1. Introduction
Saharan dust storms, also known as Saharan dust
events, are natural phenomena characterized by the transport of
vast quantities of mineral dust from the Sahara Desert across the
African continent and beyond. These dust events occur predominantly
during the dry season, typically from November to March, when
intense atmospheric pressure systems over North Africa drive the
movement of dust-laden air masses towards the Atlantic Ocean and
surrounding regions. In West Africa, the Harmattan winds are a
specific example of winds that can deliver Saharan dust, but other
wind patterns contribute to dust transport across wider areas
(1,2).
The Sahara desert, the largest hot desert in the
world, serves as the primary source of Saharan dust emissions. With
its extensive arid and semi-arid landscapes, the Sahara experiences
frequent dust uplift due to strong surface winds, convective
processes, and occasional thunderstorms. The resulting dust plumes
can travel thousands of kilometers, crossing international borders
and affecting diverse ecosystems, from the Caribbean to the Amazon
rainforest and even reaching as far as Europe and North America
(3,4).
The global impact of Saharan dust storms is
profound, influencing various environmental, atmospheric and
socio-economic processes. Dust particles suspended in the
atmosphere play a crucial role in modulating Earth's radiative
balance, affecting regional and global climate patterns through the
scattering and absorption of solar radiation. Additionally, Saharan
dust deposition contributes essential nutrients, such as iron and
phosphorus, to marine and terrestrial ecosystems, influencing
ecosystem dynamics and productivity (5,6).
Furthermore, Saharan dust can have significant
implications for air quality and human health, particularly in
regions downwind of dust source areas. Dust storms can elevate
levels of particulate matter (PM) in the atmosphere, including
coarse and fine particles capable of penetrating deep into the
respiratory system. This can exacerbate respiratory conditions,
trigger allergic reactions, and contribute to cardiovascular
morbidity, posing risks to vulnerable populations, such as
children, the elderly, and individuals with pre-existing
respiratory diseases (7,8).
In recent years, there has been increasing
recognition of the association between exposure to Saharan dust
particles and the incidence and exacerbation of lung diseases.
While research on this topic is still evolving, emerging evidence
suggests that inhalation of Saharan dust may contribute to
respiratory symptoms, exacerbate pre-existing lung conditions, and
increase the risk of developing respiratory illnesses (9,10).
The composition and characteristics of Saharan dust
particles, including their size distribution, mineralogical
composition, and surface chemistry, play a critical role in
determining their biological effects on the respiratory system.
Fine dust particles, with diameters <2.5 micrometers (PM2.5),
are of particular concern due to their ability to penetrate deep
into the lungs and potentially induce inflammation, oxidative
stress and tissue damage (11).
The associations between Saharan dust events and
adverse respiratory health outcomes in affected populations are
well documented. These include an increase in hospital admissions
for respiratory conditions, such as asthma exacerbations, chronic
obstructive pulmonary disease (COPD) exacerbations and respiratory
tract infections, during periods of elevated dust concentrations.
Additionally, epidemiological investigations have identified
correlations between dust exposure levels and respiratory symptoms,
such as coughing, wheezing and shortness of breath, particularly
among individuals with underlying respiratory conditions (12,13).
The present review focuses on the critical
interactions between Saharan dust particles and respiratory health,
highlighting how the unique physical and chemical properties of the
dust exacerbate conditions such as asthma and COPD, particularly in
vulnerable populations.
2. Composition and characteristics of
Saharan dust
Origins and pathways of Saharan dust
transport
The Sahara desert, spanning over 9 million square
kilometers, serves as the primary source of Saharan dust emissions
(14). Dust uplift events occur
throughout the year but peak during the dry season, from late fall
to early spring, when intense surface heating leads to convective
instability and strong winds across the desert region. These winds,
often associated with the Saharan heat low and the Azores high
pressure systems, drive the movement of dust-laden air masses
towards the Atlantic Ocean and surrounding continents (15).
Several pathways facilitate the long-range transport
of Saharan dust across the globe. The most prominent is the Saharan
Air Layer (SAL), a well-defined layer of warm, dry and dusty air
that extends from the Sahara across the tropical North Atlantic.
The SAL acts as a conduit for dust particles, carrying them
thousands of kilometers westward towards the Caribbean, South
America and North America. Additionally, atmospheric circulation
patterns, such as the African easterly jet and the African easterly
waves, play crucial roles in transporting dust plumes across
Africa, Europe and the Mediterranean basin (16-18).
The interplay between synoptic weather systems,
regional topography and land-atmosphere interactions influences the
spatial and temporal variability of dust emissions and transport.
Dust storms can originate from various source regions within the
Sahara, including the Bodele Depression in Chad, the Bodélé
Escarpment in Niger, and the Libyan desert, each characterized by
unique geomorphological features and dust emission mechanisms.
Moreover, episodic weather phenomena, such as convective
thunderstorms and haboobs (dust storms associated with cold
fronts), can locally enhance dust production and mobilization,
leading to intense dust storms with significant impacts on air
quality and visibility (19,20).
Chemical composition of Saharan dust
particles
Saharan dust particles are predominantly
mineralogical in nature, composed primarily of silicates,
carbonates, oxides and sulfates derived from the weathering and
erosion of geological formations in the Sahara desert. Quartz,
feldspar and clay minerals are among the most abundant components
of Saharan dust, reflecting the diverse lithological composition of
the source regions (21).
In addition to mineral dust, Saharan dust particles
may also contain organic matter, trace elements and anthropogenic
pollutants, resulting from surface interactions, atmospheric
processing, and mixing with pollution plumes during transport
(22).
The chemical composition of Saharan dust particles
varies spatially and temporally, reflecting differences in source
rock types, weathering processes, and atmospheric processing during
transport. Elemental analysis of dust samples has revealed
enrichment in elements such as silicon, aluminum, iron, calcium,
magnesium and potassium, which are characteristic of silicate
minerals abundant in the Sahara region (23). Additionally, trace elements,
including heavy metals such as lead, cadmium and zinc, may be
present in Saharan dust particles, originating from both natural
sources and anthropogenic activities within the source region
(24).
Furthermore, chemical reactions occurring on the
surface of dust particles during atmospheric transport can alter
their composition and properties, affecting their reactivity,
hygroscopicity and potential health impacts. For example, iron-rich
dust particles can act as carriers of bioavailable iron, which may
stimulate biological productivity in marine and terrestrial
ecosystems upon deposition (25).
Additionally, the interaction of dust particles with atmospheric
gases, such as sulfur dioxide and nitrogen oxides, can lead to the
formation of secondary aerosols and affect regional air quality and
climate (26).
Physical properties and atmospheric
behavior
Saharan dust particles exhibit a wide range of
physical properties, including size, shape, density and aerodynamic
characteristics, which influence their transport, deposition and
atmospheric behavior (27).
Dust particles generated by aeolian processes in the
Sahara desert range in size from submicron (<1 µm) to coarse
(>10 µm) particles, with the majority falling within the fine
(<2.5 µm) and coarse (2.5-10 µm) fractions (28). Fine dust particles, known as PM2.5,
are of particular concern due to their potential to penetrate deep
into the respiratory system and impact human health (29).
The shape and morphology of Saharan dust particles
vary depending on their mineralogical composition and the processes
involved in their formation and transport. Dust particles may
exhibit angular, irregular, or spheroidal shapes, reflecting
differences in the degree of weathering, abrasion and transport
history. Coarse particles tend to be more angular and irregular,
while fine particles may undergo rounding and surface smoothing
during long-range transport, resulting in more spherical shapes
(30).
The density of Saharan dust particles also varies
depending on their mineral composition and porosity, with typical
values ranging from 2.5 to 3.5 g/cm³ for silicate minerals such as
quartz and feldspar. Coarse dust particles tend to have higher
densities than fine particles due to their larger grain sizes and
higher packing densities. Additionally, the aerodynamic properties
of dust particles, such as settling velocity and terminal velocity,
play a crucial role in determining their transport and deposition
patterns in the atmosphere and the environment (31,32).
Atmospheric behavior of Saharan dust particles is
influenced by a complex interplay of meteorological factors,
including wind speed and direction, atmospheric stability,
turbulence, and vertical mixing processes. Dust particles injected
into the atmosphere by surface winds can be transported over long
distances by prevailing winds aloft, reaching altitudes of several
kilometers and forming extensive dust plumes. The vertical
distribution of dust in the atmosphere is controlled by atmospheric
stability and vertical mixing processes, with higher concentrations
typically observed near the surface during dust events and loftier
layers aloft during transport (33,34).
3. Health effects of Saharan dust exposure
on the respiratory system
Inhalation of PM and its effects on
lung health
PM is a complex mixture of solid and liquid
particles suspended in the air, varying in size, composition and
origin. Inhalation of PM, particularly fine and ultrafine
particles, can have detrimental effects on respiratory health,
ranging from acute irritation to chronic lung diseases and
cardiovascular morbidity. Saharan dust events contribute to
elevated levels of PM in the atmosphere, exposing populations to
increased health risks, especially in regions downwind of dust
source areas. Fine dust particles, PM2.5, pose the greatest health
concern due to their ability to penetrate deep into the respiratory
system and reach the alveolar region of the lungs. Upon inhalation,
PM2.5 particles can induce inflammation, oxidative stress and
cellular damage in lung tissues, leading to a range of adverse
respiratory effects. Additionally, ultrafine particles (<0.1
micrometers) can translocate across the respiratory epithelium into
systemic circulation, potentially exacerbating cardiovascular
diseases and systemic inflammation (35,36).
The biological mechanisms underlying the respiratory
effects of PM inhalation are multifaceted and involve inflammatory
responses, oxidative stress and disruption of cellular signaling
pathways. PM particles can activate immune cells, such as
macrophages and neutrophils, leading to the release of
pro-inflammatory mediators, cytokines and reactive oxygen species
(ROS) (37,38).
Chronic exposure to PM has been associated with
airway inflammation, epithelial damage, mucous hypersecretion and
impaired lung function, contributing to the development and
progression of respiratory diseases, including asthma, chronic
bronchitis and COPD (39,40).
Association between Saharan dust
events and respiratory symptoms
Epidemiological studies have provided evidence of
associations between Saharan dust events and adverse respiratory
health outcomes in affected populations. During dust storm
episodes, increases in ambient PM concentrations have been
correlated with elevated rates of respiratory symptoms,
exacerbations of pre-existing lung conditions, and hospital
admissions for respiratory illnesses. These associations are
particularly pronounced in vulnerable individuals, such as
children, the elderly and individuals with underlying respiratory
diseases (41,42).
A study conducted in the Caribbean region found that
increases in PM10 concentrations during Saharan dust episodes were
associated with higher rates of emergency room visits for asthma
exacerbations and acute respiratory infections in children
(43). Similarly, investigations
in West Africa have reported elevated levels of respiratory
symptoms, such as coughing, wheezing and shortness of breath, among
residents exposed to high dust concentrations during Harmattan
periods (44). Furthermore,
longitudinal studies have identified temporal trends linking dust
exposure to changes in respiratory health indicators, including
decreased lung function, increased airway reactivity, and higher
medication use among asthma and COPD patients during dust storm
seasons (45).
Impact on vulnerable populations, such
as children, elderly and pregnant women
Vulnerable populations, such as children, the
elderly and individuals with pre-existing respiratory conditions,
are particularly susceptible to the adverse health effects of
Saharan dust exposure. Children, whose respiratory systems are
still developing, may experience exacerbated symptoms of asthma and
respiratory infections during dust storm episodes due to increased
airway inflammation and susceptibility to respiratory irritants
(46).
Elderly individuals, especially those with
underlying cardiovascular diseases or compromised lung function,
are at higher risk of experiencing respiratory symptoms and
exacerbations of chronic conditions during dust events. Reduced
lung elasticity and impaired mucociliary clearance in the elderly
can exacerbate the deposition and retention of dust particles in
the airways, leading to respiratory distress and functional decline
(47). Furthermore, individuals
with pre-existing respiratory diseases, such as asthma, COPD and
allergic rhinitis, may experience worsened symptoms and decreased
disease control during Saharan dust episodes. The pro-inflammatory
and irritant properties of dust particles can trigger airway
inflammation, bronchoconstriction and exacerbations of respiratory
conditions, necessitating increased medication use and healthcare
utilization among affected individuals (48,49).
Vodonos et al (50) identified a positive correlation
between dust storms and hospitalization rates for COPD
exacerbations, showing a 16% increase in Southern Israel. This
effect was more pronounced with age and higher in women. In a
laboratory study involving young healthy adults, researchers found
that women had 11-23% greater deposition of inhaled particles in
the central airways compared with men (51). This sex disparity was most evident
with coarser particles (>5 µm). Women may experience greater
susceptibility to air pollution, including dust, due to
physiological factors such as smaller lung volume and airway size,
leading to more particulate deposition in the lungs. The elevated
concentration of PM in the central airways leads to greater
irritation and inflammation, potentially triggering acute COPD
exacerbations (52). During
pregnancy, a woman's respiratory system undergoes significant
changes, including a 20% increase in oxygen consumption to
accommodate the increased oxygen demands of her and the growing
fetus (53). As a result of these
changes, pregnant women are particularly vulnerable to the effects
of air pollution because of the increased number of pollutants
inhaled.
Air pollution can trigger common respiratory
diseases such as asthma and allergic rhinitis. The major adverse
maternal outcome associated with air pollution is maternal
hypertensive disorders such as pre-eclampsia (54). A meta-analysis of 33 cohort studies
revealed that exposure to PM10 increased the relative risk
(55). Furthermore, an increasing
number of research suggests that maternal exposure to PM may also
impact the fetus. Pollutants can cross the placenta, entering the
fetal circulation during gestation (56).
Maternal exposure to Saharan dust appears to
influence the fetal lung development and respiratory system after
birth. A study evaluated that exposure to PM2.5 was associated with
tachypnea of the newborn, asphyxia and respiratory distress
syndrome (57). Different studies
have looked at the effects on fetal growth. A systematic review of
52 studies and a meta-analysis of 54 studies found that maternal
exposure to PM2.5, PM10 and other air pollutants was generally
positively associated with low birth weight (58).
4. Mechanisms underlying the pathogenicity
of Saharan dust
Inflammatory responses triggered by
dust particle exposure
Inhalation of Saharan dust particles can trigger
inflammatory responses in the respiratory system, leading to acute
and chronic respiratory conditions. Upon deposition in the airways,
dust particles activate innate immune cells, such as macrophages
and neutrophils, through pattern recognition receptors and
toll-like receptors (59,60). Recognition of microbial components
and danger-associated molecular patterns on the surface of dust
particles induces the production of pro-inflammatory cytokines,
chemokines and ROS by immune cells, initiating an inflammatory
cascade. It has been demonstrated that exposure to Saharan dust
induces significant expression of pro-inflammatory cytokines such
as GM-CSF and G-CSF, which play crucial roles in the exacerbation
of respiratory conditions (61).
Pro-inflammatory cytokines, such as tumor necrosis factor-alpha
(TNF-α), interleukin-1 beta (IL-1β), and interleukin-6 (IL-6),
recruit additional immune cells to the site of inflammation and
activate downstream signaling pathways, amplifying the inflammatory
response (62,63). Chemokines, such as interleukin-8
(IL-8), promote the migration of neutrophils and other immune cells
to the airways, further exacerbating inflammation and tissue
damage. Additionally, ROS generated by activated immune cells
contribute to oxidative stress, lipid peroxidation and DNA damage,
exacerbating inflammatory responses and tissue injury (64,65).
Chronic exposure to Saharan dust particles can lead
to sustained inflammation and airway remodeling, characterized by
epithelial hyperplasia, mucus hypersecretion, fibrosis and smooth
muscle hypertrophy, contributing to the pathogenesis of respiratory
diseases such as asthma, chronic bronchitis and COPD (66,67).
Furthermore, interactions between inflammatory mediators and neural
pathways can exacerbate airway hyperresponsiveness and
bronchoconstriction, leading to respiratory symptoms and functional
impairment (68).
Moreover, it has been highlighted that airborne
particles such as PM2.5, cigarette smoke and diesel exhaust can
induce endothelial dysfunction, promoting inflammation and
increasing the risk of chronic respiratory diseases (69).
Activation of immune pathways and
oxidative stress
In addition to inflammatory responses, exposure to
Saharan dust particles can activate immune pathways and induce
oxidative stress in the respiratory system. Dust particles contain
a variety of biologically active components, including microbial
antigens, endotoxins, metals and organic pollutants, which can
stimulate immune cells and promote inflammatory and immune
responses. Upon inhalation, Saharan dust particles interact with
the respiratory epithelium, triggering an inflammatory response
that can exacerbate pre-existing respiratory conditions. The
interaction of fine PM (PM2.5) with immune cells, such as
macrophages, further amplifies oxidative stress, leading to airway
hyperresponsiveness and long-term damage (70,71).
Endotoxins, derived from the outer membrane of
gram-negative bacteria, are abundant in Saharan dust and can
activate toll-like receptor 4 (TLR4) signaling pathways, leading to
the production of pro-inflammatory cytokines, such as interleukin-1
beta (IL-1β) and interleukin-6 (IL-6), by immune cells (72,73).
Additionally, microbial components and allergens present in dust
particles can trigger allergic immune responses, leading to the
production of immunoglobulin E antibodies and the activation of
mast cells and eosinophils, contributing to allergic asthma and
allergic rhinitis (74).
Oxidative stress, resulting from an imbalance
between the production of ROS and antioxidant defenses, is a common
feature of Saharan dust-induced inflammation and respiratory
injury. Dust particles can contain transition metals, such as iron,
manganese and copper, which catalyze the generation of ROS through
Fenton and Haber-Weiss reactions, leading to lipid peroxidation,
protein oxidation and DNA damage in lung tissues (75,76).
Additionally, ROS can activate redox-sensitive transcription
factors, such as nuclear factor kappa B (NF-κB) and activator
protein 1 (AP-1), leading to the upregulation of pro-inflammatory
genes and the perpetuation of inflammatory responses (77,78).
Moreover, inhalation of Saharan dust has been demonstrated to
induce oxidative stress and activate the NLRP3 inflammasome,
leading to significant release of pro-inflammatory cytokines,
thereby exacerbating lung inflammation (79).
Contribution to the development and
exacerbation of lung diseases
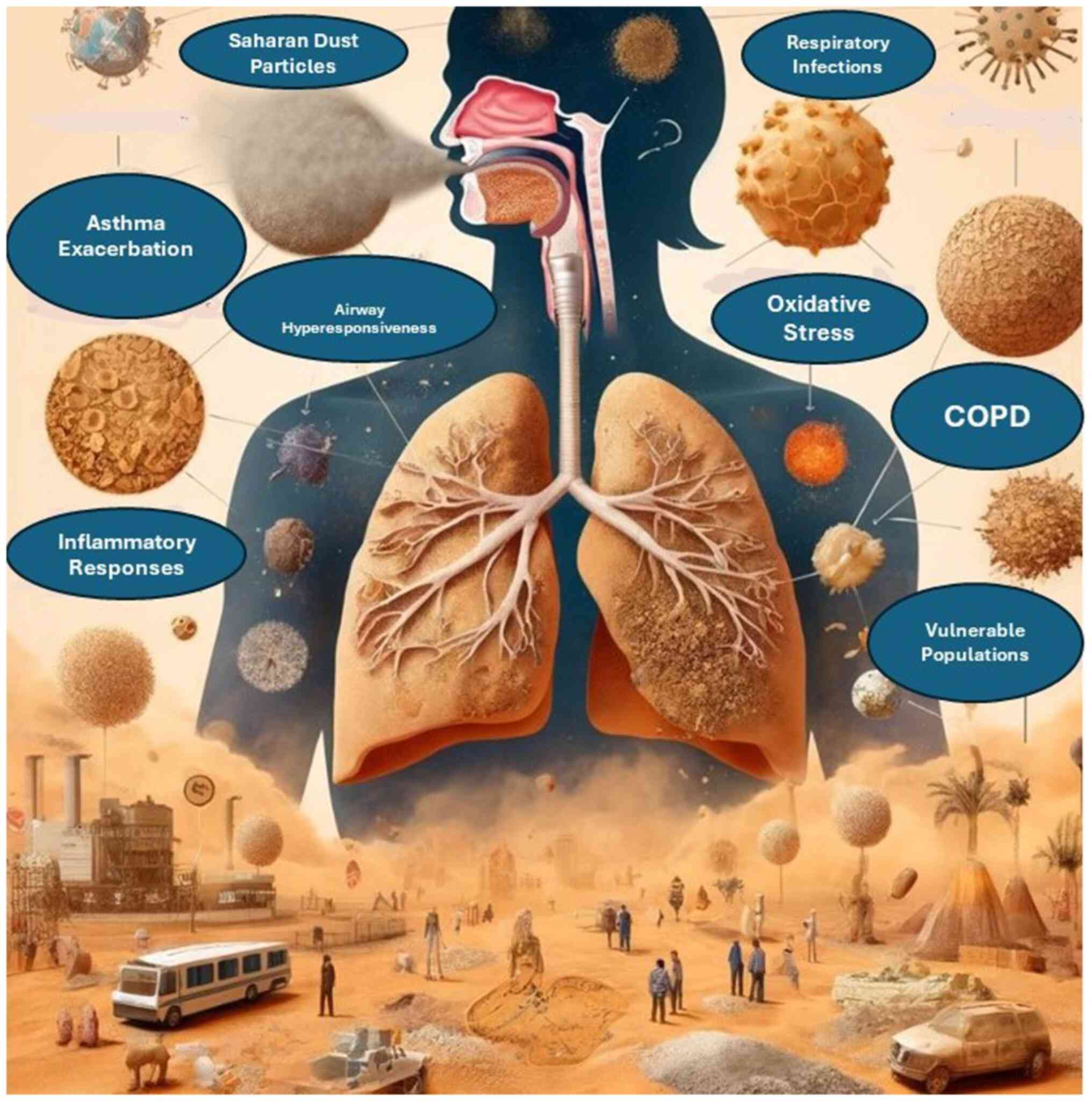
The inflammatory and oxidative effects of Saharan
dust exposure contribute to the development and exacerbation of
various respiratory diseases, including asthma, chronic bronchitis,
COPD and allergic rhinitis. Acute exposure to high levels of
Saharan dust particles can trigger asthma exacerbations and
respiratory symptoms in susceptible individuals, leading to
increased medication use, emergency department visits, and hospital
admissions (80,81).
Chronic exposure to Saharan dust particles can
exacerbate pre-existing respiratory conditions and impair lung
function over time, particularly in vulnerable populations, such as
children, the elderly, and individuals with underlying lung
diseases. The persistent inflammatory responses induced by dust
exposure can lead to airway remodeling, fibrosis and bronchial
hyperresponsiveness, contributing to the progression of chronic
respiratory diseases and the development of irreversible airflow
obstruction (82,83).
Furthermore, Saharan dust exposure may interact with
other environmental pollutants, such as vehicular emissions,
industrial pollutants and biomass burning aerosols, to exacerbate
respiratory health effects and increase the risk of adverse
outcomes. Synergistic interactions between dust particles and other
pollutants can amplify inflammatory responses, oxidative stress and
airway injury, leading to more severe respiratory symptoms and
poorer health outcomes (84). The
various respiratory health effects associated with the inhalation
of Saharan dust particles are illustrated in Fig. 1.
5. Geographic variability and environmental
factors influencing health outcomes
The health effects of Saharan dust exposure exhibit
geographic variability, with differences observed in the magnitude
and frequency of dust events, as well as in the susceptibility of
populations to respiratory health effects. Environmental factors,
including meteorological conditions, air pollution levels, land use
patterns and socio-economic factors, play crucial roles in
modulating the health impacts of dust storms and influencing health
outcomes in affected regions.
Regions located downwind of major dust source areas,
such as the Sahel region of West Africa and the Caribbean islands,
experience higher levels of dust exposure and are more susceptible
to respiratory health effects during dust events (85). The frequency and intensity of dust
storms in these regions are influenced by seasonal weather
patterns, such as the West African monsoon and the North Atlantic
Oscillation, which affect dust emission, transport and deposition
processes (86).
Additionally, environmental factors such as air
pollution levels and background PM concentrations can interact with
Saharan dust particles to exacerbate respiratory health effects and
increase the risk of adverse outcomes. Coarse and fine PM from
local sources, such as vehicular emissions, industrial pollution
and biomass burning, can mix with Saharan dust plumes during
transport, leading to elevated levels of airborne pollutants and
exacerbating air quality problems in dust-affected regions
(87).
Furthermore, socio-economic factors, including
housing conditions, access to healthcare and socio-demographic
characteristics, can influence the vulnerability of populations to
dust-related health risks. Socio-economically disadvantaged
communities, such as low-income neighborhoods and rural
settlements, may face greater challenges in accessing healthcare
services, implementing preventive measures and mitigating the
impacts of dust storms on respiratory health (88).
6. Mitigation strategies and public health
implications
Strategies for reducing exposure to
Saharan dust particles
Mitigating exposure to Saharan dust particles
requires a multi-faceted approach involving individual actions,
community measures and environmental management strategies. While
it may not be possible to completely eliminate exposure to dust
particles, several strategies can help reduce the risk of
respiratory health effects associated with dust storms.
To mitigate the infiltration of outdoor air laden
with dust particles into indoor environments, it is advised to keep
windows and doors closed during dust events. Additionally,
employing air purifiers equipped with high-efficiency particulate
air filters can effectively remove dust particles from indoor air
sources (14). During episodes of
poor outdoor air quality resulting from dust storms, individuals
are encouraged to utilize face masks or respirators. Optimal
choices for filtration include N95 respirators, designed to
effectively filter fine PM, thereby reducing the inhalation of dust
particles (89). Enhancing indoor
air quality can be achieved through the installation of air
filtration systems in various settings such as homes, schools and
workplaces. Employing high-efficiency HVAC filters aids in
capturing airborne dust particles and preventing their
re-circulation within indoor environments (90).
Mitigating dust impacts within urban settings
necessitates the integration of urban design elements such as green
spaces, street trees and vegetated buffers. Furthermore,
incorporating dust control measures into construction projects and
infrastructure development endeavors aids in minimizing dust
emissions (91). Employing dust
suppressants, such as water sprays, chemical stabilizers and soil
binders, offers an effective approach to reduce dust emissions from
unpaved roads, construction sites and open land areas. Consistent
application of these techniques, including regular surface wetting,
aids in controlling dust and preventing its resuspension by wind.
Promoting awareness regarding the health risks associated with
exposure to Saharan dust and advocating preventive measures are
essential components of public health initiatives. Dissemination of
educational materials, issuance of health advisories, and
implementation of outreach programs serve to inform communities
about dust-related health hazards and encourage the adoption of
protective measures (2).
Public health interventions to
mitigate respiratory health risks
In addition to individual and community-level
strategies, public health interventions play a critical role in
mitigating respiratory health risks associated with Saharan dust
exposure. These interventions aim to enhance surveillance,
monitoring and response efforts to protect vulnerable populations
and reduce the burden of dust-related respiratory diseases.
Establishing and maintaining air quality monitoring
networks is crucial for tracking dust concentrations and pollutant
levels during dust events. Real-time monitoring data should be
utilized to issue air quality alerts, advisories, and warnings to
the public and healthcare providers (92).
The development and implementation of health
surveillance systems are essential to monitor respiratory symptoms,
hospital admissions and mortality rates during dust events.
Collecting and analyzing epidemiological data enables the
assessment of the impact of dust exposure on respiratory health
outcomes and identification of at-risk populations (45).
Developing emergency response plans and protocols is
imperative to address respiratory health emergencies associated
with Saharan dust storms. Coordination with healthcare facilities,
emergency responders, and public health agencies ensures timely
access to medical care and support services for affected
individuals (81).
Providing training and education for healthcare
providers on the recognition, diagnosis, and management of
respiratory conditions related to Saharan dust exposure is
essential. Promoting evidence-based clinical practices and
treatment guidelines facilitates the management of acute
exacerbations and complications of dust-related respiratory
diseases (82).
Engaging community stakeholders, advocacy groups,
and local organizations in dust awareness campaigns, public forums,
and community-based interventions is vital. Partnerships with
schools, workplaces and community centers facilitate the
dissemination of health information and promotion of preventive
measures (71).
Policy recommendations and future
directions for research and action
Addressing the public health implications of Saharan
dust exposure necessitates coordinated efforts across multiple
sectors, including environmental protection, public health, urban
planning, and climate resilience. Future research should focus on
understanding the complex interactions between Saharan dust and
urban pollutants, as well as their combined effects on respiratory
health. Identifying how these interactions differ based on
geography and population demographics could inform more effective
public health interventions. The following policy recommendations
and future research priorities can guide efforts to mitigate
dust-related respiratory health risks and promote sustainable
development.
Developing comprehensive air quality management
strategies that address the sources, transport, and impacts of
Saharan dust on respiratory health is imperative. Integrating dust
monitoring and mitigation measures into existing air quality
management frameworks and regulations is recommended (84).
Incorporating dust-related health risks into climate
adaptation and resilience plans is essential for safeguarding
public health in the face of climate change. Implementing
strategies to enhance community resilience, build adaptive
capacity, and reduce vulnerability to dust storms and other
environmental hazards is crucial (59).
Fostering collaboration and knowledge exchange among
countries affected by Saharan dust storms is essential. Promoting
regional cooperation and joint initiatives to address transboundary
air pollution and cross-border health impacts facilitates the
sharing of best practices, research findings and capacity-building
efforts (93).
Investing in research and innovation to advance
understanding of the mechanisms, drivers, and health effects of
Saharan dust exposure is necessary. Supporting interdisciplinary
research projects, observational studies, and modeling efforts
improves predictive capabilities and informs evidence-based
interventions (94).
Ensuring coherence and alignment between policies
related to air quality, public health, environmental management and
sustainable development is critical. Integrating dust mitigation
measures into national and regional policy frameworks, including
climate action plans, health strategies and disaster risk reduction
policies, promotes policy integration and coherence (95).
These recommendations and future directions
underscore the importance of proactive measures and collaborative
approaches in addressing the complex challenges posed by Saharan
dust exposure and its implications for respiratory health and
sustainable development.
7. Conclusions
In summary, Saharan dust storms pose significant
respiratory health risks, driven by the transport of mineral dust
across continents. Inhalation of PM from these events exacerbates
respiratory conditions and increases the risk of developing lung
diseases, particularly among vulnerable populations. Tailored
mitigation strategies, including air quality management and public
health interventions, are essential for addressing these risks.
Collaboration, research investment and policy coherence are vital
for effective mitigation and promoting sustainable development in
the face of Saharan dust exposure.
Acknowledgements
Not applicable.
Funding
Funding: Not funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
AD and VEG conceptualized the study. AD, CT, VEG,
PP, DB, NT and DAS made substantial contributions to data
interpretation and analysis, and wrote and prepared the draft of
the manuscript. AD and VEG analyzed the data and provided critical
revisions. All authors contributed to manuscript revision, read and
approved the final version of the manuscript. Data authentication
is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors confirm that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools were used to improve the readability and
language of the manuscript or to generate images, and subsequently,
the authors revised and edited the content produced by artificial
intelligence tools as necessary, taking full responsibility for the
ultimate content of the present manuscript.
References
|
1
|
Knippertz P: Mineral dust generation
across northern Africa and its impacts. In: Oxford Research
Encyclopedia of Climate Science. Storch H (ed). Oxford University
Press, New York, NY, 2017.
|
|
2
|
Goudie AS: Dust storms: Recent
developments. J Environ Manage. 90:89–94. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Thomas N and Nigam S: Twentieth-century
climate change over Africa: Seasonal hydroclimate trends and Sahara
desert expansion. J Clim. 31:3349–3370. 2018.
|
|
4
|
Griffin DW, Kellogg CA, Garrison VH and
Shinn EA: The global transport of dust: An intercontinental river
of dust, microorganisms and toxic chemicals flows through the
Earth's atmosphere. Am Sci. 90:228–235. 2002.
|
|
5
|
Prospero JM: Long-range transport of
mineral dust in the global atmosphere: Impact of African dust on
the environment of the southeastern United States. Proc Natl Acad
SciUSA. 96:3396–3403. 1999.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Schepanski K: Transport of mineral dust
and its impact on climate. Geosciences. 8(151)2018.
|
|
7
|
Griffin DW: Atmospheric movement of
microorganisms in clouds of desert dust and implications for human
health. Clin Microbiol Rev. 20:459–477. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Varrica D and Alaimo MG: Influence of
Saharan dust on the composition of urban aerosols in Palermo City
(Italy). Atmosphere. 15(254)2024.
|
|
9
|
Gutierrez MP, Zuidema P, Mirsaeidi M,
Campos M and Kumar N: Association between African dust transport
and acute exacerbations of COPD in Miami. J Clin Med.
9(2496)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Schweitzer MD, Calzadilla AS, Salamo O,
Sharifi A, Kumar N, Holt G, Campos M and Mirsaeidi M: Lung health
in era of climate change and dust storms. Environ Res. 163:36–42.
2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Scheuvens D, Schütz L, Kandler K, Ebert M
and Weinbruch S: Bulk composition of northern African dust and its
source sediments-A compilation. Earth Sci Rev. 116:170–194.
2013.
|
|
12
|
Trianti SM, Samoli E, Rodopoulou S,
Katsouyanni K, Papiris SA and Karakatsani A: Desert dust outbreaks
and respiratory morbidity in Athens, Greece. Environ Health.
16(72)2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rublee CS, Sorensen CJ, Lemery J, Wade TJ,
Sams EA, Hilborn ED and Crooks JL: Associations between dust storms
and intensive care unit admissions in the United States, 2000-2015.
Geohealth. 4(e2020GH000260)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
De Longueville F, Hountondji YC, Henry S
and Ozer P: What do we know about effects of desert dust on air
quality and human health in West Africa compared to other regions?
Sci Total Environ. 409:1–8. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Marsham JH, Parker DJ, Grams CM, Taylor CM
and Haywood JM: Uplift of Saharan dust south of the intertropical
discontinuity. J Geophys Res Atmos. 113(D21102)2008.
|
|
16
|
Prospero JM and Mayol-Bracero OL:
Understanding the transport and impact of African dust on the
Caribbean Basin. Bull Am Meteorol Soc. 94:1329–1337. 2013.
|
|
17
|
Harrison AD, O'Sullivan D, Adams MP,
Porter GCE, Blades E, Brathwaite C, Chewitt-Lucas R, Gaston C,
Hawker R, Krüger OO, et al: The ice-nucleating activity of African
mineral dust in the Caribbean boundary layer. Atmos Chem Phys.
22:9663–9680. 2022.
|
|
18
|
Boose Y, Sierau B, García MI, Rodríguez S,
Alastuey A, Linke C, Schnaiter M, Kupiszewski P, Kanji ZA and
Lohmann U: Ice nucleating particles in the Saharan air layer. Atmos
Chem Phys. 16:9067–9087. 2016.
|
|
19
|
Namdari S, Karimi N, Sorooshian A,
Mohammadi G and Sehatkashani S: Impacts of climate and synoptic
fluctuations on dust storm activity over the Middle East. Atmos
Environ (1994). 173:265–276. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Knippertz P: Meteorological aspects of
dust storms. Mineral dust: A key player in the earth system,
pp121-147, 2014.
|
|
21
|
Navarro-Ciurana D, Corbella M,
Farré-de-Pablo J, Corral I, Buixadera E, Morera-Valverde R and
Proenza JA: Rare Earth Elements' particles in road dust: A
mineralogical perspective for source identification. Atmos Environ.
309(119927)2023.
|
|
22
|
Erel Y, Dayan U, Rabi R, Rudich Y and
Stein M: Trans boundary transport of pollutants by atmospheric
mineral dust. Environ Sci Technol. 40:2996–3005. 2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kumar A, Shukla G and Singh A: Long-range
global transport and characterization of dust. In Asian Atmospheric
Pollution. Elsevier, pp483-504, 2022.
|
|
24
|
Schleicher NJ, Dong S, Packman H, Little
SH, Ochoa Gonzalez R, Najorka J, Sun Y and Weiss DJ: A global
assessment of copper, zinc, and lead isotopes in mineral dust
sources and aerosols. Front Earth Sci. 8(167)2020.
|
|
25
|
Jickells TD, An ZS, Andersen KK, Baker AR,
Bergametti G, Brooks N, Cao JJ, Boyd PW, Duce RA, Hunter KA, et al:
Global iron connections between desert dust, ocean biogeochemistry,
and climate. Science. 308:67–71. 2005.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Sokan-Adeaga AA, Ana GREE, Sokan-Adeaga
MA, Sokan-Adeaga ED and Ejike OM: Secondary inorganic aerosols:
Impacts on the global climate system and human health. Biodiversity
Int J. 3:249–59. 2019.
|
|
27
|
Formenti P, Schütz L, Balkanski Y,
Desboeufs K, Ebert M, Kandler K, Petzold A, Scheuvens D, Weinbruch
S and Zhang D: Recent progress in understanding physical and
chemical properties of African and Asian mineral dust. Atmos Chem
Phys. 11:8231–8256. 2011.
|
|
28
|
González-Flórez C, Klose M, Alastuey A,
Dupont S, Escribano J, Etyemezian V, Gonzalez-Romero A, Huang Y,
Kandler K, Nikolich G, et al: Insights into the size-resolved dust
emission from field measurements in the Moroccan Sahara. Atmos Chem
Phys. 23:7177–7212. 2023.
|
|
29
|
Xing YF, Xu YH, Shi MH and Lian YX: The
impact of PM2.5 on the human respiratory system. J Thorac Dis.
8:E69–E74. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Candeias C, Vicente E, Tomé M, Rocha F,
Ávila P and Alves C: Geochemical, mineralogical and morphological
characterisation of road dust and associated health risks. Int J
Environ Res Public Health. 17(1563)2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Wagner F, Bortoli D, Pereira S, Costa MJ,
Maria Silva A, Weinzierl B, Esselborn M, Petzold A, Rasp K, Heinold
B and Tegen IN: of dust aerosol particles transported to Portugal
from the Sahara desert. Tellus B: Chem Phys Meteorol. 61:297–306.
2009.
|
|
32
|
Mallios SA, Drakaki E and Amiridis V:
Effects of dust particle sphericity and orientation on their
gravitational settling in the earth's atmosphere. J Aerosol Sci.
150(105634)2020.
|
|
33
|
Zhang J and Shao Y: A new parameterization
of particle dry deposition over rough surfaces. Atmos Chem Phys.
14:12429–12440. 2014.
|
|
34
|
Lian S, Zhou L, Murphy DM, Froyd KD, Toon
OB and Yu P: Global distribution of Asian, Middle Eastern, and
North African dust simulated by CESM1/CARMA. Atmos Chem Phys.
22:13659–13676. 2022.
|
|
35
|
Brook RD, Rajagopalan S, Pope CA III,
Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV,
Mittleman MA, et al: Particulate matter air pollution and
cardiovascular disease: An update to the scientific statement from
the American Heart Association. Circulation. 121:2331–2378.
2010.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Kim KH, Kabir E and Kabir S: A review on
the human health impact of airborne particulate matter. Environ
Int. 74:136–143. 2015.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Li N, Hao M, Phalen RF, Hinds WC and Nel
AE: Particulate air pollutants and asthma. A paradigm for the role
of oxidative stress in PM-induced adverse health effects. Clin
Immunol. 109:250–265. 2003.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Kelly FJ and Fussell JC: Size, source and
chemical composition as determinants of toxicity attributable to
ambient particulate matter. Atmos Environ. 60:504–526. 2012.
|
|
39
|
Guarnieri M and Balmes JR: Outdoor air
pollution and asthma. Lancet. 383:1581–1592. 2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Schraufnagel DE: The health effects of
ultrafine particles. Exp Mol Med. 52:311–317. 2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Perez L, Tobias A, Querol X, Künzli N, Pey
J, Alastuey A, Viana M, Valero N, González-Cabré M and Sunyer J:
Coarse particles from Saharan dust and daily mortality.
Epidemiology. 19:800–807. 2008.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Prospero JM, Blades E, Mathison G and
Naidu R: Interhemispheric transport of viable fungi and bacteria
from Africa to the Caribbean with soil dust. Aerobiologia. 21:1–9.
2005.
|
|
43
|
Gyan K, Henry W, Lacaille S, Laloo A,
Lamsee-Ebanks C, McKay S, Antoine RM and Monteil MA: African dust
clouds are associated with increased paediatric asthma accident and
emergency admissions on the Caribbean island of Trinidad. Int J
Biometeorol. 49:371–376. 2005.PubMed/NCBI View Article : Google Scholar
|
|
44
|
McElroy S, Dimitrova A, Evan A and
Benmarhnia T: Saharan dust and childhood respiratory symptoms in
Benin. Int J Environ Res Public Health. 19(4743)2022.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Pope CA III and Dockery DW: Health effects
of fine particulate air pollution: Lines that connect. J Air Waste
Manag Assoc. 56:709–742. 2006.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Mortimer KM, Neas LM, Dockery DW, Redline
S and Tager IB: The effect of air pollution on inner-city children
with asthma. Eur Respir J. 19:699–705. 2002.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Carrozzi L, Giuliano G, Viegi G, Paoletti
P, Di Pede F, Mammini U, Carmignani G, Saracci R, Giuntini C and
Lebowitz MD: The Po River Delta epidemiological study of
obstructive lung disease: Sampling methods, environmental and
population characteristics. Eur J Epidemiol. 6:191–200.
1990.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Asthma and Allergy Foundation of America.
Asthma facts and figures, 2020. Retrieved from https://www.aafa.org/asthma-facts/.
|
|
49
|
Mölter A, Simpson A, Berdel D, Brunekreef
B, Custovic A, Cyrys J, de Jongste J, de Vocht F, Fuertes E,
Gehring U, et al: A multicentre study of air pollution exposure and
childhood asthma prevalence: The ESCAPE project. Eur Respir J.
45:610–624. 2015.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Vodonos A, Friger M, Katra I, Avnon L,
Krasnov H, Koutrakis P, Schwartz J, Lior O and Novack V: The impact
of desert dust exposures on hospitalizations due to exacerbation of
chronic obstructive pulmonary disease. Air Qual Atmos Health.
7:433–439. 2014.
|
|
51
|
Kim CS and Hu SC: Regional deposition of
inhaled particles in human lungs: Comparison between men and women.
J Appl Physiol (1985). 84:1834–1844. 1998.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Seaton A, MacNee W, Donaldson K and Godden
D: Particulate air pollution and acute health effects. Lancet.
345:176–178. 1995.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Fan W and Zlatnik MG: Climate change and
pregnancy: Risks, mitigation, adaptation, and resilience. Obstet
Gynecol Surv. 78:223–236. 2023.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Sanders B and Davis M: Effects of climate
change and air pollution on perinatal health. J Midwifery Womens
Health. 68:383–390. 2023.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Aguilera J, Konvinse K, Lee A, Maecker H,
Prunicki M, Mahalingaiah S, Sampath V, Utz PJ, Yang E and Nadeau
KC: Air pollution and pregnancy. Semin Perinatol.
47(151838)2023.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Bongaerts E, Lecante LL, Bové H, Roeffaers
MBJ, Ameloot M, Fowler PA and Nawrot TS: Maternal exposure to
ambient black carbon particles and their presence in maternal and
fetal circulation and organs: an analysis of two independent
population-based observational studies. Lancet Planet Health.
6:e804–e811. 2022.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Seeni I, Ha S, Nobles C, Liu D, Sherman S
and Mendola P: Air pollution exposure during pregnancy: Maternal
asthma and neonatal respiratory outcomes. Ann Epidemiol.
28:612–618.e4. 2018.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Uwak I, Olson N, Fuentes A, Moriarty M,
Pulczinski J, Lam J, Xu X, Taylor BD, Taiwo S, Koehler K, et al:
Application of the navigation guide systematic review methodology
to evaluate prenatal exposure to particulate matter air pollution
and infant birth weight. Environ Int. 148(106378)2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Ciencewicki J and Jaspers I: Air pollution
and respiratory viral infection. Inhal Toxicol. 19:1135–1146.
2007.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Becker S, Soukup JM, Sioutas C and Cassee
FR: Response of human alveolar macrophages to ultrafine, fine, and
coarse urban air pollution particles. Exp Lung Res. 29:29–44.
2003.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Bredeck G, Dobner J, Rossi A and Schins
RPF: Saharan dust induces the lung disease-related cytokines
granulocyte-macrophage colony-stimulating factor and granulocyte
colony-stimulating factor. Environ Int. 186(108580)2024.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Cohen AJ, Brauer M, Burnett R, Anderson
HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L,
Dandona R, et al: Estimates and 25-year trends of the global burden
of disease attributable to ambient air pollution: An analysis of
data from the global burden of diseases study 2015. Lancet.
389:1907–1918. 2017.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Anderson JO, Thundiyil JG and Stolbach A:
Clearing the air: A review of the effects of particulate matter air
pollution on human health. J Med Toxicol. 8:166–175.
2012.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Mazzarella G, Ferraraccio F, Prati MV,
Annunziata S, Bianco A, Mezzogiorno A, Liguori G, Angelillo IF and
Cazzola M: Effects of diesel exhaust particles on human lung
epithelial cells: An in vitro study. Respir Med. 101:1155–1162.
2007.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Diaz-Sanchez D, Tsien A, Fleming J and
Saxon A: Combined diesel exhaust particulate and ragweed allergen
challenge markedly enhances human in vivo nasal ragweed-specific
IgE and skews cytokine production to a T helper cell 2-type
pattern. J Immunol. 158:2406–2413. 1997.PubMed/NCBI
|
|
66
|
Nel A, Xia T, Mädler L and Li N: Toxic
potential of materials at the nanolevel. Science. 311:622–627.
2006.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Valavanidis A, Fiotakis K and Vlachogianni
T: Airborne particulate matter and human health: Toxicological
assessment and importance of size and composition of particles for
oxidative damage and carcinogenic mechanisms. J Environ Sci Health
C Environ Carcinog Ecotoxicol Rev. 26:339–362. 2008.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Ghio AJ, Smith CB and Madden MC: Diesel
exhaust particles and airway inflammation. Curr Opin Pulm Med.
18:144–150. 2012.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Almeida-Silva M, Cardoso J, Alemão C,
Santos S, Monteiro A, Manteigas V and Marques-Ramos A: Impact of
particles on pulmonary endothelial cells. Toxics.
10(312)2022.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Pozzi R, De Berardis B, Paoletti L and
Guastadisegni C: Inflammatory mediators induced by coarse
(PM2.5-10) and fine (PM2.5) urban air particles in RAW 264.7 cells.
Toxicology. 183:243–254. 2003.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Becker S, Dailey LA, Soukup JM, Grambow
SC, Devlin RB and Huang YCT: Seasonal variations in air pollution
particle-induced inflammatory mediator release and oxidative
stress. Environ Health Perspect. 113:1032–1038. 2005.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Thompson JE: Airborne particulate matter:
Human exposure and health effects. J Occup Environ Med. 60:392–423.
2018.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Mar TF, Koenig JQ, Jansen K, Sullivan J,
Kaufman J, Trenga CA, Siahpush SH, Liu LJ and Neas L: Fine
particulate air pollution and cardiorespiratory effects in the
elderly. Epidemiology. 16:681–687. 2005.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Kelly FJ and Fussell JC: Linking ambient
particulate matter pollution effects with oxidative biology and
immune responses. Ann N Y Acad Sci. 1340:84–94. 2015.PubMed/NCBI View Article : Google Scholar
|
|
75
|
O'Neill MS, Veves A, Zanobetti A, Sarnat
JA, Gold DR, Economides PA, Horton ES and Schwartz J: Diabetes
enhances vulnerability to particulate air pollution-associated
impairment in vascular reactivity and endothelial function.
Circulation. 111:2913–2920. 2005.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Ghio AJ and Devlin RB: Inflammatory lung
injury after bronchial instillation of air pollution particles. Am
J Respir Crit Care Med. 164:704–708. 2001.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Li N, Sioutas C, Cho A, Schmitz D, Misra
C, Sempf J, Wang M, Oberley T, Froines J and Nel A: Ultrafine
particulate pollutants induce oxidative stress and mitochondrial
damage. Environ Health Perspect. 111:455–460. 2003.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Nunes C, Pereira AM and Morais-Almeida M:
Asthma costs and social impact. Asthma Res Pract.
3(1)2017.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Bredeck G, Busch M, Rossi A, Stahlmecke B,
Fomba KW, Herrmann H and Schins RPF: Inhalable Saharan dust induces
oxidative stress, NLRP3 inflammasome activation, and inflammatory
cytokine release. Environ Int. 172(107732)2023.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Jaspers I, Ciencewicki JM, Zhang W,
Brighton LE, Carson JL, Beck MA and Madden MC: Diesel exhaust
enhances influenza virus infections in respiratory epithelial
cells. Toxicol Sci. 85:990–1002. 2005.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Janssen NAH, Fischer P, Marra M, Ameling C
and Cassee FR: Short-term effects of PM2.5, PM10 and PM2.5-10 on
daily mortality in The Netherlands. Sci Total Environ.
463-464:20–26. 2013.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Grahame TJ, Klemm R and Schlesinger RB:
Public health and components of particulate matter: The changing
assessment of black carbon. J Air Waste Manag Assoc. 64:620–660.
2014.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Beelen R, Hoek G, van den Brandt PA,
Goldbohm RA, Fischer P, Schouten LJ, Jerrett M, Hughes E, Armstrong
B and Brunekreef B: Long-term effects of traffic-related air
pollution on mortality in a Dutch cohort (NLCS-AIR study). Environ
Health Perspect. 116:196–202. 2008.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Delfino RJ, Sioutas C and Malik S:
Potential role of ultrafine particles in associations between
airborne particle mass and cardiovascular health. Environ Health
Perspect. 113:934–946. 2005.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Chow JC, Watson JG, Edgerton SA and Vega
E: Chemical composition of PM2.5 and PM10 in Mexico City during
winter 1997. Sci Total Environ. 287:177–201. 2002.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Pope CA III, Burnett RT, Thun MJ, Calle
EE, Krewski D, Ito K and Thurston GD: Lung cancer, cardiopulmonary
mortality, and long-term exposure to fine particulate air
pollution. JAMA. 287:1132–1141. 2002.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Kelly FJ and Fussell JC: Air pollution and
airway disease. Clin Exp Allergy. 41:1059–1071. 2011.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Epton MJ, Dawson RD, Brooks WM, Kingham S,
Aberkane T, Cavanagh JAE, Frampton CM, Hewitt T, Cook JM, McLeod S,
et al: The effect of ambient air pollution on respiratory health of
school children: A panel study. Environ Health.
7(16)2008.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Yang CY, Huang CC, Chiu HF, Chiu JF, Lan
SJ and Ko YC: Effects of occupational dust exposure on the
respiratory health of Portland cement workers. J Toxicol Environ
Health. 49:581–588. 1996.PubMed/NCBI
|
|
90
|
Schwartz J and Dockery DW: Increased
mortality in Philadelphia associated with daily air pollution
concentrations. Am Rev Respir Dis. 145:600–604. 1992.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Martinez FD: Genes, environments,
development and asthma: A reappraisal. Eur Respir J. 29:179–184.
2007.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Vichit-Vadakan N and Vajanapoom N: Health
impact from air pollution in Thailand: Current and future
challenges. Environ Health Perspect. 119:A197–A198. 2011.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Rehfuess E, Mehta S and Prüss-Ustün A:
Assessing household solid fuel use: Multiple implications for the
millennium development goals. Environ Health Perspect. 114:373–378.
2006.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Bauer SE, Tsigaridis K and Miller RL:
Significant atmospheric aerosol pollution caused by world food
cultivation. Geophys Res Lett. 43:5394–5400. 2016.
|
|
95
|
Dockery DW and Pope CA III: Acute
respiratory effects of particulate air pollution. Annu Rev Public
Health. 15:107–132. 1994.PubMed/NCBI View Article : Google Scholar
|