Introduction
Upper gastrointestinal bleeding (UGIB) is a frequent
medical emergency (1) that may
arise from peptic ulcers, oesophageal varices, Mallory-Weiss tears
and malignancies and is associated with high mortality and
morbidity rates (2). Therefore,
early detection and prompt management are essential to improve
patient outcomes. However, predicting outcomes in patients with
acute UGIB is still challenging. Traditional prognostic markers
such as age, comorbidities and bleeding intensity are not
necessarily accurate indicators of how a patient will fare
(3). Therefore, identifying
accurate indicators of prognosis in patients with acute UGIB is
crucial.
Prognostic value of lactate levels as predictor of
outcomes in acute UGIB has drawn more attention in recent years
(4-6).
Lactate is a by-product of an anaerobic metabolism and builds up in
hypoxic tissues (7). Measuring
lactate levels is an easy, affordable and accessible test (8). Recent studies show that increased
lactate levels are associated with a number of unfavourable
outcomes, such as mortality, extended hospital stays and
requirement for ICU admission (4,6,9).
Increased lactate levels in critically ill patients have been
linked to poor outcomes in cases of sepsis, trauma and cardiac
arrest (9).
However, it is still debatable whether lactate
levels play a role in predicting outcomes in UGIB. While some
studies have found no significant correlation, others have
established a relationship between elevated lactate levels and
poorer outcomes in UGIB patients (4-6).
The main goal of the current systematic literature review was to
assess the evidence, summarize available findings on the
association of lactate levels with outcomes in acute UGIB and
evaluate whether the lactate levels can act as predictor for
adverse outcomes in patients with UGIB.
Materials and methods
Inclusion criteria. Study design
Observational studies, including cohort
(prospective/retrospective), case-control and cross-sectional
studies, were considered for inclusion. Full-text studies that met
the eligibility criteria were included, while case reports/series
and unpublished grey literature were excluded from the analysis.
The study was registered at PROSPERO; no. CRD42023406493.
Study participants
Studies performed in patients with acute UGIB who
underwent lactate tests were included.
Index test and reference standard
Studies comparing the prognostic role of lactate
levels with the real-time occurrence of adverse outcomes through
the follow-up of patients either through records or in-person were
included.
Outcomes
Mortality, need for packed red blood cell (pRBC)
transfusion, rebleeding and ICU admissions.
Search strategy
Search was conducted in multiple databases,
including PubMed Central (https://www.ncbi.nlm.nih.gov/pmc/), SCOPUS (https://www.scopus.com/search/form.uri?display=basic#basic),
EMBASE (https://www.embase.com/login),
MEDLINE (https://pubmed.ncbi.nlm.nih.gov), Google Scholar
(https://scholar.google.com) and
ScienceDirect (https://www.sciencedirect.com) using medical subject
headings (MeSH) and free-text terms with the appropriate Boolean
operators (‘AND,’ ‘OR,’ and ‘NOT’) to combine predefined search
terms. The search period ranged between January 1964 and February
2023, without any language restrictions (Appendix S1).
Study selection
The initial stage of the study selection process was
conducted independently by two researchers, who examined the
titles, keywords and abstracts of the identified studies. For the
second phase of screening, full texts of the selected studies were
retrieved by both investigators. Studies that met eligibility
criteria were ultimately included for further analysis. The
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
(PRISMA) checklist 2020 was used to report the present study
(10).
Data extraction
For data extraction, two researchers participated in
the manual data extraction procedure using a predefined
semi-structured data collection form. A third researcher was
involved in resolving any conflict arising out of data extraction
process.
Risk of bias assessment
Quality of the included studies was assessed by two
investigators using the Newcastle Ottawa Scale for observational
studies (11). The scale
encompasses selection, comparability and outcome domains. Based on
the responses, each study was categorized as having good/poor
quality.
Statistical analysis
The pooled effect was calculated as standardized
mean difference (SMD)/odds ratio (OR) with 95% confidence interval
(CI) depending on the type of outcome. Using the inverse variance
technique, a random effects model was applied (12). Predictive accuracy was evaluated by
calculating the combined values of sensitivity, specificity,
likelihood ratios for positive and negative outcomes as well as the
overall diagnostic OR for lactate levels. Area under the Receiver
Operator Characteristic (AUROC ) was used to produce Summary
Receiver Operator Characteristic curves (SROC) (13).
Heterogeneity was measured by I2
statistics and the χ2 of heterogeneity. The effect of a
single study on the pooled estimates was determined by sensitivity
analysis. Publication bias assessment and meta-regression could not
be performed as none of the outcomes had at ≥10 studies. STATA
version 14.2 (StataCorp LLC) was used for the analysis.
Results
Search results
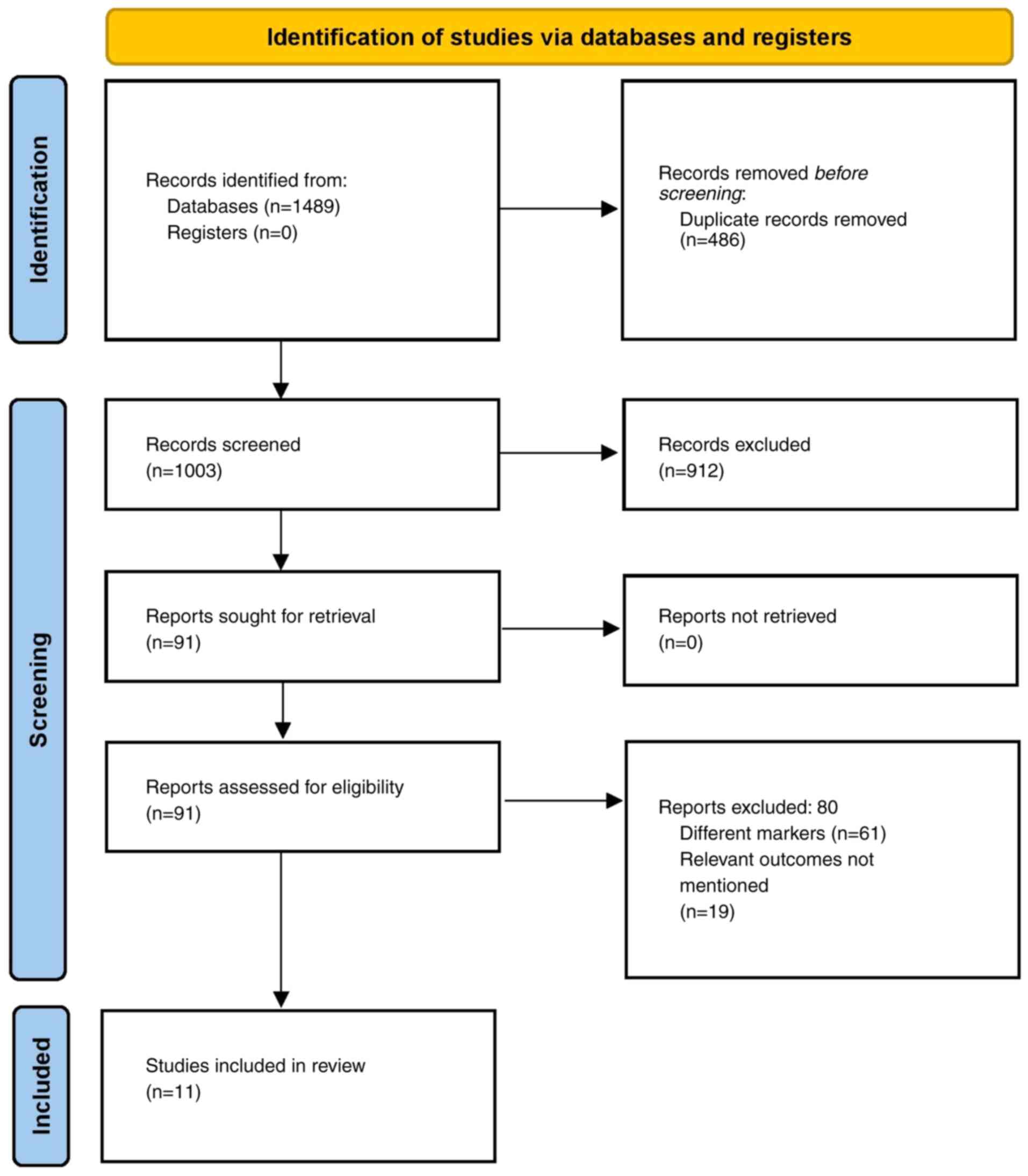
A total of 1,489 citations were identified across
the databases. Following duplicates removal, 91 full-text articles
were retrieved and underwent secondary screening. Finally, a total
of 11 studies that satisfied the eligibility criteria were included
(Fig. 1) (4-6,14-21).
Characteristics of the included
studies
The majority of the studies were conducted in the
United States of America (four studies) and Korea (three studies).
Most studies were retrospective (six out of 11 studies). Sample
size in the included studies varied between 104 and 1,644. The mean
age of the participants varied from 55.4-72.9 years. The cut-off
for the lactate levels to predict adverse outcomes ranged from 1.85
to 4.3 mmol/l. Of the studies, >50% (six out of 11 studies) had
a higher risk of bias (Table
I).
 | Table ICharacteristics of the included
studies. |
Table I
Characteristics of the included
studies.
| First author,
year | Study design | Country | Inclusion
criteria | Sample size | Cut-off for lactate
levels | Mean age, years | Sex distribution,
male:female | Outcomes
reported | Risk of bias | (Refs.) |
|---|
| Berger et al,
2019 | Retrospective | USA | Consecutive patients
presenting to the ED of a tertiary care medical center between
January 2014 and December 2015 with a charted diagnosis of acute
gastrointestinal bleeding | 366 | 2.75 | 70.9 | 204:162 | Mortality | High | (17) |
| El-Kersh et
al, 2015 | Retrospective
cohort | USA | Consecutive patients
with acute UGIB admitted to university hospital ICU between 2010
and 2013 | 133 | 2.1 | 55.4 | 86:47 | Mortality | High | (19) |
| Gulen et al,
2019 | Prospective | Turkey | Patients with UGIB
who were admitted to the emergency department between 1 June 2018
and 31 May 2019 | 139 | 2.32 | 63.34 | 100:39 | Mortality, need for
packed red blood cell transfusion | Low | (15) |
| Kim et al,
2022 | Retrospective | Korea | Patients aged ≥18
years who visited the ED, complaining of any GI bleeding symptoms
(melena, hematemesis and/or hematochezia), serum lactate levels
measured initially in the ED and then measured for follow-up after
3 h. | 104 | 3.4 | 64.6 | 74:30 | Mortality | High | (6) |
| Ko et al,
2015 | Retrospective | Korea | Consecutive adult
(>18 years) patients with UGIB who were hemodynamically stable
(defined as an SBP of ≥90 mm Hg) at presentation in the ED of
Hospital of Chengdu University of Traditional Chinese Medicine
(Chengdu, Sichuan) between January 2010 and December 2014 | 1,003 | 2.5 | 61.8 | 732:271 | Mortality, ICU
admission, need for packed red blood cell transfusion | High | (18) |
| Lee et al,
2017 | Retrospective | Korea | Adult patients
(>18 years old) with UGIB who underwent endoscopic hemostasis at
the Samsung Medical Center between January 2006 and August
2016 | 114 | NR | 65.1 | 86:28 | Mortality, ICU
admission, Rebleeding | Low | (16) |
| Shah et al,
2014 | Retrospective
cohort | USA | Medical records of
patients having acute gastrointestinal bleeding between January 1,
2004 and December 31, 2009 | 1,644 | 4 | 56.8 | 869:775 | Mortality | Low | (20) |
| Shrestha et
al, 2018 | Retrospective | USA | Patients ≥18 years
old presenting to emergency with acute GIB between January 2014 and
December 2014 | 468 | 2 | 59.5 | 250:218 | ICU admission, need
for packed red blood cell transfusion | High | (14) |
| Stokbro et
al, 2017 | Retrospective
cohort | Denmark | Patients admitted
with UGIB to Odense University Hospital in the one-year period
between March 1 2014 and February 28 2015 | 331 | 1.85 | 72.9 | 183:148 | Mortality,
Rebleeding | Low | (4) |
| Strzalka et
al, 2022 | Prospective | Poland | Adult patients with
symptoms of acute UGIB admitted to hospital between 1st January
2018 and 31st December 2019 | 221 | 4.3 | 63.5 | 151:70 | Mortality, ICU
admission, rebleeding | Low | (21) |
| Wada et al,
2016 | Retrospective | Japan | Patients who were
admitted to hospital with a primary diagnosis of UGIB | 154 | NR | 60 | 115:39 | Rebleeding | High | (5) |
Mortality
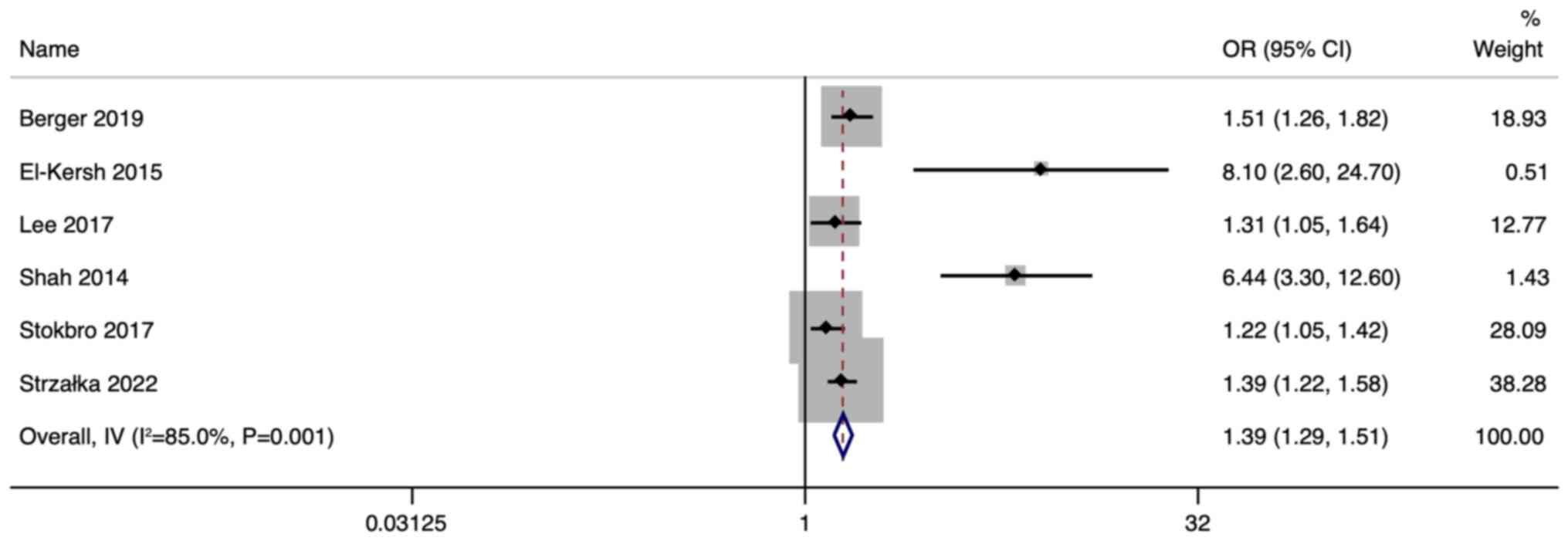
A total of nine studies reported the utility of
lactate levels for prediction of mortality in patients with acute
UGIB. Of them, six studies reported the outcomes in terms of OR,
with the pooled OR of 1.39 (95% CI: 1.29-1.51; I2=85%),
indicating that in patients with acute UGIB higher lactate level
are significantly associated with increased mortality compared with
normal lactate levels (P<0.001; Fig. 2).
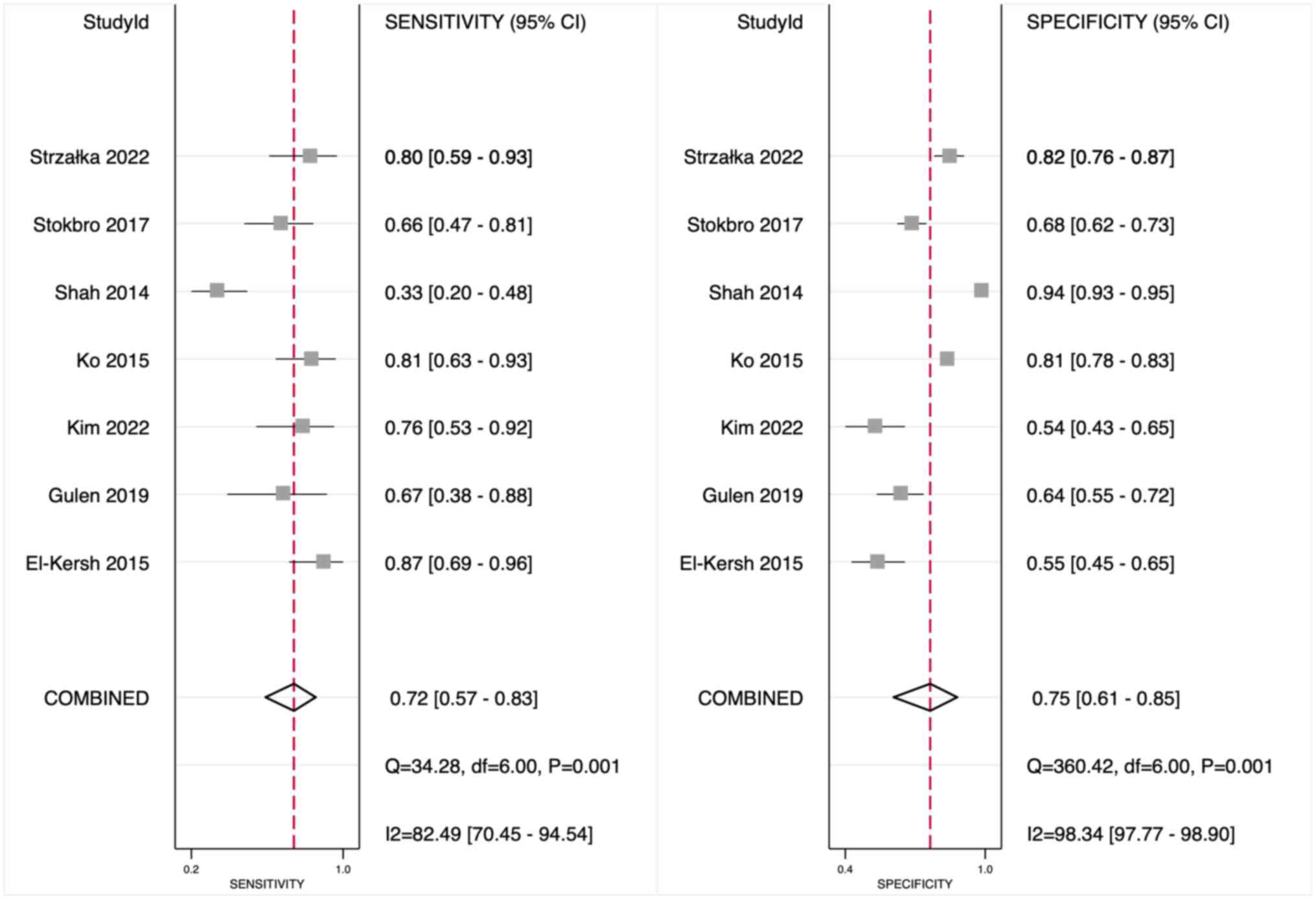
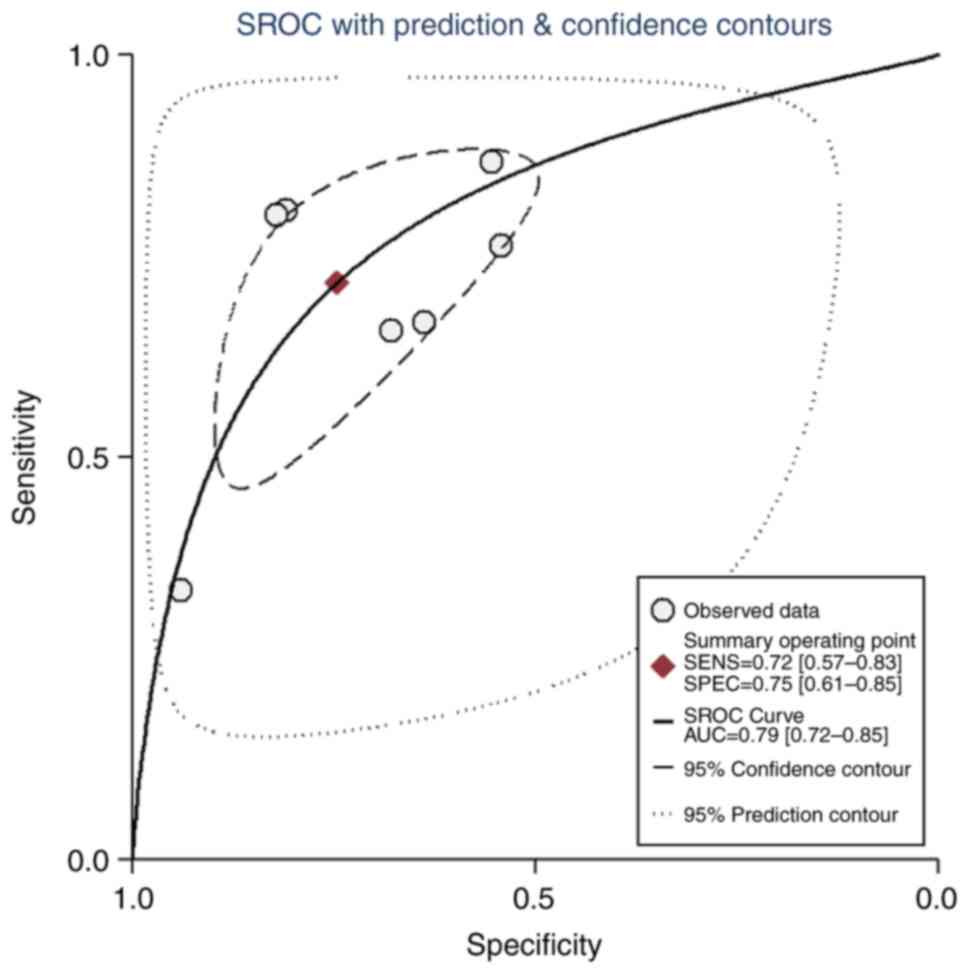
The predictive accuracy of lactate for mortality in
patients with acute UGIB is shown in Fig. 3. The diagnostic OR was 7 (95% CI:
5-12), the sensitivity and specificity were 72% (95% CI: 57-83%)
and 75% (95% CI: 61-85%), respectively and the positive and
negative likelihood ratios were 2.8 (95% CI: 2-4.1) and 0.38,
respectively (95% CI: 0.27-0.54). The AUROC was 0.79 (95% CI:
0.72-0.85) (Fig. 4).
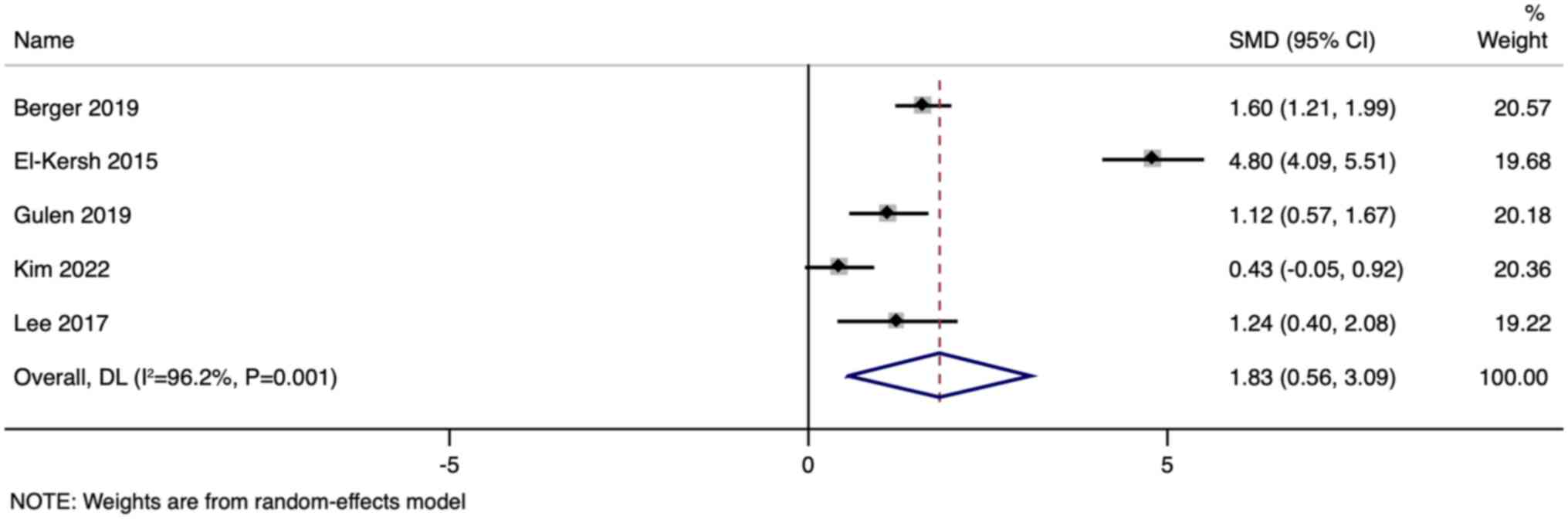
Differences in the mean values of lactate in
survivors and non-survivors were reported in five studies. The
pooled SMD was 1.83 (95% CI: 0.56-3.09; I2=96.2%),
indicating that the non-survivors had significantly higher values
of lactate when compared with survivors (P<0.001; Fig. 5).
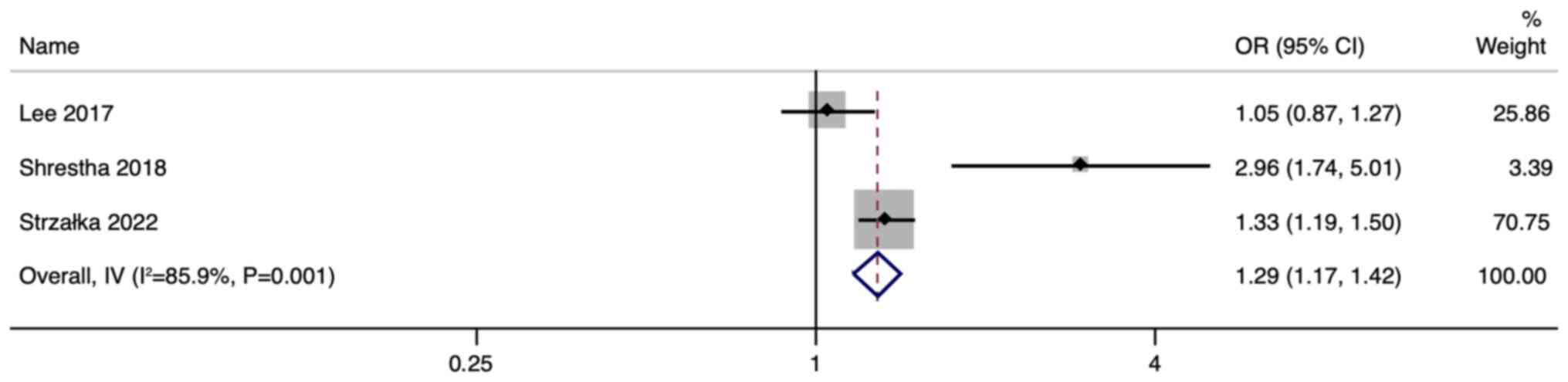
ICU admission
A total of three studies reported the value of
lactate levels for prediction of ICU admission in patients with
acute UGIB with the pooled OR of 1.29 (95% CI: 1.17-1.42;
I2=85.9%), indicating that higher lactate levels
associated with increased odds of acute UGIB patients being
admitted to ICU compared with normal lactate levels (P<0.001;
Fig. 6). Small number of studies,
reporting this outcome did not allow to assess the predictive
accuracy and mean values.
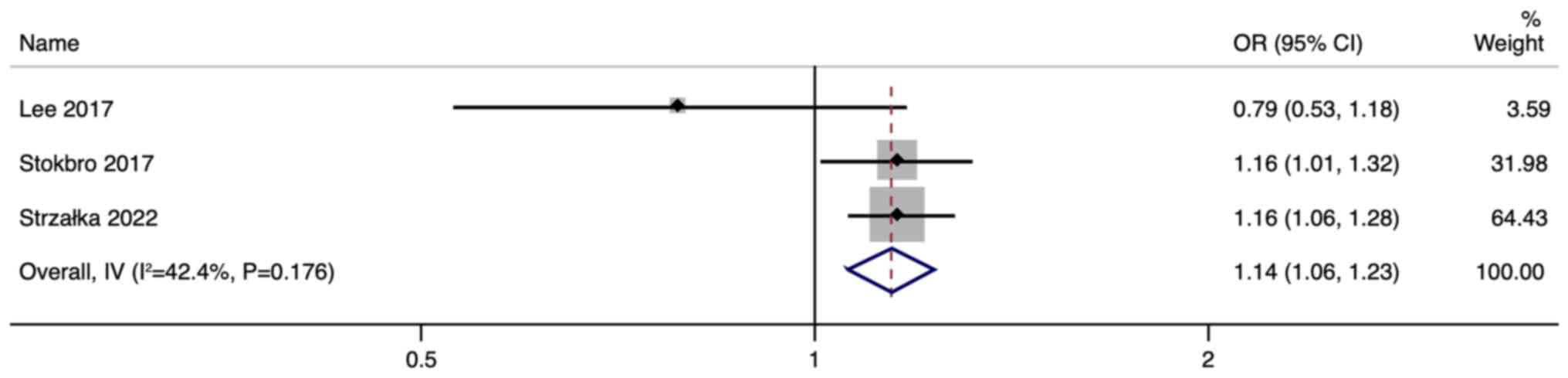
Rebleeding
A total of four studies reported the utility of
lactate levels for prediction of rebleeding in patients with acute
UGIB. Of them, three studies reported the outcomes in terms of OR.
The pooled OR was 1.14 (95% CI: 1.06-1.23; I2=42.4%)
indicating that higher lactate levels are associated with
significantly higher (P<0.001) odds of rebleeding compared with
normal lactate levels (Fig. 7).
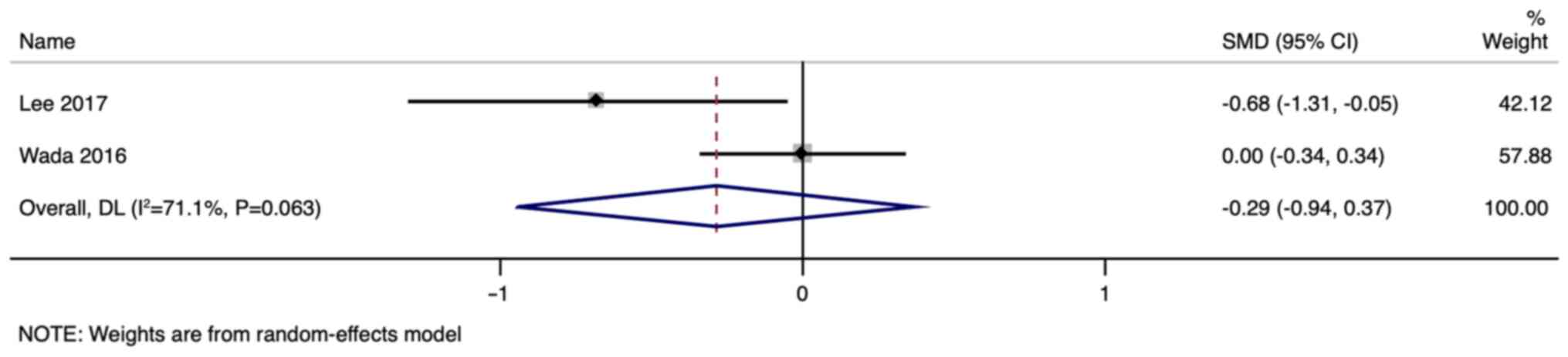
The difference in mean values of lactate between acute UGIB
patients with and without rebleeding were reported in two studies.
Pooled SMD was -0.29 (95% CI: -0.94 to 0.37; I2=71.1%;
p=0.39; Fig. 8).
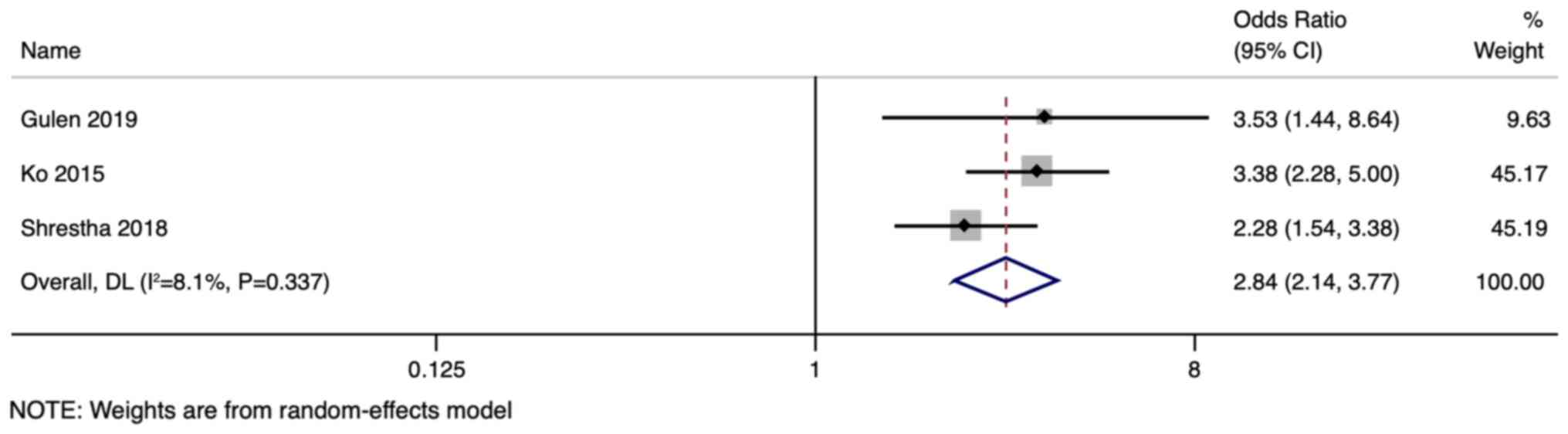
Need for pRBC transfusion
A total of three studies reported the prognostic
value of lactate levels for prediction of the need for pRBC
transfusion, with the pooled OR of 2.84 (95% CI: 2.14-3.77;
I2=8.1%). This indicated that in patients with acute
UGIB, higher lactate levels are associated with higher odds of
requiring pRBC transfusion compared with normal lactate levels
(P<0.001; Fig. 9). The
predictive accuracy and mean values are not reported due to the
small number of studies.
Additional analysis
Sensitivity analysis did not show any difference for
any of the above outcomes, indicating that there were no
single-study effects.
Discussion
The present study aimed to investigate whether the
lactate may act as a predictor for adverse clinical outcomes in
patients with UGIB. The results suggested that the lactate level is
a moderately accurate early marker for predicting most adverse
outcomes such as mortality, rebleeding, ICU admission and a need
for pRBC transfusion. Although, no previous similar reviews were
conducted, these findings were consistent across almost all the
included studies in the present review (4-6,14-21).
Presently, commonly used prognostic markers in patients with acute
UGIB include shock index (22),
hemodynamic parameters (23),
Glasgow-Blatchford score (24) and
Rockall score (24). However,
these markers have limitations, such as low sensitivity and
specificity, or a need for complex calculations. By contrast,
lactate levels have been found to be more accurate than other
markers such as base deficit or pH, as they rise earlier and more
consistently in response to hypoperfusion and provide a more
reliable marker of tissue hypoxia (25-27).
Since blood loss in patients with acute UGIB can lead to a decrease
in oxygen-carrying capacity, lactate levels can serve as a reliable
early marker of hypoperfusion. As cells switch to anaerobic
metabolism in response to hypoperfusion, lactate production is
increased and it is released into the bloodstream (27), leading to adverse outcomes such as
higher mortality rates, rebleeding and increase in ICU admission.
Therefore, using lactate levels for early detection of
hypoperfusion can help clinicians timely identify patients at risk
of adverse outcomes and take appropriate action to prevent further
deterioration (28).
Elevated lactate levels, a reflection of tissue
hypoperfusion and oxygen supply-demand imbalance, emerged as a
potent predictor in the present study. Notably, the association
between higher lactate levels and the need for pRBC transfusion was
more pronounced compared with other clinical outcomes. This
underscores the significance of early lactate measurement,
potentially guiding clinicians towards urgent interventions and
potentially preventing further complications. In addition, lactate
levels can be used to guide resuscitation efforts in patients with
acute UGIB. Early recognition of hypoperfusion can prompt
clinicians to initiate resuscitation measures such as intravenous
fluids, blood transfusions, or vasopressors. Serial lactate
measurements can also be used to monitor response to treatment and
guide ongoing resuscitation efforts (29).
The present study had some limitations. Given the
variations in methodologies and quality among the included
research, its results should interpreted with caution. For some
outcomes, there was significant between-study variability. Due to a
restriction in the number of papers, meta-regression and
publication bias evaluation were not possible. The included studies
measured lactate levels at various time points (at admission, or at
different time intervals after the admission). This variation in
the timing of measurement could have influenced the predictive
accuracy of lactate levels. Additionally, some of the included
studies reported that lactate clearance, or the change in lactate
levels over time, is more important than initial lactate levels in
predicting outcomes. This highlights the potential importance of
monitoring lactate levels serially rather than relying solely on a
single measurement. The studies included in the present review used
different lactate cut-off values to define elevated levels, which
may have affected the results. Future studies with standardized
lactate cut-off values are needed for better comparability and
generalizability of results.
Nonetheless, the present study has several important
implications for surgeons, clinicians and nursing care
professionals. Lactate levels are an important tool for managing
acute UGIB patients and should be used routinely in clinical
practice. The present study also supported the need for more
studies on the predictive accuracy of lactate. It is important to
further evaluate and compare multiple biomarkers and decide on the
best possible combination of tests for prediction of adverse
clinical outcomes in patients with acute UGIB.
Supplementary Material
SEARCH STRATEGY:
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Affiliated
Hospital of Chengdu University of Traditional Chinese Medicine
(grant no. 19KY17).
Availability of data and materials
Data sharing is not applicable to this article, as
no data sets were generated or analyzed during the current
study.
Authors' contributions
FZ conceived and designed the study. LD and LL
collected the data and performed the literature search. FZ was
involved in the writing of the manuscript. All authors read and
approved the final manuscript. Data authentication is not
applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wuerth BA and Rockey DC: Changing
epidemiology of upper gastrointestinal hemorrhage in the last
decade: A nationwide analysis. Dig Dis Sci. 63:1286–1293.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
DiGregorio AM and Alvey H:
Gastrointestinal bleeding. In: StatPearls. StatPearls Publishing,
Treasure Island, FL, 2023.
|
|
3
|
Kaya E, Karaca MA, Aldemir D and Ozmen MM:
Predictors of poor outcome in gastrointestinal bleeding in
emergency department. World J Gastroenterol. 22:4219–4225.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Stokbro LA, de Muckadell OB and Laursen
SB: Arterial lactate does not predict outcome better than existing
risk scores in upper gastrointestinal bleeding. Scand J
Gastroenterol. 53:586–591. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wada T, Hagiwara A, Uemura T, Yahagi N and
Kimura A: Early lactate clearance for predicting active bleeding in
critically ill patients with acute upper gastrointestinal bleeding:
A retrospective study. Intern Emerg Med. 11:737–743.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kim K, Lee DH, Lee DH, Choi YH and Bae SJ:
Early lactate clearance for predicting outcomes in patients with
gastrointestinal bleeding. Ir J Med Sci. 192:1923–1929.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Rabinowitz JD and Enerbäck S: Lactate: The
ugly duckling of energy metabolism. Nat Metab. 2:566–571.
2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Schmiedeknecht K, Kaufmann A, Bauer S and
Solis FV: L-lactate as an indicator for cellular metabolic status:
An easy and cost-effective colorimetric L-lactate assay. PLoS One.
17(e0271818)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Andersen LW, Mackenhauer J, Roberts JC,
Berg KM, Cocchi MN and Donnino MW: Etiology and therapeutic
approach to elevated lactate levels. Mayo Clin Proc. 88:1127–1140.
2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
11
|
Wells G, Shea B, O’Connell D, Robertson J,
Peterson J, Losos M and Tugwell P: The Newcastle-ottawa scale (NOS)
for assessing the quality of nonrandomized studies in meta-
analysis. Ottawa Hospital Research Institute, Ottawa ON, 2011.
|
|
12
|
Borenstein M, Hedges LV, Higgins JPT and
Rothstein HR: A basic introduction to fixed-effect and
random-effects models for meta-analysis. Res Synth Methods.
1:97–111. 2010.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Wang J, Keusters WR, Wen L and Leeflang
MMG: IPDmada: An R Shiny tool for analyzing and visualizing
individual patient data meta-analyses of diagnostic test accuracy.
Res Synth Methods. 12:45–54. 2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Shrestha MP, Borgstrom M and Trowers EA:
Elevated lactate level predicts intensive care unit admissions,
endoscopies and transfusions in patients with acute
gastrointestinal bleeding. Clin Exp Gastroenterol. 11:185–192.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gulen M, Satar S, Tas A, Avci A, Nazik H
and Firat BT: Lactate level predicts mortality in patients with
upper gastrointestinal bleeding. Gastroenterol Res Pract.
2019(5048078)2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lee SH, Min YW, Bae J, Lee H, Min BH, Lee
JH, Rhee PL and Kim JJ: Lactate parameters predict clinical
outcomes in patients with nonvariceal upper gastrointestinal
bleeding. J Korean Med Sci. 32:1820–1827. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Berger M, Divilov V and Teressa G: Lactic
acid is an independent predictor of mortality and improves the
predictive value of existing risk scores in patients presenting
with acute gastrointestinal bleeding. Gastroenterology Res. 12:1–7.
2019.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
Ko BS, Kim WY, Ryoo SM, Ahn S, Sohn CH,
Seo DW, Lee YS, Lim KS and Jung HY: Predicting the occurrence of
hypotension in stable patients with nonvariceal upper
gastrointestinal bleeding: Point-of-care lactate testing. Crit Care
Med. 43:2409–2415. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
El-Kersh K, Chaddha U, Sinha RS, Saad M,
Guardiola J and Cavallazzi R: Predictive role of admission lactate
level in critically Ill patients with acute upper gastrointestinal
bleeding. J Emerg Med. 49:318–325. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Shah A, Chisolm-Straker M, Alexander A,
Rattu M, Dikdan S and Manini AF: Prognostic use of lactate to
predict inpatient mortality in acute gastrointestinal hemorrhage.
Am J Emerg Med. 32:752–755. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Strzałka M, Winiarski M, Dembiński M,
Pędziwiatr M, Matyja A and Kukla M: Predictive role of admission
venous lactate level in patients with upper gastrointestinal
bleeding: A prospective observational study. J Clin Med.
11(335)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Saffouri E, Blackwell C, Laursen SB, Laine
L, Dalton HR, Ngu J, Shultz M, Norton R and Stanley AJ: The Shock
Index is not accurate at predicting outcomes in patients with upper
gastrointestinal bleeding. Aliment Pharmacol Ther. 51:253–260.
2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Benedeto-Stojanov D, Bjelaković M,
Stojanov D and Aleksovski B: Prediction of in-hospital mortality
after acute upper gastrointestinal bleeding: Cross-validation of
several risk scoring systems. J Int Med Res.
50(3000605221086442)2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chang A, Ouejiaraphant C, Akarapatima K,
Rattanasupa A and Prachayakul V: Prospective comparison of the
AIMS65 score, glasgow-blatchford score and rockall score for
predicting clinical outcomes in patients with variceal and
nonvariceal upper gastrointestinal bleeding. Clin Endosc.
54:211–221. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Neville AL, Nemtsev D, Manasrah R, Bricker
SD and Putnam BA: Mortality risk stratification in elderly trauma
patients based on initial arterial lactate and base deficit levels.
Am Surg. 77:1337–1341. 2011.PubMed/NCBI
|
|
26
|
Jansen TC, van Bommel J, Mulder PG, Rommes
JH, Schieveld SJM and Bakker J: The prognostic value of blood
lactate levels relative to that of vital signs in the pre-hospital
setting: A pilot study. Crit Care. 12(R160)2008.PubMed/NCBI View
Article : Google Scholar
|
|
27
|
Northfield TC, Kirby BJ and Tattersfield
AE: Acid-base balance in acute gastrointestinal bleeding. Br Med J.
2:242–244. 1971.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Foucher CD and Tubben RE: Lactic acidosis.
In: StatPearls. StatPearls Publishing, Treasure Island (FL),
2023.
|
|
29
|
Krishna U, Joshi SP and Modh M: An
evaluation of serial blood lactate measurement as an early
predictor of shock and its outcome in patients of trauma or sepsis.
Indian J Crit Care Med. 13:66–73. 2009.PubMed/NCBI View Article : Google Scholar
|