Introduction
As the global population ages, the number of primary
total hip arthroplasty (THA) procedures and that of THA revision
procedures is expected to increase markedly (1,2). A
systematic literature review showed that hip prosthesis survival
rates over 10 years ranged from 91.0-99.4% among 1,385 patients
with THA in the Danish National Patient Registry from January 2004
to December 2017 (3-5),
and the volume of hip revision arthroplasty in the United States
increased to 10-15% of the total joint arthroplasty (6,7). The
common causes of THA revision include wear of prosthetic
components, mechanical loosening, hip instability and infection,
among which acetabular bone defects are present in >50% cases
and are difficult to locate and quantify (8). Reconstruction of acetabular bone
defects is the most critical factor for successful replacement and
is the most daunting challenge for THA revision (9-11).
Computer-aided technology has been successfully
applied in orthopedic instrument design, materials and surgical
simulation with mature technology applications (12-14).
Previous studies have (15,16)
used Mimics software to simulate the reconstruction of a high
dislocated acetabulum, with an individualized and precise
preoperative design to obtain satisfactory acetabular cup position
and coverage and to avoid problems such as iliopsoas impingement.
However, to the best of our knowledge, no studies have been carried
out yet on computer-assisted simulation in acetabular revision.
Thus, to improve the accuracy of acetabular prosthesis implantation
and surgical efficiency during revision surgery, the present study
admitted 10 patients with loose acetabular prosthesis revision From
January 2017 to June 2021, and applied Mimics 17.0 software to
preoperatively simulate the release and acetabular prosthesis
implantation and determine the ideal acetabular center, actual
acetabular center and acetabular prosthesis size, and obtained
satisfactory acetabular prosthesis position and limb length, which
are reported below.
Materials and methods
Patient information
This study included 10 patients who underwent hip
revision at Nanchang and Yingtan hospitals of The 908th Hospital of
the Joint Logistic Support Force (Great Wall Hospital Affiliated to
Nanchang University) from January 2017 to June 2021. The ethical
approval number was approval no. Hospital Medical Service (2017)13.
Each patient included in this study provided written informed
consent. The present study included 10 hips of 10 patients [mean
age, 31-61 (44.2±10.1) years; seven men (seven hips) and three
women (three hips)]. All patients had loose or broken acetabular
prostheses, two had initial replacement femoral neck fracture and
eight had osteonecrosis of the femoral head. The time between
initial replacement and revision surgery ranged from 1 to 15
(5.2±4.3) years. Preoperative shortening of the affected limb was
evaluated by orthogonal pelvis radiography and computed tomography
(CT) from 15 to 35 (25.1±6.3) mm. Patients underwent preoperative
radiography and 3D CT to clarify the fusion of the acetabulum and
acetabular component and the acetabular bone volume and quality.
Magnetic resonance imaging (MRI) was repeated to rule out infection
in patients with a history of previously infected fusion. However,
because of significant artifacts associated with outdated models of
prosthetics, not all cases could undergo MRI to rule out infection.
For patients in whom infection could not be excluded by MRI, the
present study primarily relied on the following methods for
infection assessment: i) Preoperative levels of C-reactive protein
and erythrocyte sedimentation rate should both not exceed 40; and
ii) if infection was suspected during the operation, frozen section
was taken for pathological examination (neutrophil <5 per
high-power field) to rule out infection.
Simulated surgery and intraoperative
and perioperative management. Imaging data collection
Hardware: 64-row spiral CT (LightSpeed VCT 64) from
GE Healthcare Life Sciences; Thinkpad T460 (I5; 16G; 1TB; NVIDIA
GeForce940/2GB; Lenovo Group). Software: Win10 64-bit Professional
(Microsoft Corporation); Mimics 17.0 (Materialise NV); Solidworks
2011 SP0.0 (Dassault Systèmes SE). Patients underwent pelvic
scanning (including the hip and upper femur) with the following
parameters: Layer thickness, 0.625 mm; 120 kV; and 240 mA.
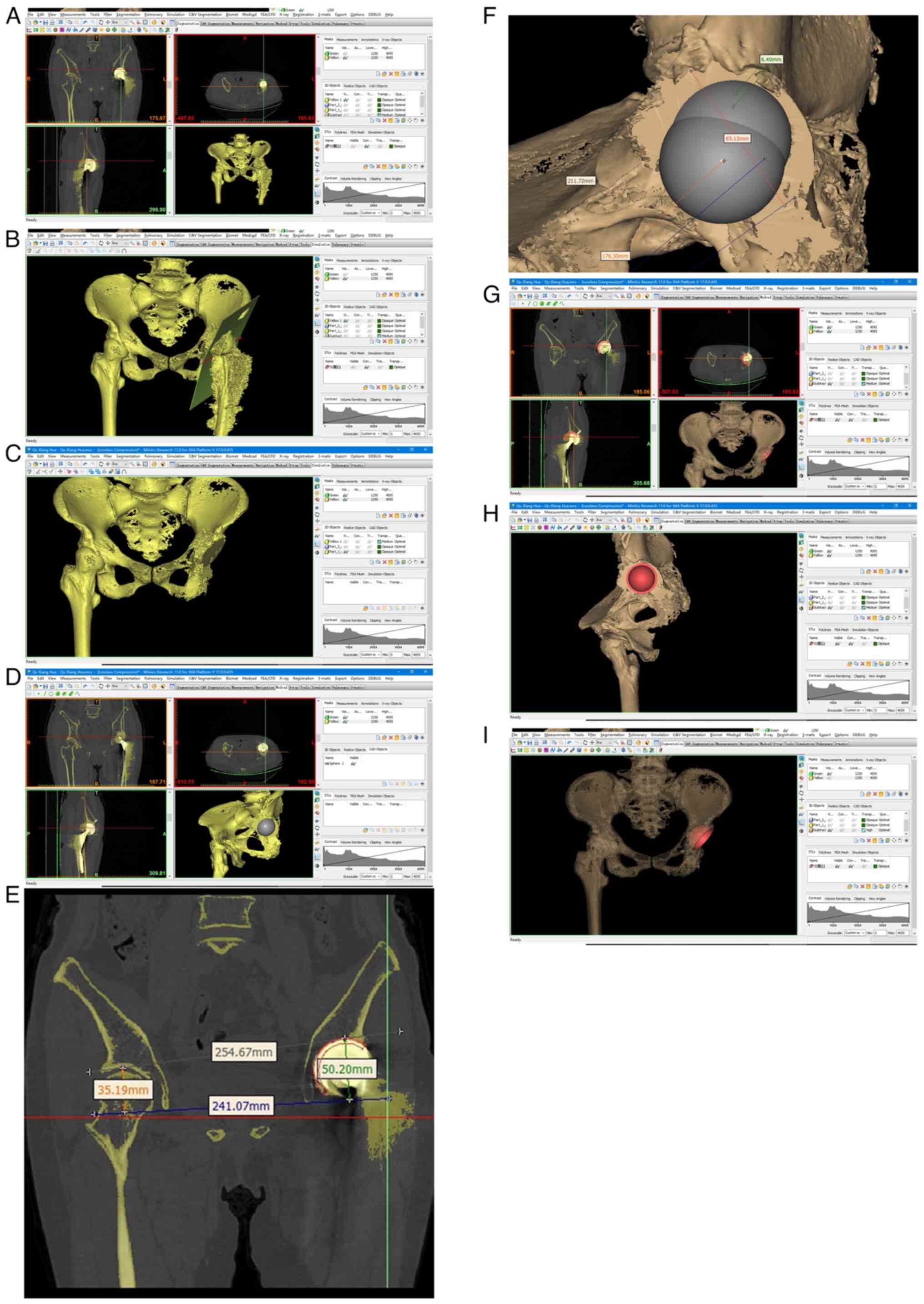
Pre-operative 3D CT
reconstruction
The preoperative CT image data were saved in Digital
Imaging and Communications in Medicine format and imported into
Mimics software. The thresholding function button in Mimics
software was used to create a bone window mask and generate a 3D
model of the pelvis. The ‘Cut with Polyplane’ function was used to
create a Polyplane (CP1) at the anterior and posterior edges of the
initial acetabulum. The osteophytes of the femur were removed using
the Split function to simulate the femoral prosthesis dislocation
and to establish the acetabular model. Subsequently, 2-3 ‘spheres’
of different diameters were created in Medcad to simulate the
reaming of the acetabulum and to confirm that they reached the
cancellous bone surface at all three levels, sagittal, coronal and
transverse. After confirming the ‘spheres’ diameter, the Boolean
calculation was performed to obtain the model of the acetabulum
after reaming. The corresponding diameter of the spherical
acetabular model was established in Solidworks according to the
hole made in the acetabulum. The model was saved in the
stereolithography format and imported into Mimics. It was placed
into the osteotomy acetabulum through movement and rotation to
retain the appropriate size of the acetabulum. A coverage rate of
>75% was considered eligible (17). There are two concepts involved in
the operation, namely the ‘ideal acetabular center’ and ‘actual
acetabular center’. The ideal acetabular center is calculated by
Sphere simulation based on the reference of the contralateral
acetabular center, while the actual acetabular center is the
position that needs to be reamed to the cancellous bone surface
when the original acetabular component is removed. The ideal
acetabular center combined with bone graft or tantalum implant was
used. If the height difference was <10 mm, the actual acetabular
center combined with lengthening of the femoral ball head was used
(Fig. 1).
Surgical method
The patient was placed in the lateral decubitus
position and general anesthesia was induced. Via a posterolateral
approach to the hip joint, the femoral neck, large trochanter and
minor trochanter and the femoral prosthesis were exposed, making
sure to protect the sciatic nerve. Upon fully loosening the
acetabulum and large trochanter and minor trochanter, the
acetabulum and the femoral prosthesis were exposed. It was
repeatedly confirmed that the femoral stem was still loose; if not,
we continued to loosen and dislocate the lateral femoral prosthesis
to the top of the outer acetabulum to provide sufficient space for
the removal of the acetabular prosthesis. After loosening the edge
of the acetabular prosthesis, the scar on the edge of the
acetabular prosthesis was removed to expose the bony border,
subsequently we tapped with a special curved osteotome close to the
edge of the acetabular prosthesis to separate it from the
acetabular bone. This separation step was performed gently to avoid
removing too much cancellous bone or causing an acetabular
fracture. After removing the prosthesis and referring to the size
of the preoperative simulated acetabular cup, the acetabulum was
reamed to 2-3 sizes smaller than the preoperative simulated size,
using the ‘wall-holding’ method when reaming the acetabulum,
starting from the position of the transverse ligament. After the
acetabular scar was basically removed, the reverse acetabulum
reamer was used when it was close to the size of the preoperative
simulation. The maximum size of the acetabulum reamer did not
exceed the maximum size of the preoperative simulation. Finally,
the appropriate acetabular cup was placed, and C-arm fluoroscopy
was used to confirm that the position of the prosthesis was correct
and then sutured layer by layer.
Perioperative management
Cefazolin sodium (1.0 g) were administered routinely
30 min preoperatively and no more than 48 h postoperatively.
Preoperative intravenous drip of 0.5 of injectable tranexamic acid,
with 20 ml saline dissolved in 0.5 g tranexamic acid was injected
into the drainage tube after closing the incision, and the drainage
tube was clamped shut for 2 h and then released. The drainage tube
was removed within 48 h postoperatively. Postoperative low
molecular-weight heparin sodium anticoagulation was performed.
Muscle strength training of hip abductors and other muscles was
started after awakening from anesthesia, and standing was assisted
by a walker 48 h postoperatively.
Observation items
The operation time, intraoperative bleeding and
Harris hip score (18) at 3 months
and 12 months after surgery were recorded, and the postoperative
acetabular anteversion and abduction angles were measured according
to the Pradhan method (19).
Statistical analysis
The statistical analysis was conducted using SPSS
25.0 software (IBM Corp.), and the measurement data are presented
as mean ± standard deviation. To assess the normal distribution of
the data, we performed the Shapiro-Wilk test and examined the
associated P-values for all test items, which indicated a normal
distribution. Repeated measures analysis of variance (ANOVA) was
employed to evaluate Harris scores at three consecutive time points
post-enrollment, with within-subject effect testing applied when
Mauchly's sphericity assumption was met. Post hoc tests for Harris
scores before operation, at 3 months, and at 12 months after
operation were conducted using Bonferroni correction. P<0.05 was
considered to indicate statistically significant differences, and a
two-tailed hypothesis test with a 95% confidence interval was
utilized.
Results
All patients were followed-up for 12-48 (23.5±11.8)
months. No postoperative dislocation or infection of the prosthesis
occurred, and one case had numbness of the lateral calf skin due to
incomplete injury of the sciatic nerve caused by intraoperative
pulling, which was treated with mecobalamin (0.5 g three times a
day) and the patient recovered 3 months after surgery.
Postoperative acetabular cup abduction angle
(39.7±3.4˚), anteversion angle (15.8±2.8˚), abduction angle and
anteversion angle were within Lewinnek's safety (20) range in all cases. Preoperative limb
shortening was 25.1±6.3 mm, intraoperative ideal acetabular center
and actual acetabular center difference was 13.3±6.3 mm and
postoperative limb shortening was 1.6±4.9 mm. Postoperative
acetabular cup bone coverage was 85.2±8.2%; the preoperative Harris
hip score points were 20.9±4.3, at 3 months post-operation it was
47.2±7.7 points and at 12 months post-operation it improved to
85.4±5.3 points; bleeding volume was 332.5±61.3 ml; and operative
time was 79.0±7.0 min (Table I)
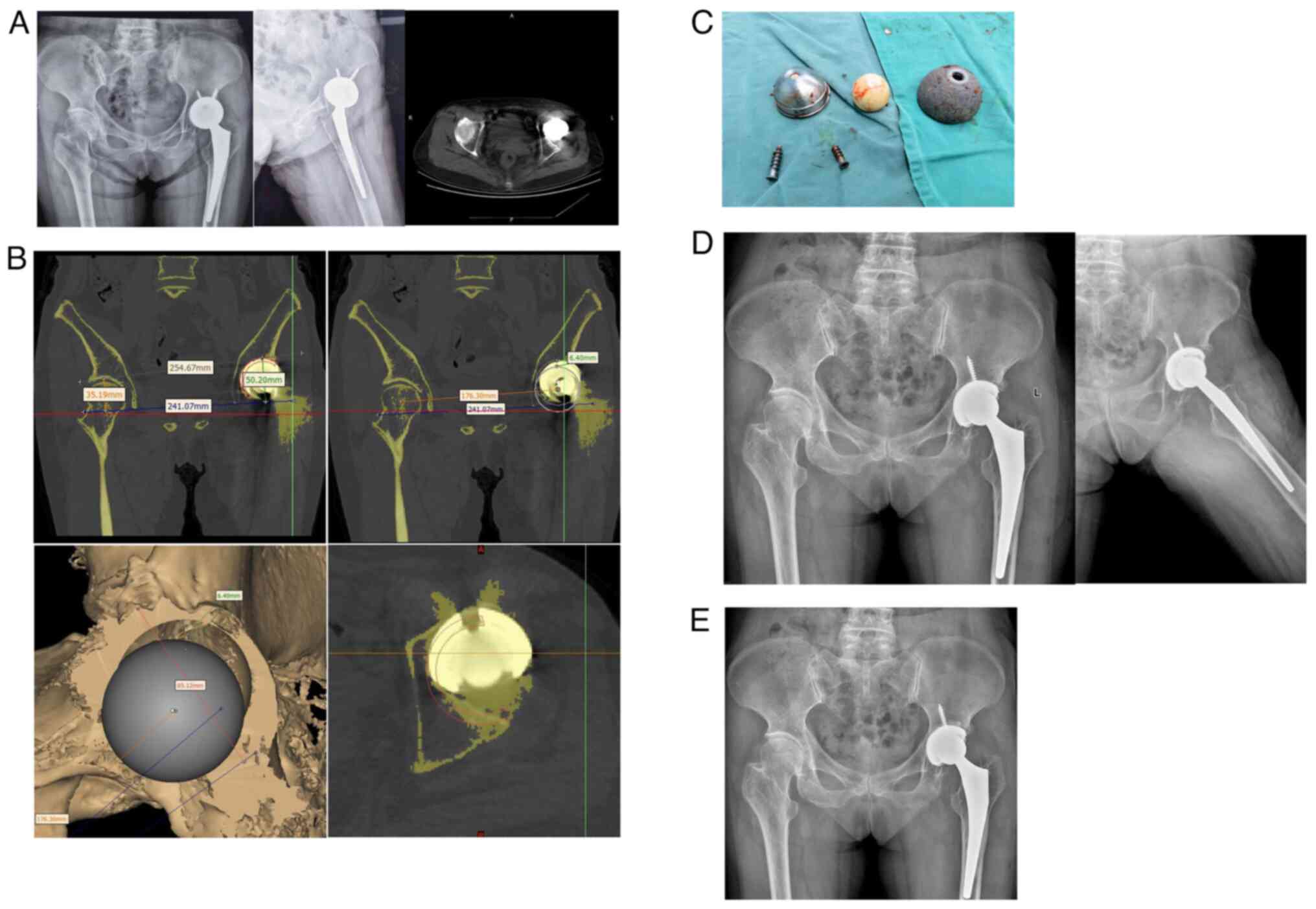
The typical cases are illustrated in Fig. 2. There was a statistically
significant overall difference in preoperative, 3 months
postoperative and 12 months postoperative Harris hip scores
(repeated measures ANOVA; F=245.23; P<0.001). There were
statistically significant differences in hip Harris scores before
and after operation, 3 months and 6 months after operation
(P<0.001; Table II).
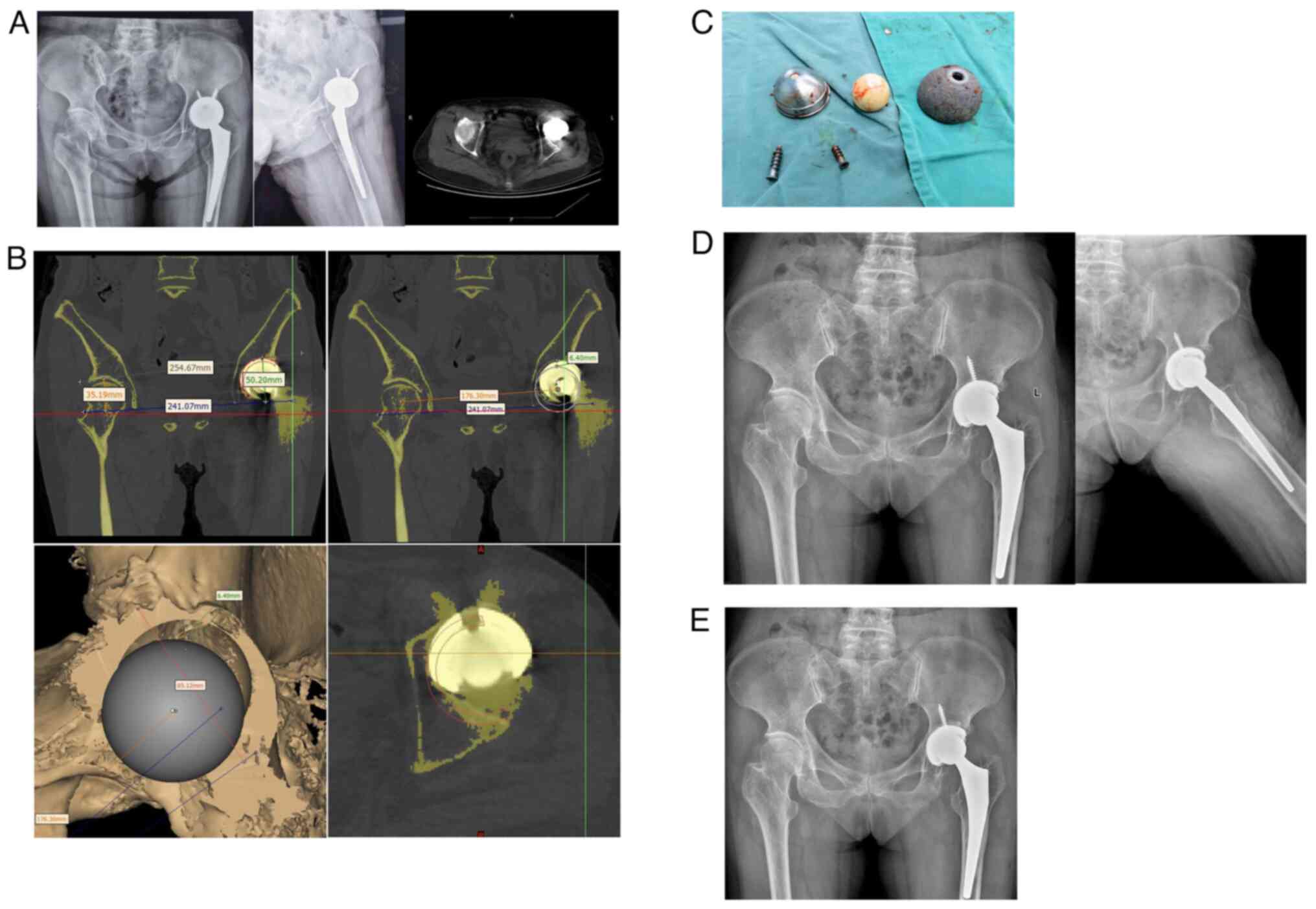 | Figure 2(A) Typical case: The patient was a
61-year-old woman who presented with a loose flip of the acetabular
lateral prosthesis 5 years after total hip arthroplasty for a
femoral neck fracture (first surgery with a Stryker all-ceramic
prosthesis). At 5 years after femoral neck fracture surgery,
radiography and computerized tomography both suggested loosening of
the lateral acetabular prosthesis and acetabular flip to the
anterior acetabulum, which was assessed as a Paprosky type I bone
defect with preoperative measurement of 28-mm shortening of the
affected limb. (B) According to the methodology of the present
paper, Mimics 17.0 software was used to preoperatively simulate the
surgery, and the maximum outer diameter of the acetabular
prosthesis could not exceed 52 mm (coverage rate, 91.7%), and the
ideal acetabular center was 6-mm lower compared with the actual
reamed acetabular cup. Moreover, the actual reamed acetabular
center was planned to be selected intraoperatively, while the long
ceramic ball head of the same brand was replaced to avoid
shortening of the affected limb. (C) During the operation, the
acetabular side prosthesis was completely removed with very little
bone destruction. The acetabular prosthesis of 52-mm diameter was
replaced according to the preoperative plan, and a large ceramic
ball head of plus 7 mm was selected. (D) On the postoperative
review radiograph, the affected limb was shortened by ~1 mm, and
the acetabular prosthesis was well positioned with an abduction
angle of 39˚ and an anteversion angle of 16˚. (E) Radiographs were
repeated 12 months after surgery and were in good position. |
 | Table IPre-operative and post-operative
follow-up data for each case. |
Table I
Pre-operative and post-operative
follow-up data for each case.
| | Harris score |
|---|
| Case | Sex | Age, years | Medical history,
years | Type of primary
acetabular component | Shortening (pre-op),
mm | Acetabular center
difference, mm | Paprosky type | Shortening (Post-op),
mma | Intraoperative
bleeding, ml | Operation duration,
min | Follow-up time,
months | Abduction angle,
˚ | Anteversion angle,
˚ | Acetabular coverage,
% | Pre-op | 3 months
(Post-op) | 12 months
(Post-op) |
|---|
| 1 | M | 32 | 1 | Zweymuller biocon
cup | 25 | 11 | I | 5 | 450 | 90 | 48 | 40 | 10 | 88.9 | 15 | 45 | 90 |
| 2 | M | 46 | 2 | Beijing AiKang APT
A-Cup | 18 | 15 | I | 2 | 275 | 80 | 37 | 41 | 15 | 94.4 | 16 | 42 | 87 |
| 3 | M | 44 | 3 | Beijing Montagne
KG | 20 | 8 | I | 2 | 350 | 70 | 24 | 39 | 13 | 77.8 | 22 | 56 | 85 |
| 4 | M | 48 | 4 | Zweymuller biocon
cup | 22 | 12 | I | 5 | 275 | 85 | 21 | 40 | 18 | 70.0 | 28 | 61 | 80 |
| 5 | M | 49 | 2 | Beijing AiKang APT
A-Cup | 31 | 15 | II | 7 | 400 | 80 | 16 | 38 | 20 | 80.6 | 23 | 43 | 81 |
| 6 | F | 42 | 8 | Beijing Montagne
KG | 15 | 20 | II | -5 | 350 | 80 | 13 | 32 | 17 | 83.3 | 19 | 39 | 90 |
| 7 | M | 56 | 15 | Zweymuller biocon
cup | 27 | 25 | III | 8 | 300 | 85 | 15 | 45 | 18 | 86.1 | 16 | 54 | 80 |
| 8 | F | 61 | 5 | Strykle Osteonics
Crossfire | 28 | 6 | I | 1 | 250 | 70 | 12 | 39 | 16 | 91.7 | 25 | 47 | 78 |
| 9 | M | 31 | 3 | Zweymuller biocon
cup | 30 | 16 | II | -3 | 350 | 80 | 18 | 43 | 15 | 97.2 | 21 | 48 | 91 |
| 10 | F | 33 | 9 | Beijing AiKang APT
A-Cup | 35 | 5 | I | -6 | 325 | 70 | 31 | 40 | 16 | 82.2 | 24 | 37 | 92 |
 | Table IIComparison of preoperative (n=10), 3
months postoperative (n=10) and 12 months postoperative (n=10)
Harris scores of patients. |
Table II
Comparison of preoperative (n=10), 3
months postoperative (n=10) and 12 months postoperative (n=10)
Harris scores of patients.
| | Repeated measures
analysis of variance |
|---|
| Group | Harris score | F | P-value |
|---|
| Preoperative | 20.9±4.3 | 245.23 | <0.001 |
| 3 months
postoperative |
47.2±7.7a | | |
| 12 months
postoperative |
85.4±5.3a,b | | |
Discussion
Loosening of the prosthesis after hip arthroplasty
often causes pain, resulting in limited walking and thus disuse
osteoporosis (21-23).
Revision hip arthroplasty has high risks and a number of variables,
making it a difficult operation in joint surgery (24). Inadequate preoperative and tools
preparation can easily lead to catastrophic intraoperative
consequences, such as massive bone loss, acetabular fracture and
acetabular prosthesis sinking into the pelvis (25,26).
Understandably, acetabular reconstruction is one of the major
difficulties of this operation. The aim of acetabular
reconstruction is to restore the anatomical center of the hip joint
and construct a peri-acetabular support band to bring the new
acetabular prosthesis into full contact with the acetabular bone
and maintain long-term stability and durability, and to minimize
the bone defects formed in the replacement (27-30).
However, the risk of a poor acetabular cup mounting position due to
unclear anatomical landmarks and inaccurate positioning during hip
revision is high, and the use of the traditional reaming acetabular
positioning method requires a high level of surgical skill and
clinical experience (31).
Moreover, it is relatively difficult to accumulate surgical
experience and hone skills given the small number of cases, too
many intraoperative variables and a long learning curve (25-27).
Preoperative 3D analysis simulates the surgery to
help preoperatively fully understand the morphological
characteristics of the acetabulum, assess the degree of bone loss
and select the appropriate size acetabular prosthesis (32-34).
Zeng et al (35) have
performed preoperative 3D simulated surgery in Mimics for patients
with congenital hip dislocation with high dislocation, but it
requires a high level of operating skills. Sugano et al
(36) report the use of an
intraoperative acetabular Computer-Aided Design (CAD) device to
improve the accuracy of acetabular cup implantation, but its
diffusion was affected by the expensive device and relatively
cumbersome intraoperative operation. Zhang et al (37) used a positioning-guidance assisted
technique for intraoperative acetabular reaming in patients with
congenital hip dislocation. This technique is accurate in
positioning and easy to operate intraoperatively, but it is
relatively difficult to produce and design, because the design of
the guide template requires CAD software operating skills and
experience. Wu et al (38)
designed a self-developed CAD/rapid prototyping/intraoperative
positioner system to simulate acetabular cup prosthesis
implantation, and used self-developed digital light processing 3D
printer-light-curing surface-forming technology to match and
position the acetabular positioner claw tip with the external
orifice edge of the model to guide the direction of acetabular
reaming. However, because the directional rod operation occupies a
certain space, the intraoperative operation requires a large
surgical area to be exposed and is not suitable for surgery to
preserve the femoral prosthesis.
Our group previously used the Mimics software for
simulations to assess acetabular prosthesis size, bone defects and
acetabular prosthesis coverage in hip dysplasia cases, but in
acetabular prosthesis revision, the bone defects resulting from
acetabular prosthesis removal need to be considered when
reconstructing the simulated surgery owing to the influence of the
original acetabular prosthesis (39,40).
Therefore, the present research will help to judge the size of the
bone defect after prosthesis implantation based on the difference
between the ideal acetabular center and the actual acetabular
center, to choose whether to add a pad or to solve the problem of
limb shortening by replacing the ceramic ball head, which is
relatively simple and easy to operate and promote the use of. The
present study also used the method provided by previous studies
(17,27) to assess the bone coverage of the
new acetabular prosthesis after removal of the loosened acetabular
prosthesis. Since the femoral stem prosthesis was not removed in
any of the cases in this group, the present study replaced the
plus-sized ball heads or padded blocks as appropriate according to
the height difference between the ideal acetabular center and the
actual acetabular center, and ground the acetabulum to match the
large ball head of 32 mm or ≥38 mm in diameter as much as possible
to compensate for the limb shortening owing to the bone defect. All
patients in this group had intraoperative loosening of the
acetabular lateral prosthesis. Because of the gentle intraoperative
operation, the degree of intraoperative acetabular lateral bone
defect due to surgical technique was mild, so none of the pads were
used. In addition, the postoperative shortening was reduced to
within 0.5 cm, and all patients were satisfied with the
postoperative results. Due to the limited number of patients in
this category, the present study collected a relatively small
number of cases. Currently, the present study is just a preliminary
experimental report, so a control group has not been established.
More data will be gathered in the future to enhance the study.
In conclusion, the use of digital simulation
assistance can improve the accuracy of hip revision acetabular
prosthesis implantation and reduce postoperative shortening of the
affected limb. Especially for surgeons with relatively little
experience in hip revision surgery, it provides a reference for the
reasonable placement of the prosthesis and greatly reduces
complications such as hip dislocation because of poor postoperative
prosthesis position. However, because of the small number of cases
in the present study and the absence of cases with bone defects of
>3 cm, the effectiveness of the method could not be verified in
such cases.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by The PLA's High-level
Talents Independently Projects [grant no. (2022)17-02] and Subject
of Health Commission of Jiangxi Province (grant no. 20203826).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JJZ, HDL, DL, BC, FS, HL, SLL and LL analyzed the
data and edited the manuscript. JJZ, HDL, DL and BC helped to
perform the follow-up and to collect patients' data. JJZ, DL and FS
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Ethics committee approval for use of individual
participant data was granted by the ethics committee of the 908th
Hospital of Joint Logistic Support Force of PLA to this study
[approval no. Hospital Medical Service (2017)13]. Signed written
informed consent was obtained from the patients and/or
guardians.
Patient consent for publication
Consent for publication of the patients' data and
images was obtained from patients or their relatives.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Schwartz AM, Farley KX, Guild GN and
Bradbury TL Jr: Projections and epidemiology of revision hip and
knee arthroplasty in the united states to 2030. J Arthroplasty. 35
(Suppl):S79–S85. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Marsh M and Newman S: Trends and
developments in hip and knee arthroplasty technology. J Rehabil
Assist Technol Eng. 8(2055668320952043)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Darrith B, Courtney PM and Della Valle CJ:
Outcomes of dual mobility components in total hip arthroplasty: A
systematic review of the literature. Bone Joint J. 100-B:11–19.
2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hauer G, Heri A, Klim S, Puchwein P,
Leithner A and Sadoghi P: Survival rate and application number of
total hip arthroplasty in patients with femoral neck fracture: An
analysis of clinical studies and National arthroplasty registers. J
Arthroplasty. 35:1014–1022. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Larsen JB, Mechlenburg I, Jakobsen SS,
Thilleman TM and Søballe K: 14-year hip survivorship after
periacetabular osteotomy: A follow-up study on 1,385 hips. Acta
Orthop. 91:299–305. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kurtz SM, Ong KL, Lau E and Bozic KJ:
Impact of the economic downturn on total joint replacement demand
in the United States: Updated projections to 2021. J Bone Joint
Surg Am. 96:624–630. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chapman RM, Van Citters DW, Chapman D and
Dalury DF: Higher offset cross-linked polyethylene acetabular
liners: Is wear a significant clinical concern? Hip Int.
29:652–659. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Petis SM, Kubista B, Hartzler RU, Abdel MP
and Berry DJ: Polyethylene liner and femoral head exchange in total
hip arthroplasty: Factors associated with long-term success and
failure. J Bone Joint Surg Am. 101:421–428. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Koob S, Scheidt S, Randau TM, Gathen M,
Wimmer MD, Wirtz DC and Gravius S: Biological downsizing:
Acetabular defect reconstruction in revision total hip
arthroplasty. Orthopade. 46:158–167. 2017.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
10
|
Miettinen HJ, Miettinen SS, Kettunen JS,
Jalkanen J and Kröger H: Revision hip arthroplasty using a porous
tantalum acetabular component. Hip Int. 31:782–788. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Garcia-Rey E, Saldaña L and
Garcia-Cimbrelo E: Impaction bone grafting in hip re-revision
surgery. Bone Joint J. 103-B:492–499. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lewinnek GE, Lewis JL, Tarr R, Compere CL
and Zimmerman JR: Dislocations after total hip-replacement
arthroplasties. J Bone Joint Surg Am. 60:217–220. 1978.PubMed/NCBI
|
|
13
|
Zhou JJ, Zhao M, Liu D, Liu HY and Du CF:
Biomechanical property of a newly designed assembly locking
compression plate: Three-Dimensional finite element analysis. J
Healthc Eng. 2017(8590251)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Shen X, Tian H, Li Y, Zuo J, Gao Z and
Xiao J: Acetabular revision arthroplasty based on 3-Dimensional
reconstruction technology using jumbo cups. Front Bioeng
Biotechnol. 10(799443)2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yang Y, Liao W, Yi W, Jiang H, Fu G, Ma Y
and Zheng Q: Three-dimensional morphological study of the proximal
femur in Crowe type IV developmental dysplasia of the hip. J Orthop
Surg Res. 16(621)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chen JX, Yu ZY, Cheng QX, Fu MQ, Shi BN,
Yang J, Zhou JJ and Zhao M: Application of personalized digital
analog assisted acetabular prosthesis precise implantation in Crowe
typeⅠand Ⅱhip dysplasia. China J Orthop Trauma. 35:605–609.
2022.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
17
|
Silber DA and Engh CA: Cementless total
hip arthroplasty with femoral head bone grafting for hip dysplasia.
J Arthroplasty. 5:231–240. 1990.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lakhotia D and Agrawal U: Functional
outcome of uncemented total hip replacement in low socioeconomic
group using modified harris hip score: A prospective midterm
Follow-Up study. Cureus. 15(e50005)2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Pradhan R: Planar anteversion of the
acetabular cup as determined from plain anteroposterior
radiographs. J Bone Joint Surg Br. 81:431–435. 1999.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Takemoto N, Nakamura T, Kagawa K,
Maruhashi Y, Sasagawa T, Funaki K, Aikawa T and Yamamoto D:
Clinical outcomes of total hip arthroplasty with the anterolateral
modified Watson-Jones approach for displaced femoral neck
fractures. Geriatr Orthop Surg Rehabil.
13(21514593221134800)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Fröschen FS, Schell S, Wimmer MD,
Hischebeth GTR, Kohlhof H, Gravius S and Randau TM: Synovial
complement factors in patients with periprosthetic joint infection
after undergoing revision arthroplasty of the hip or knee joint.
Diagnostics (Basel). 11(434)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Bondarenko S, Filipenko V, Badnaoui AA,
Ashukina N, Maltseva V, Lazarenko I and Schwarzkopf R:
Periacetabular bone changes after total hip arthroplasty with
highly porous titanium cups in patients with low bone mass. Wiad
Lek. 75:1629–1633. 2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kweon SH, Park JS and Park BH: Sarcopenia
and its association with change of bone mineral density and
functional outcome in old-aged hip arthroplasty patients. Geriatr
Orthop Surg Rehabil. 13(21514593221121377)2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Harris WH: The three revolutions in
acetabular revision surgery for total hip replacement: 1. Definite
and 2. Probable. Chir Organi Mov. 88:1–13. 2003.PubMed/NCBI
|
|
25
|
Quinlan ND, Werner BC, Brown TE and Browne
JA: Risk of prosthetic joint infection increases following early
aseptic revision surgery of total hip and knee arthroplasty. J
Arthroplasty. 35:3661–3667. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Grosso MJ, Kozaily E, Cacciola G and
Parvizi J: Characterizing femoral and acetabular bone loss in
two-stage revision total hip arthroplasty for infection. J
Arthroplasty. 36:311–316. 2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Cosyn J, Eghbali A, Hanselaer L, De Rouck
T, Wyn I, Sabzevar MM, Cleymaet R and De Bruyn H: Four modalities
of single implant treatment in the anterior maxilla: A clinical,
radiographic, and aesthetic evaluation. Clin Implant Dent Relat
Res. 15:517–530. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chiarlone F, Zanirato A, Cavagnaro L,
Alessio-Mazzola M, Felli L and Burastero G: Acetabular custom-made
implants for severe acetabular bone defect in revision total hip
arthroplasty: A systematic review of the literature. Arch Orthop
Trauma Surg. 140:415–424. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
von Lewinski G: Custom-made acetabular
implants in revision total hip arthroplasty. Orthopade. 49:417–423.
2020.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
30
|
Wirtz DC, Jaenisch M, Osterhaus TA, Gathen
M, Wimmer M, Randau TM, Schildberg FA and Rössler PP: Acetabular
defects in revision hip arthroplasty: A therapy-oriented
classification. Arch Orthop Trauma Surg. 140:815–825.
2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Giaretta S, Lunardelli E, Di Benedetto P,
Aprato A, Spolettini P, Mancuso F, Momoli A and Causero A: The
current treatment of hip arthroplasty revision: A systematic review
of the literature. Acta Biomed. 94(e2023092)2023.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Maldonado DR, Go CC, Kyin C, Rosinsky PJ,
Shapira J, Lall AC and Domb BG: Robotic Arm-assisted total hip
arthroplasty is more cost-effective than manual total hip
arthroplasty: A markov model analysis. J Am Acad Orthop Surg.
29:e168–e177. 2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Weber M, Witzmann L, Wieding J, Grifka J,
Renkawitz T and Craiovan B: Customized implants for acetabular
Paprosky III defects may be positioned with high accuracy in
revision hip arthroplasty. Int Orthop. 43:2235–2243.
2019.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Myers CA, Huff DN, Mason JB and
Rullkoetter PJ: Effect of intraoperative treatment options on hip
joint stability following total hip arthroplasty. J Orthop Res.
40:604–613. 2022.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Zeng Y, Lai OJ, Shen B, Yang J, Zhou ZK,
Kang PD, Pei FX and Zhou X: Three-dimensional computerized
preoperative planning of total hip arthroplasty with high-riding
dislocation developmental dysplasia of the hip. Orthop Surg.
6:95–102. 2014.PubMed/NCBI View
Article : Google Scholar
|
|
36
|
Sugano N: Computer-assisted orthopaedic
surgery and robotic surgery in total hip arthroplasty. Clin Orthop
Surg. 5:1–9. 2013.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Zhang YZ, Chen B, Lu S, Yang Y, Zhao JM,
Liu R, Li YB and Pei GX: Preliminary application of
computer-assisted patient-specific acetabular navigational template
for total hip arthroplasty in adult single development dysplasia of
the hip. Int J Med Robot. 7:469–474. 2011.PubMed/NCBI View
Article : Google Scholar
|
|
38
|
Wu PH, Liu ZT and Zhang YQ: Pre-clinical
application of self-developed computer assisted design/rapid
prototyping and guidance system to assist precise acetabular
component placement: A pilot study. Chin J Orthop Trauma.
19:323–328. 2017.
|
|
39
|
Li P, Tang H, Liu X, Chen Z, Zhang X, Zhou
Y and Jin Z: Reconstruction of severe acetabular bone defects with
porous metal augment in total hip arthroplasty: A finite element
analysis study. Proc Inst Mech Eng H. 236:179–187. 2022.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Kocak S and Sekercioglu T: Experimental
and numerical static failure analyses of total hip replacement
interfaces. Proc Inst Mech Eng H. 233:1183–1195. 2019.PubMed/NCBI View Article : Google Scholar
|