Introduction
Cardiac arrest remains one of the most urgent
medical emergencies worldwide, with out-of-hospital cardiac arrest
(OHCA) presenting a particular challenge due to its unpredictable
nature and the need for immediate intervention (1). The American Heart Association reports
that over 350,000 OHCAs occur in the United States annually
(2) with similar higher burden in
Europe (3), with survival rates
significantly impacted by the quality and timeliness of
cardiopulmonary resuscitation (CPR) administered.
CPR, a lifesaving technique crucial in the
management of cardiac arrest, has traditionally been performed
manually (4). Manual CPR,
involving rhythmic chest compressions and ventilations, aims to
maintain circulatory flow and oxygenation until advanced care can
be provided (4). However, the
effectiveness of manual CPR can be limited by various factors,
including the physical endurance of the rescuer, consistency in
compression depth and rate, and interruptions during patient
transfer or transport (5).
In recent years, mechanical CPR devices have emerged
as a potential solution to these limitations. These devices are
designed to deliver consistent, uninterrupted chest compressions
and are increasingly being used in pre-hospital settings (6). Proponents of mechanical CPR argue
that these devices offer several advantages over manual methods,
including the ability to provide high-quality compressions over
prolonged periods, reduced rescuer fatigue, and greater consistency
in compression depth and rate (7).
Additionally, mechanical devices potentially reduce interruptions
in chest compressions, a factor closely linked to improved survival
rates in cardiac arrest cases (7).
However, the adoption of mechanical CPR in OHCA
scenarios has been met with mixed responses from the medical
community. While some studies suggest improved outcomes with
mechanical CPR (8,9), others indicate no significant
difference or even inferior results compared with manual methods
(10,11). This discrepancy raises critical
questions about the comparative effectiveness of these two
approaches, particularly in the context of OHCA where every second
counts.
Several factors necessitate a comparative analysis
between these two methods. First, the choice between mechanical and
manual CPR can significantly impact patient outcomes, particularly
in terms of survival to hospital discharge and long-term survival
(8-11).
Second, understanding the relative benefits and limitations of each
method can inform training protocols and guidelines for emergency
medical services (EMS). Finally, with the evolving landscape of
pre-hospital emergency care and the continuous development of new
CPR technologies, it is crucial to periodically reassess and update
best practice recommendations.
The objective of the present meta-analysis was to
comprehensively evaluate and compare the effectiveness of
mechanical and manual CPR methods in improving survival outcomes in
patients experiencing OHCA.
Materials and methods
Eligibility criteria of
participants
Studies conducted in participants aged ≥18 years who
had OHCA were included.
Intervention and control group
Studies comparing the mechanical CPR using any
device against manual mode of CPR were eligible.
Outcomes
Return of spontaneous circulation (ROSC), survival
till admission, survival till discharge.
Design of the study
Studies of any of the following designs: Randomized
controlled trials (RCTs), quasi-experimental trials, non-randomized
studies or any form of interventional trials with comparison group
were eligible.
Exclusion criteria
To ensure the robustness and relevance of the
present meta-analysis, the following exclusion criteria were
applied:
Animal studies. Studies conducted on animals
were excluded to focus exclusively on human data.
Case reports and series. Individual case
reports or case series were excluded as they do not provide
comparative data between mechanical and manual CPR.
Studies with insufficient data. Studies that
did not report sufficient data on the outcomes of interest (ROSC,
survival to admission, and survival till discharge) were
excluded.
Overlapping data. Duplicate publications or
studies with overlapping data were carefully screened, and only the
most comprehensive or recent study was included.
Information sources and search
strategy
The search strategy employed a comprehensive
approach to identify relevant studies, utilizing databases such as
PubMed (https://pubmed.ncbi.nlm.nih.gov/), Scopus (https://www.scopus.com/home.uri), Cochrane
library (https://www.cochranelibrary.com/), Google Scholar
(https://scholar.google.com/),
(ScienceDirect) https://www.sciencedirect.com/ and Web of Science
(https://clarivate.com), along with the references
of the included studies. A combination of the following terms was
used, including ‘Mechanical CPR’, ‘Manual CPR’, ‘Cardiopulmonary
resuscitation’, ‘Out-of-hospital cardiac arrest’, ‘Prehospital
CPR’, ‘Randomized Controlled Trial’, ‘Autopulse’ and ‘LUCAS-2’. The
time limit of the search started from the inception of each of the
databases till December 2023. There were no restrictions in terms
of language during the search.
Search strategy in PubMed was as follows:
[‘Mechanical CPR’ (All Fields) OR ‘Mechanical Cardiopulmonary
Resuscitation’ (All Fields) OR ‘Mechanical Chest Compression’ (All
Fields) OR ‘Autopulse’ (All Fields) OR ‘LUCAS-2’(All Fields)] AND
[‘Manual CPR’(All Fields) OR ‘Manual Cardiopulmonary
Resuscitation’(All Fields) OR ‘Manual Chest Compression’(All
Fields)] AND [‘Out-of-Hospital Cardiac Arrest’(All Fields) OR
‘Prehospital Cardiac Arrest’(All Fields) OR ‘OHCA’(All Fields) OR
‘Cardiac Arrest’(All Fields)].
Study screening process
Two independent researchers thoroughly reviewed the
literature, initially assessing the relevance of each study by
examining its title, abstract and essential key words.
Subsequently, they obtained the full-text versions of articles for
a more detailed evaluation. The suitability of these studies for
inclusion in the analysis was determined based on pre-established
criteria. In cases where inconsistencies or disagreements arose
regarding the selection of a study, the two researchers worked
together to discuss and resolve these differences through
consensus. If consensus could not be reached, a third-party expert,
who was not an author of the present study but had expertise in the
field, was consulted to provide an independent assessment and
resolve the disagreement. This process ensured the methodological
integrity and reliability of the study selection process. To ensure
methodological integrity, the entire review process was documented
following the PRISMA guidelines (12).
Data extraction
The principal investigator meticulously gathered
critical data from the selected studies, recording fundamental
details such as extraction date, study titles and author names. Key
methodological elements were also noted, including the design of
each study, participant demographics, and the specific context in
which the study was conducted. Particular attention was paid to
recording the number of participants in each arm of the studies,
along with the baseline and final outcome measures, and the
criteria used for including or excluding participants. Information
about interventions, comparison groups, and the length of follow-up
periods was systematically logged. This included details of primary
and secondary outcomes, the timing of evaluations, and other
factors crucial for assessing the quality of the studies. To
maintain the accuracy of the data collection process, a second
researcher rigorously cross-checked the extracted information
against the original reports, ensuring the reliability of the
compiled data.
Risk of bias assessment
The assessment of study quality was conducted by two
evaluators using two specific bias assessment instruments. For
RCTs, they employed the Cochrane Collaboration's Risk of Bias 2
tool, (13) which evaluates
potential biases across several domains. These domains include the
process of randomization, deviations from the planned
interventions, the handling of missing outcome data, the
measurement of outcomes, and the selection of reported results. For
non-randomized studies, the reviewers used the Risk Of Bias In
non-randomized studies-of interventions (ROBINS-I) tool (14). This tool focuses on biases related
to confounding factors, selection of participants, classification
of interventions, deviations from intended interventions, missing
data, outcome measurements, and the reporting of results. Based on
these evaluations, studies were classified into categories
indicating ‘low’, ‘high’, or ‘some concerns’ regarding their risk
of bias. This categorization ensured a thorough and rigorous
quality appraisal of the evidence gathered.
Statistical analysis
The statistical analysis for the present study was
performed using STATA, version 14.2. (StataCorp LP). As all the
outcomes were measured in binary terms, the pooled odds ratio (OR)
was computed along with a 95% CI, based on the frequency of events
in both intervention and control groups, offering a comparative
perspective on the effectiveness of interventions.
A random-effects model was applied, utilizing the
inverse variance method to accommodate variations across the
included studies (15). To
evaluate heterogeneity, or the variability in results across
studies, several methods were used: Visual inspection of forest
plots to observe CI overlaps, chi-square tests, and the
I2 statistic, the latter quantifying the proportion of
total variation due to differences between studies.
For assessing publication bias, several techniques
were employed. Egger's test was used to detect asymmetry in the
data, indicative of potential bias. Funnel plots provided a visual
assessment of bias, plotting the treatment effects measured in the
studies against their precision. The Doi plot and Luis Furuya
Kanamori (LFK) index were also utilized to further explore and
quantify potential publication bias (16). The LFK index between -1 to +1
indicate no publication bias (perfect symmetry), while between -1
to -2 or +1 to +2 indicate minor asymmetry, while value less than
-2 and more than +2 indicate major asymmetry (16). To address and minimize the impact
of publication bias, the trim and fill method was utilized in
addition to traditional methods. The trim and fill analysis were
conducted using a random-effects model to adjust for the detected
publication bias.
Subgroup analysis was performed based on study
design and type of mechanical device to identify any variations in
outcomes related to different study methodologies. Sensitivity
analysis was performed to assess the robustness of the estimates by
excluding high risk of bias studies. Leave-one out sensitivity
analysis was also conducted to assess the single-study effects for
each of the outcomes.
GRADE assessment
The Grading of Recommendations, Assessment,
Development, and Evaluations (GRADE) approach plays a crucial role
in assessing the quality of evidence in healthcare research
(17). This method employs five
key domains to evaluate the strength and reliability of evidence.
Each domain addresses specific aspects of the studies under
consideration, providing a comprehensive overview of their
credibility (17).
Risk of bias assessment
This domain examines the extent to which the study
design and implementation minimize biases. It considers factors
such as randomization, blinding, and the completeness of outcome
data. Studies with a high risk of bias are considered less reliable
and can result in downgrading the quality of evidence.
Inconsistency
Inconsistency refers to the degree of variation in
the results across different studies. Significant heterogeneity in
outcomes can indicate underlying differences in study populations,
interventions, or methodologies, leading to questions about the
applicability of results. A high level of inconsistency may lead to
a lower GRADE rating.
Indirectness
This domain assesses the extent to which the
evidence directly applies to the population, intervention,
comparator, and outcomes of interest in the specific research
question. Studies with high indirectness, meaning their focus or
methods diverge significantly from the research question, are less
likely to contribute to a high-quality evidence base.
Imprecision
Imprecision evaluates the confidence in the effect
estimates provided by the evidence. It takes into account the
sample size, confidence intervals (CIs), and the number of events.
Studies with wide CIs or small sample sizes are considered
imprecise, potentially leading to a downgrade in the quality of
evidence.
Publication bias
This domain investigates the presence of selective
publication of studies, often those with positive findings. Tools
such as funnel plots, Egger's test and other statistical methods
are used to assess this bias. Evidence of publication bias can
significantly affect the trustworthiness of the evidence pool and
may result in lowering the GRADE.
By meticulously evaluating each of these domains,
the GRADE approach provides a systematic and transparent method to
assess the quality of evidence. This rigorous process ensures that
healthcare recommendations are based on the most reliable and
relevant information available.
Results
Search results
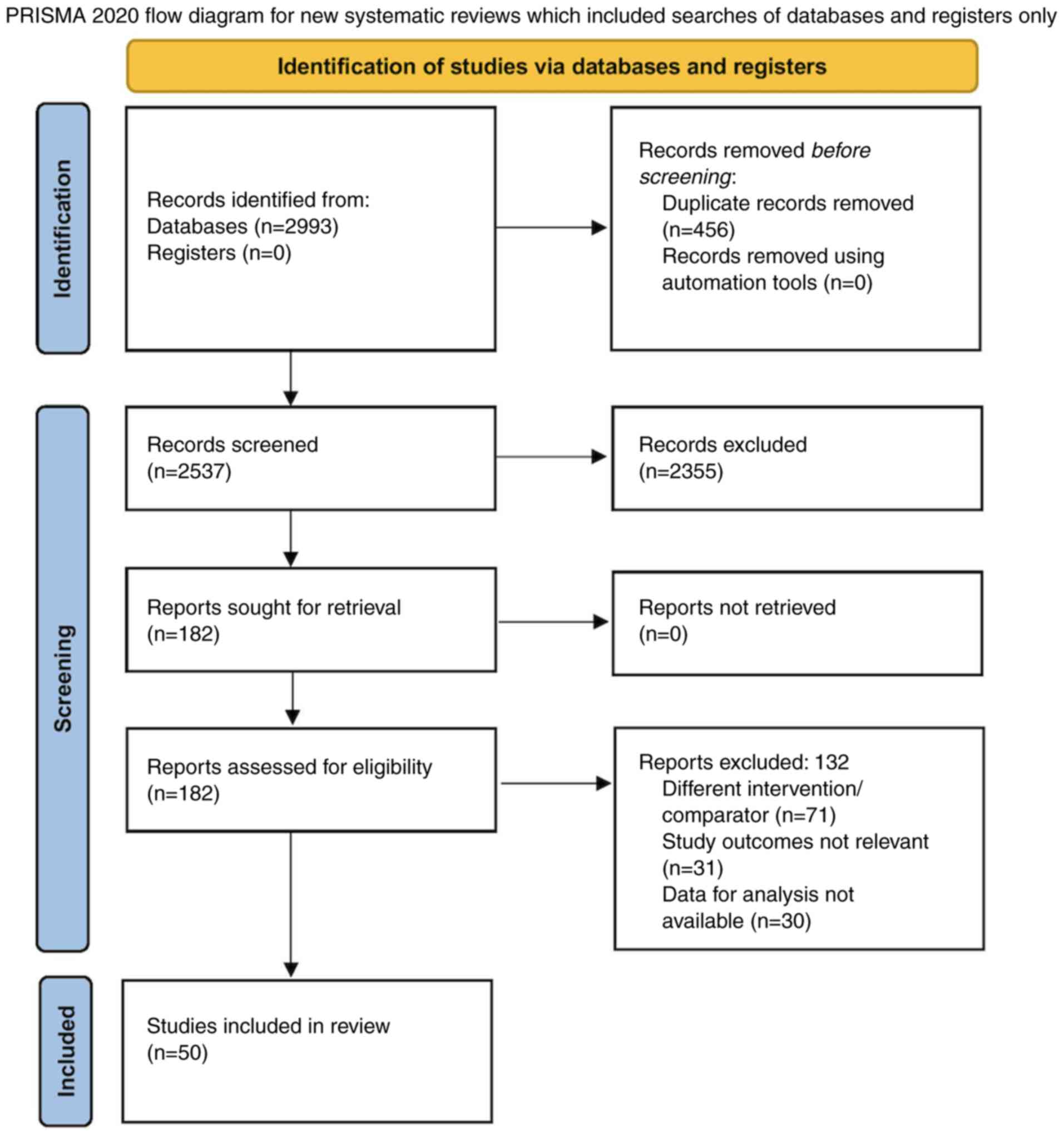
Overall, a total of 2,993 studies were obtained from
PubMed, Scopus, Cochrane library, Google Scholar, ScienceDirect and
Web of Science. A total of 182 studies were initially found
eligible based on reading of title and abstract and the full texts
were obtained for these studies. Finally, 50 studies were eligible
after reading full text and included in analysis (Fig. 1) (18-67).
Characteristics of included
studies
The present meta-analysis encompassed 50 studies
with varied designs including 11 RCTs, 15 prospective cohorts and
24 retrospective cohorts or case-controls. The total sample size
across these studies ranged significantly, from as few as 17
participants in the smallest study to as numerous as 80,690 in the
largest. Geographically, the majority of studies were conducted in
the United States, with significant contributions from European and
Asian countries. The most commonly used mechanical CPR devices were
the LUCAS and Autopulse systems, which were predominant across
these studies. The studies exhibited diverse levels of risk of
bias: 17 with a high risk, 26 with a low risk, and 7 with some
concerns (Table I).
 | Table ICharacteristics of the included
studies (N=50). |
Table I
Characteristics of the included
studies (N=50).
| Author and
Year | Study design | Country | Nation wide
Study | Sample Size
(overall) | Sample size in
mechanical CPR | Sample size in
manual CPR | Type of mechanical
device | CPR guideline | Risk of bias | (Refs) |
|---|
| Ahn et al,
2023 | Prospective
cohort | Korea | No | 3,519 | 2,759 | 760 | NR | NR | Low | (43) |
| Anantharaman et
al, 2017 | Cluster RCT | Singapore | No | 1,191 | 302 | 889 | LUCAS | 2010 ILCOR | Some concerns | (44) |
| Axelsson et
al, 2006 | Prospective
cohort | Sweden | No | 210 | 105 | 105 | LUCAS | 2000 AHA | Low | (23) |
| Axelsson et
al, 2013 | Retrospective
cohort | Sweden | No | 1,165 | 702 | 463 | LUCAS | NR | High | (29) |
| Buckler et
al, 2016 | Retrospective
cohort | USA | No | 80,690 | 17,625 | 63,065 | NR | NR | High | (21) |
| Canakci et
al, 2021 | Non-RCT | | No | 178 | 47 | 131 | LUCAS-2 | NR | Low | (63) |
| Casner et
al, 2005 | Retrospective
cohort | USA | No | 162 | 69 | 93 | Autopulse | NR | Low | (49) |
| Chen et al,
2021 | Retrospective
cohort | Taiwan | No | 552 | 279 | 273 | LUCAS | 2015 AHA | High | (48) |
| de Wilde et
al, 2008 | Prospective | Netherlands | No | 220 | 102 | 118 | LUCAS | NR | Low | (58) |
| Dickinson et
al, 1998 | RCT | USA | No | 17 | 7 | 10 | Thumper | NR | High | (27) |
| Gao et al,
2016 | Cluster RCT | China | No | 133 | 69 | 64 | Autopulse | 2010 AHA | Some concerns | (24) |
| Halhalli et
al, 2020 | Retrospective | Turkey | No | 818 | 473 | 345 | LUCAS | NR | High | (47) |
| Hallstrom et
al, 2006 | Cluster RCT | USA and Canada | No | 767 | 394 | 373 | Autopulse | 2000 AHA | Some concerns | (34) |
| Hardig et
al, 2017 | RCT | Sweden | No | 757 | 374 | 383 | LUCAS | NR | Low | (42) |
| Hayasida et
al, 2017 | Prospective | Japan | No | 6,537 | 918 | 5,619 | LUCAS and
Autopulse | NR | Low | (36) |
| Jennings et
al, 2012 | Retrospective
cohort | Australia | No | 286 | 66 | 220 | Autopulse | NR | High | (20) |
| Jin et al,
2019 | Retrospective | China | Yes | 493 | 214 | 279 | NR | NR | Low | (52) |
| Jung et al,
2019 | Prospective
cohort | Korea | Yes | 31,011 | 2,357 | 28,654 |
Autopulse/LUCAS | NR | Low | (37) |
| Karasek et
al, 2020 | Prospective | Czech Republic | No | 278 | 144 | 134 | LUCAS | NR | High | (33) |
| Kim et al,
2024 | Multi-center
observational | Korea | Yes | 842 | 421 | 421 | NR | NR | Low | (45) |
| Lairet et
al, 2005 | Retrospective
review | USA | No | 406 | 49 | 357 | Autopulse | NR | High | (56) |
| Lin et al,
2015 | Retrospective
cohort | Taiwan | No | 404 | 216 | 188 | Life-Stat 1008 | NR | Low | (26) |
| Liu et al,
2016 | RCT | China | No | 71 | 33 | 38 | LUCAS | NR | Low | (62) |
| Lu et al,
2010 | RCT | China | No | 150 | 76 | 74 | Thumper modal
1007 | NR | Some concerns | (67) |
| Mastenbrook et
al, 2022 | Retrospective | USA | No | 264 | 190 | 74 | LUCAS-2 | NR | Low | (46) |
| Maule et al,
2007 | Retrospective
cohort | Belgie | No | 290 | 150 | 140 | LUCAS | NR | High | (53) |
| Morozov et
al, 2012 | Retrospective | Russia | No | 472 | 398 | 74 | Autopulse | NR | Low | (61) |
| Newberry et
al, 2018 | Retrospective
cohort | USA | No | 2,999 | 763 | 2,236 | LUCAS | NR | Low | (41) |
| Ong et al,
2006 | Prospective
cohort | USA | No | 777 | 278 | 499 | Autopulse | NR | Low | (54) |
| Ong et al,
2012 | Prospective
cohort | Singapore | No | 1,011 | 552 | 459 | Autopulse | NR | High | (30) |
| Ornato et
al, 2005 | Retrospective | USA | No | 1,086 | 79 | 1,007 | Autopulse | NR | Low | (57) |
| Paradis et
al, 2009 | Retrospective
cohort | USA | Yes | 1,020 | 729 | 291 | Autopulse | NR | Low | (59) |
| Perkins et
al, 2015 | Cluster RCT | United Kingdom | No | 4,471 | 1,652 | 2,819 | LUCAS | 2005/2010 ERC | Some concerns | (40) |
| Primi et al,
2023 | Retrospective | Italy | No | 4,292 | 2,146 | 2,146 | LUCAS, Autopulse,
Easypulse | NR | High | (51) |
| Rubertsson et
al, 2014 | RCT | Sweden, United
Kingdom, Netherlands | No | 2,589 | 1,300 | 1,289 | LUCAS | 2005 ERC | High | (39) |
| Saleem et
al, 2022 | Retrospective | Israel | No | 107 | 62 | 45 | LUCAS | NR | Low | (66) |
| Satterlee et
al, 2013 | Retrospective
cohort | USA | No | 572 | 498 | 74 | LUCAS | NR | High | (28) |
| Savastano et
al, 2019 | Prospective
cohort | Italy | No | 1,401 | 235 | 1,166 | Autopulse | NR | Low | (32) |
| Schmidbauer et
al, 2017 | Prospective
cohort | Sweden | Yes | 13,922 | 6,961 | 6,961 | LUCAS | 2010 ERC | Low | (50) |
| Seewald et
al, 2019 | Retrospective
cohort | Germany | Yes | 17,957 | 872 | 17,085 |
LUCAS/Autopulse | NR | High | (18) |
| Smekal et
al, 2011 | RCT | Sweden | No | 148 | 75 | 73 | LUCAS | 2000 ERC | Some concerns | (19) |
| Steinmetz et
al, 2008 | Retrospective
case-control | Denmark | No | 419 | 77 | 342 | Autopulse | NR | Low | (31) |
| Swanson et
al, 2006 | Retrospective
review | USA | No | 876 | 269 | 607 | Autopulse | AHA 2000 | High | (55) |
| Takayama et
al, 2023 | Retrospective | Japan | No | 1,101 | 319 | 782 | LUCAS-3 | 2015 or 2020 AHA
and ERC Guidelines | Low | (64) |
| Tantarattanapong
et al, 2022 | Retrospective
cohort | Thailand | No | 168 | 32 | 136 | LUCAS-3 | 2015 AHA | Low | (25) |
| Truhlar et
al, 2010 | Prospective | Czech Republic | No | 30 | 19 | 11 |
LUCAS/Autopulse | NR | Low | (60) |
| Ujvárosy et
al, 2018 | Retrospective
cohort | Hungary | No | 287 | 55 | 232 | LUCAS | NR | High | (22) |
| Viniol et
al, 2020 | Retrospective | Germany | No | 64 | 32 | 32 | Autopulse | Recommendations of
the European Council for Resuscitation | Low | (65) |
| Wik et al,
2014 | RCT | Norway | No | 4,231 | 2,099 | 2,132 | Autopulse | 2005 ERC/AHA | Low | (35) |
| Zeiner et
al, 2015 | Prospective
cohort | Austria | No | 938 | 283 | 655 |
LUCAS/Autopulse | NR | Low | (38) |
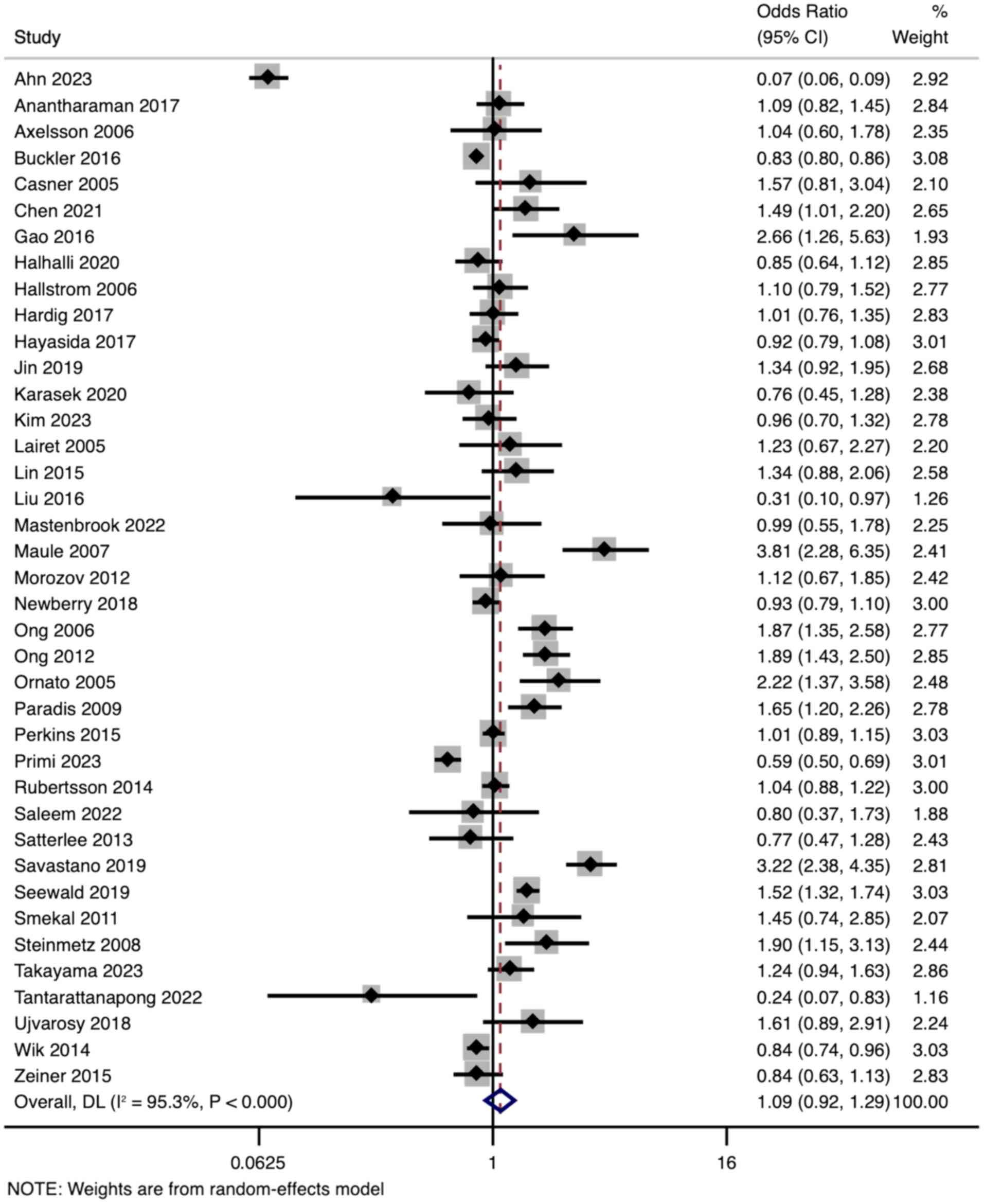
ROSC
A total of 39 studies with 144,430 participants have
compared the effectiveness of mechanical against manual CPR on ROSC
amongst patients with OHCA. Pooled OR was 1.09, with 95% CI ranging
from 0.92 to 1.29 (Fig. 2). The
analysis demonstrated a non-significant overall effect (P=0.31),
suggesting that there is no conclusive difference between
mechanical and manual CPR on ROSC. There was substantial
heterogeneity among the studies, as evidenced by an I² value of
95.3%. Subgroup analysis based on study design did not reveal any
difference in the extent and direction of the pooled effect size
(Fig. S1). The pooled estimates
from both RCTs and non-RCTs revealed non-significant difference
between mechanical and manual CPR in terms of ROSC. Subgroup
analysis based on type of mechanical device revealed that the
Autopulse subgroup had the most pronounced effect with an OR of
1.63 (95% CI: 1.20 to 2.22; Fig.
S2).
Funnel plot (Fig.
S3) revealed an asymmetrical plot, indicating the possibility
of publication bias. Egger's test was performed to confirm these
findings and it was found that the coefficient for the slope is
-0.21 with a standard error of 0.09. This slope coefficient
represents the relationship between the effect sizes and their
precision (inversely related to the standard error). A negative
coefficient suggests a trend where smaller studies (with larger
standard errors) tend to report larger effect sizes. The P=0.02,
which is less than the conventional threshold of 0.05, indicating
that the relationship is statistically significant. This suggests
that there is evidence of small-study effects in the data.
The bias coefficient (intercept) is 1.56 with a
standard error of 0.97, and a P=0.12. This P≥0.05, indicating that
the bias coefficient is not statistically significant. This means
that while there is a trend for smaller studies to report larger
effects, it is not strong enough to conclusively indicate
publication bias. The overall P-value for the test of no
small-study effects is 0.12. This is above the conventional alpha
level of 0.05, suggesting that there is no significant evidence of
small-study effects. However, since the value is relatively close
to 0.05, it warrants cautious interpretation and suggests a
possible but not definitive presence of small-study effects.
Since the funnel plot and Egger's test provided
inconclusive evidence, Doi plot and LFK index was performed to
obtain conclusive evidence on publication bias. The Doi plot
(Fig. S4) revealed major
asymmetry which was further confirmed by higher LFK index of 2.62.
Using the trim and fill method, the adjusted random-effects pooled
estimate of the effect size (ES) shifted to 0.835 (95% CI: 0.712 to
0.979, P=0.027; Fig. S5). This
suggests that after adjusting for publication bias, the results
indicate a significant effect, highlighting the potential impact of
publication bias on the initial analysis. The leave-one out
sensitivity analysis and exclusion of high risk of bias studies did
not reveal any significant change either in the form of magnitude
or the direction of association.
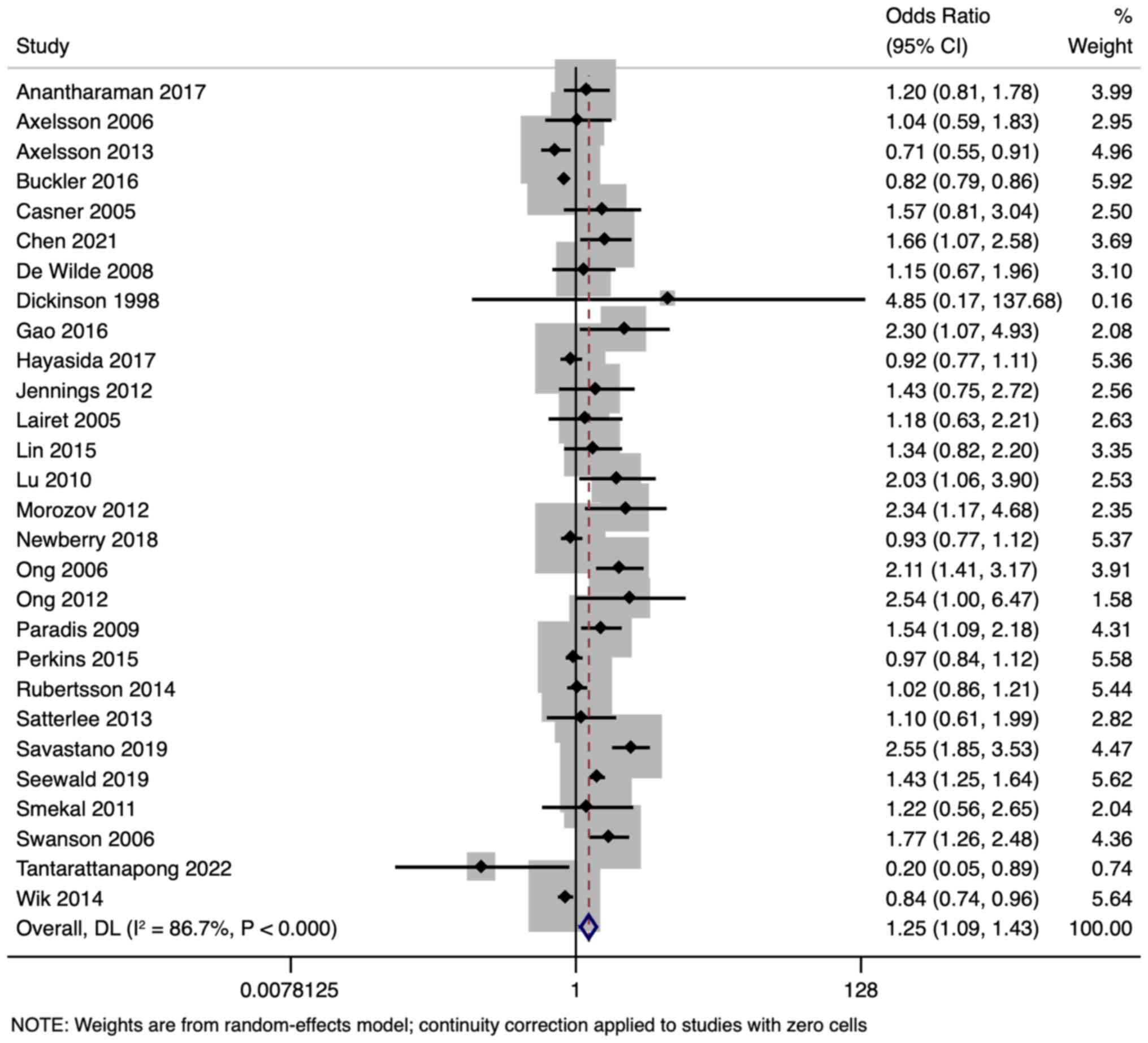
Survival to admission
A total of 28 studies with 130,499 participants have
compared the effectiveness of mechanical against manual CPR on
survival till admission amongst patients with OHCA. Pooled OR was
1.25, with 95% CI ranging from 1.09 to 1.43 (Fig. 3). The analysis demonstrated a
significant overall effect (P=0.001), suggesting that there is a
significant positive effect of mechanical against manual CPR on
survival to admission. There was substantial heterogeneity among
the studies, as evidenced by an I² value of 86.7%. Subgroup
analysis based on study design revealed a significant difference in
the extent and direction of the pooled ES (Fig. S6). The pooled estimates from RCTs
did not demonstrate a significant effect (pooled OR=1.06; 95% CI:
0.90 to 1.26), while non-RCTs revealed significant difference
between mechanical and manual CPR (pooled OR=1.30; 95% CI: 1.07 to
1.57). Subgroup analysis based on type of mechanical device
(Fig. S7) revealed that the
Autopulse subgroup revealed a significantly positive effect, with
an OR of 1.7, within CI of 1.21 to 2.37.
Funnel plot (Fig.
S8) revealed a clear asymmetrical plot with Egger's test
confirming the presence of publication bias with highly significant
P<0.001. The Doi plot (Fig.
S9) revealed major asymmetry which was further confirmed by
higher LFK index=5.79. Using the trim and fill method, the adjusted
random-effects pooled estimate of the ES shifted to 1.096 (95% CI:
0.963 to 1.248, P=0.164) (Fig.
S10). The leave-one out sensitivity analysis and exclusion of
high risk of bias did not reveal any significant change either in
the form of magnitude or the direction of association.
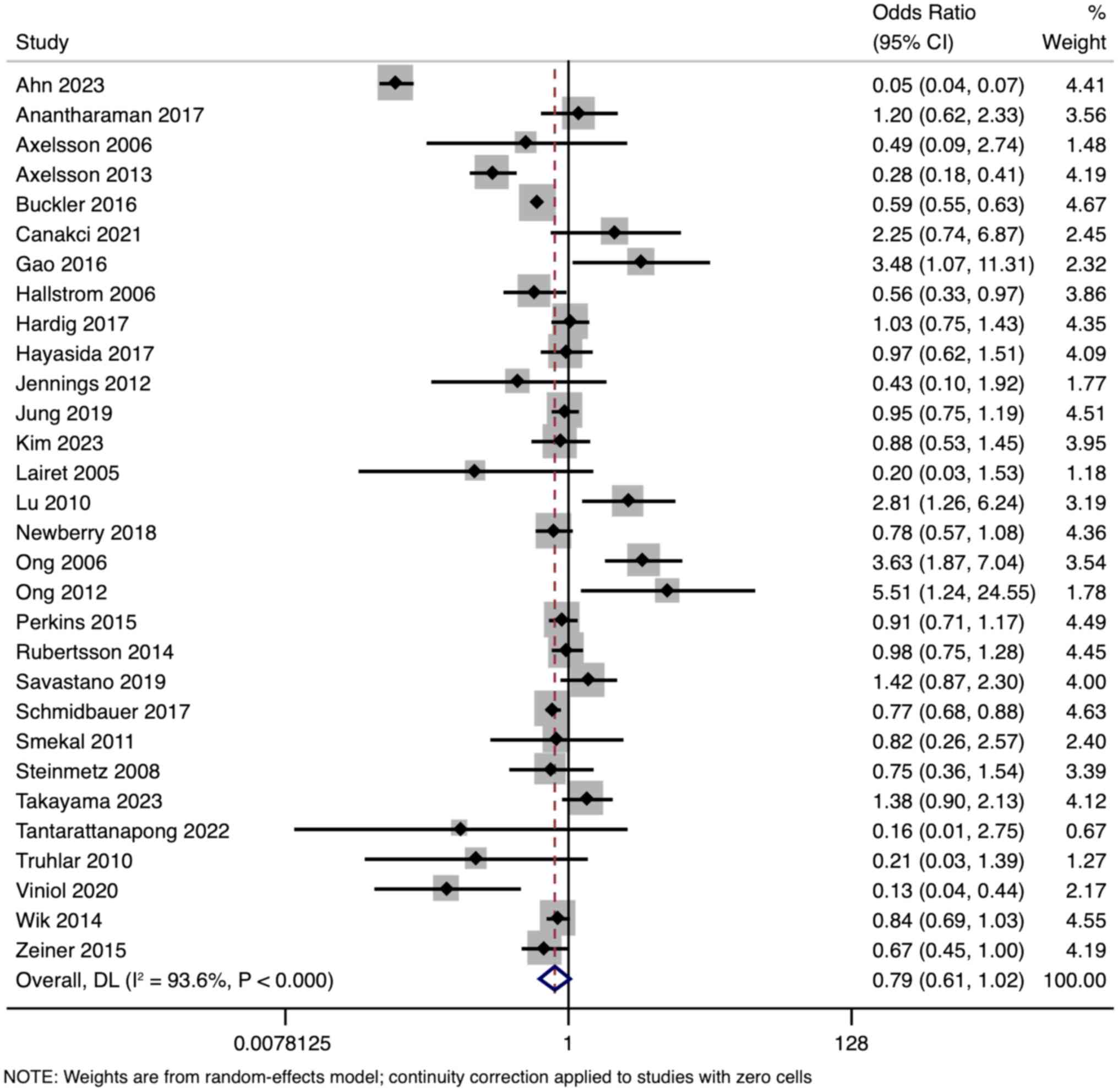
Survival till discharge
A total of 30 studies with 162,088 participants have
compared the effectiveness of mechanical against manual CPR on
survival till discharge amongst patients with OHCA. Pooled OR was
0.79, with 95% CI ranging from 0.61 to 1.02 (Fig. 4). The analysis demonstrated a
non-significant overall effect (P=0.08), suggesting that there is
no conclusive difference between mechanical and manual CPR on
survival till discharge. There was substantial heterogeneity among
the studies, as evidenced by an I² value of 93.6%. Subgroup
analysis based on study design revealed a significant difference in
the extent and direction of the pooled ES (Fig. S11). The pooled estimates from
RCTs did not demonstrate a significant effect (pooled OR=0.99; 95%
CI: 0.81 to 1.22), while non-RCTs revealed significant difference
between mechanical and manual CPR (pooled OR=0.67; 95% CI: 0.48 to
0.94). Subgroup analysis based on type of mechanical device
(Fig. S12) revealed that LUCAS
subgroup was the only one showing statistically significant
difference, with an OR of 0.78 (95% CI: 0.61 to 0.99).
Funnel plot (Fig.
S13) demonstrated a symmetrical plot with Egger's test showing
the absence of publication bias with non-significant P=0.37. The
Doi plot (Fig. S14) demonstrated
minor asymmetry which was further confirmed by higher LFK=1.33. The
leave-one out sensitivity analysis and exclusion of high risk of
bias did not reveal any significant change either in the form of
magnitude or the direction of association.
GRADE assessment results
The GRADE assessment of the present study for the
three outcomes studied, began with an initial classification of the
evidence as ‘low quality’. This starting point was chosen due to
the inclusion of observational studies, which inherently carry a
higher risk of bias compared with RCTs.
Risk of bias
A significant concern in the analysis of the present
study was the risk of bias. For some of the studies, this risk was
deemed high, leading to a downgrade in the quality of evidence to
‘very low’. The high risk of bias in these studies stemmed from
methodological issues that could potentially affect the validity of
their findings.
Indirectness of evidence
Another critical factor was the indirectness of the
evidence, particularly concerning the study design as there is
inclusion of different study designs in the review. However,
appropriate subgroup analysis was performed and separate estimates
are provided and hence, there is no need to downgrade based on
indirectness of the evidence.
Imprecision
For the outcome of survival until admission, there
was no imprecision observed. The CIs were robust, and there was no
crossing of the null value, which meant that there was no need for
a downgrade in this domain. However, for the other two
outcomes-ROSC and survival until discharge-the CIs did cross the
null value. This crossing indicated a level of imprecision,
necessitating a single downgrade in the quality of evidence for
these outcomes.
Heterogeneity
All outcomes exhibited significant heterogeneity.
While the subgroup analysis explained some of this variability, it
did not account for all of it. This unexplained heterogeneity led
to a further downgrade in the quality of evidence.
Publication bias
Finally, the assessment of the present study
revealed the presence of publication bias across all outcomes. This
bias was evidenced by the Egger's test results and visual
inspection of the funnel plots. The presence of publication bias
introduces a systematic error that could skew the overall findings,
leading to a further downgrade in the quality of evidence.
Overall quality of evidence
Considering these factors, the overall quality of
the evidence for all three outcomes was determined to be ‘very
low’. The cumulative impact of the high risk of bias in some
studies, the imprecision in certain outcomes, the significant
heterogeneity, and the presence of publication bias all contributed
to this final assessment. The ‘very low’ quality rating indicates
that there is substantial uncertainty about the accuracy of the
effect estimates for these outcomes.
Discussion
The present meta-analysis, encompassing a
comprehensive examination of the effectiveness of mechanical vs.
manual CPR in patients with OHCA, offers critical insights into
three primary outcomes: ROSC, survival to admission and survival
till discharge. For ROSC, 39 studies involving 144,430 participants
indicated no statistically significant difference between
mechanical and manual CPR. This finding suggests that mechanical
CPR does not confer a significant advantage over manual CPR in
improving the likelihood of ROSC in OHCA. The substantial
heterogeneity observed and the inconclusive evidence of publication
bias further complicate the interpretation of this outcome.
For ROSC, previous reviews on this topic has also
reported no significant difference between mechanical and manual
CPR, consistent with the findings of the present study (8-11).
However, the present analysis adds to the existing body of
knowledge by incorporating a larger sample size and more recent
studies, providing a more comprehensive overview. The absence of a
significant difference between mechanical and manual CPR in
achieving ROSC can be attributed to several factors. Mechanical CPR
devices are designed to deliver consistent, uninterrupted chest
compressions, theoretically offering an advantage over manual CPR,
where fatigue and variability in compression quality are concerns
(7). However, the transition from
manual to mechanical CPR involves a pause, potentially negating the
benefits of consistency. Furthermore, the mechanical nature of
these devices may not adequately adjust to individual patient
anatomies or the dynamic physiological conditions during
resuscitation, possibly impacting their efficacy (68).
In terms of survival to admission, 28 studies with
130,499 participants revealed a significant positive effect of
mechanical CPR over manual CPR. This result is of particular
interest as it indicates a potential advantage of mechanical CPR in
the initial stages post-resuscitation. However, the high
heterogeneity and the clear evidence of publication bias identified
necessitate cautious interpretation. The findings of the present
study for survival to admission were in line with several previous
reviews (8-11,69)
that did identify a significant advantage of mechanical over manual
CPR in the early post-resuscitation period.
The observed advantage of mechanical CPR in
improving survival to admission could be due to the sustained and
consistent quality of compressions, particularly important during
transport and in prolonged resuscitation efforts where manual CPR
effectiveness may wane due to rescuer fatigue. Mechanical CPR
ensures a constant compression depth and rate, which are critical
in the early stages of cardiac arrest management (7). This consistency could lead to
improved coronary perfusion and short-term outcomes, such as
survival to admission.
For survival till discharge, data from 30 studies
involving 162,088 participants did not reveal a conclusive
difference between the two CPR methods. This outcome aligns with
the findings for ROSC, suggesting that the long-term benefits of
mechanical CPR in improving survival rates may not be significantly
different from manual methods (8-11,69).
The lack of a significant difference in survival
till discharge between mechanical and manual CPR suggests that
while mechanical devices may offer short-term benefits, these do
not necessarily translate into long-term survival advantages. This
outcome might reflect the multifactorial nature of long-term
survival post-cardiac arrest, where factors such as the quality of
post-resuscitation care, underlying health conditions, and the
initial cause of the cardiac arrest play significant roles
(70,71).
The variations in findings across different studies
and outcomes can be attributed to several factors. The type of
mechanical CPR device used, the training and experience of the
personnel administering CPR, and the specific circumstances of each
cardiac arrest incident (such as the location and cause of arrest)
are all likely to influence outcomes. Additionally, the high degree
of heterogeneity observed in the present study and others
underscores the complexity of comparing mechanical and manual CPR
across diverse clinical settings and populations. The alignment of
the present study and deviation from previous literature highlight
the ongoing debate and the need for further research in this field.
The mixed results across different outcomes suggest that the
effectiveness of mechanical vs. manual CPR may vary depending on
the specific context and metrics of success being measured.
Strengths and limitations of the
study
The present meta-analysis included a substantial
number of studies and participants, enhancing the statistical power
and generalizability of the findings. By incorporating both RCTs
and non-RCTs, the study provided a broad overview of the existing
evidence. The use of advanced statistical tools such as Egger's
test, Doi plot and LFK index added robustness to the present
study's assessment of publication bias and data synthesis. However,
significant heterogeneity was observed among the studies,
potentially impacting the consistency and applicability of the
findings. Indications of publication bias, particularly in some
outcomes, could have skewed the results. Differences in the types
of mechanical CPR devices used and variations in manual CPR
technique across studies may have influenced the outcomes. Most
studies focused on immediate or short-term outcomes, with less
emphasis on long-term survival.
The high heterogeneity observed in the present
meta-analysis can be attributed to several factors. The present
analysis included a mix of RCTs, quasi-experimental trials,
non-randomized studies, and observational studies. The
methodological differences across these study designs contribute to
heterogeneity. Various mechanical CPR devices, such as LUCAS and
AutoPulse, were used across the studies. These devices have
different operational mechanisms and efficacy, which could lead to
variability in outcomes. Differences in the demographics and
clinical characteristics of study populations, such as age,
comorbidities and initial cardiac arrest rhythms, can significantly
affect the results and contribute to heterogeneity. The context in
which CPR was administered, including pre-hospital settings vs.
in-hospital settings, and variations in EMS protocols, can also
influence the outcomes and add to heterogeneity. Variability in the
definitions and measurements of outcomes, such as ROSC, survival to
admission and survival till discharge, across different studies,
can lead to inconsistencies in the results. A significant number of
included studies exhibited a high risk of bias.
This high risk of bias could influence the
reliability and validity of the findings and should be considered
when interpreting the results. The presence of publication bias,
particularly in the survival to admission outcome, is a significant
concern in this meta-analysis. Publication bias can lead to an
overestimation of the effectiveness of mechanical CPR due to the
preferential publication of studies with positive results. This
bias impacts the study's conclusions by potentially skewing the
overall effect estimates and reducing the reliability of the
findings. Another limitation of the present review is that the
authors focussed mainly on the short-term outcomes, while the
long-term outcomes were not considered for the review.
The GRADE approach was used to assess the quality of
evidence, and the very low quality of evidence for all outcomes
raises questions about the strength of the recommendations that can
be made based on this analysis. The implications of this
low-quality evidence on clinical practice are significant. The very
low quality of evidence suggests that there is substantial
uncertainty about the effect estimates, making it difficult to draw
definitive conclusions or provide strong clinical recommendations.
Clinicians should be cautious when interpreting these findings and
consider them as part of a broader clinical context that includes
individual patient circumstances, available resources and other
relevant clinical guidelines.
To overcome these limitations and enhance the
evidence base, future studies should aim to standardize study
designs and methodologies. Conducting more RCTs with similar
protocols can help reduce heterogeneity and provide more robust
evidence. Studies should aim to use the same type of mechanical CPR
device or, at the very least, provide detailed descriptions and
comparisons of the devices used. This will help in improved
understanding of the efficacy of specific devices. Ensuring
homogeneity in study populations by setting clear inclusion and
exclusion criteria can help minimize variability. Stratifying
results based on key demographic and clinical characteristics can
also provide more nuanced insights. Adopting standardized
definitions and measurement criteria for outcomes across studies
can reduce discrepancies and improve the comparability of
results.
Implications for clinical practice and
research
Given the very low quality of evidence and the
significant heterogeneity observed in this meta-analysis,
translating these findings into clinical practice requires careful
consideration. The variability in study designs, populations and
intervention protocols complicates the generalizability of the
results. Despite these limitations, some suggestions can be made
regarding the potential contexts in which mechanical CPR might be
preferred over manual CPR. Mechanical CPR may be more effective
during prolonged resuscitation efforts where consistent,
high-quality compressions are critical, and rescuer fatigue is a
significant concern. During patient transport, mechanical CPR can
provide continuous and consistent chest compressions, which are
challenging to maintain manually. It can be used in situations
where limited personnel is available to perform high-quality manual
CPR, mechanical devices can ensure the delivery of effective
compressions, in settings with well-trained staff in
high-performance CPR may observe less difference between manual and
mechanical methods, but in less controlled environments, mechanical
CPR might offer more consistent results.
Given the current evidence, clinicians should weigh
these factors and consider individual patient circumstances,
available resources, and existing clinical guidelines when deciding
between mechanical and manual CPR. Further research with
higher-quality studies is needed to provide more definitive
recommendations and to improve understanding of the specific
contexts in which mechanical CPR may be most beneficial. Future
studies should report the training level uniformly in their trials,
ensuring that the reviews can undertake separate subgroup analysis
based on training level of the healthcare providers. Finally, the
current review focusses exclusively on short term outcomes, and
hence the future reviews can focus on the long-term outcomes
between these interventions.
Given the variability in outcomes, a personalized
approach to CPR, considering patient-specific factors such as the
underlying cause of arrest and physiological differences, is
crucial. Since the long-term survival benefits of mechanical CPR
are not significantly different from manual CPR, emphasis should
also be placed on the quality of post-resuscitation care, including
advanced cardiac life support and critical care management.
Further studies should explore the physiological and
biomechanical mechanisms behind the effectiveness of different CPR
methods to enhance understanding and improve techniques. Research
should also focus on the development and testing of new CPR
technologies, including more advanced mechanical devices that can
better adapt to patient-specific needs and resuscitation
scenarios.
The present study underscored the complexity of CPR
methods in OHCA and the importance of context in choosing between
mechanical and manual CPR. It highlights the need for ongoing
research and training in both methods, ensuring that healthcare
providers are equipped to make the best decisions for their
patients. Ultimately, the goal is to improve the outcomes of OHCA
patients, making every second and every action count in these
critical situations.
Supplementary Material
Subgroup analysis based on study
design for ROSC in Out-of-Hospital Cardiac Arrest. This figure
provides a subgroup analysis of ROSC outcomes, comparing mechanical
and manual cardiopulmonary resuscitation across different study
designs (RCTs and non-RCTs), showing pooled estimates and effect
sizes. ROSC, return of spontaneous circulation; RCTs, randomized
controlled trials; CI, confidence interval.
Subgroup analysis based on type of
mechanical device for ROSC in Out-of-Hospital Cardiac Arrest. This
figure provides a subgroup analysis of ROSC outcomes, comparing
mechanical and manual cardiopulmonary resuscitation across
different type of mechanical device, demonstrating pooled estimates
and effect sizes. ROSC, return of spontaneous circulation; CI,
confidence interval.
Funnel plot for assessing publication
bias in return of ROSC Studies. This figure presents a funnel plot
used to evaluate publication bias among the studies comparing ROSC
outcomes between mechanical and manual cardiopulmonary
resuscitation. Asymmetry in the plot indicates potential bias.
ROSC, return of spontaneous circulation.
Doi plot for assessing asymmetry in
ROSC Studies. This figure demonstrates a Doi plot used to assess
the asymmetry of the included studies on ROSC, providing an
additional method to identify publication bias, confirmed by the
Luis Furuya Kanamori index. ROSC, return of spontaneous
circulation.
Trim and fill funnel plot for
adjusting for publication bias in ROSC studies. This figure
presents a trim and fill adjusted funnel plot used to adjust for
publication bias among the studies comparing ROSC outcomes between
mechanical and manual cardiopulmonary resuscitation. ROSC, return
of spontaneous circulation.
Subgroup analysis based on study
design for survival to admission in Out-of-Hospital Cardiac Arrest.
This figure presents a subgroup analysis comparing survival to
admission outcomes between mechanical and manual cardiopulmonary
resuscitation, highlighting differences in effect sizes across RCTs
and non-RCTs. RCTs, randomized controlled trials; CI, confidence
interval.
Subgroup analysis based on type of
mechanical device for survival to admission in Out-of-Hospital
Cardiac Arrest. This figure provides a subgroup analysis of
survival to admission outcomes, comparing mechanical and manual
cardiopulmonary resuscitation across different type of mechanical
device, demonstrating pooled estimates and effect sizes. CI,
confidence interval.
Funnel plot for assessing publication
bias in survival to admission studies. This figure illustrates a
funnel plot assessing the presence of publication bias in studies
comparing survival to admission between mechanical and manual
cardiopulmonary resuscitation. Asymmetry suggests potential
bias.
Doi plot for assessing asymmetry in
survival to admission studies. This figure demonstrates a Doi plot
to evaluate asymmetry in the studies on survival to admission, with
the Luis Furuya Kanamori index indicating the degree of bias.
Trim and fill funnel plot for
adjusting for publication bias in survival to admission studies.
This figure presents a trim and fill adjusted funnel plot used to
adjust for publication bias among the studies comparing survival to
admission outcomes between mechanical and manual cardiopulmonary
resuscitation.
Subgroup analysis based on study
design for survival till discharge in Out-of-Hospital Cardiac
Arrest. This figure provides a subgroup analysis of survival until
discharge, comparing mechanical and manual cardiopulmonary
resuscitation across various study designs, and presenting pooled
estimates and effect sizes. CI, confidence interval.
Subgroup analysis based on type of
mechanical device for survival till discharge in Out-of-Hospital
Cardiac Arrest. This figure provides a subgroup analysis of
survival until discharge, comparing mechanical and manual
cardiopulmonary resuscitation across various mechanical devices,
and presenting pooled estimates and effect sizes. CI, confidence
interval.
Funnel plot for assessing publication
bias in survival till discharge studies. This figure presents a
funnel plot used to evaluate publication bias among studies
comparing survival till discharge outcomes, indicating potential
bias based on the plot's symmetry.
Doi plot for assessing asymmetry in
survival till discharge studies. This figure demonstrates a Doi
plot for assessing asymmetry in survival till discharge studies,
with the Luis Furuya Kanamori index indicating the level of
publication bias.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
XZ and JF made substantial contributions to the
conception and design of the present study, the acquisition,
analysis and interpretation of data for the present meta-analysis.
Both authors drafted the work and revised it critically for
important intellectual content. Both authors read and approved the
final manuscript and confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Committee on the Treatment of Cardiac
Arrest; Current Status and Future Directions; Board on Health
Sciences Policy and Institute of Medicine: Strategies to Improve
Cardiac Arrest Survival: A Time to Act. Graham R, McCoy MA and
Schultz AM (eds). National Academies Press, Washington, DC,
2015.
|
|
2
|
Nichol G and Soar J: Regional cardiac
resuscitation systems of care. Curr Opin Crit Care. 16:223–230.
2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Böttiger BW and Van Aken HK: Saving
100,000 lives each year in Europe. Best Pract Res Clin
Anaesthesiol. 27:291–292. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Goyal A, Sciammarella JC, Cusick AS and
Patel PH: Cardiopul-monary resuscitation. In: StatPearls
[Internet]. StatPearls Publishing, Treasure Island, FL, 2024.
|
|
5
|
Şan İ, Bekgöz B, Ergin M and Usul E:
Manual cardiopulmonary resuscitation versus mechanical
cardiopulmonary resuscitation: Which one is more effective during
ambulance transport? Turk J Emerg Med. 21:69–74. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Couper K, Smyth M and Perkins GD:
Mechanical devices for chest compression: To use or not to use?
Curr Opin Crit Care. 21:188–194. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Poole K, Couper K, Smyth MA, Yeung J and
Perkins GD: Mechanical CPR: Who? When? How? Crit Care.
22(140)2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Chiang CY, Lim KC, Lai PC, Tsai TY, Huang
YT and Tsai MJ: Comparison between prehospital mechanical
cardiopulmonary resuscitation (CPR) devices and manual CPR for
out-of-hospital cardiac arrest: A systematic review, meta-analysis,
and trial sequential analysis. J Clin Med. 11(1448)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bonnes JL, Brouwer MA, Navarese EP,
Verhaert DVM, Verheugt FWA, Smeets JLRM and de Boer MJ: Manual
cardiopulmonary resuscitation versus CPR including a mechanical
chest compression device in out-of-hospital cardiac arrest: A
comprehensive meta-analysis from randomized and observational
studies. Ann Emerg Med. 67:349–360.e3. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Tang L, Gu WJ and Wang F: Mechanical
versus manual chest compressions for out-of-hospital cardiac
arrest: A meta-analysis of randomized controlled trials. Sci Rep.
5(15635)2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zhu N, Chen Q, Jiang Z, Liao F, Kou B,
Tang H and Zhou M: A meta-analysis of the resuscitative effects of
mechanical and manual chest compression in out-of-hospital cardiac
arrest patients. Crit Care. 23(100)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. Int J Surg. 88(105906)2021.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Sterne JA, Savović J, Page MJ, Elbers RG,
Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge
SM, et al: RoB 2: A revised tool for assessing risk of bias in
randomised trials. BMJ. 366(l4898)2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Sterne JA, Hernán MA, Reeves BC, Savović
J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT,
Boutron I, et al: ROBINS-I: A tool for assessing risk of bias in
non-randomised studies of interventions. BMJ.
355(i4919)2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Cumpston M, Li T, Page MJ, Chandler J,
Welch VA, Higgins JP and Thomas J: Updated guidance for trusted
systematic reviews: A new edition of the cochrane handbook for
systematic reviews of interventions. Cochrane Database Syst Rev.
10(ED000142)2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Furuya-Kanamori L, Barendregt JJ and Doi
SAR: A new improved graphical and quantitative method for detecting
bias in meta-analysis. Int J Evid Based Healthc. 16:195–203.
2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhang Y, Coello PA, Guyatt GH, Yepes-Nuñez
JJ, Akl EA, Hazlewood G, Pardo-Hernandez H, Etxeandia-Ikobaltzeta
I, Qaseem A, Williams JW Jr, et al: GRADE guidelines: 20. Assessing
the certainty of evidence in the importance of outcomes or values
and preferences-inconsistency, imprecision, and other domains. J
Clin Epidemiol. 111:83–93. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Seewald S, Obermaier M, Lefering R, Bohn
A, Georgieff M, Muth CM, Gräsner JT, Masterson S, Scholz J and
Wnent J: Application of mechanical cardiopulmonary resuscitation
devices and their value in out-of-hospital cardiac arrest: A
retrospective analysis of the German resuscitation registry. PLoS
One. 14(e0208113)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Smekal D, Johansson J, Huzevka T and
Rubertsson S: A pilot study of mechanical chest compressions with
the LUCAS™ device in cardiopulmonary resuscitation.
Resuscitation. 82:702–706. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jennings PA, Harriss L, Bernard S, Bray J,
Walker T, Spelman T, Smith K and Cameron P: An automated CPR device
compared with standard chest compressions for out-of-hospital
resuscitation. BMC Emerg Med. 12(8)2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Buckler DG, Burke RV, Naim MY, MacPherson
A, Bradley RN, Abella BS and Rossano JW: CARES Surveillance Group.
Association of mechanical cardiopulmonary resuscitation device use
with cardiac arrest outcomes: A population-based study using the
CARES registry (cardiac arrest registry to enhance survival).
Circulation. 134:2131–2133. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ujvárosy D, Sebestyén V, Pataki T, Ötvös
T, Lőrincz I, Paragh G and Szabó Z: Cardiovascular risk factors
differently affect the survival of patients undergoing manual or
mechanical resuscitation. BMC Cardiovasc Disord.
18(227)2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Axelsson C, Nestin J, Svensson L, Axelsson
AB and Herlitz J: Clinical consequences of the introduction of
mechanical chest compression in the EMS system for treatment of
out-of-hospital cardiac arrest-a pilot study. Resuscitation.
71:47–55. 2006.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Gao C, Chen Y, Peng H, Chen Y, Zhuang Y
and Zhou S: Clinical evaluation of the AutoPulse automated chest
compression device for out-of-hospital cardiac arrest in the
northern district of Shanghai, China. Arch Med Sci. 12:563–570.
2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Tantarattanapong S and Chantaramanee K:
Comparison of sustained return of spontaneous circulation rate
between manual and mechanical chest compression in adult cardiac
arrest. Open Access Emerg Med. 14:599–608. 2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Lin CK, Huang MC, Feng YT, Jeng WH, Chung
TC, Lau YW and Cheng KI: Effectiveness of mechanical chest
compression for out-of-hospital cardiac arrest patients in an
emergency department. J Chin Med Assoc. 78:360–363. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Dickinson ET, Verdile VP, Schneider RM and
Salluzzo RF: Effectiveness of mechanical versus manual chest
compressions in out-of-hospital cardiac arrest resuscitation: A
pilot study. Am J Emerg Med. 16:289–292. 1998.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Satterlee PA, Boland LL, Johnson PJ,
Hagstrom SG, Page DI and Lick CJ: Implementation of a mechanical
chest compression device as standard equipment in a large
metropolitan ambulance service. J Emerg Med. 45:562–569.
2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Axelsson C, Herrera MJ, Fredriksson M,
Lindqvist J and Herlitz J: Implementation of mechanical chest
compression in out-of-hospital cardiac arrest in an emergency
medical service system. Am J Emerg Med. 31:1196–1200.
2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Hock Ong ME, Fook-Chong S, Annathurai A,
Ang SH, Tiah L, Yong KL, Koh ZX, Yap S and Sultana P: Improved
neurologically intact survival with the use of an automated,
load-distributing band chest compression device for cardiac arrest
presenting to the emergency department. Crit Care.
16(R144)2012.PubMed/NCBI View
Article : Google Scholar
|
|
31
|
Steinmetz J, Barnung S, Nielsen SL, Risom
M and Rasmussen LS: Improved survival after an out-of-hospital
cardiac arrest using new guidelines. Acta Anaesthesiol Scand.
52:908–913. 2008.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Savastano S, Baldi E, Palo A, Raimondi M,
Belliato M, Compagnoni S, Buratti S, Cacciatore E, Canevari F,
Iotti G, et al: Load distributing band device for mechanical chest
compressions: An Utstein-categories based analysis of survival to
hospital discharge. Int J Cardiol. 287:81–85. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Karasek J, Ostadal P, Klein F, Rechova A,
Seiner J, Strycek M, Polasek R and Widimsky P: LUCAS II device for
cardiopulmonary resuscitation in a nonselective out-of-hospital
cardiac arrest population leads to worse 30-day survival rate than
manual chest compressions. J Emerg Med. 59:673–679. 2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Hallstrom A, Rea TD, Sayre MR, Christenson
J, Anton AR, Mosesso VN Jr, Van Ottingham L, Olsufka M, Pennington
S, White LJ, et al: Manual chest compression vs use of an automated
chest compression device during resuscitation following
out-of-hospital cardiac arrest: A randomized trial. JAMA.
295:2620–2628. 2006.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Wik L, Olsen JA, Persse D, Sterz F, Lozano
M Jr, Brouwer MA, Westfall M, Souders CM, Malzer R, van Grunsven
PM, et al: Manual vs integrated automatic load-distributing band
CPR with equal survival after out of hospital cardiac arrest. The
randomized CIRC trial. Resuscitation. 85:741–748. 2014.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Hayashida K, Tagami T, Fukuda T, Suzuki M,
Yonemoto N, Kondo Y, Ogasawara T, Sakurai A, Tahara Y, Nagao K, et
al: Mechanical cardiopulmonary resuscitation and hospital survival
among adult patients with nontraumatic out-of-hospital cardiac
arrest attending the emergency department: a prospective,
multicenter, observational study in Japan [SOS-KANTO (survey of
survivors after out-of-hospital cardiac arrest in Kanto Area) 2012
study]. J Am Heart Assoc. 6(e007420)2017.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Jung E, Park JH, Lee SY, Ro YS, Hong KJ,
Song KJ, Ryu HH and Shin SD: Mechanical chest compression device
for out-of-hospital cardiac arrest: A nationwide observational
study. J Emerg Med. 58:424–431. 2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Zeiner S, Sulzgruber P, Datler P,
Keferböck M, Poppe M, Lobmeyr E, van Tulder R, Zajicek A, Buchinger
A, Polz K, et al: Mechanical chest compression does not seem to
improve outcome after out-of hospital cardiac arrest. A single
center observational trial. Resuscitation. 96:220–225.
2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Rubertsson S, Lindgren E, Smekal D,
Östlund O, Silfverstolpe J, Lichtveld RA, Boomars R, Ahlstedt B,
Skoog G, Kastberg R, et al: Mechanical chest compressions and
simultaneous defibrillation vs conventional cardiopulmonary
resuscitation in out-of-hospital cardiac arrest: The LINC
randomized trial. JAMA. 311:53–61. 2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Perkins GD, Lall R, Quinn T, Deakin CD,
Cooke MW, Horton J, Lamb SE, Slowther AM, Woollard M, Carson A, et
al: Mechanical versus manual chest compression for out-of-hospital
cardiac arrest (PARAMEDIC): A pragmatic, cluster randomised
controlled trial. Lancet. 385:947–955. 2015.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Newberry R, Redman T, Ross E, Ely R,
Saidler C, Arana A, Wampler D and Miramontes D: No benefit in
neurologic outcomes of survivors of out-of-hospital cardiac arrest
with mechanical compression device. Prehosp Emerg Care. 22:338–434.
2018.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Hardig BM, Lindgren E, Östlund O, Herlitz
J, Karlsten R and Rubertsson S: Outcome among VF/VT patients in the
LINC (LUCAS IN cardiac arrest) trial-A randomised, controlled
trial. Resuscitation. 115:155–162. 2017.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Ahn JY, Ryoo HW, Moon S, Jung H, Park J,
Lee WK, Kim JY, Lee DE, Kim JH and Lee SH: Prehospital factors
associated with out-of-hospital cardiac arrest outcomes in a
metropolitan city: A 4-year multicenter study. BMC Emerg Med.
23(125)2023.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Anantharaman V, Ng BL, Ang SH, Lee CY,
Leong SH, Ong ME, Chua SJ, Rabind AC, Anjali NB and Hao Y: Prompt
use of mechanical cardiopulmonary resuscitation in out-of-hospital
cardiac arrest: The MECCA study report. Singapore Med J.
58:424–431. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Kim HJ, Lee D, Moon HJ, Jeong D, Shin TY,
In Hong S and Lee HJ: Korean Cardiac Arrest Research Consortium
(KoCARC) Investigators. Real-world comparison between mechanical
and manual cardiopulmonary resuscitation during the COVID-19
pandemic. Am J Emerg Med. 76:217–224. 2024.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Mastenbrook J, Redinger KE, Vos D and
Dickson C: Retrospective comparison of prehospital sustained return
of spontaneous circulation (ROSC) rates within a single basic life
support jurisdiction using manual vs lund university cardiac assist
system (LUCAS-2) mechanical cardiopulmonary resuscitation. Cureus.
14(e26131)2022.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Halhalli HC, Şancı E and Uslu T: The
comparison of manual and mechanical chest compression on survival
and long-term neurological outcome of nontraumatic out-of-hospital
cardiac arrest patients. J Emerg Med. 59:680–686. 2020.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Chen YR, Liao CJ, Huang HC, Tsai CH, Su
YS, Liu CH, Hsu CF and Tsai MJ: The effect of implementing
mechanical cardiopulmonary resuscitation devices on out-of-hospital
cardiac arrest patients in an urban city of Taiwan. Int J Environ
Res Public Health. 18(3636)2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Casner M, Andersen D and Isaacs SM: The
impact of a new CPR assist device on rate of return of spontaneous
circulation in out-of-hospital cardiac arrest. Prehosp Emerg Care.
9:61–67. 2005.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Schmidbauer S, Herlitz J, Karlsson T,
Axelsson C and Friberg H: Use of automated chest compression
devices after out-of-hospital cardiac arrest in Sweden.
Resuscitation. 120:95–102. 2017.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Primi R, Bendotti S, Currao A, Sechi GM,
Marconi G, Pamploni G, Panni G, Sgotti D, Zorzi E, Cazzaniga M, et
al: Use of mechanical chest compression for resuscitation in
out-of-hospital cardiac arrest-device matters: A
propensity-score-based match analysis. J Clin Med.
12(4429)2023.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Jin K, Fu Y, Yin L, Yu S, Zhang L, Wang Y,
Zhu H, Xu J and Yu X: Influence factors analysis of mechanical
compression and hands-only compression on restoration of
spontaneous circulation and prognosis in patients with cardiac
arrest. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 31:303–308.
2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
53
|
Maule Y: Mechanical external chest
compression: A new adjuvant technology in cardiopulmonary
resuscitation. Urgences Accueil. 7:4–7. 2007.
|
|
54
|
Ong ME, Ornato JP, Edwards DP, Dhindsa HS,
Best AM, Ines CS, Hickey S, Clark B, Williams DC, Powell RG, et al:
Use of an automated, load-distributing band chest compression
device for out-of-hospital cardiac arrest resuscitation. JAMA.
295:2629–2637. 2006.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Swanson M, Poniatowski M, O'Keefe M and
Springer P: A CPR assist device increased emergency department
admission and end tidal carbon dioxide partial pressures during
treatment of out of hospital cardiac arrest. Circulation.
114(554)2006.
|
|
56
|
Lairet JR and Lee M: A comparison of
standard manual cardiopulmonary resuscitation versus the Autopulse
mechanical cardiopulmonary resuscitation device. Ann Emerg Med. 46
(Suppl)(S114)2005.
|
|
57
|
Ornato JP, Peberdy MA, Edwards DP, et al:
Improvement in field return of spontaneous circulation using
circumferential chest compression cardiopulmonary resuscitation.
Prehosp Emerg Care. 9(104)2005.
|
|
58
|
de Wilde R, vd Weijden P, de Haan M, Bosch
J, de Nooij J and Harinck HIJ: ROSC at hospital admission in out of
hospital cardiac arrest using LUCAS. Resuscitation. 77
(Suppl)(S49)2008.
|
|
59
|
Paradis NA, Kamlan D, Ghilarducci D and
Palazzolo J: The California AutoPulse quality assurance registry.
Circulation. 120(S1457)2009.
|
|
60
|
Truhlar A, Hejna P, Zabka L, Zatopkova L
and Cerny V: Injuries caused by the autopulse and LUCAS II
resuscitation systems compared to manual chest compressions.
Resuscitation. 81 (Suppl)(S62)2010.
|
|
61
|
Morozov SN, Abdusalamov SN and Fedorov AY:
Improved prognosis after implementation of chest compression device
in out-of-hospital cardiac arrest. Eur Heart J. 3(S702)2012.
|
|
62
|
Liu Y: Two kinds of external chest
compression mode for out-of-hospital cardiac arrest patients
pressure quality effect analysis (Chinese). Chin J Emerg Disaster
Med. 10:657–659. 2016.
|
|
63
|
Canakci ME, Parpucu Bagceci K, Acar N,
Ozakin E, Baloglu Kaya F, Kuas C, Çetin M, Tiryaki Baştuğ B and
Karakılıç ME: Computed tomographic findings of injuries after
mechanical and manual resuscitation: A retrospective study. Cureus.
13(e15131)2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Takayama W, Endo A, Morishita K and Otomo
Y: Manual chest compression versus automated chest compression
device during day-time and night-time resuscitation following
out-of-hospital cardiac arrest: A retrospective historical control
study. J Pers Med. 13(1202)2023.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Viniol S, Thomas RP, Gombert S, König AM,
Betz S and Mahnken AH: Comparison of different resuscitation
methods with regard to injury patterns in cardiac arrest survivors
based on computer tomography. Eur J Radiol.
131(109244)2020.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Saleem S, Sonkin R, Sagy I, Strugo R,
Jaffe E, Drescher M and Shiber S: Traumatic injuries following
mechanical versus manual chest compression. Open Access Emerg Med.
14:557–562. 2022.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Lu XG, Kang X and Gong DB: The clinical
efficacy of Thumper modal 1007 cardiopulmonary resuscitation: A
prospective randomized control trial. Zhongguo Wei Zhong Bing Ji
Jiu Yi Xue. 22:496–497. 2010.PubMed/NCBI
|
|
68
|
Kuschner CE and Becker LB: Recent advances
in personalizing cardiac arrest resuscitation. F1000Res 8: F1000
Faculty Rev-915, 2019.
|
|
69
|
Wang PL and Brooks SC: Mechanical versus
manual chest compressions for cardiac arrest. Cochrane Database
Syst Rev. 8(CD007260)2018.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Lazzarin T, Tonon CR, Martins D, Fávero EL
Jr, Baumgratz TD, Pereira FWL, Pinheiro VR, Ballarin RS, Queiroz
DAR, Azevedo PS, et al: Post-cardiac arrest: Mechanisms,
management, and future perspectives. J Clin Med.
12(259)2022.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Nikolovski SS, Lazic AD, Fiser ZZ,
Obradovic IA, Tijanic JZ and Raffay V: Recovery and survival of
patients after out-of-hospital cardiac arrest: A literature review
showcasing the big picture of intensive care unit-related factors.
Cureus. 16(e54827)2024.PubMed/NCBI View Article : Google Scholar
|