Introduction
Endoscopic retrograde cholangiopancreatography
(ERCP) is widely used as an important diagnostic and therapeutic
procedure for pancreaticobiliary disease (1). The success rate of the procedure in
patients with normal anatomy is 90-95% (2). However, ERCP in patients with
surgically altered anatomy is challenging due to the difficulty in
accessing the afferent limb, cannulation of a papilla or
biliopancreatoenteric anastomosis with a reverse orientation, and
the difficulty in performing therapeutic interventions (3,4).
Among all types of reconstruction, Roux-en-Y
gastrectomy is one of the most difficult types of reconstruction.
During ERCP in patients with Roux-en-Y gastrectomy, entering the
afferent limb of the Y anastomosis is difficult due to the long
afferent limb length, sharp angulation and severe adhesion
(3-5).
Additionally, the position of the native papilla in Roux-en-Y
gastrectomy markedly differs from that of the normal anatomy, which
may increase the difficulty of bile duct cannulation (3,5).
Since balloon enteroscope-assisted ERCP was first
successfully performed in a patient with Roux-en-Y
choledochojejunostomy reconstruction in 2005(6), it has been demonstrated to be a
useful tool in the management of patients with surgically altered
anatomy (7). However, the balloon
enteroscope has a 200-cm working length with a small working
channel diameter (3.2 mm), which limits the use of numerous
commercial ERCP accessories, for example, the sphincterotome
(5). The short-type balloon
enteroscope has been introduced for patients with surgically
altered anatomy, and this allows the use of conventional ERCP
accessories (8,9). However, the technique is not readily
available in all centers and trained personnel are needed, limiting
its routine use (8,9).
Despite expert hands performing the procedure, the
results of Roux-en-Y reconstruction in previous studies were not
satisfactory when using various endoscopes (3-5).
Based on our practical experience, the pediatric colonoscope is
suitable for performing ERCP in patients with Roux-en-Y gastrectomy
and an intact major duodenal papilla. The pediatric endoscope is
flexible, with a 3.2-cm working channel diameter and 135-cm working
length, while maintaining a slim outer diameter (9.9 mm). This type
of endoscope is available in almost all centers and provides access
to the afferent limb; it also enables the use of conventional ERCP
accessories.
However, limited data are available regarding the
outcomes of pediatric colonoscope-assisted ERCP in patients with
Roux-en-Y gastrectomy. The present study evaluated the efficacy of
using a pediatric colonoscope in patients with Roux-en-Y
gastrectomy and an intact major duodenal papilla.
Materials and methods
Patients
Consecutive patients with Roux-en-Y gastrectomy and
an intact major duodenal papilla who underwent ERCP using a
pediatric colonoscope at the Medical Center for Digestive Diseases,
The Second Affiliated Hospital of Nanjing Medical University
(Nanjing, China) between January 2018 and December 2022 were
retrospectively reviewed. Patients with coagulation disorders,
severe cardiopulmonary insufficiency and age <18 or >86 years
were excluded. Data were extracted from the medical records and
endoscopy database. These data included patient demographics,
postsurgical anatomy, indications for ERCP, endoscopic findings and
therapies, exploration time, and procedural complications.
The present retrospective study was approved by the
Ethics Committee of The Second Affiliated Hospital of Nanjing
Medical University [approval no. (2022)-KY-122-02]. Written
informed consent was obtained from each patient before ERCP. All
patients provided written informed consent for publication.
Methods
All procedures were performed under conscious
sedation with dexmedetomidine and fentanyl or under general
anesthesia, according to the judgment of the anesthesiologist, and
vital signs were continuously monitored. The patients were placed
in the supine or left lateral position, and CO2
insufflation was used in all cases. ERCP was performed with a
pediatric colonoscope (PCF-Q260JI; Olympus Corporation). A
transparent cap (D-201-11802; Olympus Corporation) was attached to
the tip of the pediatric colonoscope for enhanced visualization of
endoscope insertion and to facilitate bile duct cannulation.
After reaching the esophagojejunal or gastrojejunal
anastomosis, the pediatric colonoscope was inserted into the Roux
limb to find the Roux-en-Y anastomosis, where one limb was selected
for insertion of the pediatric colonoscope after using a clip fixed
to the mucosa of the limb as a marker. Fluoroscopy was used to
identify the afferent limb as it led to the upper abdomen. When the
pediatric colonoscope is passed down the lower abdomen, it
naturally locates in the efferent limb. On this occasion, the
pediatric colonoscope was drawn back to the Roux-en-Y anastomosis,
and changed to the other limb (the afferent limb). Any difficulties
with endoscope insertion due to looping or long scope length
prompted changes in the patient position or compression of the
abdomen.
When selective bile duct cannulation failed and the
pancreatic duct was cannulated, the double-guidewire technique was
used with another guidewire. The sphincterotome (TRI-25M-P; Cook
Medical) was reinserted along the first guidewire after reloading
with the second guidewire to attempt cannulation of the bile duct.
After successful bile duct cannulation, the pancreatic wire was
removed or a pancreatic stent (Zimmon; Cook) was inserted by the
first guidewire. Otherwise, the precut technique was used with a
sphincterotome or a needle-knife (KD-441Q or KD-10Q-1; Olympus
Corporation). The procedure was terminated when bile duct
cannulation could not be achieved despite the use of various
techniques for ~30 min.
Treatment was performed using standard ERCP
therapeutic accessories, including the guidewire, sphincterotome,
balloon dilator, basket or retrieval balloon and biliary stent. The
endoscopic sphincterotomy (EST) was performed in the 11 to 12
o'clock position of the papilla, and minor EST (3-5 mm) was
performed. Stones were removed from the common bile duct with a
basket or a retrieval balloon. In the case of biliary strictures or
difficult bile duct stones, a plastic stent (Flextent; Changzhou
New District Garson Medical Stent Apparatus Co., Ltd.) or
self-expandable metal stent (Wallstent; Boston Scientific
Corporation) was inserted, depending on the situation.
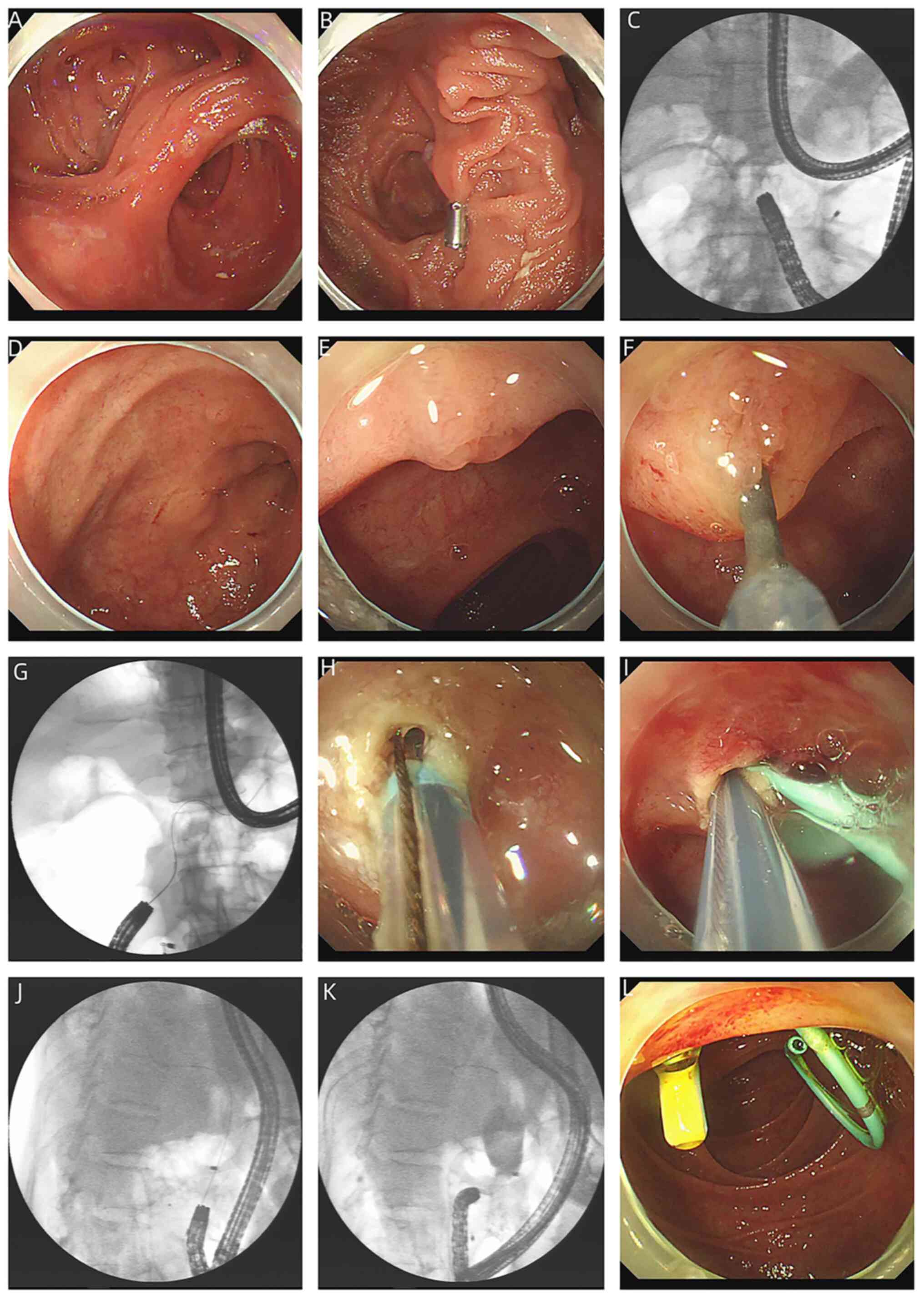
The procedure of ERCP using a pediatric colonoscope
in total gastrectomy with Roux-en-Y reconstruction is shown in
Fig. 1.
Definitions
The success of endoscope insertion was defined by
access to the afferent limb and identification of the papilla.
Endoscopic cannulation success was defined as successful bile duct
cannulation and cholangiography, whereas therapeutic ERCP success
was defined as the ability to successfully perform stone extraction
or stent placement for strictures. Clinical intervention success
was defined as successful completion of the intended treatment
(stone extraction and stent placement) after successful endoscope
insertion.
The endoscope insertion time was defined as the time
from the insertion of the scope into the mouth of the patient to
papilla identification. The ERCP procedure time was defined as the
time from the insertion of the scope into the mouth of the patient
to the complete withdrawal of the scope from the mouth of the
patient. Standard cannulation was defined by the non-use of
advanced methods such as precut or double-guidewire techniques.
ERCP complications, including cholangitis,
pancreatitis, bleeding and perforation, were defined according to
standard criteria (10,11). Data, including success of endoscope
insertion, endoscopic cannulation success, clinical intervention
success, the endoscope insertion time, the ERCP procedure time and
ERCP complications, were collected from patients over a 2-week
follow-up period after the procedure.
Statistical analysis
Statistical analysis was performed using SPSS
version 25.0 (IBM Corp.). The χ2 test or Fisher's exact
test was used to compare categorical variables, while
independent-samples Student's t-test was used to compare continuous
variables. Variables with a P-value <0.05 in univariate analysis
were included in the model of binary logistic regression analysis.
Statistical analysis was performed using SPSS statistical software
(version 25; IBM Corp.). P<0.05 was considered to indicate a
statistically significant difference.
Results
A total of 93 patients (32 female patients and 61
male patients) with Roux-en-Y gastrectomy underwent ERCP using a
pediatric colonoscope at the Medical Center for Digestive Diseases,
The Second Affiliated Hospital of Nanjing Medical University,
between January 2018 and December 2022. The mean age of the
patients was 67.35±9.45 years (range, 18-86 years). Distal
gastrectomy with Roux-en-Y reconstruction was performed in 38
patients, while total gastrectomy with Roux-en-Y reconstruction was
performed in 55 patients. The indication for all procedures was
common bile duct stones (77 patients) or biliary strictures (16
patients), which were previously confirmed by magnetic resonance
cholangiopancreatography or CT. A total of 57, 33 and 3 patients
underwent one, two and three abdominal surgeries previously,
respectively. Table I shows the
demographic, postsurgical anatomical, clinical and endoscopic
characteristics of the patients.
 | Table IClinical and endoscopic
characteristics of the patients (n=93). |
Table I
Clinical and endoscopic
characteristics of the patients (n=93).
| Characteristics | Value |
|---|
| Sex, n
(male/female) | 61/32 |
| Age,
yearsa | 67.35±9.45 |
| Indications of ERCP,
n | |
|
Common bile
duct stones | 77 |
|
Biliary
strictures | 16 |
| Stone diameter,
cma | 0.95±0.31 |
| Postsurgical anatomy,
n | |
|
Distal
gastrectomy | 38 |
|
Total
gastrectomy | 55 |
| Number of previous
abdominal surgeries, n | |
|
1 | 57 |
|
2 | 33 |
|
3 | 3 |
In the present study, the major papilla was reached
successfully in 82 patients, while the major papilla was not
successfully reached in 11 patients. Therefore, the endoscope
insertion success rate was 88.17% (82/93). One of the 11 failures
was attributed to the obstruction of the afferent limb, whereas 8
failures were due to adhesion and sharp angulation, and the
afferent limb was not reached in 2 patients due to intolerance. Of
the 11 patients with unsuccessful endoscope insertion, 2 underwent
a second ERCP with a double-balloon enteroscope, which was
successful, 3 underwent surgery successfully, 4 underwent
percutaneous transhepatic papillary balloon dilation and
anterograde stone extraction successfully, and 2 were treated
conservatively.
Sex, age, mode of anesthesia, postsurgical anatomy
and the number of previous abdominal surgeries were further
analyzed. The results showed that age and number of previous
abdominal surgeries were associated with the endoscope insertion
success rate (P<0.05). Binary logistic regression analysis was
used to explore these variables. The results showed that age and
number of previous abdominal surgeries were independent risk
factors associated with endoscope insertion failure. The risk of
failure was higher in younger patients or those who had a history
of two to three abdominal surgeries. The results of endoscope
insertion are shown in Tables II
and III.
 | Table IISuccess or failure of endoscope
insertion (n=93). |
Table II
Success or failure of endoscope
insertion (n=93).
| Characteristics | Success (n=82) | Failure (n=11) | P-value |
|---|
| Male, n (%) | 55 (67.07) | 6 (54.55) | 0.503 |
| Age,
yearsa | 68.20±9.44 | 61.09±7.11 | 0.018 |
| Anesthesia method,
n | | | >0.999 |
|
Conscious
sedation | 62 | 8 | |
|
General
anesthesia | 20 | 3 | |
| Postsurgical
anatomy, n | | | 0.754 |
|
Distal
gastrectomy | 33 | 5 | |
|
Total
gastrectomy | 49 | 6 | |
| Number of previous
abdominal surgeries, n | | | 0.001 |
|
1 | 55 | 2 | |
|
2 | 26 | 7 | |
|
3 | 1 | 2 | |
 | Table IIIBinary logistic regression analysis
of factors involved in endoscope insertion failure. |
Table III
Binary logistic regression analysis
of factors involved in endoscope insertion failure.
|
Characteristics | OR (95% CI) | P-value |
|---|
| Age (<60
years) | 1.129
(1.024-1.244) | 0.014 |
| Number of previous
abdominal surgeries | | |
|
1 | 1.000 | |
|
2 | 0.089
(0.014-0.577) | 0.011 |
|
3 | 0.009
(0.000-0.209) | 0.003 |
Selective bile duct cannulation was achieved in 70
of the 82 patients when the major papilla was reached successfully,
thus the endoscopic cannulation success rate was 85.37% (70/82). Of
the 70 patients, 48 underwent standard cannulation, while 10 were
treated with the precut technique and 12 were exposed to the
double-guidewire technique. Selective bile duct cannulation was not
completed in 12 patients due to an unfavorable orientation of the
papilla or intolerance to the procedure. Among them, 1 patient
underwent endoscopic ultrasonography-guided biliary drainage
(EUS-BD) successfully, 3 patients underwent percutaneous
transhepatic papillary balloon dilation and anterograde stone
extraction successfully, 2 patients underwent percutaneous
transhepatic biliary drainage and the ERCP rendezvous technique
successfully, 4 patients underwent surgery, and 2 patients were
treated conservatively.
Stone extraction or stent placement was performed
successfully in 67 out of 70 patients who had achieved bile duct
cannulation and cholangiography. Of the 67 patients, 64 underwent
sphincterotomy, 53 were treated with endoscopic papillary balloon
dilation, 55 underwent stone extraction and 12 were stented. A
total of 44 patients underwent endoscopic papillary balloon
dilatation (EPBD) and 12 patients underwent endoscopic papillary
large balloon dilatation (EPLBD), without any bleeding episodes or
perforation. A total of 3 patients with common bile duct stones
failed to complete the intended treatment. A total of 2 patients
underwent stent placement due to stone impaction, while 1 patient
was stented due to oxygen desaturation during the procedure.
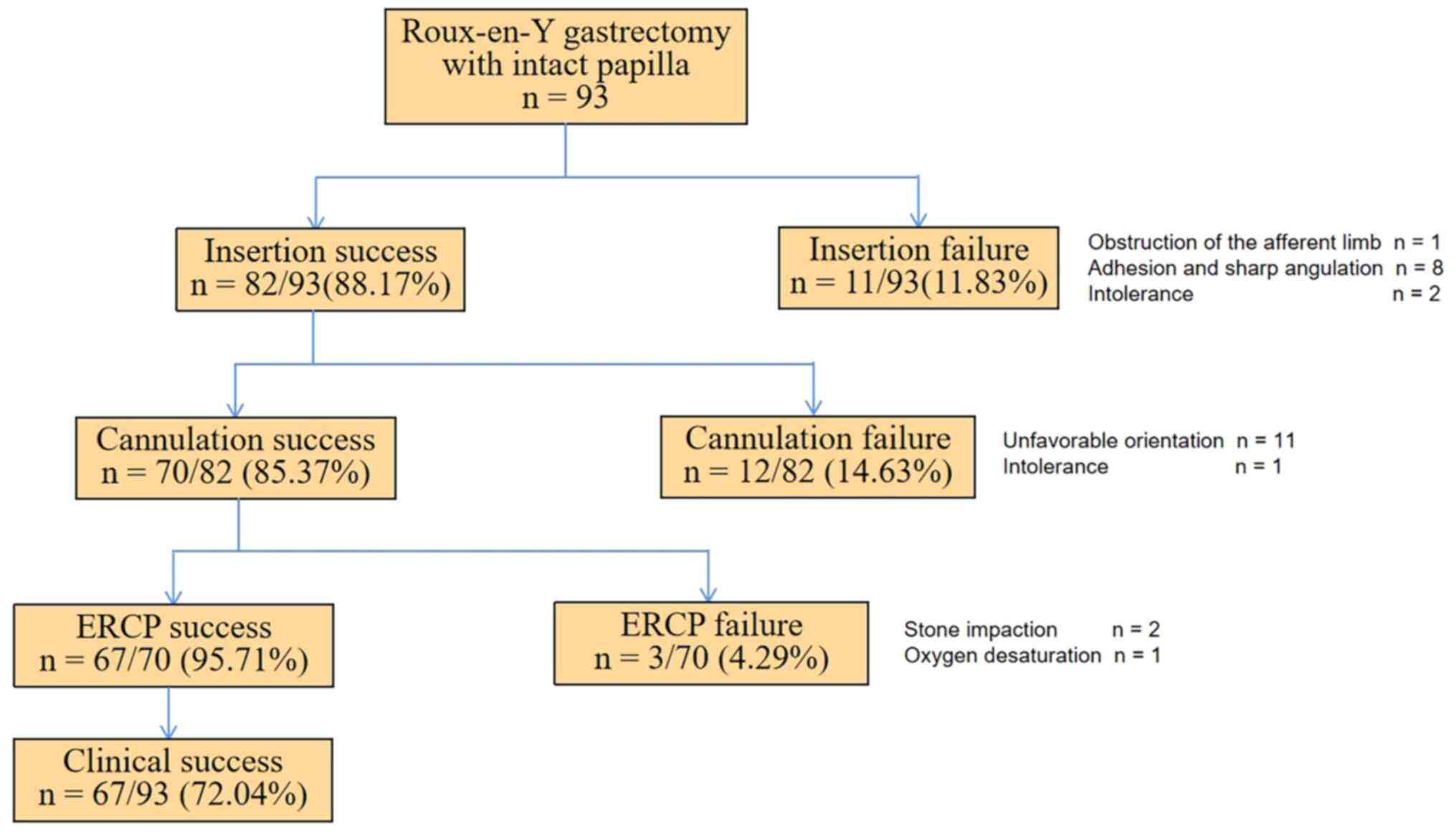
The present results demonstrated that the success
rates of endoscope insertion, endoscopic cannulation, therapeutic
ERCP and clinical intervention were 88.17% (82/93), 85.37% (70/82),
95.71% (67/70) and 72.04% (67/93), respectively. The endoscope
insertion time was 40.78±10.04 min, while the ERCP procedure time
was 88.55±16.38 min. Among the 93 patients, minor reverse EST was
performed in 67 patients in total, and no bleeding or perforation
was detected. Only 5 patients exhibited mild-to-moderate post-ERCP
pancreatitis, while 2 patients exhibited cholangitis. All patients
were managed with conventional therapy (including anti-infection
and nutrition support). The complication rate was 7.53% (7/93)
(Table IV).
 | Table IVClinical outcomes. |
Table IV
Clinical outcomes.
| Outcomes | Total (n=93) | Distal gastrectomy
(n=38) | Total gastrectomy
(n=55) | P-value |
|---|
| Endoscope insertion
success rate, %a | 88.17 (82/93) | 86.84 (33/38) | 89.09 (49/55) | 0.754 |
| Endoscopic
cannulation success rate, %a | 85.37 (70/82) | 87.88 (29/33) | 83.67 (41/49) | 0.834 |
| Therapeutic ERCP
success rate, %a | 95.71 (67/70) | 96.55 (28/29) | 95.12 (39/41) | >0.999 |
| Clinical
intervention success rate, %a | 72.04 (67/93) | 73.68 (28/38) | 70.91 (39/55) | 0.769 |
| Endoscope insertion
time, minb | 40.78±10.04 | 43.42±10.66 | 38.96±9.25 | 0.035 |
| ERCP procedure
time, minb | 88.55±16.38 | 93.68±18.48 | 85.00±13.84 | 0.011 |
| Complications,
n | | | | 0.429 |
|
Perforation | 0 | 0 | 0 | |
|
Pancreatitis | 5 | 2 | 3 | |
|
Bleeding | 0 | 0 | 0 | |
|
Cholangitis | 2 | 1 | 1 | |
The aforementioned variables were further compared
between patients undergoing distal gastrectomy with Roux-en-Y
reconstruction and patients undergoing total gastrectomy with
Roux-en-Y reconstruction. The results revealed no significant
differences in the success rates of endoscope insertion, endoscopic
cannulation and therapeutic ERCP, or in the rates of clinical
intervention success and complications, between the two groups.
However, the endoscope insertion and ERCP procedure times in
patients with distal gastrectomy were significantly longer than
those in patients who underwent total gastrectomy. These clinical
outcomes are presented in Table
IV. A summary of the ERCP results is shown in Fig. 2.
Discussion
Among the different types of postsurgical anatomy
encountered in clinical settings, Roux-en-Y gastrectomy is one of
the most difficult reconstructions. ERCP in these patients is a
greater challenge not only due to the long and tortuous afferent
limb of the Y anastomosis, but also due to the presence of the
native papilla, which is difficult to cannulate (12-14).
Only a few studies with small sample sizes have been
published on this subject, and the success rates were different
(12-14).
The present study evaluated the effect of using a pediatric
colonoscope in patients undergoing distal and total gastrectomy
with Roux-en-Y reconstruction and, to the best of our knowledge, it
is the largest study to date involving this type of postsurgical
anatomy.
At present, there is no consensus regarding the
optimal position of the patient during surgery. The supine position
or the left lateral position facilitates access to the afferent
limb, and also enables manual abdominal compression and enhances
the safety of patient sedation (15). The position of the patient is
changed if endoscope insertion is difficult or X-ray localization
is needed during the procedure. However, studies have demonstrated
that some endoscopists naturally place the patient in the prone
position (16,17), whereas others prefer the supine
position (18). All patients
received ERCP >3 months later after the gastrectomy. We consider
this to be safe, as ERCP is minimally invasive and low risk.
In the present study, the success rate of endoscope
insertion was 88.17% (82/93). Among the 11 patients with insertion
failure, the main reason was adhesion and sharp angulation of the
afferent limb (8/11). The risk of failure was increased in younger
patients or patients with a history of two to three abdominal
surgeries. The main reasons underlying endoscope insertion failure
may be adhesion and sharp angulation due to previous abdominal
surgeries and intolerance in younger patients. The variables were
further compared between patients undergoing distal gastrectomy
with Roux-en-Y reconstruction and patients undergoing total
gastrectomy with Roux-en-Y reconstruction. The results revealed
that the endoscope insertion and ERCP procedure times in patients
with distal gastrectomy were longer than those in patients with
total gastrectomy, potentially due to the sharp angulation at the
level of gastrojejunostomy or a long afferent limb leading to loop
formation in the gastric remnant, which complicated endoscope
insertion.
When the major papilla is identified, bile duct
cannulation is the first and most important step. The papilla of
Roux-en-Y gastrectomy is difficult to cannulate due to the reverse
position of the papilla, difficulty with scope manipulation and
improper accessories (lack of an elevator) (12-14).
Our clinical experience suggests that it is important to locate the
papilla directly, and ensure that the bile duct axis is parallel to
the line of sight. In case of failure, advanced methods such as
precut or pancreatic guidewire cannulation are indicated (19). In the present study, selective bile
duct cannulation was achieved in 70 out of 82 patients with
successful access to the major papilla. Selective bile duct
cannulation was not completed in 12 patients, primarily due to
unfavorable orientation of the papilla.
EST is the most frequently used technique, followed
by stone extraction. Based on our previous clinical experience, the
incision should be oriented toward 5 to 6 o'clock of the reverse
position of the papilla. However, it is difficult to perform EST in
the proper direction using the standard sphincterotome in patients
with Roux-en-Y gastrectomy. In the present study, minor EST was
performed in the 11 to 12 o'clock position of the major duodenal
papilla in 67 patients in total, and no bleeding or perforation was
detected. Therefore, it is safe and effective to perform minor
reverse EST in patients with Roux-en-Y gastrectomy and an intact
papilla.
EPBD is the first option for small common bile duct
stones (<8 mm), due to the low associated risk of bleeding and
perforation (20). By contrast,
EST combined with EPLBD is preferred for large and multiple common
bile duct stones (20). Several
randomized trials and systematic reviews have evaluated the
benefits and risks of EST combined with EPLBD vs. EST alone for the
removal of common bile duct stones, and the results showed that the
efficacy of the two methods was comparable, with no significant
differences in the rates of complication (21-23).
In the present study, 44 patients underwent EPBD and 12 patients
were exposed to EPLBD, without any bleeding episodes or
perforation. The present results demonstrated that EST combined
with EPLBD was safe and effective for stone extraction in patients
with Roux-en-Y gastrectomy.
Previous studies reported that the therapeutic ERCP
success rate of balloon enteroscope-assisted ERCP for Roux-en-Y
gastrectomy ranged between 57.1 and 87.8% (18,24,25),
while the therapeutic ERCP success rate of short-type
enteroscope-assisted ERCP ranged between 59.1 and 88.9% (26-28).
The present therapeutic ERCP success rate results were similar to
those of enteroscope-assisted ERCP. Although enteroscope-assisted
ERCP is a useful tool in the management of patients with surgically
altered anatomy, the procedure cannot be generalized due to its
non-availability in all the centers and the requirement for trained
personnel, equipment and special accessory devices (in the case of
long enteroscopes).
EUS-BD has emerged as an effective alternative for
biliary access when the afferent limb or the papilla cannot be
accessed (29,30). The success rate of the procedure
ranges between 67 and 98%, while the complication rate ranges
between 8.1 and 20.4% (31-34).
Although EUS-BD is associated with a high success rate, the
incidence of adverse events is still high. Furthermore, EUS-BD
cannot be used in all patients, only in those with small bile duct
stones or bile duct dilatation (31-34).
Tokuhara et al (35) conducted a large retrospective study
evaluating enteroscope-assisted ERCP procedures in >1,500
patients. The results showed that the overall complication rate was
5.8% and that the most common adverse event was perforation, which
was observed in 3.2% of patients. The perforation tended to occur
during endoscope insertion and ERCP intervention. Another
multi-center prospective study that included >300
enteroscope-assisted ERCP procedures reported a complication rate
of 10.6%, with perforation being the most common adverse event,
observed in 3.9% of all cases (36). In the present study, 5 patients
exhibited mild-to-moderate post-ERCP pancreatitis, while 2 patients
exhibited cholangitis. All patients were managed with conventional
therapy. The complication rate was 7.53% (7/93), which is
equivalent to that of conventional ERCP at 4.88-28.1% (11). The perforation rate in the present
study was 0%. This may be due to the endoscope insertion strategy.
Fluoroscopy was used to identify the afferent limb and a clip was
fixed to the mucosa of the limb as a marker. Any difficulties with
endoscope insertion due to looping or long scope length prompted
changes in the position of the patient or compression of the
abdomen. When the angulation was too sharp or the adhesion was too
severe to insert the endoscope, the procedure was stopped without
hesitation and other modalities were used instead, especially for
patients with two to three abdominal surgeries. Additionally, the
pediatric colonoscope is flexible and not as long as the
enteroscope, reducing the risk of perforation. However, the present
study was a single-center, retrospective study of <100 patients.
Complications may occur when the number of patients is
increased.
In conclusion, the present study demonstrated that
the use of a pediatric colonoscope is efficacious and safe for
conducting ERCP in patients with Roux-en-Y gastrectomy and an
intact major duodenal papilla. This technique is our preferred
approach and other endoscopists are encouraged to adopt these
innovations for the management of their patients. Although the
present study supports the use of a pediatric colonoscope in this
group of patients, further large prospective and multicenter
studies are needed to evaluate the efficacy of the intervention to
corroborate the present findings.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the National Natural
Science Foundation of China (grant no. 82171222).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
FW designed and performed the research, and wrote
the paper. LM designed the research and supervised the study. XXG,
XTD, JJN, YTW, QPL and GBJ contributed to the data analysis and
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The present retrospective study was approved by the
Ethics Committee of The Second Affiliated Hospital of Nanjing
Medical University [Nanjing, China; approval no. (2022)-KY-122-02].
Written informed consent was obtained from each patient before
endoscopic retrograde cholangiopancreatography.
Patient consent for publication
All patients provided written informed consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cotton PB: Endoscopic retrograde
cholangiopancreatography: Maximizing benefits and minimizing risks.
Gastrointest Endosc Clin N Am. 22:587–599. 2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Freeman ML and Guda NM: ERCP cannulation:
A review of reported techniques. Gastrointest Endosc. 61:112–125.
2005.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Krutsri C, Kida M, Yamauchi H, Iwai T,
Imaizumi H and Koizumi W: Current status of endoscopic retrograde
cholangiopancreatography in patients with surgically altered
anatomy. World J Gastroentero. 25:3313–3333. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Moreels TG: Techniques for endoscopic
retrograde cholangiopancreatography in altered gastrointestinal
anatomy. Curr Opin Gastroenterol. 33:339–345. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Shimatani M, Mitsuyama T, Tokuhara M,
Masuda M, Miyamoto S, Ito T, Nakamaru K, Ikeura T, Takaoka M,
Naganuma M and Okazaki K: Recent advances of endoscopic retrograde
cholangiopancreatography using balloon assisted endoscopy for
pancreaticobiliary diseases in patients with surgically altered
anatomy: Therapeutic strategy and management of difficult cases.
Dig Endosc. 33:912–923. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Haruta H, Yamamoto H, Mizuta K, Kita Y,
Uno T, Egami S, Hishikawa S, Sugano K and Kawarasaki H: A case of
successful enteroscopic balloon dilation for late anastomotic
stricture of choledochojejunostomy after living donor liver
transplantation. Liver Transpl. 11:1608–1610. 2005.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Gomez V and Petersen BT: Endoscopic
retrograde cholangiopancreatography in surgically altered anatomy.
Gastrointest Endosc Clin N Am. 25:631–656. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tanisaka Y, Ryozawa S, Mizuide M,
Kobayashi M, Fujita A, Minami K, Kobatake T, Omiya K, Iwano H and
Araki R: Usefulness of the ‘newly designed’ short-type
single-balloon enteroscope for ERCP in patients with Roux-en-Y
gastrectomy: A pilot study. Endosc Int Open. 6:E1417–E1422.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Shimatani M, Tokuhara M, Kato K, Miyamoto
S, Masuda M, Sakao M, Fukata N, Miyoshi H, Ikeura T, Takaoka M and
Okazaki K: Utility of newly developed short-type double-balloon
endoscopy for endoscopic retrograde cholangiography in
postoperative patients. J Gastroenterol Hepatol. 32:1348–1354.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Cotton PB, Eisen GM, Aabakken L, Baron TH,
Hutter MM, Jacobson BC, Mergener K, Nemcek AJ Jr, Petersen BT,
Petrini JL, et al: A lexicon for endoscopic adverse events: Report
of an ASGE workshop. Gastrointest Endosc. 71:446–454.
2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Dumonceau JM, Kapral C, Aabakken L,
Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro
M, Hritz I, Mariani A, et al: ERCP-related adverse events: European
society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy.
52:127–149. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ni JB, Zhu MY, Li K, Dai WM, Lu LG, Wan
XJ, Wan R and Cai XB: The feasibility of cap-assisted routine adult
colonoscope for therapeutic endoscopic retrograde
cholangiopancreatography in patients with Roux-en-Y reconstruction
after total gastrectomy. J Dig Dis. 22:721–726. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fugazza A, Anderloni A, Paduano D,
Badalamenti M, Maselli R, Carrara S, Gabbiadini R, Colombo M,
Spadaccini M, Cappello A, et al: Underwater cap-assisted endoscopic
retrograde cholangiopancreatography in patients with surgically
altered anatomy: A pilot study. Endoscopy. 53:927–931.
2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Nakaji S, Hirata N, Yamauchi K, Shiratori
T, Kobayashi M, Fujii H and Ishii E: Endoscopic retrograde
cholangiopancreatography using a cap-assisted highly flexible
colonoscope in patients with Roux-en-Y anastomosis. Endoscopy.
46:529–532. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Díez JE and Ramos ME: Single-balloon
enteroscopy-assisted ERCP in patients with Roux-en-Y anatomy and
choledocholithiasis: Do technical improvements mean better
outcomes? Rev Esp Enferm Dig. 112:929–934. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Wu WG, Qin LC, Song XL, Zhao MN, Zhang WJ,
Gu J, Weng H, Liu YB, Zhang Y, Qu CY, et al: Application of single
balloon enteroscopy-assisted therapeutic endoscopic retrograde
cholangiopancreatography in patients after bilioenteric Roux-en-Y
anastomosis: Experience of multi-disciplinary collaboration. World
J Gastroenterol. 25:5505–5514. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Nava LEZ, Terán-Ellis SM, Gomez SZ, Robles
EPC, Lora AL, Valdovinos AF and Méndez DP: Endoscopic retrograde
cholangiopancreatography by double-balloon enteroscopy in patients
with surgically altered gastrointestinal anatomy. Rev Esp Enferm
Dig. 112:278–283. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
De Koning M and Moreels TG: Comparison of
double-balloon and single-balloon enteroscope for therapeutic
endoscopic retrograde cholangiography after Roux-en-Y small bowel
surgery. BMC Gastroenterol. 16(98)2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Nakai Y, Kogure H, Yamada A, Isayama H and
Koike K: Endoscopic management of bile duct stones in patients with
surgically altered anatomy. Dig Endosc. 30 (Suppl 1):S67–S74.
2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kim GH, Kang DH, Song GA, Heo J, Park CH,
Ha TI, Kim KY, Lee HJ, Kim ID, Choi SH and Song CS: Endoscopic
removal of bile-duct stones by using a rotatable papillotome and a
large-balloon dilator in patients with a Billroth II gastrectomy
(with video). Gastrointest Endosc. 67:1134–1138. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Karsenti D, Coron E, Vanbiervliet G,
Privat J, Kull E, Bichard P, Perrot B, Quentin V, Duriez A, Cholet
F, et al: Complete endoscopic sphincterotomy with vs. without
large-balloon dilation for the removal of large bile duct stones:
Randomized multicenter study. Endoscopy. 49:968–976.
2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Teoh A, Cheung F, Hu B, Pan YM, Lai LH,
Chiu P, Wong S, Chan F and Lau J: Randomized trial of endoscopic
sphincterotomy with balloon dilation versus endoscopic
sphincterotomy alone for removal of bile duct stones.
Gastroenterology. 144:341–345. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kim JH, Yang MJ, Hwang JC and Yoo BM:
Endoscopic papillary large balloon dilation for the removal of bile
duct stones. World J Gastroenterol. 19:8580–8594. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Tanisaka Y, Ryozawa S, Mizuide M, Araki R,
Fujita A, Ogawa T, Tashima T, Noguchi T, Suzuki M and Katsuda H:
Status of single-balloon enteroscopy-assisted endoscopic retrograde
cholangiopancreatography in patients with surgically altered
anatomy: Systematic review and meta-analysis on biliary
interventions. Digest Endosc. 33:1034–1044. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ishii K, Itoi T, Tonozuka R, Itokawa F,
Sofuni A, Tsuchiya T, Tsuji S, Ikeuchi N, Kamada K, Umeda J, et al:
Balloon enteroscopy-assisted ERCP in patients with Roux-en-Y
gastrectomy and intact papillae (with videos). Gastrointest Endosc.
83:377–386. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Kawamura T, Uno K, Suzuki A, Mandai K,
Nakase K, Tanaka K and Yasuda K: Clinical usefulness of a
short-type, prototype single-balloon enteroscope for endoscopic
retrograde cholangiopancreatography in patients with altered
gastrointestinal anatomy: Preliminary experiences. Dig Endosc.
27:82–86. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Tanisaka Y, Ryozawa S, Mizuide M, Harada
M, Fujita A, Ogawa T, Nonaka K, Tashima T and Araki R: Analysis of
the factors involved in procedural failure: Endoscopic retrograde
cholangiopancreatography using a short-type single-balloon
enteroscope for patients with surgically altered gastrointestinal
anatomy. Dig Endosc. 31:682–689. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yane K, Katanuma A, Maguchi H, Takahashi
K, Kin T, Ikarashi S, Sano I, Yamazaki H, Kitagawa K, Yokoyama K,
et al: Short-type single-balloon enteroscope-assisted ERCP in
postsurgical altered anatomy: Potential factors affecting
procedural failure. Endoscopy. 49:69–74. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Khan MA, Akbar A, Baron TH, Khan S, Kocak
M, Alastal Y, Hammad T, Lee WM, Sofi A, Artifon EL, et al:
Endoscopic ultrasound-guided biliary drainage: A systematic review
and meta-analysis. Dig Dis Sci. 61:684–703. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wang K, Zhu J, Xing L, Wang Y, Jin Z and
Li Z: Assessment of efficacy and safety of EUS-guided biliary
drainage: A systematic review. Gastrointest Endosc. 83:1218–1227.
2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Weilert F, Binmoeller KF, Marson F, Bhat Y
and Shah JN: Endoscopic ultrasound-guided anterograde treatment of
biliary stones following gastric bypass. Endoscopy. 43:1105–1108.
2011.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Khashab MA, El ZM, Sharzehi K, Marson FP,
Haluszka O, Small AJ, Nakai Y, Park DH, Kunda R, Teoh AY, et al:
EUS-guided biliary drainage or enteroscopy-assisted ERCP in
patients with surgical anatomy and biliary obstruction: An
international comparative study. Endosc Int Open. 4:E1322–E1327.
2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
James TW, Fan YC and Baron TH: EUS-guided
hepaticoenterostomy as a portal to allow definitive antegrade
treatment of benign biliary diseases in patients with surgically
altered anatomy. Gastrointest Endosc. 88:547–554. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Mukai S, Itoi T, Sofuni A, Tsuchiya T,
Tanaka R, Tonozuka R, Honjo M, Fujita M, Yamamoto K and Nagakawa Y:
EUS-guided antegrade intervention for benign biliary diseases in
patients with surgically altered anatomy (with videos).
Gastrointest Endosc. 89:399–407. 2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Tokuhara M, Shimatani M, Mitsuyama T,
Masuda M, Ito T, Miyamoto S, Fukata N, Miyoshi H, Ikeura T, Takaoka
M, et al: Evaluation of complications after endoscopic retrograde
cholangiopancreatography using a short type double balloon
endoscope in patients with altered gastrointestinal anatomy: A
single-center retrospective study of 1,576 procedures. J
Gastroenterol Hepatol. 35:1387–1396. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Shimatani M, Hatanaka H, Kogure H,
Tsutsumi K, Kawashima H, Hanada K, Matsuda T, Fujita T, Takaoka M,
Yano T, et al: Diagnostic and therapeutic endoscopic retrograde
cholangiography using a short-type double-balloon endoscope in
patients with altered gastrointestinal anatomy: A multicenter
prospective study in Japan. Am J Gastroenterol. 111:1750–1758.
2016.PubMed/NCBI View Article : Google Scholar
|