Introduction
Spinal meningiomas represent 1.2-12% of all
meningiomas (1,2). Most spinal meningiomas originate in
the intradural extramedullary region, and extradural spinal
meningiomas are infrequent (2.5-3.5% of all spinal meningiomas)
(3,4). The age-adjusted incidence of spinal
meningioma ranges between 0.193 and 0.33 cases per 100,000
individuals (5,6) in the United States (7). Spinal meningiomas are primarily
located in the thoracic region but, on rare occasions, may occur in
the cervical (14-27%) or lumbar regions (2-14%) (1,2,8).
Furthermore, these tumors are most commonly observed in individuals
aged between 40 and 80 years (1),
with a higher prevalence among female individuals (female to male
ratio of 4:1) (2,9). Diagnosis is typically based on
evident neurological decline, with symptoms usually manifesting as
focal weakness, gait disturbances, pain, sensory deficits and
neurogenic bowel or bladder dysfunction attributable to spinal cord
compression (1,3). The current primary treatment option
is complete surgical resection to prevent further neurological
deterioration (10,11). The present study examined a unique
case involving an extradural meningioma that infiltrated the
brachial plexus, cervical root and spinal cord following a subtotal
resection. The patient experienced distant metastasis to the liver
within 1 year postoperatively.
Case report
A 64-year-old male patient with type 2 diabetes
mellitus and left frozen shoulder (diagnosed in December 2021) was
admitted to Chang Gung Memorial Hospital at Linkou Medical Center
(Taoyuan, Taiwan) on July 2022. The patient reported progressive
pain in the left shoulder, which had persisted for 6 months since
December 2021. Before the patient came to Chang Gung Memorial
Hospital, a shoulder X-ray, which revealed normal findings, had
been performed at a local clinic (Taoyuan, Taiwan). The patient
described that the level of pain over the left shoulder was more
intense at night than during the day and was accompanied by
numbness and tingling sensations, which negatively affected their
quality of sleep. The patient complained of experiencing mild
weakness in the left upper extremities over the last 3 months
(starting approximately in April 2022). Although the patient
attended physiotherapy and took general painkillers, the treatment
outcome was poor, and the numbness and weakness persisted. No
complaints of urinary or bowel disturbances were reported. On
admission to Chang Gung Memorial Hospital, a neurological
examination revealed full muscle strength in both the upper and
lower limbs. The grip strength of the patient was 30
kilogram-weight (kgw) in the right hand and 20 kgw in the left
hand. Pin-prick sensation tests revealed diminished sensation over
the left C5-C6 dermatome. Deep tendon reflexes were normal for both
upper and lower limbs. Regarding the left shoulder, the range of
motion was limited, with 170˚ abduction and 70˚ external rotation;
however, the patient had a full range of motion in terms of
internal rotation and adduction. The patient exhibited a typical
gait pattern during walking.
Considering the neurological findings, a diagnosis
of cervical radiculopathy accompanied by a concurrent case of mild
frozen shoulder was hypothesized. To thoroughly evaluate the
condition, electrophysiological and ultrasound examinations of the
neck and shoulder were performed.
Electrophysiological studies and
neuroimaging
An assessment of nerve conduction in the upper
extremities revealed a reduction in the amplitude of sensory nerve
action potentials, particularly in the left median and ulnar
nerves. Needle electromyography revealed complex repetitive
discharges in the left 5 and 6th cervical paraspinal muscles.
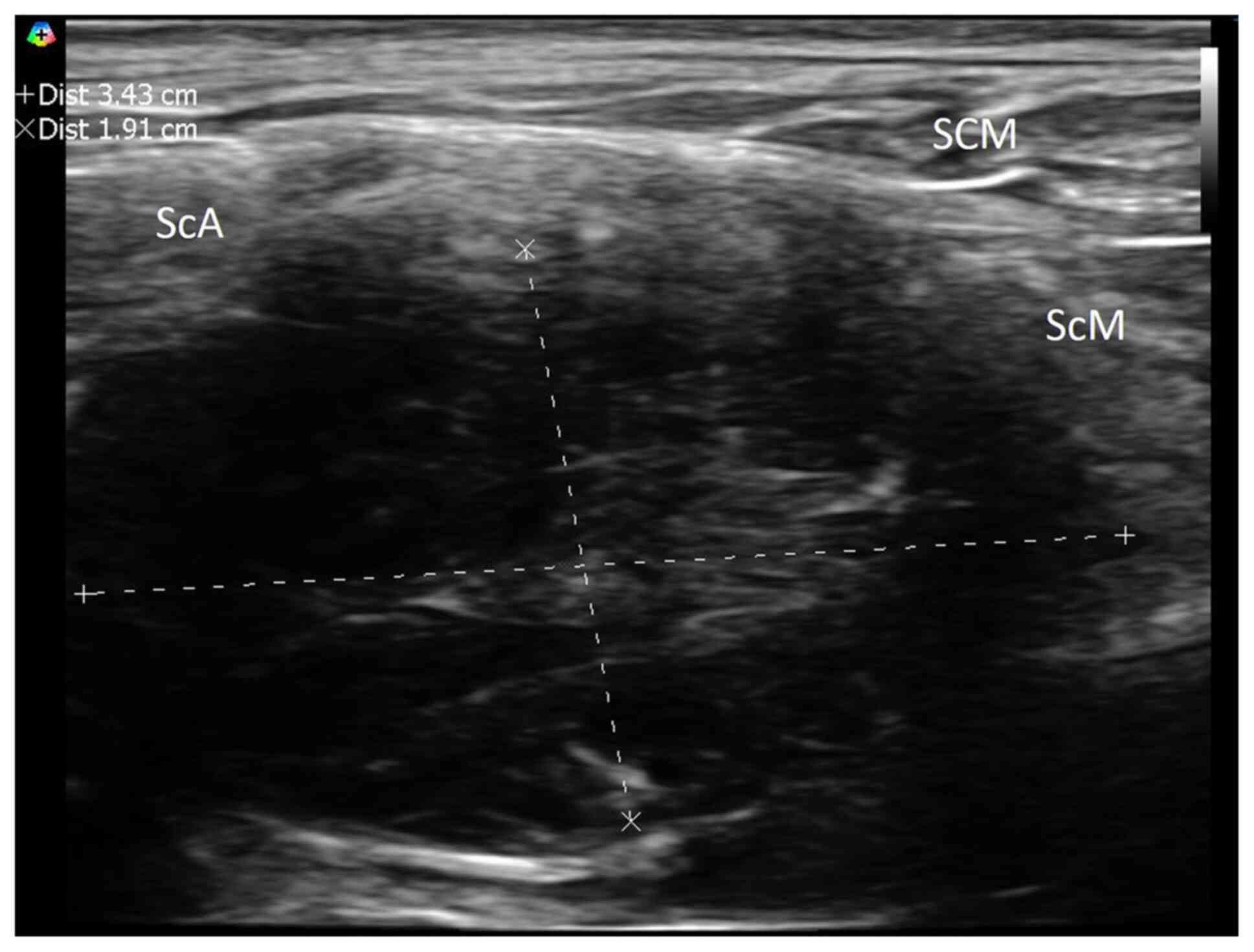
Subsequent examination using neuromuscular ultrasound revealed a
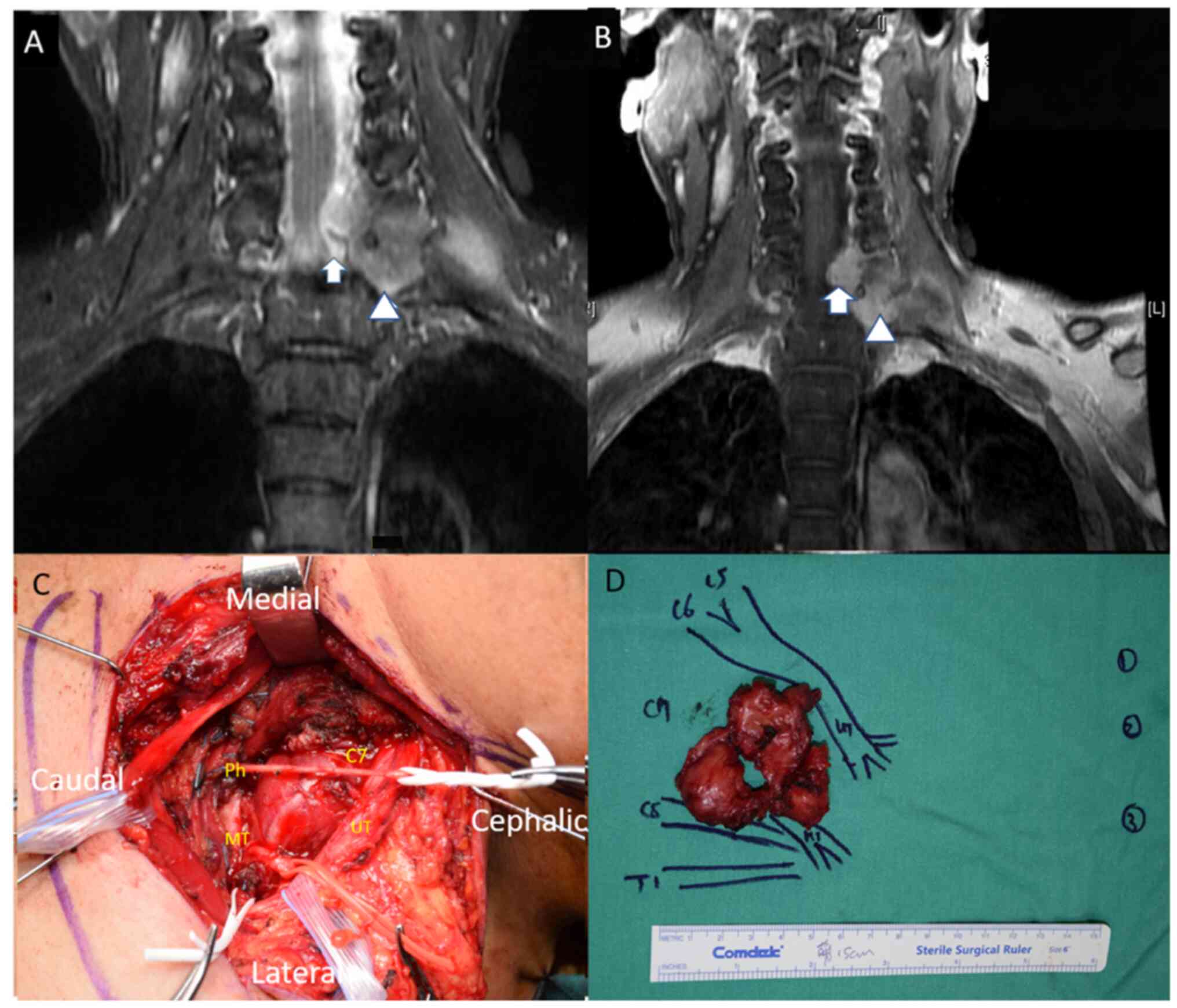
lesion localized to the left 7th cervical root (Fig. 1). Magnetic resonance imaging (MRI)
further revealed a hyperintensity fusiform mass measuring 5.5x6 cm
on T2-weighted short inversion time inversion recovery sequences.
The mass extended from the left 6/7th cervical to the 7th
cervical/1st thoracic neural foramens and reached into the left
brachial plexus. Additionally, T1-weighted images with contrast
demonstrated an enhanced mass extending into the left brachial
plexus accompanied by compression on the spinal cord (Fig. 2A and B).
Based on these findings, the presumptive diagnosis
before surgery was schwannoma or malignant nerve sheath tumor.
Surgical intervention and
histopathological findings
An incomplete tumor excision was performed due to
the encasement of the tumor around the vertebral artery. This
intervention involved a laminectomy of the 6 and 7th cervical
vertebrae, an excision of the 7th cervical nerve root, a phrenic
nerve transfer and neurolysis of the 8th cervical spinal nerve.
Intraoperative observations and gross pathology revealed tumor-like
masses (Fig. 2C and D).
The resected tissues were fixed with 10%
neutral-buffered formalin [4% (v/v) formaldehyde solution diluted
using phosphate buffer at pH 7.0] at room temperature for 8-24 h
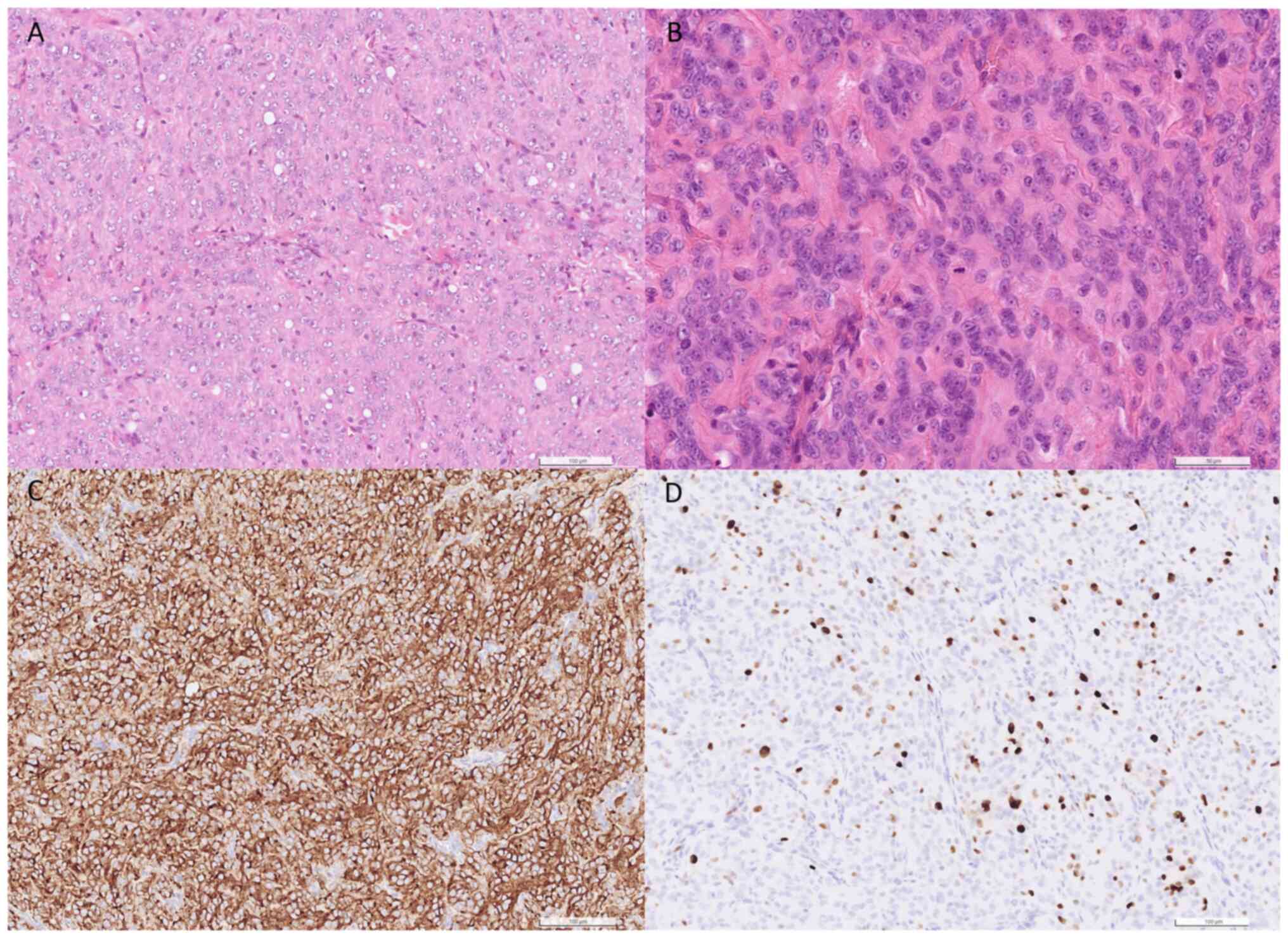
and then cut into 4- to 6-µm thick sections. Hematoxylin and eosin
staining was performed at room temperature using Mayer's
hematoxylin solution for 15 min and eosin solution for 40 sec.
Sections were observed using a light microscope (Olympus BX51) with
a digital slide scanner (Hamamatsu NanoZoomer S360). The
proliferation of epithelioid to spindle tumor cells was observed.
Furthermore, a sheet-like growth pattern, focal necrosis and
increased mitotic activity were also observed (Fig. 3A and B).
Immunohistochemical (IHC) analysis was performed.
Following tissue fixation (as aforementioned), the samples were
embedded in paraffin and cut into 4-µm thick sections. The Bond-III
Fully Automated IHC and ISH Staining System (Leica Biosystems) was
used and sections were dewaxed using Bond Dewax Solution (cat. no.
AR9222; Leica Biosystems), rehydrated with 100% alcohol, and then
washed using Bond Wash Solution (cat. no. AR9590; Leica
Biosystems). Antigen retrieval was performed using Bond Epitope
Retrieval Solution 2 (cat. no. AR9640; Leica Biosystems) in pH 9.0
for 30 min, or in acidic condition using Bond Epitope Retrieval
Solution 1 (cat. no. AR9961; Leica Biosystems) pH 6.0 for 20 min at
100˚C. Subsequently, the peroxide block reagent in Bond Polymer
Refine Detection kit (cat. no. DS9800; Leica Biosystems), which
contained 3-4% (v/v) hydrogen peroxide, was applied at room
temperature for 5 min. The following primary antibodies were
incubated with the sample for 15 min at room temperature:
Epithelial membrane antigen (EMA; 1:200; cat. no. EMA-L-CE; Leica
Biosystems), somatostatin receptor 2A (SSTR2A; 1:100; cat. no.
RBK046-05; Zytomed Systems GmbH), S100 (1:500; cat. no.
S100-167-L-CE; Leica Biosystems), SOX10 (1:100; cat. no. Z2293ML;
Zeta Corporation) and Ki-67 (1:300; cat. no. M7240; Dako; Agilent
Technologies, Inc.). The Bond Polymer Refine Detection kit also
contained a post primary linker (incubated with the sample for 8
min), DAB for visualization (incubated with the sample for 5 min)
and hematoxylin counterstain (incubated with the sample for 5 min),
which were all used at room temperature. Samples were then imaged
using a light microscope. IHC analysis indicated positive reactions
to EMA and SSTR2 and negative reactions to S100 and SOX10 (Fig. S1A-C). This distinct immunoprofile
serves a role in differentiating this tumor from neurogenic mimics,
such as cellular schwannoma or malignant peripheral nerve sheath
tumor.
The Ki-67 labeling index was determined to be 15%.
Based on these pathological characteristics, the tumor was
classified as a World Health Organization Grade II atypical
meningioma (12) (Fig. 3C and D).
Postoperative follow-up
Following the surgical intervention, radiotherapy
was administered to target any remaining tumor tissue, with a total
dose of 5,000 cGy provided in 25 fractions (five sessions per week,
administered once daily, over a period of 5 weeks). The pathology
findings confirmed the classification of grade II meningioma.
However, during the 1-year follow-up of the patient in Chang Gung
Memorial Hospital (Taoyuan, Taiwan) on October 2023, distant
metastasis to the liver and lumbar spine was observed in the
patient without local recurrence. The patient continues to receive
follow-up care in the Department of Radiation Oncology at Chang
Gung Memorial Hospital (Taoyuan, Taiwan).
Discussion
Spinal meningiomas are more common (approximately a
4:1 ratio) in women compared with in men (6,13,14),
and the majority occur in the thoracic region (77%), followed by
the cervical region (14-27%), and less frequently in the lumbar
region (2-14%) (1,2,8).
Extradural spinal meningiomas are rare (2.5-3.5% or lower of all
spinal meningiomas) (3,4) and are associated with a more rapid
progression and an aggressive phenotype compared with intradural
spinal meningiomas (7,15). In previous studies, the nerve root
tumor was usually found in patients that already had obvious
neurology signs, such as paraplegia (9,16-18),
and to the best of our knowledge, there have only been four
previous reports of extradural spinal meningiomas diagnosed without
signs of clinical myelopathy (19-22);
these are presented in Table
I.
 | Table IExtradural spinal meningiomas: A
literature review. |
Table I
Extradural spinal meningiomas: A
literature review.
| First author,
year | Age, years | Sex | Clinical
features | Duration of
symptoms | Location | Histopathology | Treatment | (Refs.) |
|---|
| Raesh and Shetty,
2021 | 18 | M | Swelling on the left
side of the neck for 1 year associated with neck pain radiating to
the left upper limb | 1 year | C4-C5 | Fibroblastic
meningioma | C4-C5 laminectomy;
subtotal tumor excision | (19) |
| Sakamoto et
al, 2018 | 57 | F | Progressive
sensorimotor disturbance in the left upper extremity | 1 year | C6-T1 | Fibrous
meningioma | C5-C7
hemilaminectomy; subtotal excision | (20) |
| Zevgaridis and
Thomé, 2002 | 75 | F | Incidental finding
by magnetic resonance imaging | Unknown | T11-T12 | Psammomatous
meningioma | laminectomy of T11
and T12; total tumor excision | (21) |
| Saade et al,
2014 | 59 | M | Right neck
stiffness | Several months | C1-C3 | Pathognomonic
spindled or polygonal cell | Complete
resection | (22) |
The present case presented with left neck and
shoulder pain, both subtle clinical signs commonly encountered in
clinical practice. Compared with previous cases, the present case
was atypical meningioma with brachial plexus involvement. The
abnormality detected during electrophysiological examination and
the neuromuscular ultrasound provided an indication that led to the
to the investigation of a tumor on the left cervical root.
Furthermore, the previous 4 cases (Table I) also exhibited no apparent signs
of myelopathy, despite the prior observation of radiculopathy signs
or the existence of a neck mass. Despite aggressive treatment, the
patient in the present study demonstrated an occurrence of distant
metastasis, an atypical finding in a meningioma case. According to
Kobayashi et al, it took a mean time of 11.3 months for the
tumor to be revealed in patients (1), and that more than half of the
diagnoses were made after clinical signs of weakness and the
development of gait disturbance (1). Due to this, these tumors typically
usually have long delays between the onset of symptoms and
diagnosis.
We hypothesize that cervical and thoracic spinal
meningiomas may exhibit distinct clinical features. In cases of
cervical spinal meningiomas, the tumor may be in close proximity to
the brachial plexus. Unlike thoracic spinal meningiomas, which
typically cause direct compression on the spinal cord, cervical
tumors may extend through the neuroforamen into the brachial
plexus. This anatomical association can pose a challenge for early
detection, as the presence of the tumor might not immediately
manifest as sensory deficits or signs of myelopathy (9,22,23).
Instead, the extension into the brachial plexus may allow for
further growth of the tumor before clinical symptoms become evident
(9,22,23).
Extradural meningiomas in the cervical region are more difficult to
excise compared with those in the thoracic region, leading to
variations in prognoses between cervical and thoracic extradural
meningiomas. Cervical extradural meningiomas are difficult to
excise because of their close proximity to the vertebral artery
(9,24-26).
However, extradural meningiomas located in the thoracic region
generally allow for a total excision of the tumor (9,24-26).
Since the clinical features of extradural and
intradural meningiomas are not markedly different, in cases where
patients exhibit an inadequate response to conservative treatment
for shoulder pain, a comprehensive examination, including
electrophysiological studies and neuromuscular ultrasound, may
serve as valuable and cost-effective screening tools for detecting
structural lesions affecting the nerve root (27,28).
Neuromuscular ultrasound is a portable and real-time tool that is
useful for disease diagnosis in an outpatient setting (27,29,30).
However, MRI remains the gold standard for diagnosis and surgical
planning (31). Risk factors for
the recurrence of extradural meningioma are being of a younger age,
being of the male sex, having dural tail signs on an MRI and a high
Simpson grade (1,13). The majority of patients experience
improvement after surgery, leading to improved functional outcomes
(13). However, distance
metastases in meningioma to the liver have been reported, even when
the extradural meningioma was detected before notable neurological
defects and standard aggressive treatment was used (32). This suggests a more aggressive
course of the meningioma. Furthermore, the occurrence of distant
metastasis in meningioma is rare, with an incidence rate of ~0.18%
across all types of meningioma. A larger tumor size, being of male
sex and having a high Simpson grade have been identified as
independent factors contributing to the likelihood of distant
metastasis (33,34). The spread of meningioma metastases
is hypothesized to occur through the venous system, lymphatics or
cerebrospinal fluid (32,35).
In the extradural space, arachnoid cells are
typically absent. The development of extradural meningiomas is
considered to occur through two possible mechanisms: i) Tumor cells
arising from ectopic arachinoidal cap cells surrounding the
periradicular root sleeves (24,36,37);
and ii) embryonic cell remnants of the arachnoid mater in the thin
periradicular dural producing extradural meningiomas near the root
(24,38).
In the present case, regular clinical monitoring and
close long-term follow-up are required for further management. In
conclusion, detecting cervical extradural meningioma at an early
stage is challenging when a patient presents with non-specific
clinical symptoms or signs. Early detection is necessary for a
timely and effective treatment. This case demonstrated that
neuromuscular ultrasound is a valuable tool, aiding physicians in
identifying lesions over the nerve root and brachial plexus,
thereby enhancing the screening and diagnosis of meningiomas.
Supplementary Material
Immunohistochemical analysis of
atypical meningiomas. (A) Somatostatin receptor 2A staining, (B)
S100 staining and (C) SOX10 staining (magnification, x200).
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article.
Authors' contributions
PCH performed the ultrasound, followed the patient
clinically and was responsible for the initial drafting of the
manuscript. JCYL performed the operation. SCH performed the
histological and pathological analyses. CHT was responsible for
analyzing the MRI images. HCK was responsible for the
interpretation of data. PCH and HCK confirm the authenticity of all
the raw data. All authors contributed to revising the draft
critically for important intellectual content. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained for the
publication of the details of the patient described in this
report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kobayashi K, Ando K, Matsumoto T, Sato K,
Kato F, Kanemura T, Yoshihara H, Sakai Y, Hirasawa A, Nakashima H
and Imagama S: Clinical features and prognostic factors in spinal
meningioma surgery from a multicenter study. Sci Rep.
11(11630)2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sandalcioglu IE, Hunold A, Müller O,
Bassiouni H, Stolke D and Asgari S: Spinal meningiomas: Critical
review of 131 surgically treated patients. Eur Spine J.
17:1035–1041. 2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ben Nsir A, Boughamoura M, Mahmoudi H,
Kilani M and Hattab N: Uncommon progression of an extradural spinal
meningioma. Case Rep Surg. 2014(630876)2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Dehcordi SR, Ricci A, Chiominto A, De
Paulis D, Di Vitantonio H and Galzio RJ: Dorsal extradural
meningioma: Case report and literature review. Surg Neurol Int.
7(76)2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Westwick HJ and Shamji MF: Effects of sex
on the incidence and prognosis of spinal meningiomas: A
surveillance, epidemiology, and end results study. J Neurosurg
Spine. 23:368–373. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kshettry VR, Hsieh JK, Ostrom QT, Kruchko
C, Benzel EC and Barnholtz-Sloan JS: Descriptive epidemiology of
spinal meningiomas in the United States. Spine (Phila Pa 1976).
40:E886–E889. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Milz H and Hamer J: Extradural spinal
meningiomas. Report of two cases. Neurochirurgia (Stuttg).
26:126–129. 1983.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gottfried ON, Gluf W, Quinones-Hinojosa A,
Kan P and Schmidt MH: Spinal meningiomas: Surgical management and
outcome. Neurosurg Focus. 14(e2)2003.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sivaraju L, Thakar S, Ghosal N and Hegde
AS: Cervical en-plaque extradural meningioma involving brachial
plexus. World Neurosurg. 108:994.e7–994.e10. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Elsamadicy AA, Reeves BC, Craft S, Sherman
JJZ, Koo AB, Sayeed S, Sarkozy M, Kolb L, Lo SL, Shin JH, et al: A
current review of spinal meningiomas: Epidemiology, clinical
presentation and management. J Neurooncol. 161:395–404.
2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
El-Hajj VG, Pettersson Segerlind J,
Burström G, Edström E and Elmi-Terander A: Current knowledge on
spinal meningiomas: A systematic review protocol. BMJ Open.
12(e061614)2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
WHO Classification of Tumours Editorial
Board. World Health Organization Classification of Tumours of the
Central Nervous System. 5th edition. International Agency for
Research on Cancer, Lyon, 2021.
|
|
13
|
Kwee LE, Harhangi BS, Ponne GA, Kros JM,
Dirven CMF and Dammers R: Spinal meningiomas: Treatment outcome and
long-term follow-up. Clin Neurol Neurosurg.
198(106238)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Solero CL, Fornari M, Giombini S, Lasio G,
Oliveri G, Cimino C and Pluchino F: Spinal meningiomas: Review of
174 operated cases. Neurosurgery. 25:153–160. 1989.PubMed/NCBI
|
|
15
|
Levy WJ Jr, Bay J and Dohn D: Spinal cord
meningioma. J Neurosurg. 57:804–812. 1982.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Takeuchi H, Kubota T, Sato K and Hirose S:
Cervical extradural meningioma with rapidly progressive myelopathy.
J Clin Neurosci. 13:397–400. 2006.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hong W, Kim ES, Lee Y, Lee K, Koh SH, Song
H and Kwon MJ: Spinal extradural meningioma: A case report and
review of the literature. J Korean Soc Radiol. 79:11–17. 2018.
|
|
18
|
Mu L, Wang M, Cheng L, Chu G and Song Z:
Atypical meningioma with destruction of cervical vertebrae inside
the spinal canal: A case report and literature review. Oncol Lett.
27(45)2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Raesh T and Shetty D: Primary cervical
extradural Meningioma presenting as neck mass-an unusual
presentation of rare case. Int J Preclinical Clin Res. 2:51–55.
2021.
|
|
20
|
Sakamoto K, Tsutsumi S, Nonaka S, Suzuki
T, Ishii H, Ito M and Yasumoto Y: Ossified extradural en-plaque
meningioma of the cervical spine. J Clin Neurosci. 50:124–126.
2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zevgaridis D and Thomé C: Purely epidural
spinal meningioma mimicking metastatic tumor: Case report and
review of the literature. Spine (Phila Pa 1976). 27:E403–E405.
2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Saade R, Hessel A, Ginsberg L, Fuller G
and Bell D: Primary extradural meningioma presenting as a neck
mass: Case report and review of the literature. Head Neck.
37:E92–E95. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lai AL, Salkade PR, Chuah KL and Sitoh YY:
Extradural cervical spinal meningioma mimicking malignancy. J
Radiol Case Rep. 12:1–10. 2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Tuli J, Drzymalski DM, Lidov H and Tuli S:
Extradural en-plaque spinal meningioma with intraneural invasion.
World Neurosurg. 77:202.e5–e13. 2012.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mariniello G, Briganti F, De Caro ML and
Maiuri F: Cervical extradural ‘en-plaque’ meningioma. J Neurol Surg
A Cent Eur Neurosurg. 73:330–333. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Frank BL, Harrop JS, Hanna A and Ratliff
J: Cervical extradural meningioma: Case report and literature
review. J Spinal Cord Med. 31:302–305. 2008.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Mah JK and van Alfen N: Neuromuscular
ultrasound: Clinical applications and diagnostic values. Can J
Neurol Sci. 45:605–619. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Telleman JA, Stellingwerff MD, Brekelmans
GJ and Visser LH: Nerve ultrasound: A useful screening tool for
peripheral nerve sheath tumors in NF1? Neurology. 88:1615–1622.
2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Rattay TW, Winter N, Décard BF, Dammeier
NM, Härtig F, Ceanga M, Axer H and Grimm A: Nerve ultrasound as
follow-up tool in treated multifocal motor neuropathy. Eur J
Neurol. 24:1125–1134. 2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lu M, Wang Y, Yue L, Chiu J, He F, Wu X,
Zang B, Lu B, Yao X and Jiang Z: Follow-up evaluation with
ultrasonography of peripheral nerve injuries after an earthquake.
Neural Regen Res. 9:582–588. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gezen F, Kahraman S, Canakci Z and Bedük
A: Review of 36 cases of spinal cord meningioma. Spine (Phila Pa
1976). 25:727–731. 2000.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sheng B, Liu Y and Liu C: Liver metastasis
from typical meningioma. World Neurosurg. 145:334–337.
2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Vuong HG, Ngo TNM and Dunn IF: Incidence,
risk factors, and prognosis of meningiomas with distant metastases
at presentation. Neurooncol Adv. 3(vdab084)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Himič V, Burman RJ, Fountain DM, Hofer M,
Livermore LJ and Jeyaretna DS: Metastatic meningioma: A case series
and systematic review. Acta Neurochir (Wien). 165:2873–2883.
2023.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Lee GC, Choi SW, Kim SH and Kwon HJ:
Multiple extracranial metastases of atypical meningiomas. J Korean
Neurosurg Soc. 45:107–111. 2009.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Buetow MP, Buetow PC and Smirniotopoulos
JG: Typical, atypical, and misleading features in meningioma.
Radiographics. 11:1087–1106. 1991.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Tohma Y, Yamashima T and Yamashita J:
Immunohistochemical localization of cell adhesion molecule
epithelial cadherin in human arachnoid villi and meningiomas.
Cancer Res. 52:1981–1987. 1992.PubMed/NCBI
|
|
38
|
Haft H and Shenkin HA: Spinal epidural
meningioma: Case report. J Neurosurg. 20:801–804. 1963.PubMed/NCBI View Article : Google Scholar
|