Introduction
Lumbar disc herniation (LDH) refers to a series of
syndromes characterized by low back pain and lower limb radiation
pain induced by the stimulation or compression of nerves due to
degeneration or injury of the lumbar intervertebral disc, leading
to rupture of the fibrous ring and protrusion of the nucleus
pulposus (1,2). LDH mainly occurs at L4-5 and L5-S1
and is mainly observed in middle-aged and elderly individuals, with
a male predominance (3). LDH can
limit mobility and the ability to perform physical activities, and
cause disability (4), thereby
reducing the quality of life of patients and increasing medical
costs. Although conservative treatment is the first choice for
treating LDH, surgery is necessary for severe LDH to achieve good
clinical outcomes (5,6).
With the continuous development of minimally
invasive spinal technology, percutaneous endoscopic lumbar
discectomy (PELD) is the main method of surgical treatment for LDH
(7). PELD has numerous advantages,
such as minimal trauma, less bleeding, a clear surgical field,
relatively low surgical costs and high patient satisfaction
(8). In addition, PELD can be
performed under local anaesthesia, which may lead to the
acquisition of knowledge regarding a patient's neurological and
vascular injuries during surgery (9). Whether from a medical or patient
perspective, the use of PELD to treat LDH has numerous technical
advantages. However, the widespread application of endoscopic
technology has led to post-PELD complications, including recurrent
LDH (rLDH), receiving increased attention (10). According to the literature, 2-25%
of patients who undergo PELD experience rLDH after surgery
(10-12).
Surgical intervention is necessary for patients with rLDH who have
been clearly diagnosed and have not yet achieved remission after
conservative treatment. However, scar tissue after the initial
surgery increases the difficulty of repeated discectomy and
increases the risk of dural tears or nerve damage (13,14).
In addition, removing the posterior structure during reoperation
may increase the risk of lumbar segmental instability (15,16).
There is no doubt that both reoperation and the clinical symptoms
associated with rLDH have a significant negative impact on the
psychological burden and economic pressure of patients.
PELD is a common surgical method for the treatment
of LDH, and rLDH is a possible serious complication. In this
context, identifying the risk factors for rLDH after PELD has
important clinical value for formulating appropriate surgical
protocols and evaluating postoperative efficacy. However, there is
a lack of high-level evidence regarding the risk factors for rLDH
after PELD. To fill this gap, a meta-analysis was performed to
evaluate and identify the risk factors for rLDH after PELD. The
conclusions of this study are intended to provide a theoretical
basis for the clinical prevention and reduction of postoperative
rLDH after PELD.
Materials and methods
Data sources and retrieval
strategies
The design and implementation of the present study
followed the Preferred Reporting Items for Systematic Reviews and
Meta-Analyses guidelines (17).
Three databases, including PubMed (www.pubmed.ncbi.nlm.nih.gov), Cochrane Library
(www.cochranelibrary.com) and Embase
(www.embase.com), were searched to identify
studies that examined risk factors for rLDH after PELD. The
databases were searched from inception to March 30th, 2023.
Furthermore, the reference lists of the included studies were
manually searched to obtain additional eligible studies. The search
strategy included a combination of MeSH terms and free words. The
key words included ‘recurrent lumbar disc herniation’, ‘rLDH’,
‘reoperation’, ‘repeat discectomy’, ‘PELD’, ‘percutaneous
endoscopic lumbar discectomy’, ‘percutaneous transforaminal
endoscopic discectomy’, and ‘Yeung endoscopic spine system’. The
details of the search strategies for each database are provided in
Appendix S1.
Inclusion and exclusion criteria
The inclusion criteria were as follows: i) Study
participants of any age, sex, ethnicity or region, including
patients in need to be diagnosed with LDH and treated with PLED;
ii) the research topic was risk factors for rLDH and complete data
on grouping comparison of rLDH and non-rLDH were available in the
literature; iii) due to the fact that the present study is a
secondary literature analysis, the study type was limited to cohort
and case-control studies based on the existing literature.
Ostensibly, rLDH typically occurs after surgery. Due to ethical
considerations and implementation difficulties, randomized
controlled trials may not be the most appropriate method for
studying risk factors, and thus, the present quantitative review
only included cohort studies and case-control studies; iv) the
included literature was required to contain reports of at least one
risk factor; v) the outcome measurement data were required to be
expressed as the frequency (%) or mean ± standard deviation in
order to help reduce statistical heterogeneity. There were no
restrictions regarding the language of the publications.
The exclusion criteria were as follows: i) Duplicate
literature, case reports and animal experiments; ii) obvious
statistical errors in the literature; iii) repeated publications of
the same study population; and iv) the full text cannot be
obtained.
Data extraction. Two researchers (GL, BS)
independently extracted data from the included literature and
cross-checked them. Disagreements were resolved through discussion
or consultation with the corresponding author. The process of
literature selection included selecting the literature that met the
research purpose by reading the titles and abstracts, then reading
the full texts of the literature according to the inclusion and
exclusion criteria, and finally selecting the literature that met
the research purpose. The following data were extracted: First
author, publication time, research design type, sample size,
follow-up time and risk factors.
Literature quality evaluation
The quality of the included studies was evaluated by
two researchers using the Newcastle-Ottawa scale (NOS) (18). The NOS consists of three
components, including study subject selection (4 points),
intergroup comparability (2 points) and outcome or exposure factor
evaluation (3 points), with a total score of 9 points. Scores of 0
to 3, 4 to 6 and 7 to 9 were considered to indicate low-, moderate-
and high-quality research, respectively.
Data analysis
RevMan 5.3 software (The Cochrane Collaboration) was
used for data analysis. For categorical and continuous variables,
odds ratios (ORs) and weighted mean differences (WMDs) were used as
effect size measures, respectively, and point estimates and 95%
confidence intervals (CIs) for each effect size measure were
calculated. The random-effects model was used for all
meta-analyses. The test level for meta-analysis was set to α=0.05.
Sensitivity analysis was performed by comparing the result
consistency between the fixedeffects and randomeffects models and
eliminating studies with greater impact. And the method exclusion
of one study at a time and re-performing the meta-analysis was also
performed. A funnel plot was constructed to assess whether there
was evidence of publication bias. In addition, each outcome was
required to be examined by at least 3 studies to be considered for
pooled data analysis.
Results
Literature search results
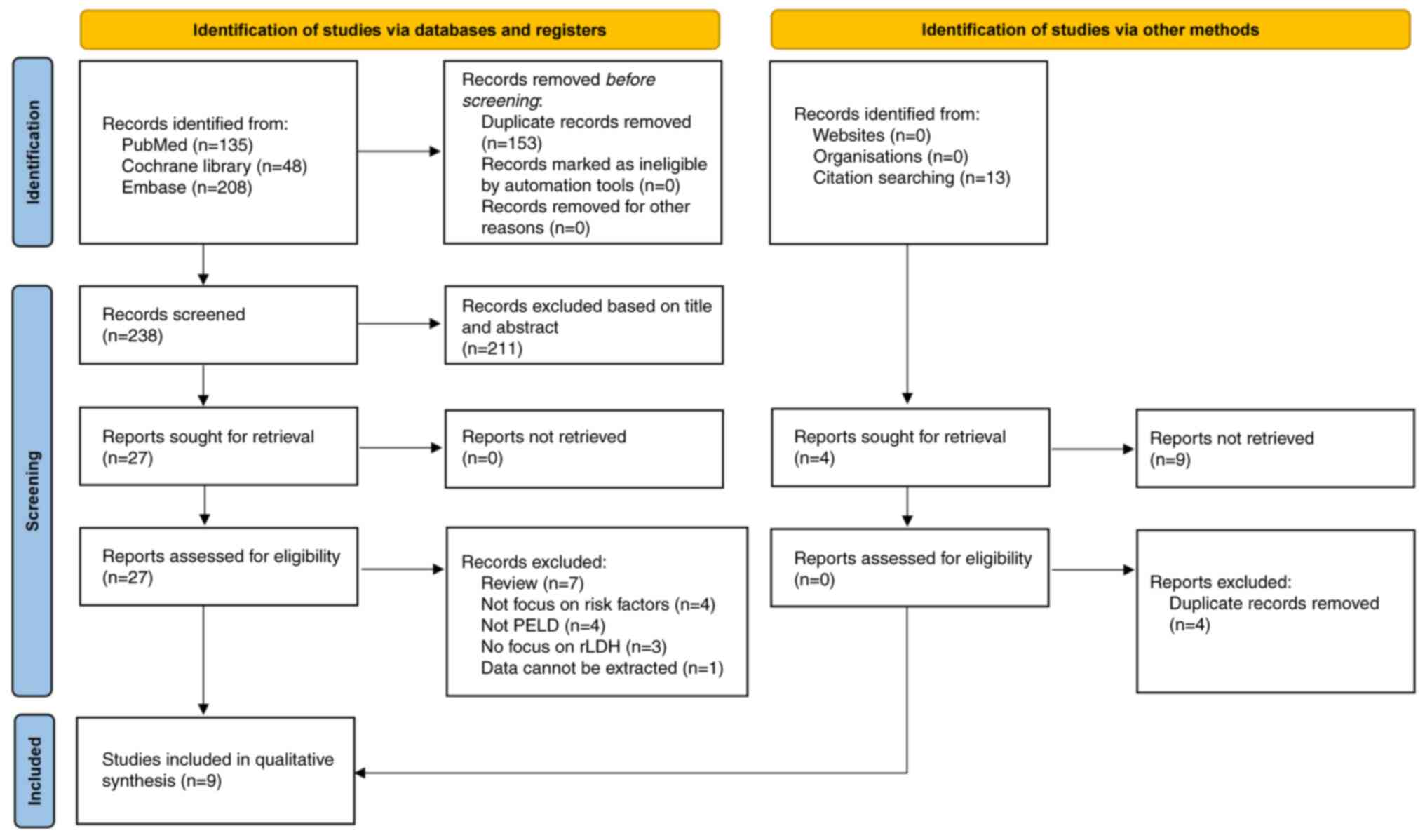
Based on the search strategy of the present study, a
total of 391 relevant documents were retrieved. After removing
duplicate publications and reading the titles and abstracts of the
studies, 27 articles remained for full-text screening. Referring to
the inclusion criteria of the present study and after reading the
full texts, 9 case-control studies were ultimately included in the
present meta-analysis (19-27).
The specific details of the study selection process are presented
in Fig. 1.
Basic characteristics of the included
studies
A total of 9 case-control studies were included in
the present study and they were published between 2020 and 2023,
indicating that research on rLDH after PELD has received extensive
attention from researchers in recent years. A total of 5,446
patients who underwent PELD were included in this meta-analysis,
with 560 rLDH patients (343 males and 217 females) and 4,886
non-rLDH patients (2,811 males and 2,075 females). The weighted
mean age was 50.75 in the rLDH group and 44.53 in the non-rLDH
group. The follow-up period ranged from 6-48 months. The operative
segments of LDH were mainly L4/5 and L5/S1. The basic
characteristics of the nine included studies are presented in
Table I.
 | Table ICharacteristics of the included
studies. |
Table I
Characteristics of the included
studies.
| | Sample size (M/F),
n | Mean age,years | Level of herniated
disk, n (L2/L3,L3/L4,L4/5,L5/S1) | Type of herniation,
n (central/paracentral/lateral or extreme lateral) | |
|---|
| First author,
year | Design | RLDH | Non-RLDH | RLDH | Non-RLDH | RLDH | Non-RLDH | RLDH | Non-RLDH | Follow-up
(months) | (Refs.) |
|---|
| He et al,
2023 | Case-control
study | 63 (45/18) | 627 (410/217) | 51.49 | 42.87 | 0/0/37/26 | 0/0/370/257 | NR | NR | 24 | (19) |
| Jia et al,
2021 | Case-control
study | 32 (18/14) | 320 (212/108) | NR | NR | 0/2/18/12 | 0/12/165/143 | 1/31/0 | 3/177/140 | 6 | (20) |
| Kong et al,
2020 | Case-control
study | 46 (22/24) | 608 (333/275) | 54.4 | 44.9 | NR | NR | 31/13/20 | 165/212/231 | 28 | (21) |
| Li et al,
2023 | Case-control
study | 56 (30/26) | 589 (296/293) | 51.82 | 48.32 | 4/6/29/17 | 6/22/412/149 | 4/26/11 | 50/360/179 | 24 | (22) |
| Ren et al,
2023 | Case-control
study | 130 (80/50) | 1059 (640/419) | 46.62 | 44.2 | NR | NR | NR | NR | 38 | (23) |
| Shi et al,
2021 | Case-control
study | 68 (47/21) | 136 (94/42) | 46.21 | 47.36 | 0/0/41/27 | 0/0/82/54 | NR | NR | 24 | (24) |
| Wang et al,
2022 | Case-control
study | 57 (39/18) | 885 (462/423) | 56.7 | 41.2 | 0/0/30/27 | 3/18/405/459 | 6/42/9 | 69/732/84 | 24 | (25) |
| Yu et al,
2020 | Case-control
study | 46 (25/21) | 438 (229/209) | 52.98 | 47.74 | NR | NR | 13/27/6 | 100/237/101 | 12 to 48 | (26) |
| Zhao et al,
2021 | Case-control
study | 62 (37/25) | 224 (135/89) | 52.1 | 44.9 | NR | NR | NR | NR | 24 | (27) |
Results of the literature quality
evaluation
The NOS scores of the nine included studies
(19-27)
are shown in Table II. The NOS
scores ranged from 7-8, which indicates that the methodological
quality of all studies included in the present study is high.
 | Table IINewcastle-Ottawa scale for risk of
bias assessment of studies included in the meta-analysis. |
Table II
Newcastle-Ottawa scale for risk of
bias assessment of studies included in the meta-analysis.
| | Selection | | Outcome | |
|---|
| First author,
year | Representativeness
of exposed cohort | Selection of
nonexposed | Ascertainment of
exposure | Outcome not present
at start | Comparability | Assessment of
outcome | Adequate follow-up
length | Adequacy of
follow-up | Overall | (Refs.) |
|---|
| He et al,
2023 | - | * | * | * | ** | * | * | * | 8 | (19) |
| Jia et al,
2021 | - | * | * | * | ** | * | * | - | 7 | (20) |
| Kong et al,
2020 | - | * | * | * | ** | - | * | * | 7 | (21) |
| Li et al,
2023 | - | * | * | * | ** | * | * | * | 8 | (22) |
| Ren et al,
2023 | - | * | * | * | ** | - | * | * | 7 | (23) |
| Shi et al,
2021 | - | * | * | * | ** | * | * | * | 7 | (24) |
| Wang et al,
2022 | - | * | * | * | ** | * | * | * | 8 | (25) |
| Yu et al,
2020 | - | * | * | * | ** | * | * | * | 8 | (26) |
| Zhao et al,
2021 | - | * | * | * | ** | - | * | * | 7 | (27) |
Meta-analysis. Sociodemographic and
anthropometry factors
A total of 9 related factors were analysed (Table III) and the corresponding forest
maps of sociodemographic and anthropometry factors are shown in
Fig. S1, Fig. S2, Fig. S3, Fig. S4, Fig. S5, Fig. S6, Fig. S7, Fig. S8 and Fig. S9. The meta-analysis found that age
and body mass index (BMI) are both significant risk factors for
rLDH. Sex, symptom duration, smoking, drinking, DM and hypertension
were not risk factors for rLDH (all P>0.05). A total of 8
studies (19,21-27)
reported an association between age and rLDH, and there was
heterogeneity among the studies (I2=93%). The
random-effects model was used to perform meta-analysis and the
results showed that higher patient age was associated with a
greater risk of rLDH after PELD (WMD=6.49, 95% CI: 2.52 to 10.46,
P=0.001).
 | Table IIIMeta-analysis of the risk
factors. |
Table III
Meta-analysis of the risk
factors.
| A, Sociodemographic
and anthropometry factors |
|---|
| Factor | Studies, n | OR or WMD | 95% CI | P-value |
I2,% | Analysis model |
|---|
| Age, years | 8 | 6.49 | 2.52-10.46 | 0.001 | 93 | IV, random |
| Male sex | 9 | 1.08 | 0.90-1.30 | 0.410 | 2 | M-H, random |
| Female sex | 9 | 0.92 | 0.77-1.11 | 0.410 | 2 | M-H, random |
| BMI,
kg/m2 | 8 | 1.16 | 0.69-1.62 | <0.001 | 69 | IV, random |
| Symptom duration,
months | 4 | 1.71 | -0.18-3.59 | 0.080 | 97 | IV, random |
| Smoking (yes vs.
no) | 8 | 1.43 | 0.95-2.14 | 0.090 | 69 | M-H, random |
| Drinking (yes vs.
no) | 5 | 1.13 | 0.83-1.53 | 0.450 | 0 | M-H, random |
| DM (yes vs.
no) | 7 | 1.22 | 0.85-1.74 | 0.280 | 5 | M-H, random |
| Hypertension (yes
vs. no) | 4 | 1.00 | 0.69-1.47 | 0.990 | 1 | M-H, random |
| B, Clinical and
imaging factors |
| Factor | Studies, n | OR or WMD | 95% CI | P-value |
I2,% | Analysis model |
| Operation time,
min | 3 | -0.19 | -5.54-5.15 | 0.940 | 59 | IV, random |
| Modic change (yes
vs. no) | 7 | 2.48 | 1.54-3.99 | <0.001 | 73 | M-H, random |
| Pfirrmann grade
≥4 | 3 | 2.84 | 1.30-6.16 | 0.008 | 81 | M-H, random |
| DHI | 5 | -0.01 | -0.04-0.02 | 0.640 | 92 | IV, random |
| sROM, ° | 5 | 1.50 | -0.59-3.58 | 0.160 | 96 | IV, random |
| Facet orientation,
° | 3 | -1.82 | -3.72-0.07 | 0.060 | 76 | IV, random |
| Facet tropism,
° | 3 | -0.36 | -0.80-0.08 | 0.110 | 10 | IV, random |
| Lumbar lordosis
angle, ° | 4 | -1.18 | -6.43-4.07 | 0.660 | 95 | IV, random |
| Sacral slope angle,
° | 3 | 3.48 | 0.53-6.42 | 0.020 | 86 | IV, random |
A total of 8 studies (19,21-27)
reported the association between BMI and rLDH. There was
heterogeneity among the eight studies, and thus, a random-effects
model was used for meta-analysis. It was found that a higher BMI
significantly increased the risk of rLDH (WMD=1.16, 95% CI: 0.69 to
1.62, P<0.001).
Clinical and imaging factors
Similarly, this study also analysed the association
of 9 clinical and imaging factors with rLDH (Table III) the corresponding forest maps
are provided in Fig. S10,
Fig. S11, Fig. S12, Fig. S13, Fig. S14, Fig. S15, Fig. S16, Fig. S17 and Fig. S18. A total of 7 studies (19,20,22-25,27)
reported the effect of modic change on rLDH, and there was
heterogeneity among these studies (I2=73%). The
meta-analysis results showed that there was an association between
modic change and the risk of rLDH after PELD (OR=2.48, 95% CI: 1.54
to 3.99, P=0.0002).
A total of 3 studies (19,25,27)
reported the association of the Pfirrmann grade with rLDH. The
meta-analysis results showed that a Pfirrmann grade ≥4 was a risk
factor for rLDH after PELD (OR=2.84, 95% CI: 1.30 to 6.16) and this
association was statistically significant (P=0.008).
A total of 3 studies (23,26,27)
reported the association between sacral slope angle and rLDH, and
there was heterogeneity among these three studies
(I2=86%). Meta-analysis showed that a larger
sacral slope angle was a risk factor for rLDH after PELD (WMD=3.48,
95% CI: 0.53 to 6.42), with a statistically significant difference
(P=0.02).
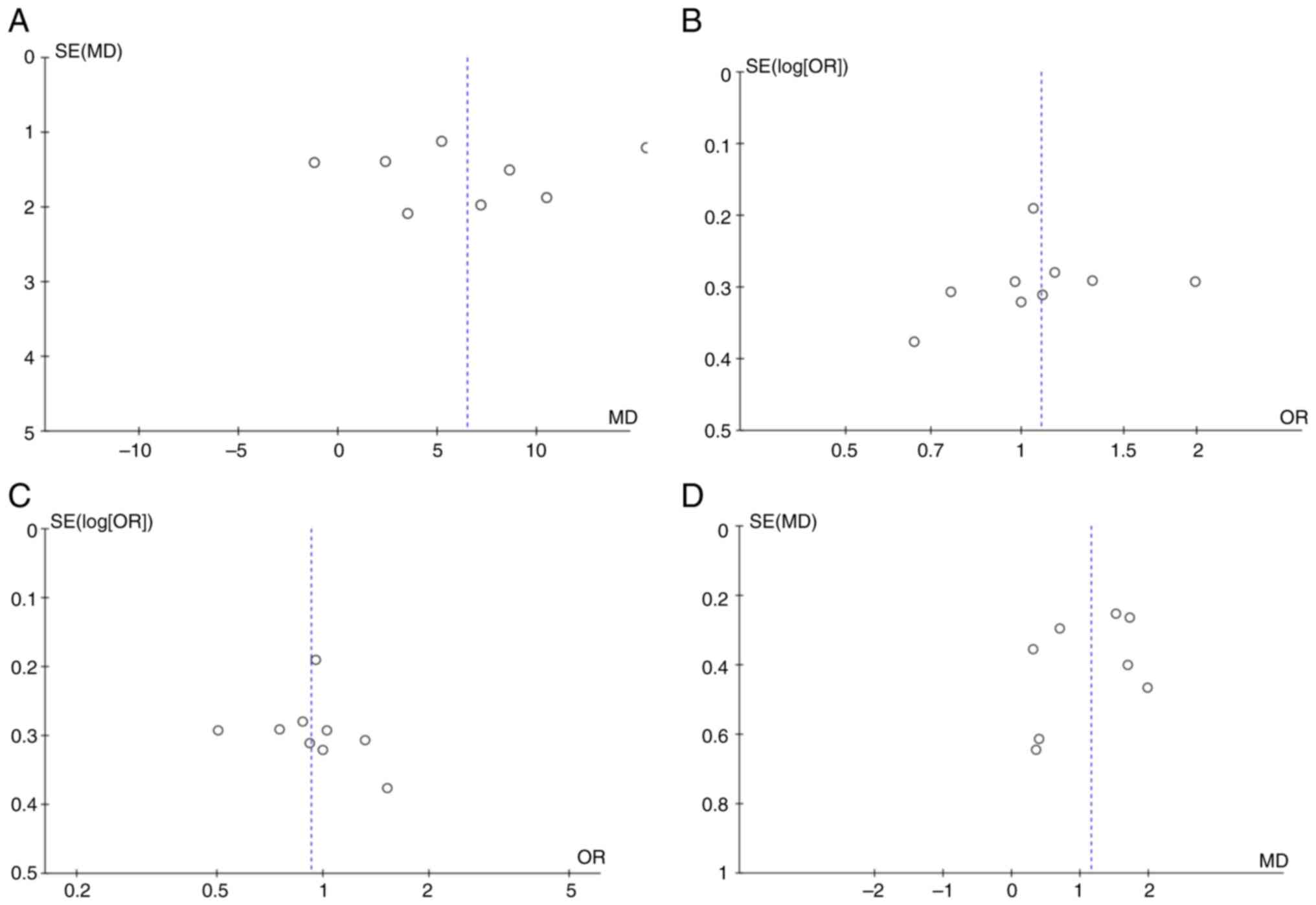
Publication bias
Four funnel plots (age, male, female, BMI) were
constructed to evaluate publication bias (Fig. 2). The scattered points in the
funnel diagram are basically symmetrical, suggesting that there is
no evidence of publication bias in the evaluation of age, male,
female and BMI.
Discussion
Due to population ageing and changes in modern
lifestyles, the occurrence of LDH exhibits a trend of growth
(28). Epidemiological studies
have shown that the overall incidence rate of LDH ranges from 2-3%,
but the incidence rates among men and women aged >35 years are
4.8 and 2.5%, respectively (28).
PELD is often used to treat LDH that is not effectively managed by
conservative treatment (6).
Identifying the risk factors for rLDH after PELD surgery and
formulating the best treatment strategy or informing patients of
the risks before surgery is an important task. In the past 20
years, there have been 2 systematic reviews evaluating the risk
factors for rLDH (29,30), but these two studies have certain
limitations that may prevent us from applying their conclusions to
the identification of rLDH after PELD. The two systematic
evaluations (29,30) comprised patients who underwent
surgery, including microdiscectomy, laminotomy, PELD,
decompression, lumbar fusion and open discectomy, indicating
significant clinical heterogeneity among the included studies. In
addition, both systematic evaluations are concerned with a small
number of potential risk factors, providing less evidence for
clinical application. Since PELD is the most commonly used surgical
method, only the risk factors for rLDH after PELD were examined;
the present results may allow clinicians to evaluate risk of rLDH
following PELD. In addition, there were 18 potential risk factors
observed in the present meta-analysis, but only 5 factors were
significant, which provide more comprehensive information. The
present study found that higher age, greater BMI, modic change,
Pfirrmann grade ≥4 and greater sacral slope angle are all
significant risk factors for rLDH after PELD. Therefore, PELD may
not be the best option at the stage of developing medical
strategies for patients with one or more of the above risk factors.
The findings of the present study will help spine surgeons develop
appropriate surgical protocols and better inform patients of
surgical risks.
Regarding sociodemographic and anthropometry
factors, consistent with previously published research findings
(31-33),
the present study also found a significant association between
higher age and the occurrence of rLDH. A retrospective cohort study
showed that the reoperation rate of patients aged ≥57 years who
underwent PELD was higher than that of patients aged <57 years
(34), and this study found that
rLDH after PELD was the main reason for reoperation. As ageing
progresses, the degradation of spinal tissue becomes increasingly
severe. Ehrendorfer et al (35) found that the severity of
preoperative disc degeneration in patients with rLDH is
significantly higher than that in non-rLDH patients. A study
indicated that obese patients are more prone to LDH (36) and are prone to adverse clinical
outcomes after surgery. A Cox regression analysis showed that a BMI
≥25 kg/m2 is an important risk factor for rLDH after
PELD (37). The study by Yaman
et al (38) indicated that
the reoperation rate of overweight or obese patients after PELD is
significantly higher than that of patients with LDH with a normal
BMI, which may be related to increased load on the intervertebral
disc. Therefore, it may be indicated that both older age and a
greater BMI are highly associated with the risk of rLDH.
Clinical and imaging factors were also examined in
the present meta-analysis. Modic changes typically include reactive
vertebral changes associated with inflammation, an unstable
microenvironment or degenerative disc disease (39,40).
As the intervertebral disc itself does not contain vascular tissue,
the micropores in the endplate are exchange channels for nutrients,
water and other metabolic products. When the endplate changes, its
nutritional effect on the intervertebral disc decreases (39,40).
Therefore, it is not difficult to understand that modic changes are
associated with a higher risk of rLDH. The present study found that
a Pfirrmann grade ≥4 is associated with a higher risk of rLDH,
which is consistent with the findings of Kim et al (41). This latter study concluded that a
higher degree of intervertebral disc degeneration is associated
with a higher risk of rLDH (41).
During the process of intervertebral disc degeneration, type I
collagen increases, while type II collagen decreases, and the
content of proteoglycans and elastin decreases (42), which causes the nucleus pulposus to
lose elasticity and the annulus fibrosus to appear cracked.
Therefore, more severe degeneration of the intervertebral disc is
associated with poorer self-repairing ability of the fibrous ring,
ultimately leading to the protrusion of the nucleus pulposus
(42). The present study found
that the sacral slope angle is associated with the risk of rLDH
after PELD. Studies have shown that a large sacral slope angle can
lead to L5-S1 vertebral body slippage and its mechanism is
increased stress in the L5-S1 vertebral body (43-45),
which may indicate a potential association between the
susceptibility to rLDH after PELD. A biomechanical study found that
a larger sacral slope angle can lead to lumbar lordosis (45) and increase stress in the lumbar
intervertebral disc. Therefore, correcting the sacral slope angle
can reduce the risk of rLDH after PELD. A larger sacral slope angle
can be considered a risk factor for rLDH.
The present study has several limitations, and
resolving these limitations will further increase the reliability
of its findings. Due to these limitations, readers need to consider
not only the conclusions of this study but also real clinical
scenarios to interpret them. First, the present meta-analysis
involved only association analyses, so the determination of causal
relationships requires further prospective cohort studies or
Mendelian randomization studies in the future. Furthermore,
although strict inclusion and exclusion criteria were established
to ensure comparability among studies, unclear definitions of rLDH,
inconsistent sample sizes and differences in follow-up time between
certain studies may reduce the reliability of the conclusions of
the present study. Finally, there was high statistical
heterogeneity for most risk factors in the present study, but our
attempt to find the source of heterogeneity was not successful.
Therefore, the application of the conclusions of the present study
requires clinical workers to consider their clinical
experiences.
In conclusion, as significant risk factors for rLDH
after PELD surgery, older age, higher BMI, modic change,
intervertebral disc degeneration and larger sacral slope angle were
identified in the present study. These findings will enable medical
workers to identify high-risk populations early and to choose
appropriate surgical procedures to reduce the risk of rLDH. Future
research should further validate the modifiable risk factors
identified in the present study to improve outcomes for patients
with rLDH.
Supplementary Material
The search strategy of 3 electronic
databases. PubMed
Forest plot of the influence on rLDH
per increment in age in year. rLDH, recurrent lumbar disc
herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of the association of male
sex with rLDH. rLDH, recurrent lumbar disc herniation; df, degrees
of freedom; M-H, Mantel-Haenszel.
Forest plot of the association of
female sex with rLDH. rLDH, recurrent lumbar disc herniation; df,
degrees of freedom; M-H, Mantel-Haenszel.
Forest plot of the influence of BMI
per increment on rLDH. BMI, body mass index; rLDH, recurrent lumbar
disc herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of the influence on rLDH
per increment in symptom duration in months. rLDH, recurrent lumbar
disc herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of odds ratio for the
association of smoking with rLDH. rLDH, recurrent lumbar disc
herniation; df, degrees of freedom; M-H, Mantel-Haenszel.
Forest plot of odds ratio for the
association of drinking with rLDH. rLDH, recurrent lumbar disc
herniation; df, degrees of freedom; M-H, Mantel-Haenszel.
Forest plot of odds ratio for the
association of diabetes mellitus with rLDH. rLDH, recurrent lumbar
disc herniation; df, degrees of freedom; M-H, Mantel-Haenszel.
Forest plot of odds ratio for the
association of hypertension with rLDH. rLDH, recurrent lumbar disc
herniation; df, degrees of freedom; M-H, Mantel-Haenszel.
Forest plot of the influence on rLDH
per increment in operantive time in min. rLDH, recurrent lumbar
disc herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of the odds ratio for the
association of modic change with rLDH. rLDH, recurrent lumbar disc
herniation; df, degrees of freedom; M-H, Mantel-Haenszel.
Forest plot of odds ratio for the
association of Pfirrmann grade ≥4 with rLDH. rLDH, recurrent lumbar
disc herniation; df, degrees of freedom; M-H, Mantel-Haenszel.
Forest plot of the influence on rLDH
per increment in disc height index. rLDH, recurrent lumbar disc
herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of the influence on rLDH
per increment in sagittal range of motion. rLDH, recurrent lumbar
disc herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of the influence on rLDH
per increment in facet orientation. rLDH, recurrent lumbar disc
herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of the influence on rLDH
per increment in facet tropism. rLDH, recurrent lumbar disc
herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of the influence on rLDH
per increment in lumbar lordosis angle. rLDH, recurrent lumbar disc
herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Forest plot of the influence on rLDH
per increment in sacral slope. rLDH, recurrent lumbar disc
herniation; SD, standard deviation; IV, inverse variance; df,
degrees of freedom.
Acknowledgements
Not applicable.
Funding
Funding: This work was supported by the National Key Research
and Development Program (grant no. 2021YFC1712804), Guangdong Basic
and Applied Basic Research Foundation (grant no. 2022A1515220131)
and Research Fund for Bajian Talents of Guangdong Provincial
Hospital of Chinese Medicine (grant no. BJ2022KY01).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JZ, JL and YZ conceived the study and are
responsible for the overall content. Literature screening and data
processing were performed by GL and BS. SZ, LZ, GL, BS, HF, WY and
JZ analyzed and interpreted the data. JZ, LZ and GL prepared the
manuscript. JL and LZ edited the manuscript. JZ, LZ and SZ
contributed equally to this work. JL and YZ confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Amin RM, Andrade NS and Neuman BJ: Lumbar
disc herniation. Curr Rev Musculoskelet Med. 10:507–516.
2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Benzakour T, Igoumenou V, Mavrogenis AF
and Benzakour A: Current concepts for lumbar disc herniation. Int
Orthop. 43:841–851. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gadjradj PS, Smeele NVR, de Jong M, Depauw
PRAM, van Tulder MW, de Bekker-Grob EW and Harhangi BS: Patient
preferences for treatment of lumbar disc herniation: A discrete
choice experiment. J Neurosurg Spine. 36:704–712. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Protzer LA, Glassman SD, Mummaneni PV,
Bydon M, Bisson EF, Djurasovic M and Carreon LY: Return to work in
patients with lumbar disc herniation undergoing fusion. J Orthop
Surg Res. 16(534)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Cho S, Lim YC, Kim EJ, Park Y, Ha IH, Lee
YS and Lee YJ: Analysis of conservative treatment trends for lumbar
disc herniation with radiculopathy in Korea: A population-based
cross-sectional study. Healthcare (Basel). 11(2353)2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Saravi B, Zink A, Ülkümen S,
Couillard-Despres S, Wollborn J, Lang G and Hassel F: Clinical and
radiomics feature-based outcome analysis in lumbar disc herniation
surgery. BMC Musculoskelet Disord. 24(791)2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sun DD, Lv D, Wu WZ, Ren HF, Bao BH, Liu Q
and Sun ML: Estimation and influence of blood loss under endoscope
for percutaneous endoscopic lumbar discectomy (PELD): A clinical
observational study combined with in vitro experiment. J Orthop
Surg Res. 15(281)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Jarebi M, Awaf A, Lefranc M and Peltier J:
A matched comparison of outcomes between percutaneous endoscopic
lumbar discectomy and open lumbar microdiscectomy for the treatment
of lumbar disc herniation: A 2-year retrospective cohort study.
Spine J. 21:114–121. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mooney J, Laskay N, Erickson N, Salehani
A, Mahavadi A, Ilyas A, Mainali B, Nowak B and Godzik J: General vs
local anesthesia for percutaneous endoscopic lumbar discectomy
(PELD): A systematic review and meta-analysis. Global Spine J.
13:1671–1688. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Shepard N and Cho W: Recurrent lumbar disc
herniation: A review. Global Spine J. 9:202–209. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Dower A, Chatterji R, Swart A and Winder
MJ: Surgical management of recurrent lumbar disc herniation and the
role of fusion. J Clin Neurosci. 23:44–50. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hlubek RJ and Mundis GM Jr: Treatment for
recurrent lumbar disc herniation. Curr Rev Musculoskelet Med.
10:517–520. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Luo L, Zhao C, Li P, Liu L, Zhou Q, Luo F
and Liang L: Posterior dynamic stabilization with limited
rediscectomy for recurrent lumbar disc herniation. Pain Res Manag.
2021(1288246)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Le H, Sandhu FA and Fessler RG: Clinical
outcomes after minimal-access surgery for recurrent lumbar disc
herniation. Neurosurg Focus. 15(E12)2003.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Arif S, Brady Z, Enchev Y and Peev N: Is
fusion the most suitable treatment option for recurrent lumbar disc
herniation? A systematic review. Neurol Res. 42:1034–1042.
2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chen Z, Zhao J, Liu A, Yuan J and Li Z:
Surgical treatment of recurrent lumbar disc herniation by
transforaminal lumbar interbody fusion. Int Orthop. 33:197–201.
2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
O'Dea RE, Lagisz M, Jennions MD, Koricheva
J, Noble DWA, Parker TH, Gurevitch J, Page MJ, Stewart G, Moher D
and Nakagawa S: Preferred reporting items for systematic reviews
and meta-analyses in ecology and evolutionary biology: Aprisma
extension. Biol Rev Camb Philos Soc. 96:1695–1722. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Stang A: Critical evaluation of the
newcastle-ottawa scale for the assessment of the quality of
nonrandomized studies in meta-analyses. Eur J Epidemiol.
25:603–605. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
He H, Ma J, Xiong C, Wei T, Tang A, Chen Y
and Xu F: Development and validation of a nomogram to predict the
risk of lumbar disk reherniation within 2 years after percutaneous
endoscopic lumbar discectomy. World Neurosurg. 172:e349–e356.
2023.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jia M, Sheng Y, Chen G, Zhang W, Lin J, Lu
S, Li F, Ying J and Teng H: Development and validation of a
nomogram predicting the risk of recurrent lumbar disk herniation
within 6 months after percutaneous endoscopic lumbar discectomy. J
Orthop Surg Res. 16(274)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kong M, Xu D, Gao C, Zhu K, Han S, Zhang
H, Zhou C and Ma X: Risk factors for recurrent L4-5 disc herniation
after percutaneous endoscopic transforaminal discectomy: A
retrospective analysis of 654 cases. Risk Manag Healthc Policy.
13:3051–3065. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Li X, Pan B, Cheng L, Li G, Liu J and Yuan
F: Development and validation of a prognostic model for the risk of
recurrent lumbar disc herniation after percutaneous endoscopic
transforaminal discectomy. Pain Physician. 26:81–90.
2023.PubMed/NCBI
|
|
23
|
Ren G, Liu L, Zhang P, Xie Z, Wang P,
Zhang W, Wang H, Shen M, Deng L, Tao Y, et al: Machine learning
predicts recurrent lumbar disc herniation following percutaneous
endoscopic lumbar discectomy. Global Spine J. 14:146–152.
2024.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Shi H, Zhu L, Jiang ZL and Wu XT:
Radiological risk factors for recurrent lumbar disc herniation
after percutaneous transforaminal endoscopic discectomy: A
retrospective matched case-control study. Eur Spine J. 30:886–892.
2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wang F, Chen K, Lin Q, Ma Y, Huang H, Wang
C and Zhou P: Earlier or heavier spinal loading is more likely to
lead to recurrent lumbar disc herniation after percutaneous
endoscopic lumbar discectomy. J Orthop Surg Res.
17(356)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Yu C, Zhan X, Liu C, Liao S, Xu J, Liang
T, Zhang Z and Chen J: Risk factors for recurrence of L5-S1 disc
herniation after percutaneous endoscopic transforaminal discectomy:
A retrospective study. Med Sci Monit. 26:e919888-1–e919888-12.
2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Zhao C, Zhang H, Wang Y, Xu D, Han S, Meng
S, Han J, Liu H, Zhou C and Ma X: Nomograms for predicting
recurrent herniation in PETD with preoperative radiological
factors. J Pain Res. 14:2095–2109. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Vialle LR, Vialle EN, Suárez Henao JE and
Giraldo G: LUMBAR DISC HERNIATION. Rev Bras Ortop. 45:17–22.
2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Huang W, Han Z, Liu J, Yu L and Yu X: Risk
factors for recurrent lumbar disc herniation: A systematic review
and meta-analysis. Medicine (Baltimore). 95(e2378)2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Yang J, Liu R, Miao Y, Nian L and Meng X:
Risk factors for recurrence after percutaneous endoscopic lumbar
discectomy: A meta-analysis. World Neurosurg. 172:88–93.
2023.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Shin EH, Cho KJ, Kim YT and Park MH: Risk
factors for recurrent lumbar disc herniation after discectomy. Int
Orthop. 43:963–967. 2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Kang MS, Hwang JH, Choi DJ, Chung HJ, Lee
JH, Kim HN and Park HJ: Clinical outcome of biportal endoscopic
revisional lumbar discectomy for recurrent lumbar disc herniation.
J Orthop Surg Res. 15(557)2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Rossi V, Maalouly J and Choi JYS: Lumbar
arthroplasty for treatment of primary or recurrent lumbar disc
herniation. Int Orthop. 47:1071–1077. 2023.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kim CH, Chung CK, Choi Y, Shin S, Kim MJ,
Lee J and Park BJ: The selection of open or percutaneous endoscopic
lumbar discectomy according to an age cut-off point: Nationwide
cohort study. Spine (Phila Pa 1976). 40:E1063–E1070.
2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Ehrendorfer S: Ipsilateral recurrent
lumbar disc herniation. J Bone Joint Surg Br.
81(368)1999.PubMed/NCBI
|
|
36
|
Patgaonkar P, Goyal V, Agrawal U, Marathe
N and Patel V: Impact of body weight, height, and obesity on
selection of skin entry point for transforaminal endoscopic lumbar
discectomy. Asian J Neurosurg. 17:262–267. 2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Yao Y, Liu H, Zhang H, Wang H, Zhang C,
Zhang Z, Wu J, Tang Y and Zhou Y: Risk factors for recurrent
herniation after percutaneous endoscopic lumbar discectomy. World
Neurosurg. 100:1–6. 2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Yaman ME, Kazancı A, Yaman ND, Baş F and
Ayberk G: Factors that influence recurrent lumbar disc herniation.
Hong Kong Med J. 23:258–263. 2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Udby PM, Modic M, Elmose S, Carreon LY,
Andersen MØ, Karppinen J and Samartzis D: The clinical significance
of the modic changes grading score. Global Spine J.
2022(21925682221123012)2022.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print).
|
|
40
|
Li Z, Gao X, Ding W, Li R and Yang S:
Asymmetric distribution of modic changes in patients with lumbar
disc herniation. Eur Spine J. 32:1741–1750. 2023.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Kim KT, Park SW and Kim YB: Disc height
and segmental motion as risk factors for recurrent lumbar disc
herniation. Spine (Phila Pa 1976). 34:2674–2678. 2009.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Moriguchi Y, Borde B, Berlin C, Wipplinger
C, Sloan SR, Kirnaz S, Pennicooke B, Navarro-Ramirez R, Khair T,
Grunert P, et al: In vivo annular repair using high-density
collagen gel seeded with annulus fibrosus cells. Acta Biomater.
79:230–238. 2018.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Labelle H, Mac-Thiong JM and Roussouly P:
Spino-pelvic sagittal balance of spondylolisthesis: A review and
classification. Eur Spine J. 20(Suppl 5):641–646. 2011.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Roussouly P, Gollogly S, Berthonnaud E,
Labelle H and Weidenbaum M: Sagittal alignment of the spine and
pelvis in the presence of L5-s1 isthmic lysis and low-grade
spondylolisthesis. Spine (Phila Pa 1976). 31:2484–2490.
2006.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Kumaran Y, Nishida N, Tripathi S, Mumtaz
M, Sakai T, Elgafy H and Goel VK: Effects of sacral slope changes
on the intervertebral disc and hip joint: A finite element
analysis. World Neurosurg. 176:e32–e39. 2023.PubMed/NCBI View Article : Google Scholar
|