Introduction
Coronavirus disease-19 (COVID-19), caused by severe
acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has altered
the strategies applied in public health and caused numerous
fatalities worldwide (1). For ~3
years it has been evident that the healthcare system has been
adversely confronted by the pandemic crisis and this has suppressed
the therapeutic management of patients in a global perspective,
especially patients managed in the intensive care units (ICUs)
(2).
China, characterized by its distinct strategy to
counter the outbreak prior to November 2022, employed a series of
interventions commencing with the Wuhan lockdown (2020) and
executed a dynamic zero-COVID policy. Additionally, the Chinese
government employed preventive and control measures to stop the
proliferation of SARS-CoV-2, and these measures made them unique in
comparison to other nations (3).
As deregulation contributed to the COVID-19 outbreak, there are
expectations that China makes modifications to its prevention and
control strategies by November 2022. The sudden emergence of the
SARS-CoV-2 in China adversely impacted the country's healthcare
sector, resulting in remarkable disruption and nearly complete
breakdown of the medical infrastructure. Despite hospitals
admitting a considerable number of patients with COVID-19, few
pieces of literature exist on the likelihood of severe illness
connected to several comorbidities that present together with
COVID-19(4). In particular, heart
failure (HF) combined with COVID-19 infection can escalate into a
severe respiratory condition, resulting in a heightened surge in
mortality rates (5,6).
Acute heart failure (ACF) is a common clinical
severe disease that is characterized by ischemia, hypoxia, dyspnea
and other clinical symptoms. Acute pulmonary edema is the main
clinical manifestation, which can progress to cardiogenic shock or
cardiac arrest and can lead to mortality in severe cases (7). COVID-19 exacerbates HF in patients
with preexisting conditions by affecting the cardiovascular system
(8). A significant association has
been found between COVID-19 and ischemic HF (IHF), contributing to
the progression of the disease and increasing mortality in patients
with IHF (9). Bhatt et al
(10) also reported that patients
with cardiovascular disease and HF are more likely to experience
complications from COVID-19 compared with patients without
cardiovascular disease and HF. In India, it was found that there is
no significant difference in outcomes for acute decompensated HF,
and length of hospital stay remained unchanged during the COVID-19
pandemic (11). Hraiech et
al (12) demonstrated that,
during the COVID-19 epidemic in France, acute respiratory distress
syndrome (ARDS) was more likely to develop in undocumented
individuals who entered the neonatal ICU.
Previous studies inferred that infection with
SARS-CoV-2 caused COVID-19, and the major clinical feature and
cause of mortality is respiratory failure (13-15).
Millions of patients globally have experienced acute lung injury
secondary to the COVID-19 epidemic, with ~5% of infected patients
classified as severe (13). This
makes these patients susceptible to complications including ARDS,
HF, cytokine storms, respiratory failure, VTE, sepsis, and the rate
of mortality is >30% (16).
Michalski et al (17) also
revealed that despite COVID-19 being a multi-system disease, it
predominantly damages the lungs where severe cases culminate in
ARDS and respiratory failure.
During the SARS-CoV-2 outbreak, there has been a
notable absence of literature concerning medical characteristics
and epidemiology of HF in China. Therefore, the present study aimed
to ascertain how the SARS-CoV-2 pandemic impacted shared risk
factors and therapeutic approaches employed for individuals with
HF.
Materials and methods
Study design and patients
From November 2022 to April 2023, a single-center
observational study was carried out at the 904th Hospital of Joint
Logistic Support Force (Wuxi, China). Inclusion criteria
incorporated the following: i) Patients diagnosed with HF upon
admission by two intensivists; and ii) patients aged 18-90 years.
The exclusion criteria were as follows: i) Patients with poor
prognosis and low expectation of recovery upon admission; ii)
patients who were pregnant; iii) patients with multiple organ
dysfunction syndrome (MODS); and iv) All patients who underwent
treatments which could affect treatment and prognosis were excluded
(such as antiviral treatment, hemodialysis treatment, immunotherapy
and anti-tumor treatment before admission). Utilizing their
COVID-19 infection status, the patients were classified into HF
with COVID-19 compared against HF only, and no significant
difference in drug treatment was observed between the two
groups.
The present study enrolled 210 individuals with HF
who satisfied the aforementioned specifications, including 117
(55.71%) male and 93 (44.29%) female patients. The mean age was
65.18 years (standard deviation, 8.71 years) in the HF with
COVID-19 group, and 66.43 years (standard deviation, 9.14 years) in
the HF without COVID-19 group. Patient data was collected from The
904th Hospital of Joint Logistic Support Force (Wuxi, China), in
patients with HF of all ages (aged 18-90 years). Information
depicted in pre-existing medical records was analyzed, focusing on
factors that may influence prognosis; for instance, sex, age, BMI,
smoking history, drinking history and past medical history.
Follow-up was conducted via online channels or telephone
communication.
The study procedures were designed and executed to
ensure the safety and efficacy profiles among individuals with HF
after the outbreak of the SARS-CoV-2 virus. The Clinical Research
Ethics Committees at Wuxi Taihu Hospital (Wuxi, China) approved the
study protocol (approval no. THH-YXLL-2022-1101).
Follow-up and outcome evaluation
All patients completed 6 months of follow-up and
survival information was provided for all the patients. Clinical
outcomes, complications, hospital stays and hospitalization costs
were evaluated. The incidence of delirium within 7 days was
evaluated methods as performed in our previous study (18). Delirium was evaluated for a week
from patient admission to hospital, but it was not evaluated if the
patient remained in a coma.
Statistical analysis
The student's unpaired t-test was used for normally
distributed continuous data (mean ± SD), whereas the χ2
test or the χ2 test with continuity correction compared
the categorical data. The Kolmogorov-Smirnov test was used to
assess the normality of data distribution. Calculations for
significant risk ratios or mean differences were performed, with
two-sided 95% confidence intervals (CI) and P<0.05 was
considered to indicate a statistically significant difference.
Statistical analyses were performed using the IBM SPSS Statistics
version 24 for Windows (IBM Corp.).
Results
Baseline patient characteristics:
Overall population
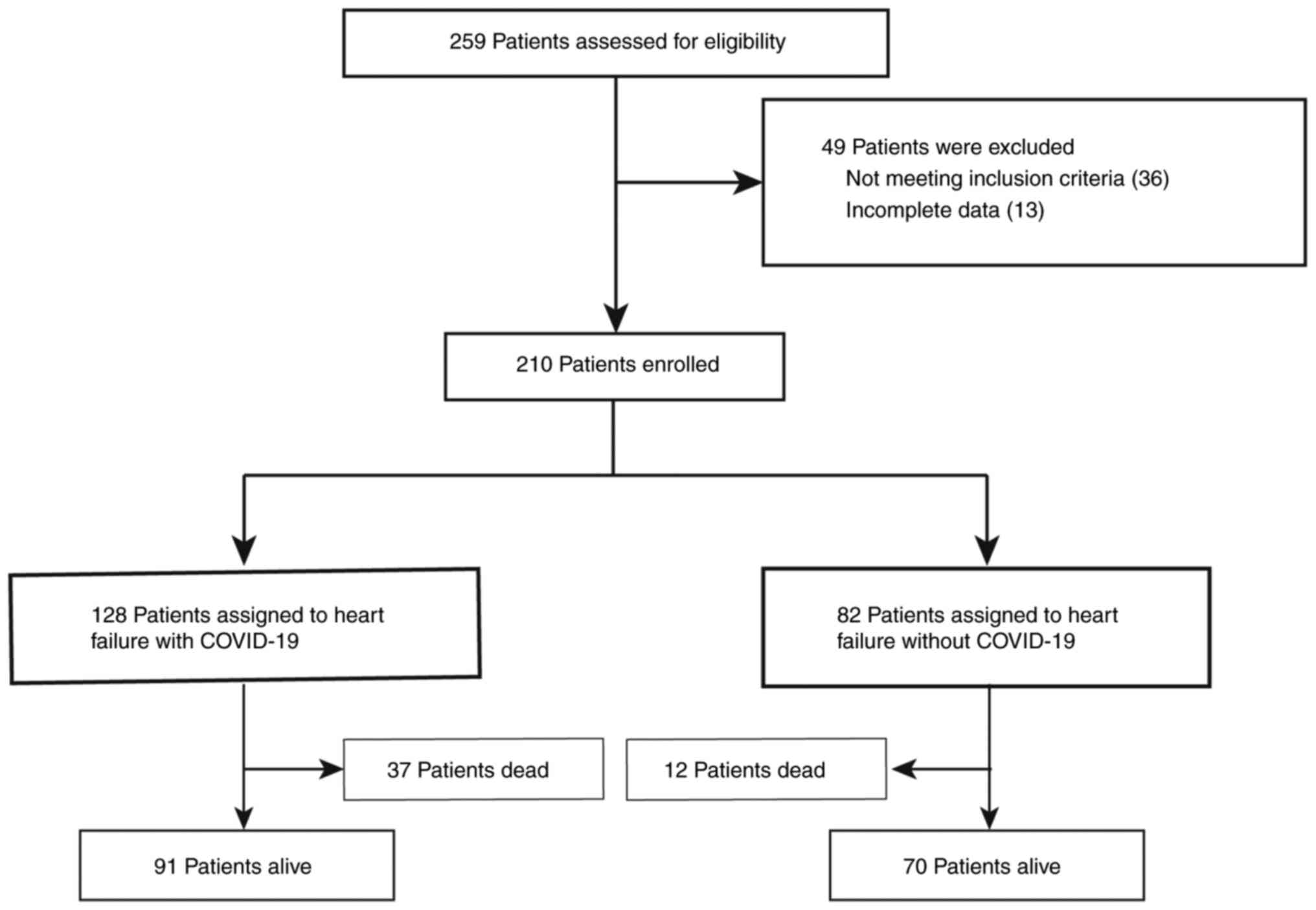
During the study period, a comprehensive assessment
was executed on the 210 individuals with HF. RT-PCR was utilized to
conduct COVID-19 testing on patients. COVID-19 was present in 128
patients who experienced HF, while the remaining 82 patients had HF
but did not have COVID-19 (Fig.
1). COVID-19 was used to separate patients into two groups. The
group with COVID-19 infection and the group without COVID-19 had
average ages of 65.18±8.71 years (range, 43-85 years) and
66.43±9.14 years (range, 46-88 years), respectively. Moreover, no
significant distinctions were present in the baseline
characteristics (Table I) when
comparing HF combined with COVID-19 infection to those without
COVID-19. There was no significant difference in drug treatment
between the two groups.
 | Table IComparison of baseline data at
admission. |
Table I
Comparison of baseline data at
admission.
| Characteristic | COVID-19 (n=128) | Non-COVID-19
(n=82) | P-value |
|---|
| Age, years | 65.18±8.71 | 66.43±9.14 | 0.321 |
| Sex, n (%) | | | 0.845 |
|
Male | 72 (56.25) | 45 (54.88) | |
|
Female | 56 (43.75) | 37 (45.12) | |
| BMI,
kg/cm2 | 23.14±4.88 | 23.85±5.12 | 0.314 |
| Heart rate, bpm | 87.59±12.33 | 88.29±12.84 | 0.693 |
| Respiratory rate,
bpm | 20.06±4.23 | 21.02±4.84 | 0.131 |
| PaO2, mm
Hg | 57.15±8.71 | 56.94±8.67 | 0.865 |
| PaCO2, mm
Hg | 80.29±15.47 | 79.83±14.66 | 0.830 |
| Blood, pH | 7.30±1.63 | 7.33±1.74 | 0.899 |
| MAP, mm Hg | 134.65±22.37 | 136.49±24.18 | 0.574 |
| Admitted BNP,
ng/ml | 972.35±95.39 | 987.42±92.71 | 0.260 |
| Smoking history, n
(%) | | | 0.568 |
|
Yes | 52 (40.63) | 37 (45.12) | |
|
No | 76 (59.37) | 45 (54.88) | |
| Drinking history, n
(%) | | | 0.778 |
|
Yes | 59 (46.09) | 36 (43.90) | |
|
No | 69 (53.91) | 46 (56.10) | |
| Living environment, n
(%) | | | 0.659 |
| Town | 84 (65.63) | 51 (62.20) | |
| Countryside | 44 (34.37) | 31 (37.80) | |
| Past medical history,
n (%) | | | |
|
Hypertension | 89 (69.53) | 53 (64.63) | 0.459 |
|
Hyperlipidemia | 60 (46.88) | 39 (47.56) | 0.923 |
|
Diabetes | 45 (35.16) | 27 (32.93) | 0.740 |
|
Respiratory
system disease | 41 (32.03) | 25 (30.49) | 0.814 |
|
Chronic
kidney disease | 14 (10.94) | 7 (8.54) | 0.572 |
|
Cerebrovascular
disease | 33 (25.78) | 24 (29.27) | 0.579 |
| Etiology of heart
failure, n (%) | | | |
|
Coronary
artery disease | 72 (56.25) | 46 (56.10) | 0.983 |
|
Dilated
cardiomyopathy | 21 (16.41) | 14 (17.07) | 0.899 |
|
Valvular
heart disease | 16 (12.50) | 12 (14.63) | 0.657 |
|
Hypertensive
heart disease | 11 (8.59) | 6 (7.32) | 0.741 |
|
Congenital
heart disease | 5 (3.91) | 3 (3.66) | >0.999 |
|
Myocarditis | 3 (2.34) | 1 (1.22) | >0.999 |
| Severity of heart
failure, n | | | |
|
< III
level | 27 | 19 | |
|
III
level | 46 | 27 | |
|
IV
level | 55 | 36 | |
Clinical outcome between the two
groups
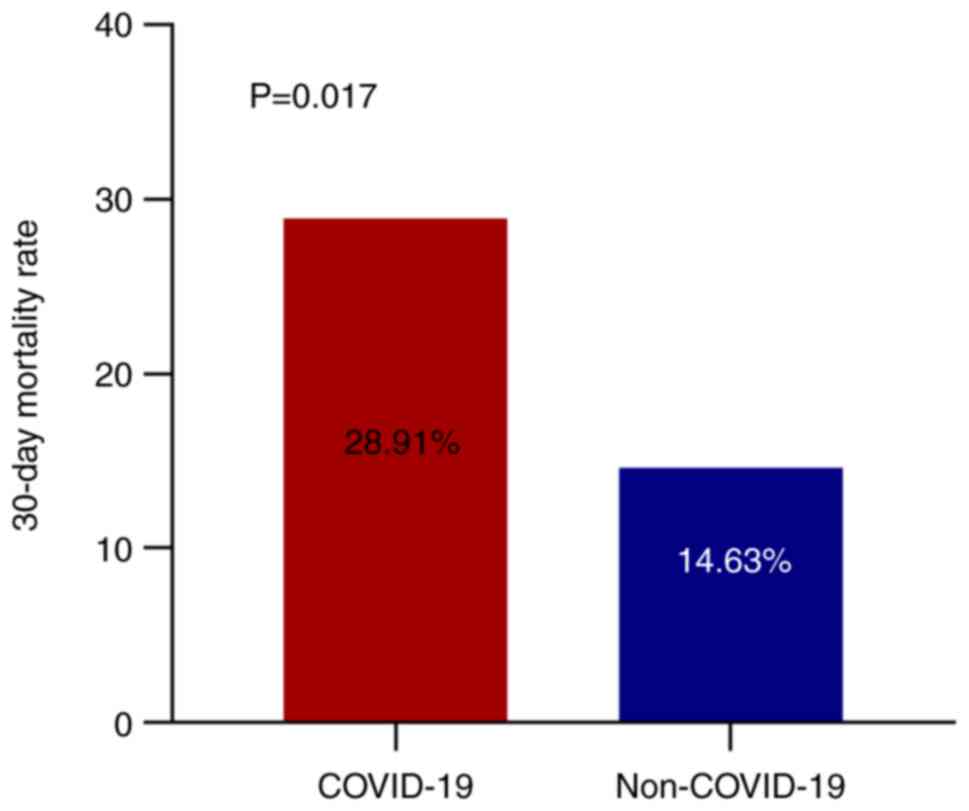
Patients with HF may be predisposed to an elevated
risk of mortality following COVID-19 infection. Therefore the
present study evaluated the 30-day mortality rate between the two
groups. The rate of mortality within 30 days of patient admission
to hospital for the group with HF combined with COVID-19 infection
and the group with HF without COVID-19 infection was 28.91% (37 out
of 128) and 14.63% (12 out of 82), respectively (Fig. 2). The 30-day mortality rate was
significantly increased in the group with COVID-19 infection
compared with the group without COVID-19 (P=0.017; Fig. 2). A higher total 30-day mortality
was linked to the combination of COVID-19 and HF regarding clinical
outcomes.
Hospital stays and hospitalization
costs
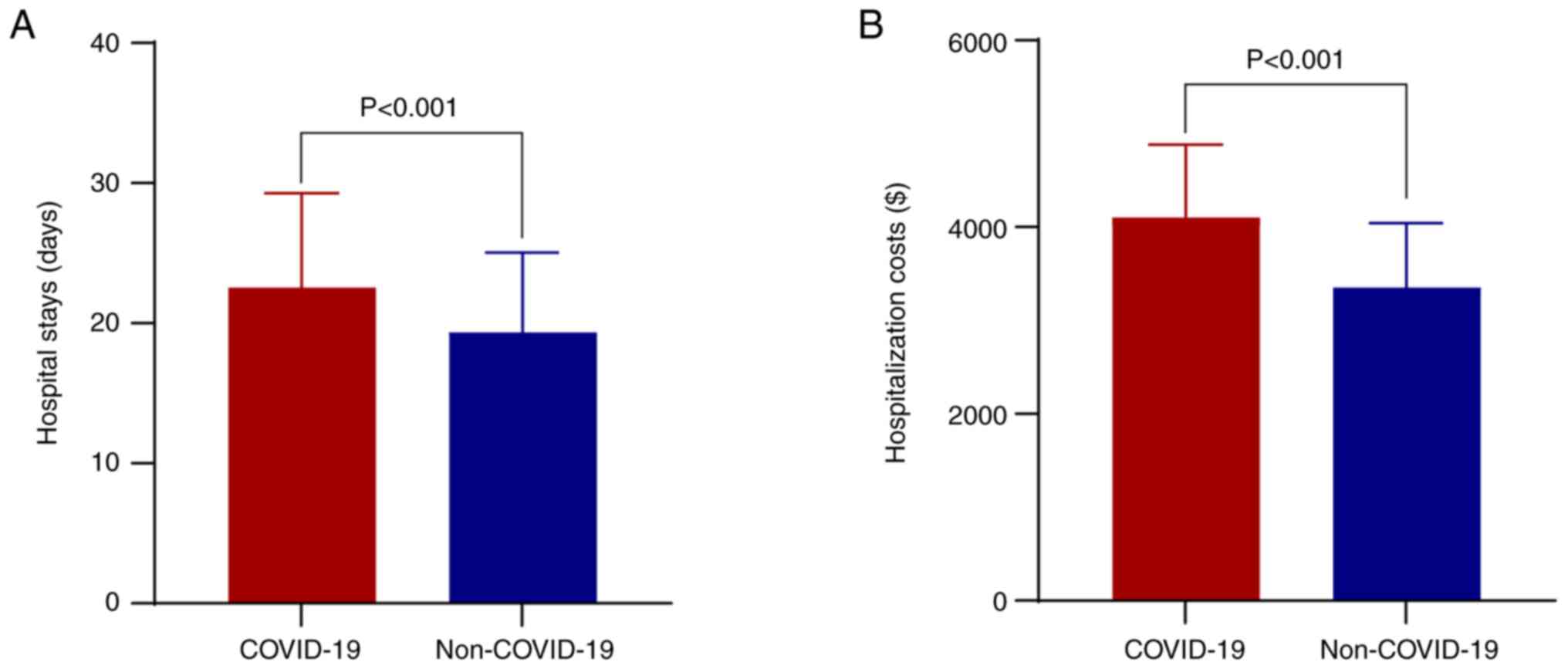
Patients with HF combined with COVID-19 infection
had an average length of hospitalization of 22.54±6.73 days. On the
other hand, patients without COVID-19 had an average stay of
19.35±5.69 days, inferring a statistically substantial disparity
(P<0.001; Fig. 3A). In terms of
hospitalization costs, the costs for COVID-19-infected and
non-COVID-19-infected patients were 4,100$ and 3,350$,
respectively, inferring a significantly increased cost for patients
with COVID-19 (P<0.001; Fig.
3B). Therefore, the hospital costs and stays for patients with
HF have been substantially elevated due to the COVID-19
infection.
Complications between the two
groups
While providing treatment for HF, the present study
determined a greater incidence of complications in patients who
were diagnosed with COVID-19. The incidence of pneumonia (76.56 vs.
35.37%; P=1.0x10-4; Table
II), respiratory failure (47.66 vs. 24.39%; P=0.001; Table II), pulmonary embolism (8.59 vs.
2.44%; P=0.031; Table II), deep
vein thrombosis (DVT; 30.47 vs. 14.63%; P=0.009; Table II), 7 days delirium (60.16 vs.
45.12%; P=0.033; Table II),
multiple organ dysfunction syndrome (MODS; 32.81 vs. 18.29%;
P=0.021; Table II) and
neurological deficits (30.47 vs. 17.07%; P=0.029; Table II) were markedly significantly
among COVID-19-infected patients compared with those not infected
with COVID-19. The two groups had no substantial disparities in
renal failure (21.88 vs. 13.41%; P=0.147), abnormal liver enzymes
(41.41 vs. 34.15%; P=0.292), diarrhea (26.56 vs. 18.29%; P=0.167),
vomiting (15.63 vs. 10.98%; P=0.341) and electrolyte imbalance
(71.88 vs. 64.63%; P=0.268). Table
II displays the complications results.
 | Table IIComparison of complications between
two groups. |
Table II
Comparison of complications between
two groups.
| | COVID-19
(n=128) | Non-COVID-19
(n=82) | P-value |
|---|
| Pneumonia, n
(%) | 98 (76.56) | 29 (35.37) | <0.001 |
| Respiratory
failure, n (%) | 61 (47.66) | 20 (24.39) | 0.001 |
| Pulmonary embolism,
n (%) | 11 (8.59) | 2 (2.44) | 0.031 |
| Deep vein
thrombosis, n (%) | 39 (30.47) | 12 (14.63) | 0.009 |
| 7 days delirium, n
(%) | 77 (60.16) | 37 (45.12) | 0.033 |
| Multiple organ
dysfunction syndrome, n (%) | 42 (32.81) | 15 (18.29) | 0.021 |
| Renal failure, n
(%) | 28 (21.88) | 11 (13.41) | 0.147 |
| Neurological
deficit, n (%) | 39 (30.47) | 14 (17.07) | 0.029 |
| Abnormal liver
enzymes, n (%) | 53 (41.41) | 28 (34.15) | 0.292 |
| Diarrhea, n
(%) | 34 (26.56) | 15 (18.29) | 0.167 |
| Vomiting, n
(%) | 20 (15.63) | 9 (10.98) | 0.341 |
| Electrolyte
imbalance | 92 (71.88) | 53 (64.63) | 0.268 |
ICU stays and mechanical
ventilation
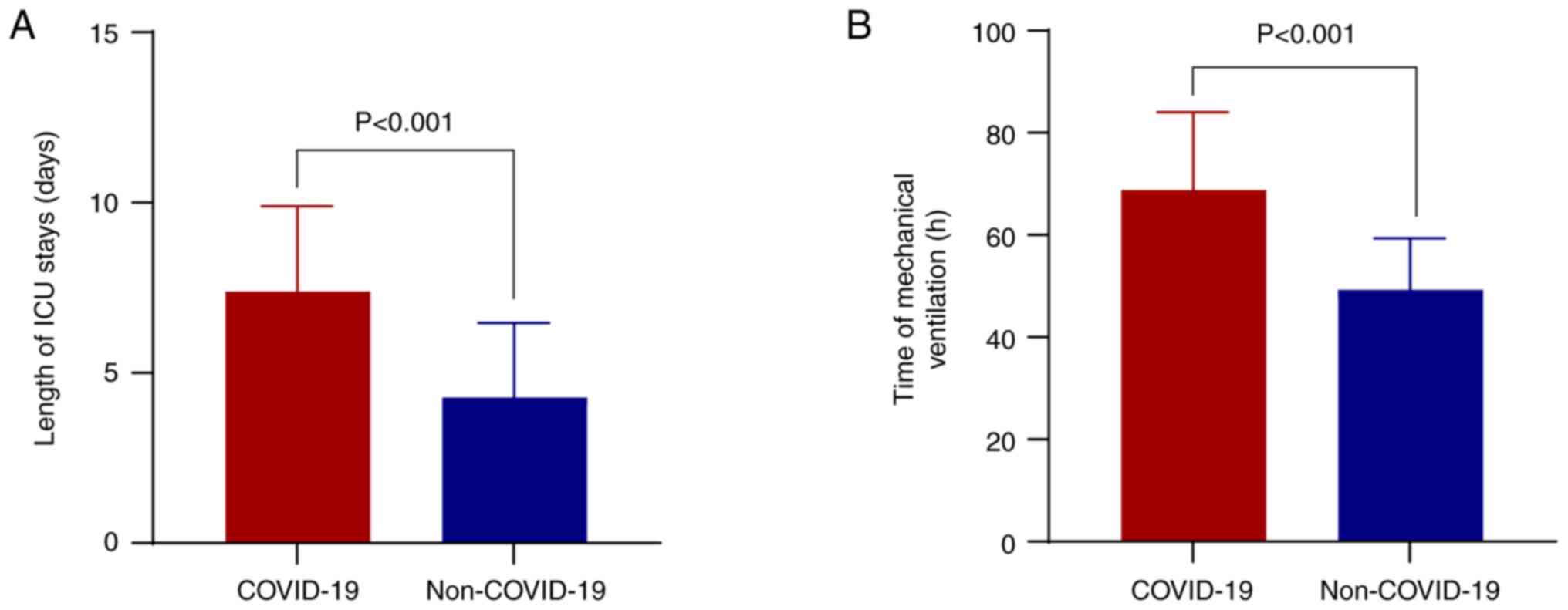
Patients with AHF are critically ill, and most need
to be treated in the ICU and receive mechanical ventilation. The
present study revealed that the mean length of ICU stays was
increased significantly in the patients with HF and COVID-19 group
compared with patients without COVID-19 (7.39±2.51 vs. 4.28±2.19,
P<0.001; Fig. 4A).
Additionally, the present study revealed that the time of
mechanical ventilation was longer in the patients with HF and
COVID-19 group compared with the patients without COVID-19
(68.77±15.24 vs. 49.28±10.09; P<0.001; Fig. 4B).
Discussion
The present study was executed at a single center
and evaluated the impact of the SARS-CoV-2 pandemic on common risk
factors and therapeutic management for patients with HF. Between
the two groups, the current findings of the present study affirm
that no remarkable distinction in the characteristics of patients
on admission. The combination of COVID-19 and HF was linked to an
increased in the overall rate of mortality within 30 days. The
costs as well as the length of hospital stays were also increased
by COVID-19-related HF. COVID-19 along with HF increased the risk
of hospitalization complications, including pneumonia, respiratory
failure, pulmonary embolism, DVT, delirium, HF, neurological
deficits and MODS.
Healthcare systems and practitioners have incurred
global repercussions due to the COVID-19 pandemic. Following
December 2022, the termination of the zero-COVID strategy led to an
escalation in the transmission of COVID-19. A number of patients
admitted to the hospital were detected to have contracted COVID-19
before or after admission (4).
Overall, there were no discernable disparities in baseline
characteristics between HF and COVID-19 infection and those
without. The present study ascertained that the concurrence of
COVID-19 and HF culminated in worsened clinical results,
complications, markedly longer hospital stays and increased costs
for patients with HF. In comparison to patients without pulmonary
embolism, patients with COVID-19 comorbid with pulmonary embolism
exhibit a greater 30-day mortality rate as per Tilliridou et
al (19). The synergy of
COVID-19 infection, multiple traumas and positive CT results
elevate the risks of developing pulmonary complications (20). Driessen et al (21) demonstrated that the rate of
mortality throughout the SARS-CoV-2 pandemic was higher compared
with the previous period. In this current investigation, a greater
number of patients developed HF infected with COVID-19, and the
most common cause of mortality was multiple organ failure from
severe lung infections. Moreover, Htay et al (22) revealed a significant increase in
the rate of mortality among patients with COVID-19 undergoing
peritoneal dialysis during the COVID-19 outbreak.
The present study revealed that the total 30-day
mortality was higher compared with that in a previous study
(11); the main reason for this
may be that our hospital is a regional treatment center for
critically ill patients, and the patients treated had more serious
stages of disease. A high total 30-day mortality was linked to the
combination of COVID-19 and HF in the perspective of clinical
outcomes in the present study. On the one hand, the COVID-19
pandemic strains medical resources, and when there is a shortage of
beds and medicines this results in patients with HF not being able
to get effective, rapid treatment. On the other hand, COVID-19
causes many complications in the cardiovascular system and systemic
system, which worsens the disease (23). Additionally, the present study also
revealed that COVID-19 could lead to more complications. Fatuyi
et al (24) reported that
when acute decompensated HF coexisted with COVID-19 infection this
was associated with a higher in-hospital mortality rate.
Clinically, patients with HF along with COVID-19 infection need
high attention due to higher mortality rates and complications.
To the best of our knowledge, the present study was
the first to report the clinical data of HF in patients with
COVID-19 infection and explore how the pandemic has impacted the
common risk factors and therapeutic approaches for patients with
HF. Currently, there is a lack of relevant experience in diagnosis
and treatment, the present preliminary results provide a basis for
future research on large samples. Additionally, it is not yet clear
whether COVID-19 and similar infectious diseases will cause another
pandemic again. Therefore, HF along with COVID-19 infection
requires high attention.
The present study had two limitations in the study
design. Firstly, the sample size was small and this necessitates
the conduction of extensive studies in the future to ascertain the
impact of the SARS-CoV-2 outbreak on the common risk factors and
the therapeutic approaches for individuals with HF. The other
limitation is that it is difficult to ascertain a causal
relationship utilizing the obtained data because of the nature of
our cross-sectional as well as retrospective study. As a result,
future research focusing on the impact of COVID-19 on respiratory
failure should thus adopt a prospective, longitudinal design. This
will facilitate the detection of risk factors in conjunction with
the assessment of causal relationships between variables. Moreover,
the present study centers on the immediate negative outcomes as
well as the effectiveness of COVID-19 infection in patients with
HF, stressing the need for long-term findings. Therefore, it is
imperative to scrutinize larger and additional groups of patients
with HF as a result of COVID-19.
In conclusion, patients with COVID-19 and HF
demonstrated heightened mortality rates within 30 days, higher
hospitalization expenses, extended hospital stays and a greater
possibility of complications occurring during their
hospitalization. The results of the present study will provide a
reference for future patients with HF along with COVID-19 and need
a larger sample study to clarify the long-term prognosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
XL and TL contributed to the conception and design
of the study. XL, TL and RW conducted the data collection and the
statistical analysis. XL wrote the first draft of the manuscript.
RW revised the manuscript, managed the project, coordinated the
study and gave final approval for the version to be published. XL,
TL and RW confirm the authenticity of all the raw data. All of the
authors contributed to manuscript revision and read and approved
the final version of the manuscript.
Ethics approval and consent to
participate
The registration number THH-IPR-20221101 (date,
01/Nov 2022) was obtained with protocol approval from the Clinical
Research Ethics Committees of the Wuxi Taihu Hospital (approval no.
THH-YXLL-2022-1101). Prior to enrollment in the study, all
participants (or their legal representatives) provided informed
written consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yasin AL, Aydin SG, Sümbül B, Koral L,
Şimşek M, Geredeli Ç, Öztürk A, Perkin P, Demirtaş D, Erdemoglu E,
et al: Efficacy and safety profile of COVID-19 vaccine in cancer
patients: A prospective, multicenter cohort study. Future Oncol.
18:1235–1244. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Villarreal-Zegarra D, Bellido-Boza L,
Erazo A, Pariona-Cárdenas M and Valdivia-Miranda P: Impact of the
COVID-19 pandemic on the services provided by the Peruvian health
system: An analysis of people with chronic diseases. Sci Rep.
14(3664)2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Pan Y, Wang L, Feng Z, Xu H, Li F, Shen Y,
Zhang D, Liu WJ, Gao GF and Wang Q: Characterisation of SARS-CoV-2
variants in Beijing during 2022: An epidemiological and
phylogenetic analysis. Lancet. 401:664–672. 2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hon C, Liang J, Chen R, Lin Z, Wang Y, He
W, Liu R, Sun J, Li Q, Liang L, et al: Temporary impact on medical
system and effectiveness of mitigation strategies after COVID-19
policy adjustment in China: A modeling study. Front Public Health.
11(1259084)2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bime C, Carr GE, Pu J, Kou S, Wang Y and
Simons M: Delayed intubation associated with in-hospital mortality
in patients with COVID-19 respiratory failure who fail heated and
humified high flow nasal canula. BMC Anesthesiol.
23(234)2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Huang S, Vieillard-Baron A, Evrard B, Prat
G, Chew MS, Balik M, Clau-Terré F, De Backer D, Mekontso Dessap A,
Orde S, et al: Echocardiography phenotypes of right ventricular
involvement in COVID-19 ARDS patients and ICU mortality: Post-hoc
(exploratory) analysis of repeated data from the ECHO-COVID study.
Intensive Care Med. 49:946–956. 2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Arrigo M, Jessup M, Mullens W, Reza N,
Shah AM, Sliwa K and Mebazaa A: Acute heart failure. Nat Rev Dis
Primers. 6(16)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Olszanecka A, Wojciechowska W, Bednarek A,
Kusak P, Wizner B, Terlecki M, Stolarz-Skrzypek K, Klocek M, Drożdż
T, Sładek K, et al: Serial echocardiographic evaluation of COVID-19
patients without prior history of structural heart disease: A
1-year follow-up CRACoV-HHS study. Front Cardiovasc Med.
10(1230669)2023.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wu G, Zhou J, Ren H, Qin Y, Qian D, Hu Q,
Xu P, Yu T, Ma H, Chen H, et al: Unraveling the molecular crosstalk
and immune landscape between COVID-19 infections and ischemic heart
failure comorbidity: New insights into diagnostic biomarkers and
therapeutic approaches. Cell Signal. 112(110909)2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bhatt AS, Jering KS, Vaduganathan M,
Claggett BL, Cunningham JW, Rosenthal N, Signorovitch J, Thune JJ,
Vardeny O and Solomon SD: Clinical outcomes in patients with heart
failure hospitalized with COVID-19. JACC Heart Fail. 9:65–73.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Jayagopal B, Ramakrishnan S, Mohanan PP,
Jabir A, Venugopal K, Das MK, Santhosh K, Syam N, Ezhilan J,
Agarwal R, et al: Impact of COVID-19 on heart failure
hospitalization and outcome in India-A cardiological society of
India study (CSI-HF in COVID 19 times study-‘The COVID C-HF
study’). Indian Heart J. 75:370–375. 2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hraiech S, Pauly V, Orleans V, Auquier P,
Azoulay E, Roch A, Boyer L and Papazian L: COVID-19 among
undocumented migrants admitted to French intensive care units
during the 2020-2021 period: A retrospective nationwide study. Ann
Intensive Care. 13(99)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lu S, Huang X, Liu R, Lan Y, Lei Y, Zeng
F, Tang X and He H: Comparison of COVID-19 induced respiratory
failure and typical ARDS: Similarities and differences. Front Med
(Lausanne). 9(829771)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Liu Q, Nair R, Huang R, Zhu H, Anderson A,
Belen O, Tran V, Chiu R, Higgins K, Chen J, et al: Using machine
learning to determine a suitable patient population for anakinra
for the treatment of COVID-19 under the emergency use
authorization. Clin Pharmacol Ther: Feb 13, 2024 (Epub ahead of
print).
|
|
15
|
Phillips T, Mughrabi A, Garcia LJ, El
Mouhayyar C, Hattar L, Tighiouart H, Moraco AH, Nader C and Jaber
BL: Association of body mass index with multiple organ failure in
hospitalized patients with COVID-19: A multicenter retrospective
cohort study. J Intensive Care Med: Feb 11, 2024 (Epub ahead of
print).
|
|
16
|
King CS, Mannem H, Kukreja J, Aryal S,
Tang D, Singer JP, Bharat A, Behr J and Nathan SD: Lung
transplantation for patients with COVID-19. Chest. 161:169–178.
2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Michalski JE, Kurche JS and Schwartz DA:
From ARDS to pulmonary fibrosis: The next phase of the COVID-19
pandemic? Transl Res. 241:13–24. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yin B, Ye T, Liu X, Wan R, Gu L and Zong
G: Effects of melatonin for delirium in elderly acute heart failure
patients: A randomized, single-center, double-blind, and
placebo-controlled trial. Heart Surg Forum. 25:E037–E041.
2022.PubMed/NCBI View
Article : Google Scholar
|
|
19
|
Tilliridou V, Kirkbride R, Dickinson R,
Tiernan J, Yong GL, van Beek EJ, Murchison JT and Williams MC:
Pulmonary embolism severity before and during the COVID-19
pandemic. Br J Radiol. 94(20210264)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Scheurer F, Halvachizadeh S, Berk T, Pape
HC and Pfeifer R: Chest CT Findings and SARS-CoV-2 infection in
trauma patients-is there a prediction towards higher complication
rates? J Clin Med. 11(6401)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Driessen MLS, Sturms LM, Bloemers FW, Duis
HJT, Edwards MJR, den Hartog D, Kuipers EJ, Leenhouts PA, Poeze M,
Schipper IB, et al: The Detrimental Impact of the COVID-19 pandemic
on major trauma outcomes in the Netherlands: A comprehensive
nationwide study. Ann Surg. 275:252–258. 2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Htay H, Foo MWY, Jayaballa M, Johnson DW,
Oei EL, Tan BH, Wang W, Wu SY and Tan CS: Clinical features,
management and outcomes of peritoneal dialysis patients during
Delta and Omicron waves of COVID-19 infections. Int Urol Nephrol.
55:2075–2081. 2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ren X, Chen B, Hong Y, Liu W, Jiang Q,
Yang J, Qian Q and Jiang C: The challenges in colorectal cancer
management during COVID-19 epidemic. Ann Transl Med.
8(498)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Fatuyi M, Amoah J, Egbuchiem H, Antia A,
Akinti S, Mararenko A, Alzamara M and Bhatia A: Impact of COVID-19
infection on clinical outcomes among patients with acute
decompensated heart failure: A nationwide analysis. Curr Probl
Cardiol. 48(101908)2023.PubMed/NCBI View Article : Google Scholar
|