Introduction
Thermal-crush injuries belong to composite injuries
caused by both thermal burns and mechanical compression, and they
often accompany tissue damages of the skin, muscles, blood vessels
and bones, with a high amputation rate of 13.3% (1,2).
Thermal-crush injuries of the hand often occur in workplaces and
fire accidents (3). Due to the
complex condition and severe injury, functional recovery through
limb preservation and reconstruction is challenging (4).
Treatment processes of thermal-crush injuries of the
hand (1) are generally divided
into three stages, namely limb salvage, functional reconstruction
and functional rehabilitation. They are indispensable and important
during the whole process of treatment. After designing a limb
salvage reconstruction plan, bone and joint injuries often require
an external fixation or simple internal fixation. Based on the
general principles of burn treatment, an early and thorough
debridement is necessary (5).
Microsurgery and plastic surgery for soft tissue injuries are
performed after the successful debridement. Thermal-crush injuries
of the hand often involve severe composite injuries and defects of
bones and soft tissues that require the bone and soft tissue
reconstruction (6). Free tissues
are usually used for reconstruction, especially free toe
transplantation and free skin flap repair (7). Notably, an external fixation using
Ilizarov external frame and bone transport technology is preferred
to the reconstruction of bones and soft tissues in patients with
thermal-crush injuries of the hand due to the fragile structure of
the soft tissues of the hand (8).
A former soviet orthopedic physician, Ilizarov,
hypothesized that human bones and soft tissues have great potential
for regeneration and plasticity. They are able to grow longer or
shortened by medical methods to reconstruct damaged tissues. Since
then, Ilizarov's external frame and bone handling techniques have
been widely used in clinical practice to correct bone deformities
(9). Ilizarov's technology
combined with soft tissue stretching is of great significance in
the treatment of common orthopedic problems like bone defects,
finger absence, joint contracture and joint stiffness following
thermal-crush injuries of the hand (10).
For challenging cases of thermal-crush injuries of
the hand, a comprehensive hand microsurgical repair and
reconstruction plan enhances the success rate of limb salvage
(11). A further evaluation of
limb salvage through mid-term and long-term follow-up is useful to
provide references for an individualized therapeutic strategy of
limb salvage and assessment of functional recovery (12).
Previously, we have treated similar cases in the
upper, lower and hand regions. We used the Ilizarov technique for
hand extension in 10 patients, traction correction in 5 patients
with flexion contracture and limb extension in 5 patients after
lower limb replantation or severe injury. Subsequently, 5 patients
with limb extension after replantation or severe injury achieved
successful surgery, restored limb length and plantar function and
had no pain in the affected limb. In patients with flexion
contracture and extension, the affected limbs had achieved
improvement in range of motion, but due to the severity of flexion
contracture and poor soft tissue conditions, they had not fully
recovered their active and passive range of motion. We have
extensive experience in applying Ilizarov treatment. Based on this,
we successfully treated the current case. The present study reports
a case of thermal-crush injuries of the hand treated with
microsurgical technology combined with Ilizarov treatment for limb
salvage and functional reconstruction.
Case report
A 25-year-old male patient sought for limb salvage
treatment 1 month after sustaining thermal-crush injuries of the
right hand and forearm. He had been treated with multiple
procedures of debridement and was recommended for forearm
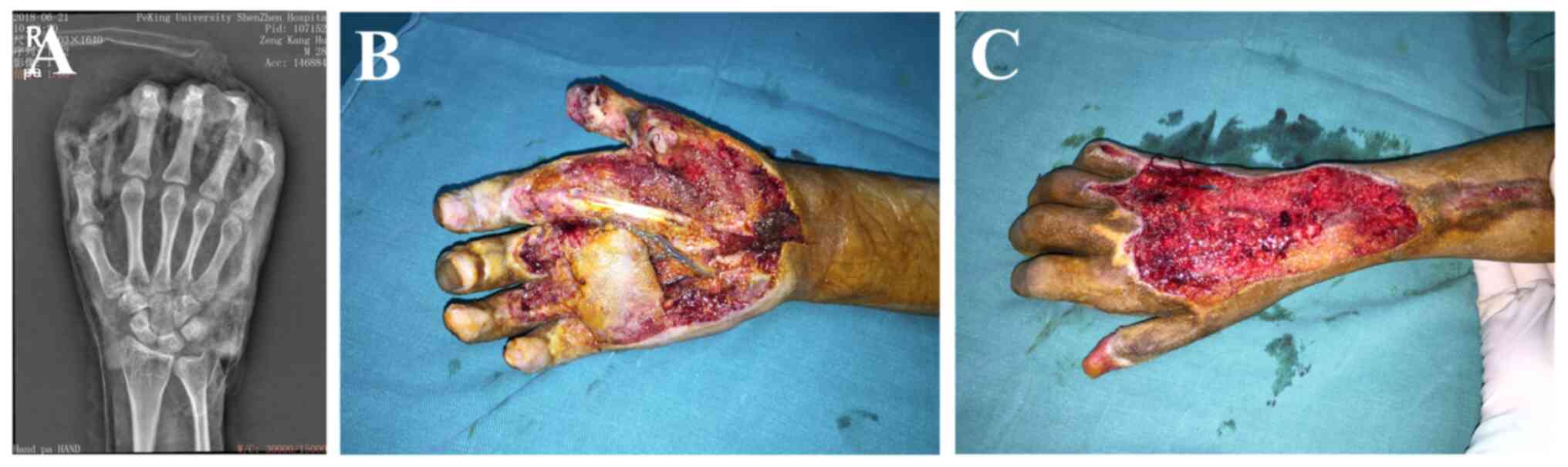
amputation in another hospital. X-ray scans showed fractures of the
proximal and distal segments of the thumb, and damage of the
interphalangeal joint. After admission to Peking University
Shenzhen Hospital (Shenzhen, China) in June 2018, the patient was
treated with debridement procedures for skin defects of the whole
palm, including palmar skin defects of the proximal phalanx of the
index, middle, ring and pinkie fingers and exposures of the flexor
tendon articular capsule and phalanges of the thumb. Only a small
piece of dorsal skin of the thumb with 1.5 cm2 in width
remained. Other skin defects were present on the dorsal side of the
hand and forearm, 10x3 cm2 in width. Fortunately, the
granulation tissues grew well without an exposure of deep tissues
like tendons (Fig. 1A-C). The
patient was therefore diagnosed with: i) Postoperative infection of
thermal-crush injuries of the right hand and right forearm; ii)
comminuted open fractures of the proximal and distal phalanges of
the right thumb; iii) osteomyelitis; iv) palm skin defects with
exposed tendons; and v) skin defects of the opisthenar and the
forearm.
Treatment processes and follow-up
After admission, the patient was sequentially
managed by debridement procedures, amputation of the distal
phalange of the thumb and resections of the necrotic flexor tendon
from the metacarpophalangeal joints of the thumb and index finger
to the wrist joint [negative pressure wound therapy (NPWT)
(13) technology was used].
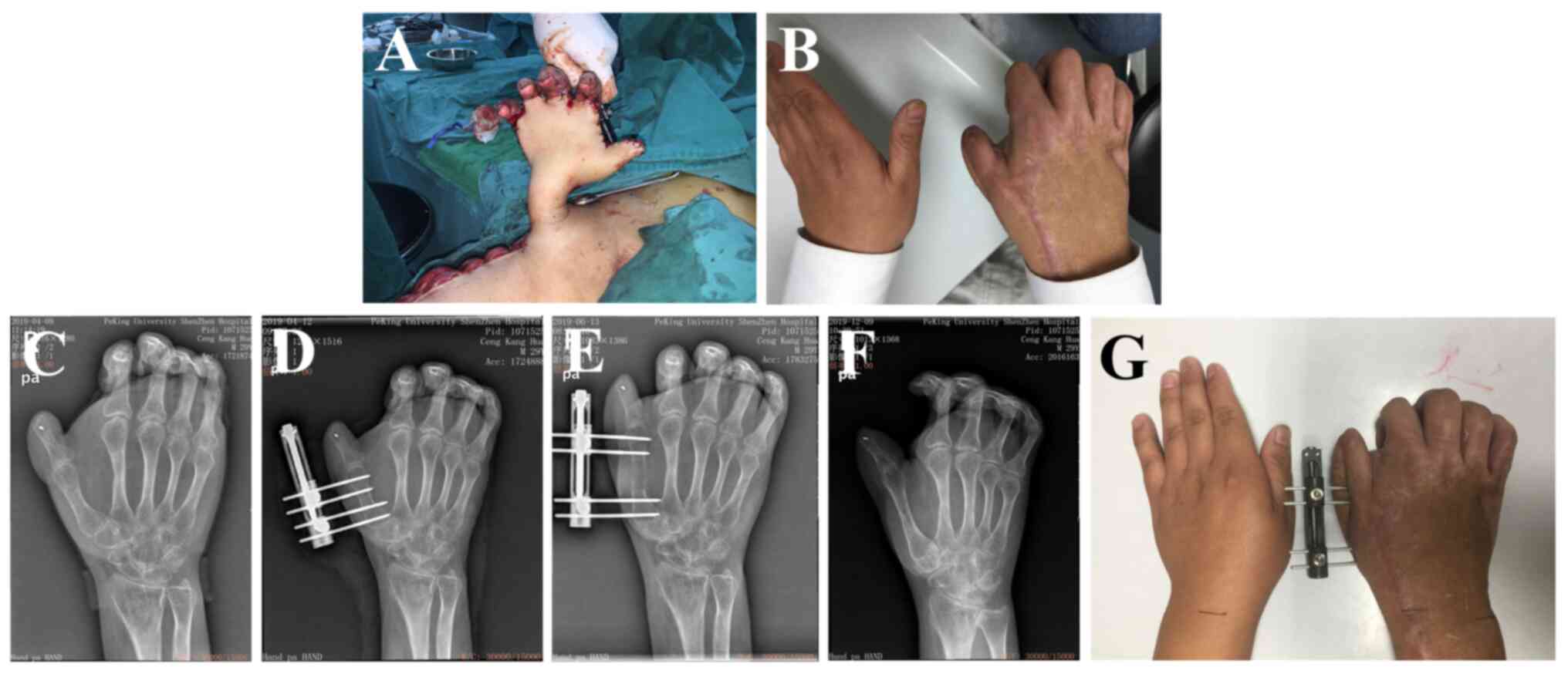
At 5 weeks post-injury, a pedicled anterolateral
thigh perforator flap was transplanted to repair skin defects on
the palm, thumb and the palmar side of the index, middle, ring and
pinkie fingers. The deep flexor tendon of the index finger and the
flexor hallucis longus tendon were repaired by transplanting an
autologous palmaris longus tendon. Full-thickness skin grafts were
used to repair the skin defects of the opisthenar (Fig. 2).
The skin pedicle was severed at 3 weeks
postoperation. At 3 months after the soft tissue repair, the
patient was managed by minimally invasive osteotomy bone
lengthening for the first metacarpal bone, and thinning and shaping
of the palmar skin flap were performed.
At 1 week after the first metacarpal osteotomy
(Fig. 3A-D), a 50-day thumb
metacarpal lengthening for 2.5 cm was performed (Fig. 3E-G). At 3 months after the
lengthening (Fig. 4A), an
enlargement of the first web space, flexor tendon relaxation,
fusion of the first carpometacarpal joint, capsular release of the
index, middle, ring and pinkie fingers and Ilizarov external
fixation of the right hand were performed (Fig. 4B and C).
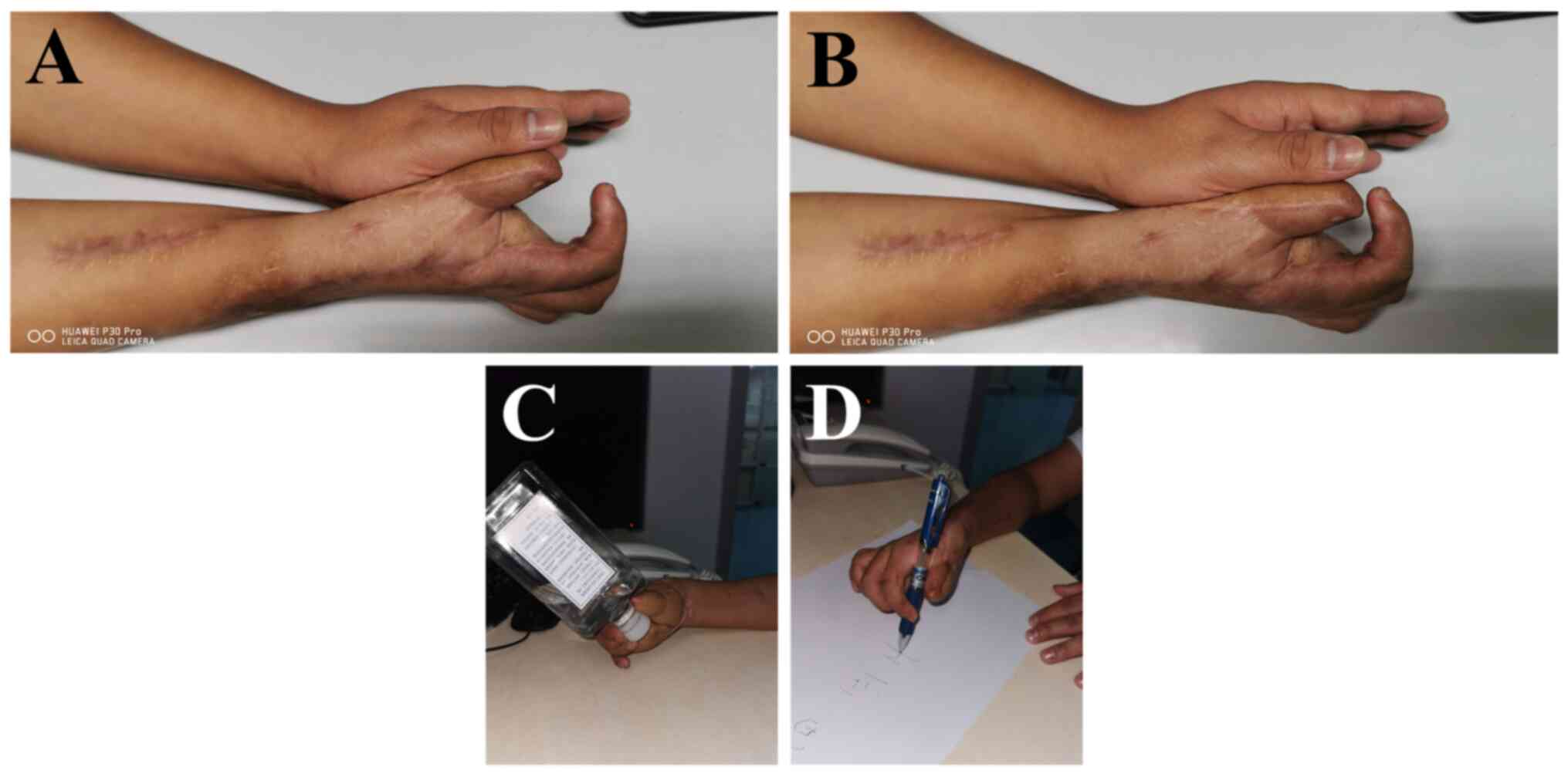
At 1 week after the external fixation, the flexion
contracture deformity was corrected by using an external frame to
stretch the index, middle, ring and pinkie fingers. The thumb was
slowly extended for the opening and extension of the first web
space. The traction speed and frequency gradually increased to
yield 5-10 times of a reciprocating motion of the stretching and
flexibility, which were terminated 20 days after surgery. The outer
frame was removed, followed by the intervention of rehabilitation
exercises. After discharge, the patient received training with a
rehabilitation therapist, wearing orthodontic braces throughout the
early stages for fixation, and intermittently wearing braces after
4 weeks.
After the first skin flap surgery, the
metacarpophalangeal joints of the index, middle, ring and little
fingers were stiffened at 0˚, the proximal interphalangeal joint
was stiffened at 90˚, the distal interphalangeal joint was flexed
at 30˚ and the ROM was at 0˚. After the second Ilizarov stretch,
the metacarpophalangeal joints of the index, middle, ring and
little fingers moved at 30-60˚, the proximal interphalangeal joint
moved at 40-70˚ and the distal interphalangeal joint flexed at
10-30˚ with ROM at 60˚. After follow-up for 1 year, hand function
was recovered well with a QuickDASH (14) (Disabilities of Arm, Shoulder and
Hand) score of 35 points, and Chen's criteria (15) of grade 2 (Fig. 5A-D).
Discussion
With the advancement of technologies and industry
development, case numbers of thermal-crush injuries of the hand are
gradually on the rise (16).
Thermal-crush injuries of the hand are severe and complex due to
the dual-injury of thermal burns and mechanical compression, as
well as the anatomical characteristics of the hand. A timely
transfer to medical institutions with clinical experience of limb
salvage and reconstruction is essential (17). In clinical practice, an accurate
staging of thermal-crush injuries of the hand is necessary, and it
usually requires an emergency X-ray or even CT based on the Mangled
Extremity Severity Score (MESS) (18) and the Ganga Hospital Score (GHS)
(19).
In the present case report, the patient was graded
with 5 points and 10 points of MESS and GHS, respectively. An
optimal treatment plan was comprehensively decided based on
objective diagnostic scores and individualized conditions (20). Both individualized conditions of
patients (21) and experiences of
the medical institutions are two vital factors to influence the
accurate clinical decision-making for limb salvage reconstruction
(22). Amputation is an option for
patients with thermal-crush injuries of the hand (23). The upper and lower limbs are
flexible and highly needed in the daily life. Their functions
usually cannot be replaced by the prosthetics. Therefore, great
efforts have be made on limb salvage and limb reconstruction
(24). Through the successful
treatment of the present case, the current study suggested that the
injured limb should be fully protected without violating existing
medical treatment principles. Multidisciplinary consultations
involving specialists of burn surgery, microsurgery, repair and
reconstruction surgery and plastic surgery, and even multi-center
remote consultations are recommended to reduce the amputation
rate.
Principles of timely and thorough debridement in
hand surgery (25) and early
escharotomy in burn surgery (26)
should be strictly conformed to during debridement procedures of
thermal-crush injuries of the hand. A complete removal of obvious
necrotic and inactivated tissues is required. A third-degree burn
usually causes full-thickness skin necrosis, and the removal of the
necrotic skin and soft tissues is necessary to reduce the risk of
infection (27). NPWT is
recommended for exposed wounds in order to regenerate the wound
tissue in cases when there is a lack of effective soft tissue for
reconstruction (28).
Soft tissue reconstruction is the major event of
limb salvage for thermal-crush injuries of the hand (29). Following the general process of
skin defect treatment in hand surgery (30), free skin grafting is often used to
repair the wound surface in patients with well-growing granulation
and lack of deep tissue exposure. Skin flap transplantation is the
only choice for patients with a high demand for wear resistance and
weight bearing, and those with a deep tissue exposure. In the
present case, the pedicled anterolateral thigh flap (ALTP) was
adopted for its high success rate of transplantation (31). Moreover, the impact of skin flap
vascular anastomosis on the hand blood supply should be concerned
due to the full hand injury, which can be preoperatively assessed
by the angiography to localize the vascular recipient area, if
necessary.
The Ilizarov treatment has been used clinically for
a long time (32), and it was
important in the reconstruction of hand function in the present
case. The Ilizarov technique can effectively release and correct
joint stiffness and flexion contractures without complex and
dangerous release surgeries (33).
At the same time, slow stretching of soft tissue can simultaneously
correct defects in tendons, nerves, blood vessels and skin,
avoiding complex micro repair and reconstruction surgeries
(34). Additionally, the Ilizarov
bone lengthening technique can correct thumb shortening without the
need for complex toe transplantation and thumb reconstruction,
without donor site damage (35).
However, its drawbacks are that Ilizarov technology
requires specialized technical training and a longer learning curve
for doctors. The cost of using an external frame is relatively
high, and there is a risk of nail path infection and joint
stiffness when using an external frame. Patients may feel
uncomfortable wearing an external frame compared with patients who
do not use external frame for other treatment methods and it takes
a longer time to wear it until the limb function is recovered. In
addition, for patients with finger elongation, it is not possible
to achieve good appearance and function after toe transplantation
and reconstruction. For the correction of flexion contracture, the
release effect for injured limbs of using Ilizarov technology is
not as complete as patients using surgical release of soft tissue
transfer coverage and there will be rebound after removing the
external frame (36).
Some treatment innovations in the present case
should be highlighted. First of all, the distal phalange of the
thumb was amputated during the debridement procedures, resulting in
a type 2 thumb defect. The patient refused a toe transplantation
for finger reconstruction, and finally, a mini track bracket was
used to perform a minimally invasive osteotomy plus bone
lengthening for the middle phalanx of the first metacarpal bone.
The thumb was ultimately lengthened by 2.5 cm, restoring its normal
physiological length. Notably, severe soft tissue loss was repaired
using the ALTP for the range of 2/3 of the circumference of the
wound in the soft tissue defect. The successful finger lengthening
indicated that the bone transport distraction osteogenesis via the
Ilizarov method can still be applied to patients with severe finger
injuries for limb reconstruction.
Although finger lengthening surgery is not the gold
standard for finger reconstruction (37), the present study preferred not to
create a functional thumb using the toe due to the poor overall
condition of this patient. Secondly, a narrow first web space
restricted active flexion and extension activities of the thumb
after an initial treatment. Following the thumb lengthening, the
present study performed an incisional release of subcutaneous scars
in the first web space, installed a track-type external fixation
frame between the first and second metacarpal bone and gently
expanded the soft tissues in the first web space at 1 week
postoperation (38). In addition,
a gradual traction of the thumb to the palm opposition on the
circular external fixator of the second to the fifth metacarpal
bones and a fixation of the thumb to the palm opposition were
performed to achieve the bony palmar opposition, which eventually
yielded a successful reconstruction of thumb opposition.
Thirdly, the patient had scar hyperplasia after
thermal-crush injuries of the hand. Although the index, middle,
ring and pinkie fingers of the patient were able to be preserved,
they were not functional. A conventional tendon release surgery
requires extensive incisions (39), which inevitably causes defects in
the palmar skin and soft tissues and damages the palmar nerve and
vascular bundles of the fingers, leading to the high risk of finger
necrosis (40). Using the Ilizarov
method to achieve soft tissue traction, a traction device with the
metacarpal ring as the fulcrum was designed to slowly stretch the
index, middle and ring fingers, which successfully corrected
flexion contracture deformities, restored finger pinching movements
and reconstructed partial hand functions. Through the successful
reconstruction of hand function in the present case of
thermal-crush injuries using the Ilizarov external fixation method,
the present study provided an alternative treatment plan of
functional reconstruction for those with poor soft tissue
conditions.
However, due to the small sample size, the treatment
plan for the current case needs to be re-evaluated and optimized in
future clinical applications. A long-term follow-up is also
essential to assess the recovery condition. We hypothesize that for
such patients, thumb extension can be performed after the wound
treatment is completed. When flexion contracture occurs, stretching
surgery can generally be considered when the scar softens 6 months
after the last surgery. Attention should be paid to the hand
function assessment during follow-up and the patient should be
observed for secondary fractures and osteomyelitis.
We also gained experiences from the treatment
processes of this case. Firstly, a more reasonable skin flap design
(such as trying to reduce the amount of skin flaps taken from the
donor area) is needed to avoid the pain and a long treatment cycle
caused by pedicle skin flap transplantation. Free skin flap
transplantation is recommended to achieve a better outcome through
advanced microsurgical techniques. Secondly, doctors and materials
science experts should aim to jointly design a multi-angle
stretching device to achieve bone extension and a 10-15˚ recovery
of the interphalangeal joint angle; thereafter improving hand
appearance and function during thumb lengthening. Thirdly, the
Ilizarov method and device can also be modified to achieve a
simultaneous soft tissue stretching of the index, middle, ring and
pinkie fingers during thumb extension, thus shortening the
treatment cycle. An individual stretching of each finger may be
useful to maximize the stretching effect and achieve a better
functional reconstruction. Fourthly, the present study should
strengthen the follow-up examinations and guidance for
postoperative functional exercises throughout the entire treatment
process. Their effective interventions after soft tissue
reconstruction with the assistance of orthodontic fixed braces are
expected to reduce or even avoid the flexion contracture
deformities of the index, middle, ring and pinkie fingers.
In conclusion, microsurgery combined with Ilizarov
technology can effectively reconstruct the function of complex
thermal-crush injuries of the hand. Through the present successful
treatment, we provide experience and strategies for clinical
management for specialized doctors.
Acknowledgements
Not applicable.
Funding
Funding: This research was supported by grants from the National
Natural Science Foundation of China (grant nos. 82172432 and
82102568), Guangdong Medical Science and Technology Research
Funding (grant no. A2022390), Shenzhen Key Medical Discipline
Construction Fund (grant no. SZXK023), Shenzhen ‘San-Ming’ Project
of Medicine (grant no. SZSM202211038), Shenzhen Science and
Technology Program (grant nos. JCYJ2022 0818102815033,
KCXFZ20201221173411031 and JCYJ20210324110214040), Guangdong Basic
and Applied Basic Research Foundation (grant nos. 2022B1515120046,
2022A1515220111 and 2021A1515012586) and The Scientific Research
Foundation of Peking University Shenzhen Hospital (grant no.
KYQD2021099).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JY, FY and ZZ confirm the authenticity of all the
raw data. JY, FY and ZZ carried out conceptualization. FY acquired
the funding. JY, LY, FM, JW, SW and YX carried out the
investigation. FY and ZZ supervised the study. JY wrote the
original draft. FY and ZZ reviewed and edited the draft. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Research Ethics
Committee of Peking University Shenzhen Hospital (Peking University
Shenzhen Hospital Ethical Review (Research) (2023) no. 12).
Patient consent for publication
Written informed consent was obtained from the
participant/s for the publication of this case report and any
potentially identifiable images or data included in this
article.
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
Fan Y, Pan Y, Chen C, Cui S, Li J, Jin G,
Huang N and Xu S: Use of composite acellular dermal
matrix-ultrathin split-thickness skin in hand hot-crush injuries: A
one-step grafting procedure. Biomed Res Int.
2022(1569084)2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zhang W, W L, Li Y and Xu D: Skin flap
repair of electric shock and hot-crush injury of hand. Chin J
Microsurgery. 31(242)2008.(In Chinese).
|
|
3
|
Li Q, Wang LF, Chen Q, Wang SJ, Li F and
Ba T: Amputations in the burn unit: A retrospective analysis of 82
patients across 12 years. Burns. 43:1449–1454. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wu YZ, Huang CH, Zhang XY and Shen GL: The
clinical application effects of artificial dermis scaffold and
autologous split-thickness skin composite grafts combined with
vacuum-assisted closure in refractory wounds. Int Wound J.
20:2113–2120. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Legemate CM, Kwa KAA, Goei H, Pijpe A,
Middelkoop E, van Zuijlen PPM, Beerthuizen GIJM, Nieuwenhuis MK,
van Baar ME and van der Vlies CH: HyCon Study Group. Hydrosurgical
and conventional debridement of burns: Randomized clinical trial.
Br J Surg. 109:332–339. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wang XX, Wang HS, Xiao SC, Wang CY, Ji SZ,
Chai YM and Wen G: N klA Case Report on a IV-degree thermal crush
injury of right upper Arm: The application of functional prosthesis
implantation technology. J Burn Care Res. 43:487–491.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Shao H, Luo R, Wang X, Pan X and Chen G:
Management of a patient with small-area burns, severe sepsis and
superficial vein thrombosis. J Wound Care. 24:73–74, 77-78.
2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhu YL, Guo BF, Zang JC, Pan Q, Zhang DW,
Peng Y and Qin SH: Ilizarov technology in China: A historic review
of thirty-one years. Int Orthop. 46:661–668. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kirienko A and Malagoli E: Ilizarov
technique in severe pediatric foot disorders. Foot Ankle Clin.
26:829–849. 2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wu YJ, Zhang YB, Hamushan M, Zhang WJ,
Zhang T, Li XJ, Han P and Lou TF: Role of perforating artery
pedicled neurotrophic flap in the treatment of compound tissue
defect of Tibia using the ilizarov technique. Orthop Surg.
14:1294–1299. 2022.PubMed/NCBI View
Article : Google Scholar
|
|
11
|
Zhang X, Yao Y, Rao L, Qin Z, Zhang L, Xu
Y, Chen Y, Yao J and Song D: Free sensate intercostal artery
perforator flap for hand soft tissue reconstruction. Zhongguo Xiu
Fu Chong Jian Wai Ke Za Zhi. 34:497–500. 2020.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
12
|
Di Castri A, Quarta L, Mataro I, Riccardi
F, Pezone G, Giordano L, Shoham Y, Rosenberg L and Caleffi E: The
entity of thermal-crush-avulsion hand injury (hot-press roller
burns) treated with fast acting debriding enzymes (nexobrid):
Literature review and report of first case. Ann Burns Fire
Disasters. 31(31)2018.PubMed/NCBI
|
|
13
|
Shi J, Gao Y, Tian J, Li J, Xu J, Mei F
and Li Z: Negative pressure wound therapy for treating pressure
ulcers. Cochrane Database Syst Rev. 5(CD011334)2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Pyörny J, Sletten IN and Jokihaara J:
Concurrent validity study of QuickDASH with respect to DASH in
patients with traumatic upper extremity amputation. BMC
Musculoskelet Disord. 25(86)2024.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ramji M, Steve AK, Premji Z and Yeung J:
Functional outcomes of major upper extremity replantation: A
scoping review. Plast Reconstr Surg Glob Open.
8(e3071)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ruan J, Xi M and Xie W: Analysis of 12,661
pediatric burns in Wuhan institute of burns: A retrospective study
of fifteen years. Burns. 47:1915–1921. 2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Pang M, Xiao H, Wang H, Liu X, Chen J and
Cen Y: Effectiveness of different flaps for repair of severe palm
scar contracture deformity. Zhongguo Xiu Fu Chong Jian Wai Ke Za
Zhi. 30:382–384. 2016.PubMed/NCBI(In Chinese).
|
|
18
|
Gratl A, Kluckner M, Gruber L, Klocker J,
Wipper S and Enzmann FK: The mangled extremity severity score
(MESS) does not predict amputation in popliteal artery injury. Eur
J Trauma Emerg Surg. 49:2363–2371. 2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Parikh S, Singh H, Devendra A,
Dheenadhayalan J, Sethuraman AS, Sabapathy R and Rajasekaran S: The
use of the Ganga Hospital Score to predict the treatment and
outcome of open fractures of the Tibia. Bone Joint J. 102-B:26–32.
2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fillingim RB: Individual differences in
pain: Understanding the mosaic that makes pain personal. Pain. 158
(Suppl 1):S11–S18. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Tonn JC, Thon N, Schnell O and Kreth FW:
Personalized surgical therapy. Ann Oncol. 23 (Suppl 10):x28–x32.
2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tosti R and Eberlin KR: ‘Damage control’
Hand surgery: Evaluation and emergency management of the mangled
hand. Hand Clin. 34:17–26. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ye S, Teng X, Chen H, Jing J and Zhang J:
Clinical application of lateral arm lobulated flaps to repair
multiple soft tissue defect of hand. Zhongguo Xiu Fu Chong Jian Wai
Ke Za Zhi. 30:444–446. 2016.PubMed/NCBI(In Chinese).
|
|
24
|
Bakhach J, Abu-Sitta G and Dibo S:
Reconstruction of blast injuries of the hand and upper limb.
Injury. 44:305–312. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Cao Z, Li C, He J, Qing L, Yu F, Wu P and
Tang J: Early reconstruction delivered better outcomes for severe
open fracture of lower extremities: A 15-Year retrospective study.
J Clin Med. 11(7174)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Widgerow AD, King K, Tocco-Tussardi I,
Banyard DA, Chiang R, Awad A, Afzel H, Bhatnager S, Melkumyan S,
Wirth G and Evans GR: The burn wound exudate-an under-utilized
resource. Burns. 41:11–17. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Gallentine A: Third-degree burn on the
neuropathic lower extremity in a patient with diabetes while
wearing a copper-containing compression sock: A case report. Wound
Manag Prev. 67:26–29. 2021.PubMed/NCBI
|
|
28
|
Pappalardo V, Frattini F, Ardita V and
Rausei S: Negative pressure therapy (NPWT) for management of
surgical wounds: Effects on wound healing and analysis of devices
evolution. Surg Technol Int. 34:56–67. 2019.PubMed/NCBI
|
|
29
|
Li M, Liang W, Luo Z, Huang S, Ma L, Yang
Y and Zhang Z: Toe fibular-dorsal artery flap anastomosed to dorsal
digital artery in repairing dorsal soft tissue defect of fingers.
Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 30:732–735.
2016.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
30
|
Milner CS and Thirkannad SM: Resurfacing
glabrous skin defects in the hand: The thenar base donor site. Tech
Hand Up Extrem Surg. 18:89–91. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Vijayasekaran A, Gibreel W, Carlsen BT,
Moran SL, Saint-Cyr M, Bakri K and Sharaf B: Maximizing the Utility
of the Pedicled Anterolateral Thigh Flap for Locoregional
Reconstruction: Technical Pearls and Pitfalls. Clin Plast Surg.
47:621–634. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Aktuglu K, Erol K and Vahabi A: Ilizarov
bone transport and treatment of critical-sized tibial bone defects:
A narrative review. J Orthop Traumatol. 20(22)2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Hou N, Zhang H, Bai M, Chen H, Song W and
Wang L: The old supracondylar fracture of femur treated by gradual
deformity correction using the ilizarov technique followed by the
second-stage internal fixation in an elderly patient with
osteoporosis. Geriatr Orthop Surg Rehabil.
11(2151459320931673)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Zhang Q, Kang Y, Wu Y, Ma Y, Jia X, Zhang
M, Lin F and Rui Y: Masquelet combined with free-flap technique
versus the Ilizarov bone transport technique for severe composite
tibial and soft-tissue defects. Injury: Apr 4, 2024 (Epub ahead of
print).
|
|
35
|
Feng D, Zhang Y, Jia H, Xu G, Wu W, Yang
F, Ding J, Li D, Wang K, Luo Y, et al: Complications analysis of
Ilizarov bone transport technique in the treatment of tibial bone
defects-a retrospective study of 199 cases. BMC Musculoskelet
Disord. 24(864)2023.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Gülaydin A and Sarierler M: Treatment of
long bone fractures in calves with ilizarov external fixator. Vet
Comp Orthop Traumatol. 31:364–372. 2018.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Ding Z, Zhu X, Fu K and Zheng X: Digital
lengthening to treat finger deficiency: An experience of 201 digits
in 104 patients. Biomed Res Int. 2017(4934280)2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Baruah RK: Modified Ilizarov in difficult
Fracture of the Patella. A case report. J Orthop Case Rep. 6:26–28.
2016.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Johnson WO, Sellon JL, Moore BJ, Levy BA,
Lachman N and Finnoff JT: Ultrasound-Guided iliopsoas tendon
release: A cadaveric investigation. PM R. 13:397–404.
2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Faucher GK, Daruwalla JH and Seiler JG
III: Complications of surgical release\break of carpal tunnel
Syndrome: A systematic review. J Surg Orthop Adv. 26:18–24.
2017.PubMed/NCBI
|