Introduction
Epibulbar dermoid is a common congenital tumor
located on normal tissues (1). It
contains tissues from various layers of the eye and skin, such as
follicles, sweat glands and sebaceous glands, covered by epithelium
(1). Most cases of epibulbar
dermoid occur at the inferior-temporal part of the limbus.
Occasionally, the lesions can involve the anterior chamber, lens,
iris and ciliary body (2). If
limbal epibulbar dermoid is combined with other diseases, such as
auricle deformity, maxillofacial dysostosis or vertebral
abnormality, it is known as Goldenhar's syndrome.
Epibulbar dermoid can cause astigmatism-related
amblyopia, ocular surface disturbances as well as cosmetic concern
in children (3). Management of
epibulbar dermoid should consider age, tumor size, tumor depth,
growth speed and psychological issues (1-4).
Various surgical techniques were reported for the treatment of
epibulbar dermoid, including simple excision for small dermoid
(Grade I, <50 µm in thickness and <1 mm in diameter) and
lamellar keratoplasty with corneoscleral graft for moderate dermoid
(Grade II, <100 µm in thickness and <1 mm in diameter)
(2,4,5). In
other previous studies, new techniques were developed, including
excision, grafts (6,7), amniotic membrane transplantation
(8,9), mitomycin C (10) and fibrin glue-assisted lenticule
(11). The aforementioned
approaches are considered more convenient in terms of surgical
complexity and associated complications. The present study reports
on the case of a superficial limbal dermoid surgically treated
without suture using a new technique of lamellar keratoplasty with
an allogenic lenticule obtained by small incision lenticule
extraction (SMILE). A novel surgical approach is thus introduced
for treating dermoid cysts, utilizing post-operative SMILE
lenticules without sutures, achieving satisfactory surgical
outcomes.
Case report
Case
All procedures performed in the current study were
approved by the Ethics Committee of Shanxi Aier Eye Hospital
(Taiyuan, China; approval no. 2020QYSXAEYK01). A 20-year-old male
patient had a whitish mass in his right eye since birth, which
progressively grew. The patient was admitted into the Shanxi Aier
Eye Hospital in July 2020 and the surgery was performed the next
day. Systemic examination showed that the patient had an auricular
anomaly, a history of mandibular and facial plastic surgery
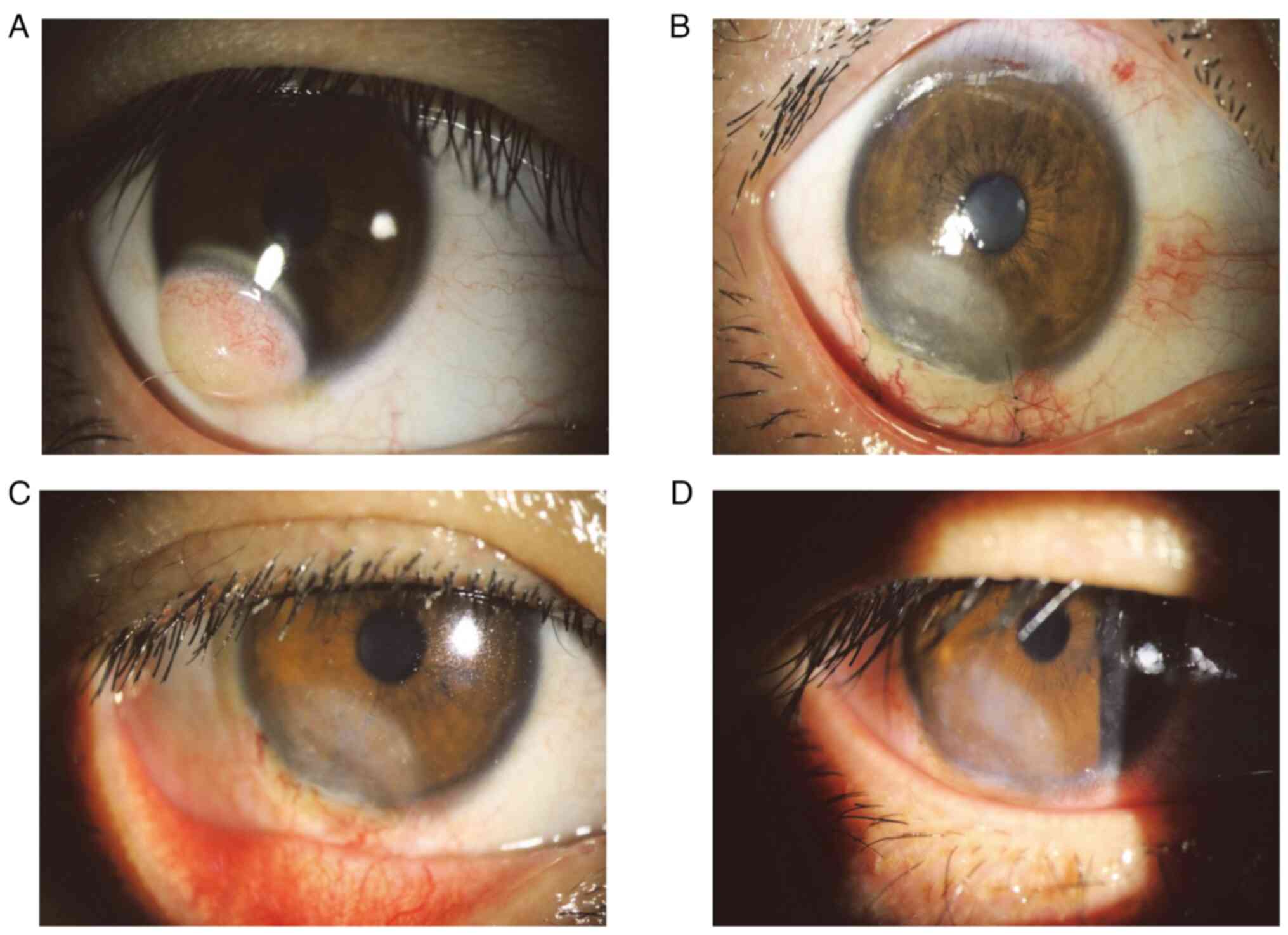
(details unknown) and vertebral anomalies (Fig. 1). Ophthalmic examination revealed a
solid, white and ovoid mass located at 6 to 8 o'clock below
inferotemporal limbus of the right eye, and the lesion was ~7 mm in
diameter and 200 µm in depth. The visual acuity test indicated that
the best corrected visual acuity (BCVA) was 20/40 with astigmatic
error -2.00 D ax 50. A mild limitation of movement was observed for
the right eye when looking at the inferotemporal direction.
Anterior segment optical coherence tomography (Visante OCT; Carl
Zeiss Meditec, Inc.) revealed superficial corneal involvement by
the tumor but no signs of anterior chamber invasion. Due to
increasing astigmatic error and cosmetic concerns, the decision to
perform surgical excision was made. The surgical procedure and
possible postoperative complications were known to the patient and
his legal representatives.
Surgical technique
Local anesthesia was achieved by subconjunctival
injection of 0.3 ml lidocaine into the inferior fornix. The border
of the limbal dermoid was marked using a 7 mm in diameter trephine
and lamellar dissection of the corneal limbal dermoid was performed
using a surgical knife. Following the complete excision of the
dermoid, residual dermoid fibers were scraped from the corneal
stroma using a 57 straight beaver blade knife. Subsequently,
redundant liquid on the corneal stromal bed was absorbed with a
cotton pad.
A fresh donor lenticule was obtained from a
refractive patient who underwent SMILE. This refractive patient was
negative for anti-HIV-1 and anti-HIV-2, as well as for hepatitis B
and C viruses. The lenticule was 6.5 mm in diameter, its cap
thickness was 129 µm and its periphery thickness was 20 µm. The
lenticule was lied within the margins of the defects and the
scleral part of the lenticule was carefully trimmed by scissors to
keep the lenticule within the limbus. A 3x3 mm conjunctival flap
was dissociated from the superior limbus, put on the defect area of
the limbus and sclera, and then sutured with adjacent conjunctiva
using a 10-0 nylon suture (Alcon, Inc.). Finally, no obvious
bubbles or liquids were found at the interface between lenticule
and stroma bed. A bandage contact lens (Bausch & Lomb, Inc.)
was applied to the eye, and tobramycin and dexamethasone eye
ointments (S.A. Alcon-Couvreur N.V.) were applied in the
conjunctival sac. Then, the surgery was completed.
Postoperative medication and
results
After surgery, the patient was given topical
loteprednol etabonate ophthalmic suspension (Bausch & Lomb,
Inc.) four times a day, deproteinized calf blood extract eye drop
(Qixin Pharmaceutical Co., Ltd.) four times a day, and levofloxacin
eye drop (Santen Pharmaceutical Co., Ltd.) four times a day.
On the first day after the operation, the patient
reported somewhat tearing and pain. Slit-lamp examination showed
mild conjunctival hyperemia, and the graft exhibited moderate edema
(Grade 2, iris detail could not be recognized). BCVA was 30/40
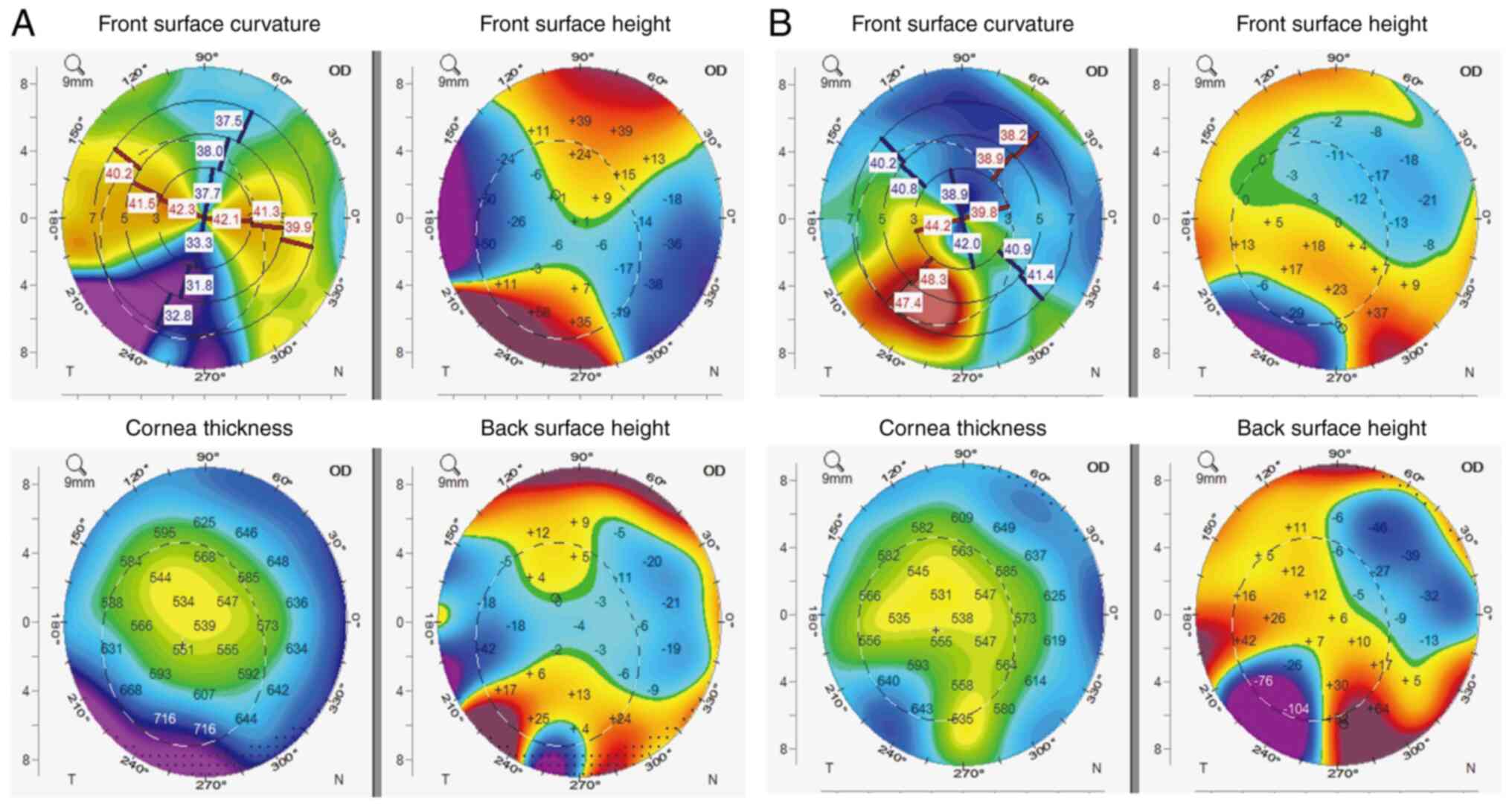
(refractive correction, -2.75 Dcy ax 50). Corneal topography
(OCULUS Pentacam®; OCULUS Optikgeräte GmbH) showed that
the thickness of the lesion area was higher than that of the
adjacent cornea and corneal curvature and refractive power of the
lesion area was less than that of the adjacent cornea.
At 1 week after the operation, the patient reported
no discomfort and conjunctival sutures were removed. Slit-lamp
examination showed mild conjunctival hyperemia around the limbus of
the graft. In addition, the graft showed mild edema (Grade 1, iris
detail could be recognized) and corneal re-epithelization overlay
the graft. BCVA was 30/40 (refractive correction, -2.50 Dcy ax 50).
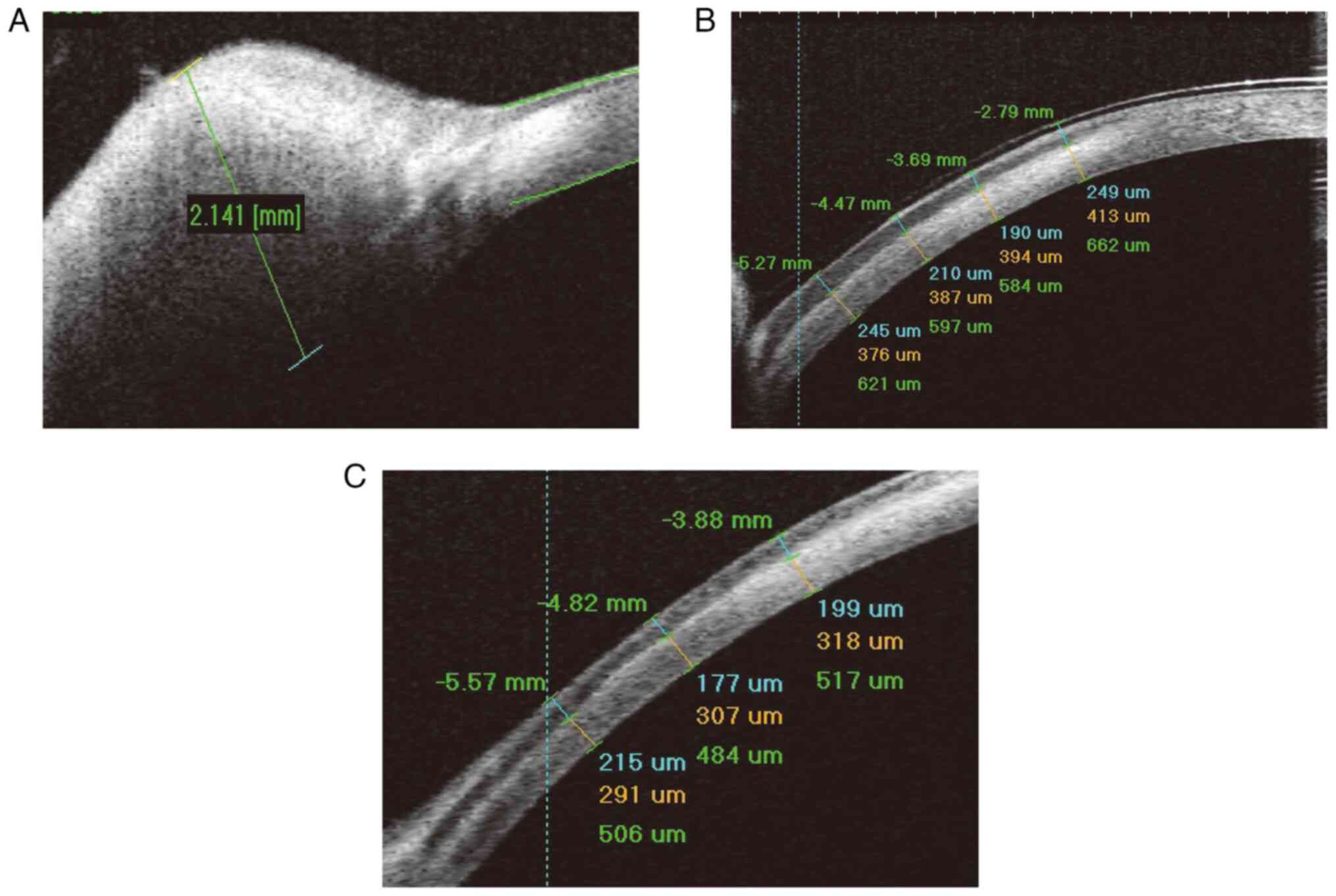
Anterior segment optical coherence tomography (AS-OCT) showed that
the graft was tight and closed on the stroma bed. In addition, the
thickness of the graft was from 238-279 µm and the total cornea
thickness was from 590-636 µm (Fig.
2).
At 1 month after the operation, BCVA was 30/40
(refractive correction, -2.50 Dcy ax 50). AS-OCT showed that the
thickness of the graft was from 95-192 µm and the total cornea
thickness was from 483-536 µm (Fig.
2). Corneal topography showed that the thickness of lesion area
was similar to that of the adjacent cornea, and corneal curvature
and refractive power of the lesion area were higher than that of
the adjacent cornea (Fig. 3).
At 3 months after operation, the patient was
satisfied with the cosmetic outcome and no sign of corneal
neovascularization, graft rejection or pseudo-pterygium formation
was observed. The astigmatic error remained at 2.50D.
Discussion
Various techniques can be used to remove limbal
dermoid, including simple lamellar dissection, reconstruction with
lamellar corneoscleral graft, anterior corneal button from DSAEK
donor tissue, pericardial patch graft and multilayered amniotic
membrane graft (2,5-9).
Additionally, recent advances in the use of fibrin glue in
conjunction with amniotic membrane transplantation have
significantly enhanced the application of tissue adhesives in
ocular surface reconstruction (9).
Simple excision and/or keratectomy of smaller lesions were shown to
lead to pseudo-pterygium and conjunctival symblepharon formation
due to surface tear fluid irregularities (12). At present, using dried preserved
donated cornea for lamellar keratoplasty is the mostly used
surgical procedure in China, due to a great lack of donation of
cornea (13-15).
Using donated intrastromal SMILE-extracted lenticule has been
proven an alternative because it is fresh and easy to obtain
(16). The present case report
discussed a novel technique that had not been performed before.
The surgical suture was the worldwide most used
method to secure grafts. Suture-related complications include
astigmatism, corneal neovascularization and scar formation.
Postoperative persistent eye abrasion, foreign body sensation and
conjunctival hyperemia are also common. On the other hand, suture
removal is another burden for children and doctors. The advantage
of sutureless lamellar keratoplasty is reported to minimize these
issues. The use of fibrin-glue with amniotic membrane or
SMILE-extracted lenticule have been reported in recent years
(9,11,17).
Notably, the present authors achieved similar results without using
fibrin-glue to fix graft. The reason may be that the interlayer
liquid was removed as much as possible during the operation and
this procedure generated hydrostatic pressure to adsorb the graft
on the stroma bed. Therefore, this technique is suitable for
clinical applications in areas where fibrin glue is not available
or too expensive. Moreover, the safety issue of fibrin glue cannot
be ignored (18). Fiber glue
production originates from human plasma and, due to contamination
or low virus detection sensitivity, it may cause fiber glue to
carry viruses and infect the host (18). Although the graft is fixed by a
bandage lens and the corneal epithelium covers the graft 1 week
after grafting, potential graft displacement needs to be taken
seriously, especially in the early postoperative stage. Due to the
rejection rate of LK ranging from 5-8% (19), very few cases will experience
rejection after 1 year. Early dislocation of the implant may be due
to normal blinking, squeezing, rubbing, etc., even with the
protection of a bandage lens. After 1 week, the graft is covered by
the corneal epithelium and the possibility of graft dislocation is
relatively low but it can still occur after trauma. After 1 month,
the possibility of dislocation is less due to fibrosis of the graft
and the underlying implant bed. In this case, the use of hormonal
eye drops was stopped within 3 months due to the stable condition
of the eye surface. It is a common practice of the present authors
to use hormones for 3-6 months after LK surgery. Although the graft
was close to the corneal margin in this case, the graft area was
small and relatively thin, and most rejection reactions occurred 1
week to 1 month after surgery. Most rejection reactions are
recovered through local treatment. In addition, the patient's
remote residence made follow-up inconvenient; therefore,
hormone-based medication was stopped after 3 months post-surgery to
avoid the side effects of long-term use of glucocorticoids, such as
glaucoma and cataracts.
Amniotic membrane transplantation also shows an
excellent surgical outcome in the treatment of limbal dermoid
(8,9). However, unpredictable corneal scar or
thinning after the dissolution of the amniotic membrane can enlarge
the structural difference between the cornea in the lesion area and
the normal cornea (20). The
present case report described the changes in corneal thickness and
corneal topography at different time points after the operation.
These results will help surgeons to predict the outcomes of
surgeries.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YH contributed to the design of the study. BZ
analyzed the data. TW performed data collection. XG designed the
operation and prepared the manuscript. BZ and TW confirm the
authenticity of all the raw data. All the authors read and approved
the final version of the manuscript.
Ethics approval and consent to
participate
All procedures performed in the current study were
approved by the Ethics Committee of Shanxi Aier Eye Hospital
(approval no. 2020QYSXAEYK01; Taiyuan, China).
Patient consent for publication
Written informed consent for the publication of any
associated data and accompanying images was obtained from the
patient and his father.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Robb RM: Astigmatic refractive errors
associated with limbal dermoids. J Pediatr Ophthalmol Strabismus.
33:241–243. 1996.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Scott JA and Tan DT: Therapeutic lamellar
keratoplasty for limbal dermoids. Ophthalmology. 108:1858–1867.
2001.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Shen YD, Chen WL, Wang IJ, Hou YC and Hu
FR: Full-thickness central corneal grafts in lamellar
keratoscleroplasty to treat limbal dermoids. Ophthalmology.
112(1955)2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Watts P, Michaeli-Cohen A, Abdolell M and
Rootman D: Outcome of lamellar keratoplasty for limbal dermoids in
children. J AAPOS. 6:209–215. 2002.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Pirouzian A: Management of pediatric
corneal limbal dermoids. Clin Ophthalmol. 7:607–614.
2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lazzaro DR and Coe R: Repair of limbal
dermoid with excision and placement of a circumlimbal pericardial
graft. Eye Contact Lens. 36:228–229. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wu KI, Chu HS, Pai AS, Hou YC, Lin SY,
Chen WL and Hu FR: Surgical management of limbal dermoids using
anterior corneal buttons from descemet stripping automated
endothelial keratoplasty donor tissue as patch grafts. Cornea.
36:64–67. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Pirouzian A, Holz H, Merrill K, Sudesh R
and Karlen K: Surgical management of pediatric limbal dermoids with
sutureless amniotic membrane transplantation and augmentation. J
Pediatr Ophthalmol Strabismus. 49:114–119. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Pirouzian A, Ly H, Holz H, Sudesh RS and
Chuck RS: Fibrin-glue assisted multilayered amniotic membrane
transplantation in surgical management of pediatric corneal limbal
dermoid: A novel approach. Graefes Arch Clin Exp Ophthalmol.
249:261–265. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lang SJ, Böhringer D and Reinhard T:
Surgical management of corneal limbal dermoids: Retrospective study
of different techniques and use of Mitomycin C. Eye (Lond).
28:857–862. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Jacob S, Narasimhan S, Agarwal A, Agarwal
A and Ai S: Combined interface tattooing and fibrin glue-assisted
sutureless corneal resurfacing with donor lenticule obtained from
small-incision lenticule extraction for limbal dermoid. J Cataract
Refract Surg. 43:1371–1375. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Panda A, Ghose S, Khokhar S and Das H:
Surgical outcomes of epibulbar dermoids. J Pediatr Ophthalmol
Strabismus. 39:20–25. 2002.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Luo S, Xu J, Shao T and Qu X: Refractive
characteristics and related factors of amblyopia after lamellar
keratoscleroplasty in children with limbal dermoids. J Clin Med.
11(4176)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zhong J, Deng Y, Zhang P, Li S, Huang H,
Wang B, Zhang H, Peng L, Yang R, Xu J and Yuan J: New grading
system for limbal dermoid: A retrospective analysis of 261 cases
over a 10-year period. Cornea. 37:66–71. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hong J, Shi W, Liu Z, Pineda R, Cui X, Sun
X and Xu J: Limitations keratoplasty in of China: A survey
analysis. PLoS One. 10(e0132268)2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Pant OP, Hao JL, Zhou DD, Wang F, Zhang BJ
and Lu CW: Lamellar keratoplasty using femtosecond laser
intrastromal lenticule for limbal dermoid: Case report and
literature review. J Int Med Res. 46:4753–4759. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhou AX and Ambati BK: Sutureless lamellar
corneoscleral patch graft with fibrin sealant for limbal dermoid
removal. J Pediatr Ophthalmol Strabismus. 53 Online:e22–e25.
2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hino M, Ishiko O, Honda KI, Yamane T, Ohta
K, Takubo T and Tatsumi N: Transmission of symptomatic parvovirus
B19 infection by fibrin sealant used during surgery. Br J Haematol.
108:194–195. 2000.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Watson SL, Ramsay A, Dart JK, Bunce C and
Craig E: Comparison of deep lamellar keratoplasty and penetrating
keratoplasty in patients with keratoconus. Ophthalmology.
111:1676–1682. 2004.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Prabhasawat P, Tesavibul N and
Komolsuradej W: Single and multilayer amniotic membrane
transplantation for persistent corneal epithelial defect with and
without stromal thinning and perforation. Br J Ophthalmol.
85:1455–1463. 2001.PubMed/NCBI View Article : Google Scholar
|