pseudoaneurysms are rarely
reported. To the best of our knowledge, pseudoaneurysms have been
reported in only eight cases, including our own experience
(3-7).
Pseudoaneurysms are rare vascular lesions formed by
damage to the arterial wall that occurs after a trauma or
postoperatively, causing difficult-to-control bleeding (3). The injured vessels in the previously
seven cases were the facial, maxillary, and inferior alveolar
arteries. Pseudoaneurysms are at risk of rupturing and, if not
treated appropriately, may result in neurological damage or death.
Therefore, pseudoaneurysms should be treated in all cases. In our
case, angiography was performed to confirm the lesion site,
endovascular treatment was successful and produced good results. If
a pseudoaneurysm is superficial, surgical treatment is possible.
However, when an aneurysm is deeply located, as in our case,
endovascular treatment which we performed for this patient, is
indicated.
Here, we report a rare case of a female patient with
a pseudoaneurysm arising from the superficial temporal artery
(STA), as a postoperative complication of SSRO, for whom a timely
diagnosis was made using angiography, and endovascular treatment
with a discussion of the literature.
Case report
A 22-year-old healthy, 150 cm female, weighing 45 kg
(body mass index, 20 kg/m2), with a history of
preoperative orthodontic treatment was referred to our department
for improvement of her gummy smile and mandibular asymmetry. Le
Fort I osteotomy and bilateral SSRO were performed under general
anesthesia. The surgery began with a Le Fort I osteotomy and
maxillary positioning using the intermediate splint described by
Ellis (8), followed by
osteosynthesis using a miniplate and monocortical screws. SSRO was
then performed in accordance with Obwegeser's original method
(9), and right-sided SSRO was
performed uneventfully. While osteotomizing the inside of the left
SSRO using an ultrasonic cutting instrument, a large amount of
suspected arterial bleeding was observed in the soft tissue of the
posterior margin of the mandibular branch. Hemostasis was
challenging; however, after using gauze compression and direct
compression with hemostatic microfibrous collagen (Aviten; Zeria
Pharmaceuticals, USA) the bleeding stopped.
After hemostasis, lateral osteotomy, bone division,
and bone union were performed with a miniplate and monocortical
screws in the planned occlusal position. After intraoperative
hemostasis, there was no significant bleeding, and the estimated
blood loss was approximately 1,600 ml.
After consulting the anesthesiologist in charge of
the patient, intraoperative transfusion of allogeneic blood was not
performed because the patient was young and had returned 800 ml of
autologous transfusion. As no bleeding was observed after
extubation and hemostasis was achieved, the patient was returned to
the oral and maxillofacial surgery ward. Immediately after
returning to the room, we observed bleeding from the left wound
site and significant swelling of the left buccal area. Bleeding was
stopped by direct compression with gauze. The patient was managed
in the intensive care unit (ICU) for airway management, and because
he continued to bleed after returning to the ICU, transfusions of
six units of red blood cells and four units of fresh frozen plasma
were administered.
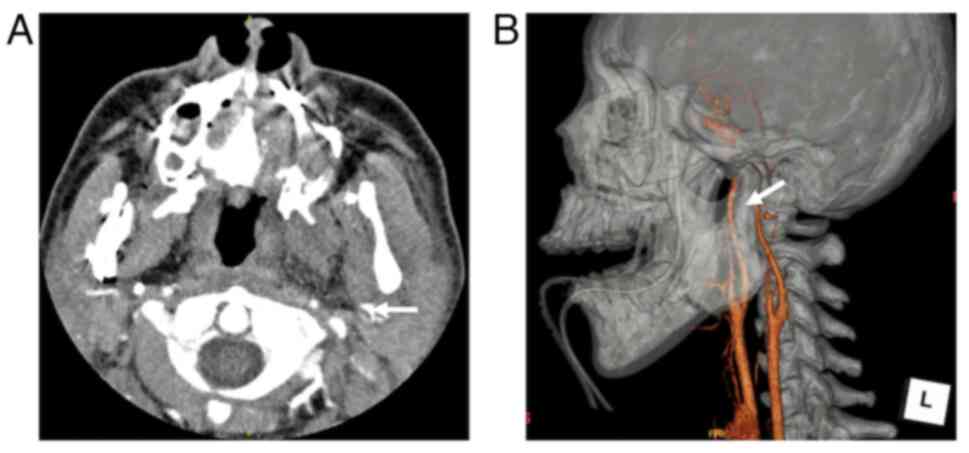
Contrast-enhanced computed tomography (CT) was
performed to confirm the vascular injury using a 320-detector row
CT scanner (Aquilion One; Canon Medical Systems Corporation,
Japan), with the following parameters: tube voltage: 120 kVp; tube
current: 150 mA; spiral pitch factor: 0.844. A pseudoaneurysm of
the left external carotid artery was observed in the left external
carotid artery (Fig. 1).
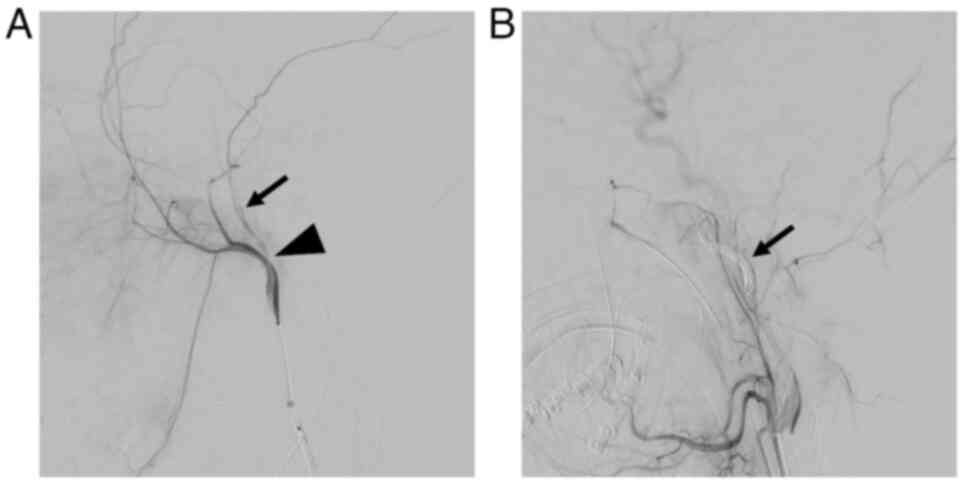
Angiography and endovascular treatment were performed on
postoperative day one using an angiography system (Azurion; Philips
Healthcare, Netherlands). The right femoral artery was punctured,
and a 5F sheath was placed. A JB2 catheter was used to select the
left external carotid artery. Angiography of the left external
carotid artery revealed stenosis at the origin of the STA and
delayed contrast of the STA. We considered this stenosis to be the
site of vascular injury because it was close to the site where a
pseudoaneurysm was observed on contrast-enhanced CT (Fig. 2A). Therefore, embolization of the
proximal portion of the STA and the area from the proximal portion
of the maxillary artery to the distal portion of the external
carotid artery, where the STA branches, was desirable. However, the
stenosis of the STA was so severe that the microwire could not be
advanced into it. Therefore, detachable coil (Target 360 soft,
Stryker, USA) and pushable coil (C-stopper coil, Piolax, Japan)
were placed from the proximal portion of the maxillary artery to
the distal portion of the external carotid artery (Fig. 2B). Angiography confirmed that the
vessel was occluded in the area where the coil was placed, and the
endovascular treatment was completed. On postoperative day three,
the patient was discharged from the ICU and returned to the oral
and maxillofacial surgery ward. Postoperative delirium was
observed; however, the patient gradually recovered and was
discharged on postoperative day 27 after rehabilitation.
Discussion
SSRO is one of the most common orthognathic surgical
procedures. Similar to any surgical procedure, various intra- and
postoperative complications can occur, including bleeding, fusion
failure, infection, and nerve damage (1,2).
Among intraoperative complications, bleeding is considered the most
serious, and among the main causes of intraoperative bleeding in
SSROs are damage to the facial, maxillary, and inferior alveolar
arteries (10,11). Injury to the retromandibular vein
can also cause bleeding that is difficult to stop (10,12).
Panula et al (2) reported
an injury to the maxillary artery during medial osteotomy of the
SSRO that resulted in 4,000 ml of bleeding per hour, and Lanigan
et al (10) reported an
increased likelihood of maxillary artery laceration during medial
osteotomy when the osteotomy was performed at a higher position
near the sigmoid notch. In this case, contrast-enhanced CT and
angiography suggested that an injury slightly above the bifurcation
of the STA and the maxillary artery had caused the pseudoaneurysm.
Vascular injury occurred despite careful and conservative osteotomy
using an ultrasonic cutting instrument rather than a rotary cutting
instrument to reduce the risk of bleeding due to entrapment of the
surrounding tissue. Therefore, to prevent vascular injury, it is
important to clearly define the operative field, carefully dissect
the periosteum to prevent perforation into the subperiosteum, and
correctly use the retractor.
Pseudoaneurysms have been reported to occur less
frequently in mandibular osteotomies than in maxillary osteotomies
(13,14). The first report of a pseudoaneurysm
in a mandibular osteotomy was by Clark et al (15) in 1987 who reported a pseudoaneurysm
following a mandibular vertical branch osteotomy. The first report
of a pseudoaneurysm in an SSRO was by Silva et al (3) in 2007, and seven cases have been
reported to date (Table I). Madani
et al (16) reported a case
of a pseudoaneurysm after SSRO; however, it was excluded because of
postoperative trauma and controversy concerning whether it was a
complication of SSRO (17). The
mean age in the seven reported cases was 24 years (five males, two
females), and all the affected vessels were right-sided. Aneurysms
were identified in the maxillary artery (one patient), inferior
alveolar artery (one patient), and facial artery (five patients),
and the most common symptoms during the first episode were
swelling, pain, and bleeding. The time from the first episode to a
diagnosis of pseudoaneurysm was frequently reported as being as
soon as the symptoms were recognized; however, there were also
reports of between 1 and 4 weeks passing prior to a diagnosis
having been made, suggesting that a pseudoaneurysm should be
suspected when swelling, edema, and pain in the cheek area are
observed with no known cause.
 | Table ICases of pseudoaneurysm after sagittal
split ramus osteotomy. |
Table I
Cases of pseudoaneurysm after sagittal
split ramus osteotomy.
| First author/s,
year | No. | Age, years | Sex | Affected side | First episode | Time from surgery to
first episode | Artery | Time from surgery to
diagnosis | Intervention | (Refs.) |
|---|
| Silva et al,
2007 | 1 | 20 | M | Right | Cheek swelling;
pulsations | N.A. | Maxillary artery | 6 weeks | Embolization with
coils | (3) |
| Precious et
al, 2012 | 2 | 32 | M | Right | Increasing swelling
and pain | 2 weeks | Facial artery | 3 weeks | Embolization with
coils | (4) |
| | 3 | 26 | M | Right | Mild discomfort | 1 week | Facial artery | 5 weeks | Embolization with
coils | |
| | 4 | 20 | M | Right | Increased edema | 1 week | Facial artery | 1 week | Embolization | |
| Jo et al,
2013 | 5 | 19 | M | Right | Pain with
swelling | N.A. | Facial artery | 3 weeks | Embolization with
coils | (5) |
| Neto et al,
2019 | 6 | 33 | F | Right | Swelling, pain | 3 days | Facial artery | 15 days | Cyanoacrylate
embolization | (6) |
| AbuKaraky et
al, 2021 | 7 | 21 | F | Right | Recurring bleeding;
throbbing pain of the throat | 18 days | Inferior alveolar
artery | 18 days | Embolization with
coils | (7) |
| Present study | 8 | 22 | F | Left | Bleeding, swelling
temporal artery | 0 days | Superficial | 1 day | Embolization with
coils | - |
AlQahtani et al (14) reported that CT angiography should
be performed, and intervention should be indicated in the presence
of epistaxis, significant facial edema, and pain after Le Fort I
osteotomy. In our case, a pseudoaneurysm of the left STA was
diagnosed using CT angiography after sudden hemorrhage and
swelling. Our patient's initial symptoms were similar to those
reported in previous studies; however, the pseudoaneurysm site was
the STA and our patient was female, which differed from those
reported in previous studies.
Unlike true aneurysms, pseudoaneurysms are formed
owing to arterial wall rupture. The outer layer of hematoma or
fibrin in the surrounding tissue of the arterial wall becomes
organic and forms a wall structure, and the lumen created through
internal melting and resorption is then connected to the original
arterial lumen (3). The period
until the occurrence of a pseudoaneurysm varies, with cases
reported as early as 4 h after a penetrating orbitofacial wound
injury (18) and as late as 8
months after injury to the common carotid artery (19). In our case, a pseudoaneurysm was
confirmed on postoperative contrast-enhanced CT, suggesting that
the formation of the pseudoaneurysm occurred within a few hours
after the artery was injured, causing rebleeding.
Endovascular treatment, as the first choice of
treatment for pseudoaneurysms, is a safe procedure to perform
(20). Kumar et al
(13) suggested that embolization
of pseudoaneurysms after orthognathic surgery is always
advantageous over surgical intervention as it spares more proximal
vessels and allows selective embolization of distal bleeding
sources. Furthermore, it has the advantage of maintaining blood
supply to the osteotomized segment through preventing aseptic
necrosis, which is particularly important after orthognathic
surgery. In our case, angiography was performed to confirm the
lesion site, followed by endovascular treatment with a good
outcome.
If an aneurysm of the external carotid artery is
superficial, surgical treatment is possible. However, when an
aneurysm is deeply located, as in our case, endovascular treatment
such as stent grafting (21) and
coil embolization, which we performed for this patient, is
indicated. Since the external carotid artery that feeds the
maxillofacial region has well-developed collateral vasculature and
embolization rarely causes soft tissue necrosis (22), preservation of blood flow to the
mother vessel through stent grafting is not always necessary.
Therefore, we opted for coil embolization to ensure hemostasis
rather than to preserve blood flow. When coil embolization of
cerebral aneurysms is performed, antithrombotic agents are
typically administered pre- and postoperatively in consideration of
the risk of cerebral infarction in clinical practice. However, in
our case, coil embolization was performed without antithrombotic
agents for the following two reasons. First, the embolization site
was at the junction of the maxillary artery and superficial
temporal artery, and the risk of cerebrovascular disease due to
thrombosis was considered to be low. Second, administration of
antithrombotic agents carries a risk of hemorrhagic complications
during the embolization procedure.
Pseudoaneurysms are at risk of rupturing and, if not
treated appropriately, may result in neurological damage or death.
Therefore, pseudoaneurysms should be treated in all cases. In our
case, endovascular treatment was successful and produced good
results. However, since endovascular treatment may not be effective
and surgical intervention may be necessary, prompt collaboration
with head and neck surgeons as well as radiologists is extremely
important.
In conclusion, we report a rare case of a female
patient with a pseudoaneurysm, as a postoperative complication of
SSRO in the STA, for whom a timely diagnosis was made using
angiography. The pseudoaneurysm was treated with therapeutic
embolization.
Acknowledgements
The authors would like to thank Dr Chikashi Takeda
and Dr Gento Yasuhara (Department of Anesthesia, Kyoto University
Hospital, Kyoto, Japan) who contributed to patient treatment and
care.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TK and YO acquired the clinical data of the patient,
performed the literature review, and edited the manuscript. TK and
TY contributed substantially to the study concept and design. KN,
TW, SY and SF acquired data and provided clinical advice. TK and YO
revised the manuscript. TK had a major role in writing the
manuscript. TK, TY and YO confirm the authenticity of all the raw
data. All authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this case report and accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ferri J, Druelle C, Schlund M, Bricout N
and Nicot R: Complications in orthognathic surgery: A retrospective
study of 5025 cases. Int Orthod. 17:789–798. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Panula K, Finne K and Oikarinen K:
Incidence of complications and problems related to orthognathic
surgery: A review of 655 patients. J Oral Maxillofac Surg.
59:1128–1137. 2001.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Silva AC, O'Ryan F, Beckley ML, Young HY
and Poor D: Pseudoaneurysm of a branch of the maxillary artery
following mandibular sagittal split ramus osteotomy: Case report
and review of the literature. J Oral Maxillofac Surg. 65:1807–1816.
2007.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Precious DS, Powell JE, Tuzuner AM,
Schmidt M, Doucet JC and Vandorpe R: False aneurysms after sagittal
split ramus osteotomies. J Oral Maxillofac Surg. 70:e58–e65.
2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Jo HW, Kim YS, Kang DH, Lee SH and Kwon
TG: Pseudoaneurysm of the facial artery occurred after mandibular
sagittal split ramus osteotomy. Oral Maxillofac Surg. 17:151–154.
2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Neto TJL, Maranhão CAA and Neto PJO:
Pseudoaneurysm of facial artery after orthognathic surgery. J
Craniofac Surg. 30:e607–e609. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
AbuKaraky A, Al Mousa M, Samara OA and
Baqain ZH: Pseudoaneurysm in the inferior alveolar artery following
a bad split in bilateral sagittal split osteotomy. Int J Oral
Maxillofac Surg. 50:798–800. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ellis E III: Bimaxillary surgery using an
intermediate splint to position the maxilla. J Oral Maxillofac
Surg. 57:53–56. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Trauner R and Obwegeser H: The surgical
correction of mandibular prognathism and retrognathia with
consideration of genioplasty. I. Surgical procedures to correct
mandibular prognathism and reshaping of the chin. Oral Surg Oral
Med Oral Pathol. 10:677–689. 1957.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lanigan DT, Hey J and West RA: Hemorrhage
following mandibular osteotomies: A report of 21 cases. J Oral
Maxillofac Surg. 49:713–724. 1991.PubMed/NCBI View Article : Google Scholar
|
|
11
|
MacIntosh RB: Experience with the sagittal
osteotomy of the mandibular ramus: A 13-year review. J Maxillofac
Surg. 9:151–165. 1981.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Behrman SJ: Complications of sagittal
osteotomy of the mandibular ramus. J Oral Surg. 30:554–561.
1972.PubMed/NCBI
|
|
13
|
Kumar A, Kaur A, Singh M, Rattan V and Rai
S: ‘Signs and symptoms tell all’-pseudoaneurysm as a cause of
postoperative bleeding after orthognathic surgery-report of a case
and a systematic review of literature. J Maxillofac Oral Surg.
20:345–355. 2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
AlQahtani FA, Kuriadom ST, Bishawi K and
AlAssiri N: Pseudoaneurysms and orthognathic surgery: A systematic
review and a proposed algorithm of treatment. J Craniofac Surg.
34:1031–1035. 2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Clark R, Lew D, Giyanani VL and Gerlock A:
False aneurysm complicating orthognathic surgery. J Oral Maxillofac
Surg. 45:57–59. 1987.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Madani M, Veznedaroglu E, Pazoki A, Danesh
J and Matson SL: Pseudoaneurysm of the facial artery as a late
complication of bilateral sagittal split osteotomy and facial
trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
110:579–584. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Dediol E: Pseudoaneurysm of the facial
artery as a complication of the sagittal split osteotomy. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod. 110:683–684.
2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ferry DJ Jr and Kempe LG: False aneurysm
secondary to penetration of the brain through orbitofacial wounds.
Report of two cases. J Neurosurg. 36:503–506. 1972.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Beale PJ: Late development of a false
aneurysm of the facial region. J Oral Surg. 58:76–78.
1971.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fernández-Prieto A, García-Raya P,
Burgueño M, Muñoz-Caro J and Frutos R: Endovascular treatment of a
pseudoaneurysm of the descending palatine artery after orthognathic
surgery: Technical note. Int J Oral Maxillofac Surg. 34:321–323.
2005.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Nadig S, Barnwell S and Wax MK:
Pseudoaneurysm of the external carotid artery-review of literature.
Head Neck. 31:136–139. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Guss J, Cohen MA and Mirza N: Hard palate
necrosis after bilateral internal maxillary artery embolization for
epistaxis. Laryngoscope. 117:1683–1684. 2007.PubMed/NCBI View Article : Google Scholar
|