Introduction
Colorectal cancer (CRC) is one of the most prevalent
types of cancer worldwide, with a varying incidence from country to
country. In the United States of America, it is the third most
commonly diagnosed cancer in both men and women, while it is the
most diagnosed cancer among men and the third most diagnosed cancer
among women in Saudi Arabia, as of a 2018 report (1). The incidence of CRC is increasing in
Saudi Arabia, with a median detection age of 55 years in women and
60 years in men (2). Despite being
less common in Saudi Arabia compared with some other countries, CRC
is the leading cause of cancer mortality among men and top five in
women (3). This represents a
significant health concern. The Saudi Ministry of Health aims to
reduce the impact of CRC by introducing screening and diagnostic
programs. CRC may occur infrequently due to genetic cancer
syndromes or inflammatory bowel disorders. However, even if they
don't meet the criteria for hereditary CRC, ~20% of all cases of
this disorder are considered to have some degree of familial risk
(4).
Certain risk factors, such as diet, smoking and
obesity, are associated with some of the most common forms of
cancer, including breast, gynaecological, liver and CRCs (5,6).
Obesity is characterized by the accumulation of excess body fat,
which leads to a higher risk of metabolic syndrome. The global
obesity epidemic is a significant public health issue, and Saudi
Arabia is one of the countries with the highest obesity rates, at
24% (7). As obesity becomes more
prevalent, research into the link between excess weight and CRC has
become more prominent. Based on multiple studies, obese patients
with CRC tend to have shorter survival rates, as discussed
previously (8,9)
Insulin resistance and hyperinsulinemia are
significant contributors to CRC (10,11).
Insulin resistance is a form of type 2 diabetes. Diabetes mellitus
(DM) is a general term that encompasses a wide range of metabolic
disorders, with chronic hyperglycaemia being the most common. Type
2 diabetes affects 18.3% of the population in Saudi Arabia
(12). Although various
epidemiological studies have shown that the prevalence of CRC is
higher among diabetic patients than non-diabetic individuals, some
studies, particularly those investigating the risk of CRC, have
considered type II diabetes as more prevalent and relevant
(13,14).
The liver plays a vital role in metabolism by
converting carbohydrates, fats, proteins and lipids into active
forms that circulate in the blood (15). Additionally, it functions to
detoxify harmful substances and produce essential enzymes for cell
growth and energy expenditure (16). Abnormalities in liver function can
result in various diseases including CRC (17) and cirrhosis (18). A recent UK biobank analysis
suggests that higher levels of alanine transaminase (ALT),
aspartate transferase (AST), total bilirubin (TBIL), γ-glutamyl
transferase (GGT), prothrombin time (PT) and albumin (ALB) may be
associated with lower risk for CRC (19). Studies have also found associations
between markers of liver function such as ALT bilirubin and albumin
with chronic illnesses including CRC as well as increased toxicity
among patients diagnosed with this type of cancer (19-21).
The purpose of the present study was to provide an
updated report on the rates of obesity and diabetes among CRC
patients in Saudi Arabia and to investigate how these conditions
were associated with the elevation of liver metabolite markers such
as ALT, AST, bilirubin, GGT, ALB and lactate dehydrogenase (LDH).
By doing so, the study aims to provide further evidence regarding
the role played by obesity and diabetes as widespread factors in
Saudi Arabia in the progression of CRC.
Patients and methods
Patient data
The present study was a retrospective chart review
that utilized medical records from the Saudi Ministry of National
Guards Hospital and Health Affairs, which is a tertiary hospital
located in Riyadh, Saudi Arabia. The study was approved by the King
Abdullah International Medical Research Center Institutional Review
Board (IRB), Ministry of National Guard-Health Affairs (approval
no. NRC22R/144/03). The IRB approved the waiver of informed consent
when using medical records since research involves no more than
minimal risk to the subjects.
The selection criteria included all medical records
of patients who were diagnosed with CRC between January 2015 and
December 2019 and met the inclusion criteria, which was a confirmed
CRC diagnosis. The present study employed a non-probability
consecutive sampling technique to select the patients, which means
all conveniently available populations were included. The
confounding variables were addressed through matching. The
assessment of each patient included their age, sex, body mass index
(BMI), complete blood cell count, haematocrit, haemoglobin,
platelet count, liver profile (TBIL, ALB, GGT, direct bilirubin,
AST, LDH, ALT and PT), kidney profile (creatinine, estimated
glomerular filtration rate) and diabetes status. Exclusion criteria
included patients with incomplete clinical records or missing
treatment information. The study included 147 women and 172 men.
The BMI was calculated according to standard scale: BMI ≥30 was
obese, ≥25 was overweight, ≥18.5 was normal and <18.5
kg/m2 was underweight as mentioned previously (22).
Statistical analysis
The present study used Epi Info 7.2.5 software
(trademark of CDC, USA) for statistical analysis of the data, a
tool designed for epidemiological statistics in public health
practice. To assess significance, a one-tailed P-value and employed
Pearson's χ2 test was used. P<0.05 was considered to
indicate a statistically significant difference. Significance
calculations were based on a confidence interval of 95%. In the
tables, (Row%) refers to row percentage which represents the
proportion or percentage of a specific row's value in relation to
the total of that row. Similarly, (Col%) refers to column
percentage which represents the proportion or percentage of a
specific column's value in relation to the total of that column.
The survival data was created by OncoLnc data portal (http://www.oncolnc.org/), which links survival data
from The Cancer Genome Atlas (TCGA) to mRNA, microRNA and long
non-coding RNA expression levels. The data was downloaded on July
1, 2023(23).
Results
Age groups and CRC prevalence
The present study reviewed 319 patients when
investigating the prevalence of CRC among different age groups
between January 2015 and December 2019 (Table I). The participants were divided
into four categories: i) Under 30 years; ii) 30-49 years; iii)
50-59 years; and iv) ≥60 years. Reviewing CRC frequencies showed
that there were only 3 individuals under the age of 30, while there
were 70 between the ages of 30 and 49 years, 115 between the ages
of 50 and 59 years, and 131 ≥60 years (Table I). The groups 50-59 years and ≥60
years had higher patient percentages, at 36.05 and 41.07%,
respectively. The other two groups of 30-49 years and <30 years
had less members, at 21.94 and 0.94%, respectively. The age range
for males was 24-95 years old, while that for females was 36-87
years old. The median age for the entire sample was 57 years, while
the median age was 58 years for men and 57 years for women.
Applying the null hypothesis revealed that age classification had
significant P-value (P<0.01) in comparison to the healthy
control (Table I).
 | Table IPrevalence of colorectal cancer in
correlation with age. |
Table I
Prevalence of colorectal cancer in
correlation with age.
| Age in years | n (%) | One-tailed
P-value |
|---|
| <30 | 3 (0.94) | 0.0001 |
| 30-49 | 70 (21.94) | 0.0034 |
| 50-59 | 115 (36.05) | 0.0067 |
| ≥60 | 131 (41.07) | 0.0082 |
| Total | 319 (100.00) | - |
Sex
In order to gain a deeper understanding of the
prevalence of CRC, an analysis of sex contributions to the
incidence of CRC was conducted. The participants were divided into
two categories based on sex: Male and female. The findings showed a
sex disparity in the incidence rates of CRC across age
demographics. Specifically, among female patients, 55 (37.41%) were
≥60 years, 57 (38.78%) were 50-59 years, 35 (23.81%) were 30-49
years and 0 (0.0%) were <30 years. Meanwhile, among male
patients, 76 (44.19%) were ≥60, 58 (33.72%) were 50-59 years, 35
(20.35%) were 30-49 years and 3 (1.74%) were <30 years (Table II).
 | Table IIInvestigating the prevalence of
colorectal cancer based on sex. |
Table II
Investigating the prevalence of
colorectal cancer based on sex.
| | Age in years | |
|---|
| Sex | <30 | 30-49 | 50-59 | ≥60` | Total |
|---|
| Female | 0 | 35 | 57 | 55 | 147 |
|
Row% | 0.00 | 23.81 | 38.78 | 37.41 | 100.00 |
|
Col% | 0.00 | 50.00 | 49.57 | 41.98 | 46.08 |
| Male | 3 | 35 | 58 | 76 | 172 |
|
Row% | 1.74 | 20.35 | 33.72 | 44.19 | 100.00 |
|
Col% | 100.00 | 50.00 | 50.43 | 58.02 | 53.92 |
| Total | 3 | 70 | 115 | 131 | 319 |
|
Row% | 0.94 | 21.94 | 36.05 | 41.07 | 100.00 |
|
Col% | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
This analysis revealed that males had a higher
percentage of CRC incidence compared with females in two age
groups: ≥60 and <30 years. Specifically, the incidence rate of
CRC among males was 16% higher for those ≥60 years and 100% for
those <30 years when compared with females of the same age
groups. These results may be of value in developing sex-specific
strategies for the prevention and treatment of CRC.
BMI
The results presented in Table III present the investigation into
the relationship between BMI measurements and their association
with CRC. Patients were classified into normal, underweight,
overweight or obese categories based on BMI. Frequency and
percentage data were obtained for each group by sex. The results
reveal that the majority of patients with CRC 185 (57.9%) are
overweight, which includes obese patients. Notably, participants
with a normal BMI had a higher occurrence rate of CRC 112 (35.11%)
compared with those with an underweight BMI category 22 (6.90%).
This emphasizes the significance of maintaining lower BMI even if
less than normal healthy weight levels when it comes to preventing
and managing this type of cancer effectively. These numbers failed
to confirm association statistically, as χ2=5.38 and
P=0.145.
 | Table IIIAssociation between obesity (body
mass index) and sex of colorectal cancer. |
Table III
Association between obesity (body
mass index) and sex of colorectal cancer.
| | BMI status | |
|---|
| Sex | Normal | Obese | Overweight | Underweight | Total |
|---|
| Female, n (%) | 45 (30.61) | 55 (37.41) | 36 (24.49) | 11 (7.48) | 147 (100.00) |
| Male, n (%) | 67 (38.95) | 45 (26.16) | 49 (28.49) | 11 (6.40) | 172 (100.00) |
| Total, n (%) | 112 (35.11) | 100 (31.35) | 85 (26.65) | 22 (6.90) | 319 (100.00) |
Obesity and diabetes
The study investigated the link between
obesity-related complications and diabetes incidence in 319
participants with CRC. The results, presented in Table IV, showed that out of a total of
147 women and 172 men, only 63 female patients (42.86%) did not
have diabetes while the rest did; similarly, for males, only 59
(34.30%) did not have diabetes compared with 113 (65.70%) males who
did. Measurement of risk ratio, risk differences and odd ratio
turn-out to be 1.25, 8.55 and 1.44, respectively, at 95% confidence
interval. The positive risk and odd ratio in these findings
strongly suggest an association between CRC and diabetes among both
sexes (P=0.05). Although more research is required to determine
precisely how this connection occurs, these results indicate that
people with type II Diabetes are at greater risk for developing CRC
compared with those without it due to their condition caused by
excessive body weight which can lead them into a higher rate of
health problems associated with overweight or obese
individuals.
 | Table IVAssociation between colorectal cancer
with diabetes among both male and female populations. |
Table IV
Association between colorectal cancer
with diabetes among both male and female populations.
| | Diabetes
(yes/no) | |
|---|
| Sex | No | Yes | Total |
|---|
| Female, n (%) | 63 (42.86) | 84 (57.14) | 147 (100.00) |
| Male, n (%) | 59 (34.30) | 113 (65.70) | 172 (100.00) |
| Total, n (%) | 122 (38.24) | 197 (61.76) | 319 (100.00) |
Obesity and liver disease
The present study examined liver metabolite
abnormalities in patients with CRC who were overweight or obese and
diabetic to investigate the association between excess weight,
diabetes and liver function markers. The objective was to establish
a possible link between these factors. The results revealed that
106 (33.23%) of obese patients with CRC had significantly elevated
levels of GGT enzyme (P=0.026; Table
V). However, most overweight or obese patients with CRC showed
normal levels of other indicators including ALT, LDH, AST, ALB and
TBIL (Table SI, Table SII, Table SIII, Table SIV and Table SV). Improving our understanding of
how obesity and diabetes affect the liver can be beneficial for
managing related health issues among CRC sufferers.
 | Table VAssociation between high body mass
index and liver function metabolites in patients with colorectal
cancer. |
Table V
Association between high body mass
index and liver function metabolites in patients with colorectal
cancer.
| BMI vs. liver
GGT | n (%) |
|---|
| Abnormal liver
GGT | 106 (33.23) |
| Not overweight with
abnormal GGT | 135 (42.32) |
| Normal liver
GGT | 78 (24.45) |
| Total | 319 (100.00) |
Obesity and GGT
In 197 diabetic patients with CRC, the present study
examined a link between overweight/or obesity and GGT levels when
compared to 122 non-diabetic patients with CRC in Table VI. The subjects were split into
four groups based on their GGT and whether they had diabetes. The
first group was made up of 33 people (27.05%), all of whom had a
normal BMI and did not have diabetes. The second group was made up
of 45 individuals (22.84%) with diabetes and a normal BMI. The
third group had 38 patients (31.15%), none of whom had diabetes but
whose BMI was abnormally high. The fourth group was made up of 16
patients (13%), all of whom had diabetes and an abnormal BMI. The
result of this categorization (data not shown) show that there were
more people with diabetes in the normal BMI group 45 (57.69%) than
people without diabetes 33 (42.31%) in the normal group. In the
group of people with an abnormal BMI, there were more people with
diabetes 68 (64.15%) than people without diabetes 38 (35.85%)
(P=0.04; Table VI).
 | Table VIAssociation between body mass index,
GGT levels and diabetic status in patients with colorectal
cancer. |
Table VI
Association between body mass index,
GGT levels and diabetic status in patients with colorectal
cancer.
| | Diabetes
(yes/no) | |
|---|
| BMI vs. liver
GGT | No | Yes | Total |
|---|
| Abnormal, n
(%) | 38 (35.85) | 68 (64.15) | 106 (100.00) |
| NA, n (%) | 51 (37.78) | 84 (62.22) | 135 (100.00) |
| Normal, n (%) | 33 (42.31) | 45 (57.69) | 78 (100.00) |
| Total, n (%) | 122 (38.24) | 197 (61.76) | 319 (100.00) |
Diabetes and GGT
The present study subsequently evaluated patients
with CRC exhibiting GGT abnormalities and further classified these
patients based on their diabetic status, as shown in Table VII. Out of the total 183
patients, 44 (55.70%) of the women were diabetic and 35 (44.30%)
were non-diabetic. By contrast, 71 (68.27%) of the men were
diabetic and 33 (31.73%) were non-diabetic. Notably, the risk
ratio, risk differences and odds ratio increased to 1.39, 12.57 and
1.71, respectively. These changes were significant (P=0.05).
 | Table VIIAssociation between abnormal GGT
levels and diabetic status then weighted by sex in patients with
colorectal cancer. |
Table VII
Association between abnormal GGT
levels and diabetic status then weighted by sex in patients with
colorectal cancer.
| | Diabetes
(yes/no) | |
|---|
| Sex | No | Yes | Total |
|---|
| Female, n (%) | 35 (44.30) | 44 (55.70) | 79 (100.00) |
| Male, n (%) | 33 (31.73) | 71 (68.27) | 104 (100.00) |
| Total, n (%) | 68 (37.16) | 115 (62.84) | 183 (100.00) |
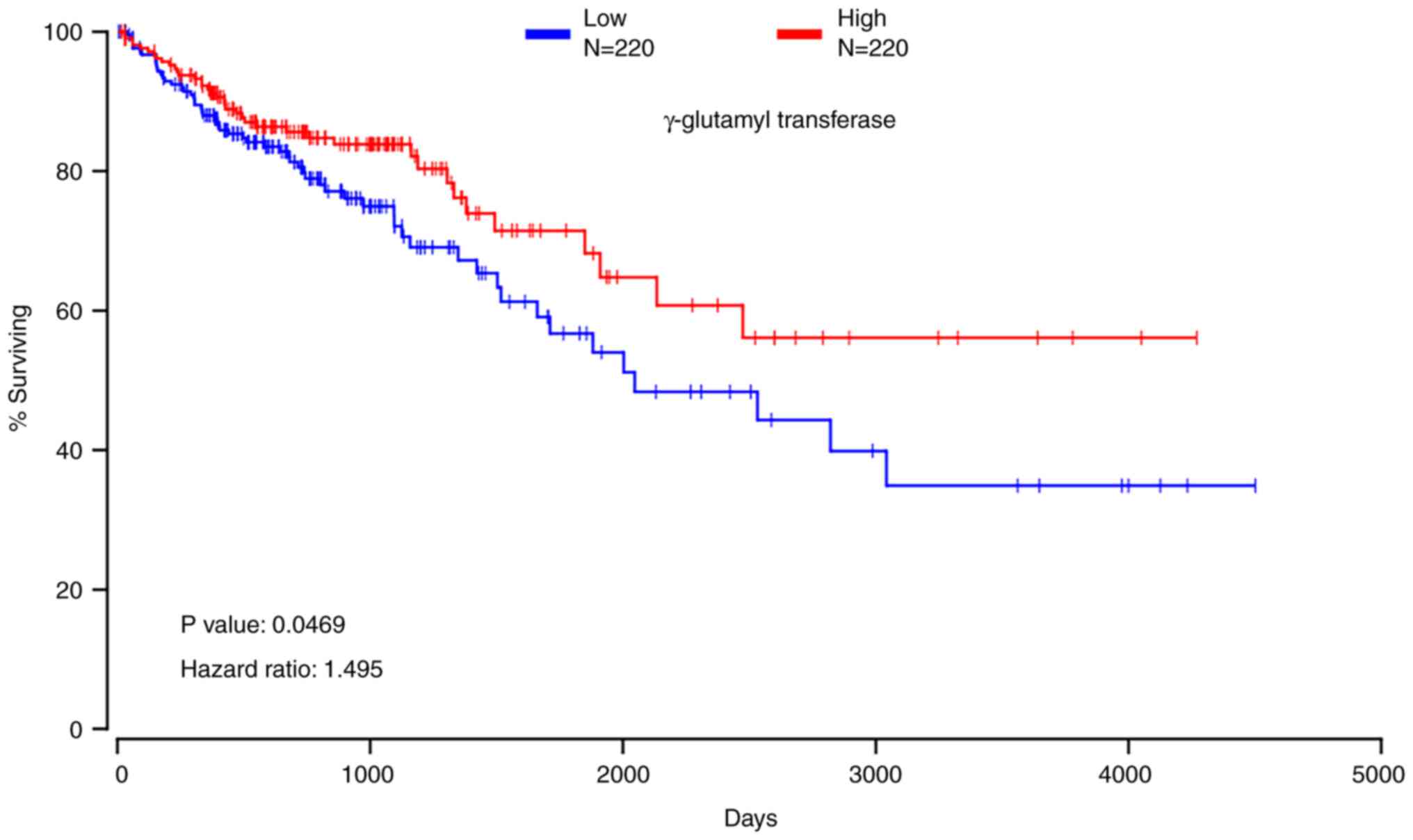
GGT level in public database
The present study analysed the levels of GGT6 in
colon adenocarcinoma, using TCGA database through Oncolnc tool. The
OncoLnc is a data portal that explore correlations between survival
data and gene expression from TCGA. Based on the data, the present
study reported a significant correlation (P=0.0469) between the
reduction in GGT6 and poor prognosis, as depicted in Fig. 1.
Discussion
CRC ranks as the third most prevalent type of cancer
worldwide and stands as the second leading cause of death from
cancer (1). Unhealthy lifestyle
habits, such as high BMI, smoking, alcohol consumption and poor
diet have been associated with CRC onset (13). Notably, several studies also link
hyperglycaemia to a higher incidence of CRC (24). Another study based on UK biobank
data highlights that liver enzymes play an essential role in CRC
progression (19). The present
research revealed that individuals diagnosed with CRC were more
likely to be diabetic or overweight. Furthermore, the present study
suggested that the GGT enzyme could serve as a valuable predictive
marker for detecting early-stage colon cancers.
A previous study conducted by The International
Agency for Research on Cancer stated that cancer incidence and
prevalence generally increase with age, particularly after the age
of 50(25). Additionally, it has
been established that there exists an association between sex and
CRC incidence, wherein men are at higher risk for developing CRC
compared with women. The same study revealed that ~23 out of every
100,000 men have this condition in comparison to only ~16 cases per
100,000 women (25). Most
participants in the present research were aged >50 years, which
further supports the link between patient age and CRC progression.
The finding also suggests sex differences play a role in
contributing towards the development of CRC as more males had this
disease compared with females.
Based on the present results, it appeared that
individuals aged ≥60 years had a significantly higher incidence
rate of CRC (41.07%), whereas those aged <30 years have an
incidence rate of only 0.94%. A two-tailed test conducted on the
data revealed a significant difference between the two groups, with
P=0.001. These results highlight the crucial role of age as a
predictive factor in preventing and treating CRC. Consequently,
there is a need to implement age-specific screening measures as a
critical preventive measure against this illness.
The analysis conducted on the incidence of CRC in
males and females shows that males may be at a higher risk of
developing this malignancy than females. The data suggested that,
despite advancements in cancer prevention and diagnosis, males
continue to have a higher incidence rate, indicating the urgency
for further research on colon cancer prevention. These findings
underscore the need for more focused and concerted efforts on colon
cancer prevention and research among males. Additionally, more
extensive research is required to better understand the underlying
mechanisms of this malignancy. Such understanding can help in
developing targeted and effective intervention strategies to curb
the rise in the incidence of CRC, especially among males, and
mitigate the burden of this disease on population health.
The connection between obesity and CRC is well
established, with the accumulation of visceral adipose tissue (VAT)
serving as a hallmark for this condition (26,27).
Lipoid tissues are responsible for secreting hormones such as
leptin, adiponectin and resistin, which can have an impact on
insulin resistance (28,29). The build-up of VAT in the body
creates a state of persistent low-grade systemic inflammation that
exacerbates insulin resistance (30,31).
The accumulation of VAT can cause persistent low-grade inflammation
that worsens insulin resistance and promotes tumour growth within
the microenvironment (32). The
measures used to determine obesity include both BMI and waist
circumference. The present study relied solely on BMI to evaluate
obesity, which provided further evidence for obesity being a
significant risk factor for CRC development as previously reported
(33).
Diabetes is associated with several types of cancer,
including colon, liver, pancreas, endometrial and breast cancer
(34). Both diabetes and obesity
lead to insulin resistance and hyperinsulinemia in patients
triggering cell signalling pathways that cause tumorigenesis
(35). The insulin-like growth
factor 1 signalling pathway promotes cell proliferation while
inhibiting apoptosis in CRC cells (36). The present study showed a
prevalence of ≥60% for obesity and diabetes among patients with
CRC; hence it is imperative to manage these conditions to prevent
CRC.
In a recent UK biobank data analysis, it was found
that higher levels of ALT, AST, TBIL, GGT, PT and ALB are
associated with lower risk for CRC (19). Furthermore, previous studies have
indicated a correlation between liver function markers such as ALT,
bilirubin and ALB with chronic diseases, including CRC (19-21).
To better understand the impact of the GGT enzyme in CRC, the
current study examined the levels of GGT6 in colon adenocarcinoma
from TCGA database. The findings showed a significant association
(P=0.0469) between the downregulation of GGT6 and poor prognosis.
The present study in Saudi Arabia supports previous reports that
suggest using abnormal liver enzymes as markers in patients with
CRC. The present study revealed that obese individuals had elevated
levels of GGT, which confirmed and complemented previous research
(37-39).
Additionally, the current study revealed that diabetic individuals
with CRC also had high levels of GGT, indicating its potential use
as an indicator marker for overweight or diabetic patients with
CRC.
The present study revealed a low familial prevalence
of CRC with only 0.62% (1 patient) of participants reporting a
family history. This may suggest a lower genetic predisposition in
our sample, or possibly underreporting. However, in line with the
majority of CRC cases being sporadic, 49.69% (80 patients) of the
study participants had no family history of the disease,
emphasizing the significance of lifestyle factors and acquired
genetic mutations in CRC development.
The management strategies for GGT involve several
aspects. Monitoring GGT levels can help assess liver function and
detect any liver damage or disease. Additionally, GGT levels can be
used as a biomarker to evaluate the effectiveness of treatment and
predict outcomes in patients with CRC with hepatic metastases
(40). In the clinical management
of CRC, patient-reported outcomes (PROs) play a crucial role.
Self-reported symptoms, including those related to liver function,
can guide the management of patients with CRC. Incorporating PROs
into clinical trials and routine practice helps assess treatment
efficacy and measure health-related quality of life (41).
It is important to note that GGT is not a direct
treatment target in CRC management. Instead, it serves as an
indicator of liver function and can provide valuable information
for healthcare providers in monitoring and managing patients with
CRC. The specific management strategies for GGT in CRC may vary
depending on individual patient characteristics and the overall
treatment plan. Therefore, it is essential for healthcare providers
to interpret GGT test results in conjunction with other clinical
information and tailor management strategies accordingly.
In summary, the current study highlighted the
critical role of obesity and diabetes as major risk factors for the
development of CRC in Saudi Arabia and potentially across the Arab
States of the Gulf region. It is important to recognize the
limitations of generalizing these findings to other populations.
Conducting additional research with larger and more diverse cohorts
would be valuable in confirming the observed associations and
examining potential variations across populations. These conditions
harm the colonic epithelium, leading to an increase in tumour
formation that can metastasize and result in cancer-related deaths
if left untreated. Additionally, we recommend further research to
investigate the mechanisms connecting obesity, diabetes and CRC
development, which would contribute to the existing knowledge in
the field. Moreover, the present research draws attention to the
growing incidence of CRC and proposes the need for preventive
measures to curb its rise. Our research provides valuable insights
into CRC prevalence, associated factors and the potential link
between CRC and liver function enzymes in Saudi Arabia. This
enhances our understanding of this significant health issue.
Supplementary Material
Level of LDH in circulation of
overweight (high BMI) patients.
Level of ALB in circulation of
overweight (high BMI) patients.
Level of ALT in circulation of
overweight (high BMI) patients.
Level of AST in circulation of
overweight (high BMI) patients.
Level of TBIL in circulation for
overweight (high BMI) patients.
Acknowledgements
The authors would like to thank Dr Suliman Alghnam,
Chairman of Data Management, from King Abdullah International
Medical Research Center (Riyadh, Saudi Arabia) for facilitating
data collection. TCGA database and OncoLnc were utilized for data
analysis and description in this manuscript (23).
Funding
Funding: This research was funded by King Abdullah International
Medical Research Center (grant no. NRC22R/144/03).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AMAlm, RHA, NFB and HHA collected data and organized
it. GA, JAA, AMAlj and BMA analysed data. GA validated the data.
BMA and GA supervised the project and wrote manuscript. BMA
obtained resources. GA and BMA confirm the authenticity of all the
raw data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The Institutional Review Board of The Ministry of
National Guard-Health Affairs approved this project (approval no.
NRC22R/144/03).
Patient consent for publication
This work involves searching and analysing a
hospital database, and the Institutional Review Board has waived
the requirement for patient consent since no patients' identifiable
information will be disclosed, and all data were coded and
delinked.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rawla P, Sunkara T and Barsouk A:
Epidemiology of colorectal cancer: Incidence, mortality, survival,
and risk factors. Prz Gastroenterol. 14:89–103. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Registry SC: Kingdom of Saudi Arabia Saudi
Health council national health information center Saudi cancer
registry. Saudi Health Council https://shc.gov.sa/Arabic/NCC/Activities/AnnualReports/2018.pdf2018.
|
|
3
|
Aleanizy FS, Alqahtani FY, Alanazi MS,
Mohamed RAEH, Alrfaei BM, Alshehri MM, AlQahtani H, Shamlan G,
Al-Maflehi N, Alrasheed MM and Alrashed A: Clinical characteristics
and risk factors of patients with severe COVID-19 in Riyadh, Saudi
Arabia: A retrospective study. J Infect Public Health.
14:1133–1138. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jasperson KW, Tuohy TM, Neklason DW and
Burt RW: Hereditary and familial colon cancer. Gastroenterology.
138:2044–2058. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sawicki T, Ruszkowska M, Danielewicz A,
Niedźwiedzka E, Arłukowicz T and Przybyłowicz KE: A review of
colorectal cancer in terms of epidemiology, risk factors,
development, symptoms and diagnosis. Cancers (Basel).
13(2025)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Balwan WK and Kour S: Lifestyle diseases:
The link between modern lifestyle and threat to public health.
Saudi J Med Pharm Sci. 7:179–184. 2021.
|
|
7
|
Althumiri NA, Basyouni MH, AlMousa N,
AlJuwaysim MF, Almubark RA, BinDhim NF, Alkhamaali Z and Alqahtani
SA: Obesity in Saudi Arabia in 2020: Prevalence, distribution, and
its current association with various health conditions. Healthcare
(Basel). 11(311)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cavagnari MAV, Silva TD, Pereira MAH,
Sauer LJ, Shigueoka D, Saad SS, Barão K, Ribeiro CCD and Forones
NM: Impact of genetic mutations and nutritional status on the
survival of patients with colorectal cancer. BMC Cancer.
19(644)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Capece D, D'Andrea D, Begalli F, Goracci
L, Tornatore L, Alexander JL, Di Veroli A, Leow SC, Vaiyapuri TS,
Ellis JK, et al: Enhanced triacylglycerol catabolism by
carboxylesterase 1 promotes aggressive colorectal carcinoma. J Clin
Invest. 131(e137845)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Liu T, Zhang Q, Wang Y, Ma X, Zhang Q,
Song M, Cao L and Shi H: Association between the TyG index and
TG/HDL-C ratio as insulin resistance markers and the risk of
colorectal cancer. BMC Cancer. 22(1007)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Màrmol JM, Carlsson M, Raun SH, Grand MK,
Sørensen J, Lehrskov LL, Richter EA, Norgaard O and Sylow L:
Insulin resistance in patients with cancer: A systematic review and
meta-analysis. Acta Oncol. 62:364–371. 2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Gosadi IM: Lifestyle counseling for
patients with type 2 diabetes in the Southwest of Saudi Arabia: An
example of healthcare delivery inequality between different
healthcare settings. J Multidiscip Healthc. 14:1977–1986.
2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Yu J, Feng Q, Kim JH and Zhu Y: Combined
Effect of healthy lifestyle factors and risks of colorectal
adenoma, colorectal cancer, and colorectal cancer mortality:
Systematic review and meta-analysis. Front Oncol.
12(827019)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Krämer HU, Schöttker B, Raum E and Brenner
H: Type 2 diabetes mellitus and colorectal cancer: Meta-analysis on
sex-specific differences. Eur J Cancer. 48:1269–1282.
2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Rui L: Energy metabolism in the liver.
Compr Physiol. 4:177–197. 2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Casas-Grajales S and Muriel P:
Antioxidants in liver health. World J Gastrointest Pharmacol Ther.
6:59–72. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jiang H, Dong L, Gong F, Gu Y, Zhang H,
Fan D and Sun Z: Inflammatory genes are novel prognostic biomarkers
for colorectal cancer. Int J Mol Med. 42:368–380. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Alrfaei BM, Almutairi AO, Aljohani AA,
Alammar H, Asiri A, Bokhari Y, Aljaser FS, Abudawood M and Halwani
M: Electrolytes play a role in detecting cisplatin-induced kidney
complications and may even prevent them-retrospective analysis.
Medicina (Kaunas). 59(890)2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
He MM, Fang Z, Hang D, Wang F,
Polychronidis G, Wang L, Lo CH, Wang K, Zhong R, Knudsen MD, et al:
Circulating liver function markers and colorectal cancer risk: A
prospective cohort study in the UK Biobank. Int J Cancer.
148:1867–1878. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Khoei NS, Jenab M, Murphy N, Banbury BL,
Carreras-Torres R, Viallon V, Kühn T, Bueno-de-Mesquita B,
Aleksandrova K, Cross AJ, et al: Circulating bilirubin levels and
risk of colorectal cancer: Serological and Mendelian randomization
analyses. BMC Med. 18(229)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lv L, Sun X, Liu B, Song J, Wu DJH, Gao Y,
Li A, Hu X, Mao Y and Ye D: Genetically predicted serum albumin and
risk of colorectal cancer: A bidirectional mendelian randomization
study. Clin Epidemiol. 14:771–778. 2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Alqahtani FY, Aleanizy FS, Mohamed RAEH,
l-Maflehi N, Alrfaei BM, Almangour TA, Alkhudair N, Bawazeer G,
Shamlan G and Alanazi MS: Association between obesity and COVID-19
disease severity in Saudi Population. Diabetes Metab Syndr Obes.
15:1527–1535. 2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Anaya J: OncoLnc: linking TCGA survival
data to mRNAs, miRNAs, and lncRNAs. PeerJ Computer Science.
2(e67)2016.
|
|
24
|
González N, Prieto I, Del Puerto-Nevado L,
Portal-Nuñez S, Ardura JA, Corton M, Fernández-Fernández B,
Aguilera O, Gomez-Guerrero C, Mas S, et al: 2017 update on the
relationship between diabetes and colorectal cancer: Epidemiology,
potential molecular mechanisms and therapeutic implications.
Oncotarget. 8:18456–18485. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
International Agency for Research on
Cancer: Globocan 2018: Cancer Fact Sheets-Colorectal Cancer.
https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf.
Accessed, March 20, 2023.
|
|
26
|
Bardou M, Barkun AN and Martel M: Obesity
and colorectal cancer. Gut. 62:933–947. 2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chaplin A, Rodriguez RM, Segura-Sampedro
JJ, Ochogavía-Seguí A, Romaguera D and Barceló-Coblijn G: Insights
behind the relationship between colorectal cancer and obesity: Is
visceral adipose tissue the missing link? Int J Mol Sci.
23(13128)2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Stern JH, Rutkowski JM and Scherer PE:
Adiponectin, leptin, and fatty acids in the maintenance of
metabolic homeostasis through adipose tissue crosstalk. Cell Metab.
23:770–784. 2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zieba D, Biernat W and Barć J: Roles of
leptin and resistin in metabolism, reproduction, and leptin
resistance. Domest Anim Endocrinol. 73(106472)2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Bullon-Vela V, Abete I, Tur JA, Konieczna
J, Romaguera D, Pintó X, Corbella E, Martínez-González MA,
Sayón-Orea C, Toledo E, et al: Relationship of visceral adipose
tissue with surrogate insulin resistance and liver markers in
individuals with metabolic syndrome chronic complications. Ther Adv
Endocrinol Metab. 11(2042018820958298)2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Zatterale F, Longo M, Naderi J, Raciti GA,
Desiderio A, Miele C and Beguinot F: Chronic adipose tissue
inflammation linking obesity to insulin resistance and type 2
diabetes. Front Physiol. 10(1607)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Lee JY, Lee HS, Lee DC, Chu SH, Jeon JY,
Kim NK and Lee JW: Visceral fat accumulation is associated with
colorectal cancer in postmenopausal women. PLoS One.
9(e110587)2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Lauria MW, Moreira LM, Machado-Coelho GL,
Neto RM, Soares MM and Ramos AV: Ability of body mass index to
predict abnormal waist circumference: Receiving operating
characteristics analysis. Diabetol Metab Syndr.
5(74)2013.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Giovannucci E, Harlan DM, Archer MC,
Bergenstal RM, Gapstur SM, Habel LA, Pollak M, Regensteiner JG and
Yee D: Diabetes and cancer: A consensus report. Diabetes Care.
33:1674–1685. 2010.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Wondmkun YT: Obesity, insulin resistance,
and type 2 diabetes: Associations and therapeutic implications.
Diabetes Metab Syndr Obes. 13:3611–3616. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Kasprzak A: Insulin-like growth factor 1
(IGF-1) signaling in glucose metabolism in colorectal cancer. Int J
Mol Sci. 22(6434)2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Liu C, Shao M, Lu L, Zhao C, Qiu L and Liu
Z: Obesity, insulin resistance and their interaction on liver
enzymes. PLoS one. 16(e0249299)2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Verrijken A, Francque S, Mertens I,
Talloen M, Peiffer F and Van Gaal L: Visceral adipose tissue and
inflammation correlate with elevated liver tests in a cohort of
overweight and obese patients. Int J Obes. 34:899–907.
2010.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ali N, Sumon AH, Fariha KA, Asaduzzaman M,
Kathak RR, Molla NH, Mou AD, Barman Z, Hasan M, Miah R and Islam F:
Assessment of the relationship of serum liver enzymes activity with
general and abdominal obesity in an urban Bangladeshi population.
Sci Rep. 11(6640)2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Brennan PN, Dillon JF and Tapper EB:
Gamma-Glutamyl transferase (γ-GT)-an old dog with new tricks? Liver
Int. 42:9–15. 2022.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Xiao B, Peng J, Tang J, Deng Y, Zhao Y, Wu
X, Ding P, Lin J and Pan Z: Serum Gamma Glutamyl transferase is a
predictor of recurrence after R0 hepatectomy for patients with
colorectal cancer liver metastases. Ther Adv Med Oncol.
12(1758835920947971)2020.PubMed/NCBI View Article : Google Scholar
|