Introduction
Recent advancements in breast cancer treatment have
established chemotherapy, hormone therapy, and radiation therapy as
standard adjuvant therapies after surgery (1). Additionally, CDK4/6 inhibitors are
recommended as the first-line treatment for hormone
receptor-positive, HER2-negative advanced, or recurrent breast
cancer in combination with endocrine therapies, such as aromatase
inhibitors or fulvestrant. This combination substantially improves
the progression-free survival of patients (2-4).
In addition, abemaciclib in an adjuvant setting improves the
invasive disease-free survival in patients with high-risk
HR+/HER2-early breast cancer (1).
However, these treatments are associated with a potential risk of
inducing interstitial pneumonitis, which can sometimes become
severe and impact subsequent treatments. Herein, we report a case
of acute fibrinous and organizing pneumonia (AFOP) diagnosed using
transbronchial lung cryobiopsy (TBLC), complicating adjuvant
therapy in a patient who had undergone surgical intervention for
breast cancer.
Case report
A 52-year-old woman underwent left total mastectomy
with axillary dissection and right total mastectomy for pT2N3aM0
stage IIIC breast cancer (left breast; invasive ductal carcinoma,
estrogen receptor-positive, progesterone receptor-negative, Ki-67
25%) and pTisN0M0 stage 0 breast cancer (right breast; ductal
carcinoma in situ, estrogen receptor-positive, progesterone
receptor-positive, Ki-67 5%). Post-surgery, the patient received
adjuvant therapy consisting of four cycles of dose-dense
doxorubicin and cyclophosphamide chemotherapy, four cycles of
dose-dense paclitaxel monotherapy, tamoxifen hormone therapy, and
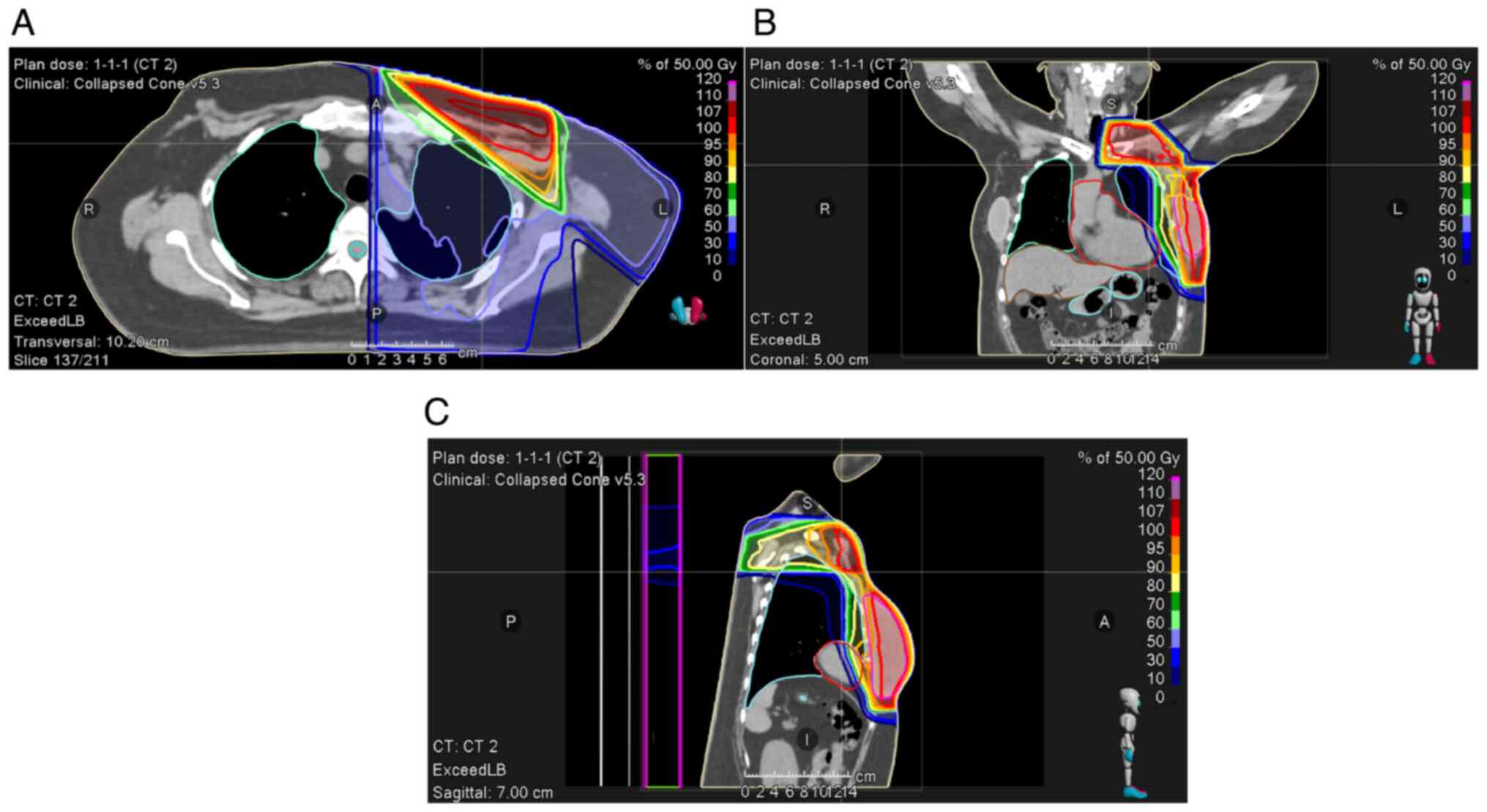
tangential irradiation therapy of 50 Gy in 25 fractions (Fig. 1). The radiation therapy caused
erythema at the irradiation site, which improved after application
of dimethyl isopropyl azulene ointment (dermatitis radiation grade
2). On day 366 after mastectomy and 20 days after the completion of
radiation therapy, the adjuvant therapy with abemaciclib (300
mg/day) was initiated. On day 85 of abemaciclib treatment and 157
days after completion of radiation therapy, the patient presented
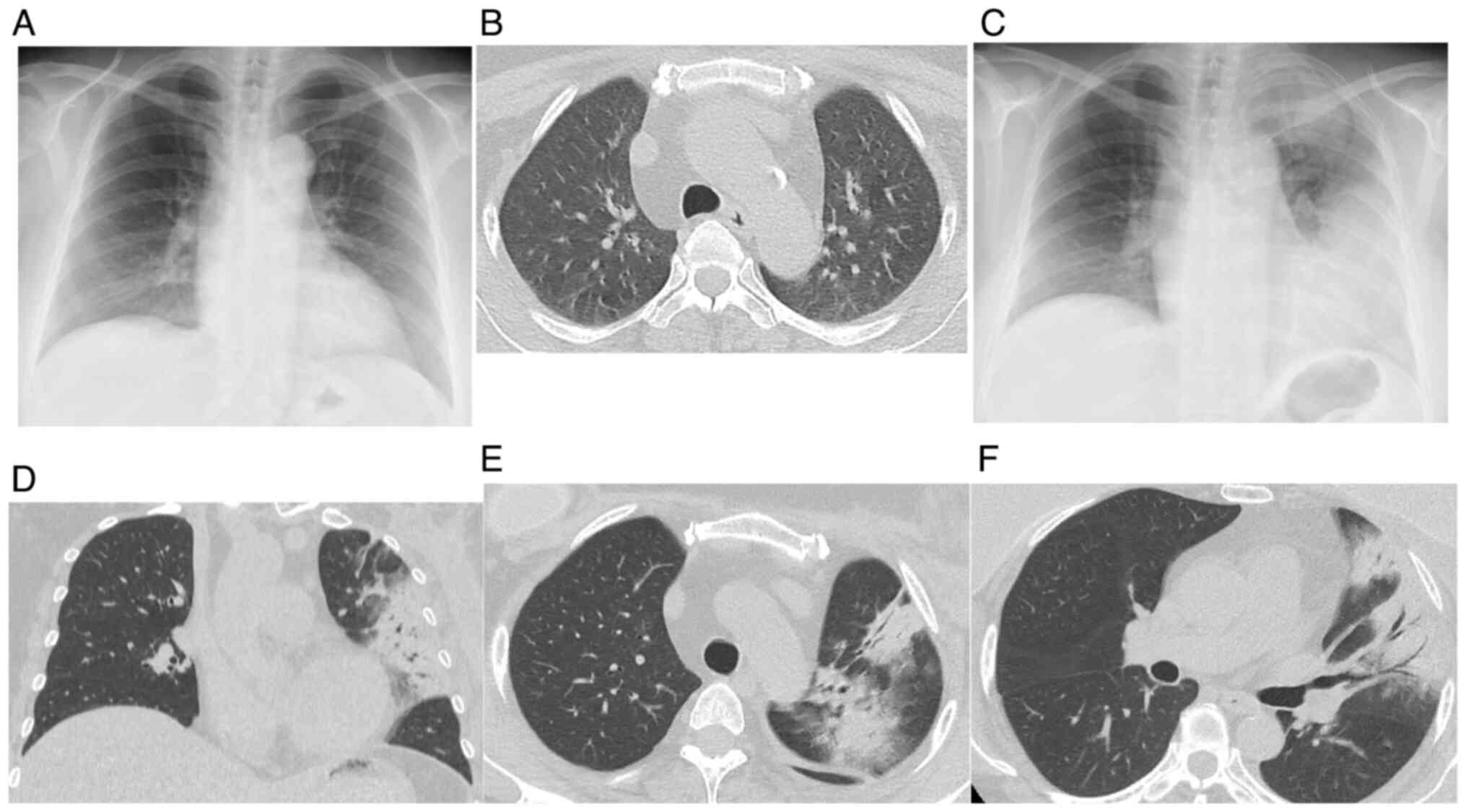
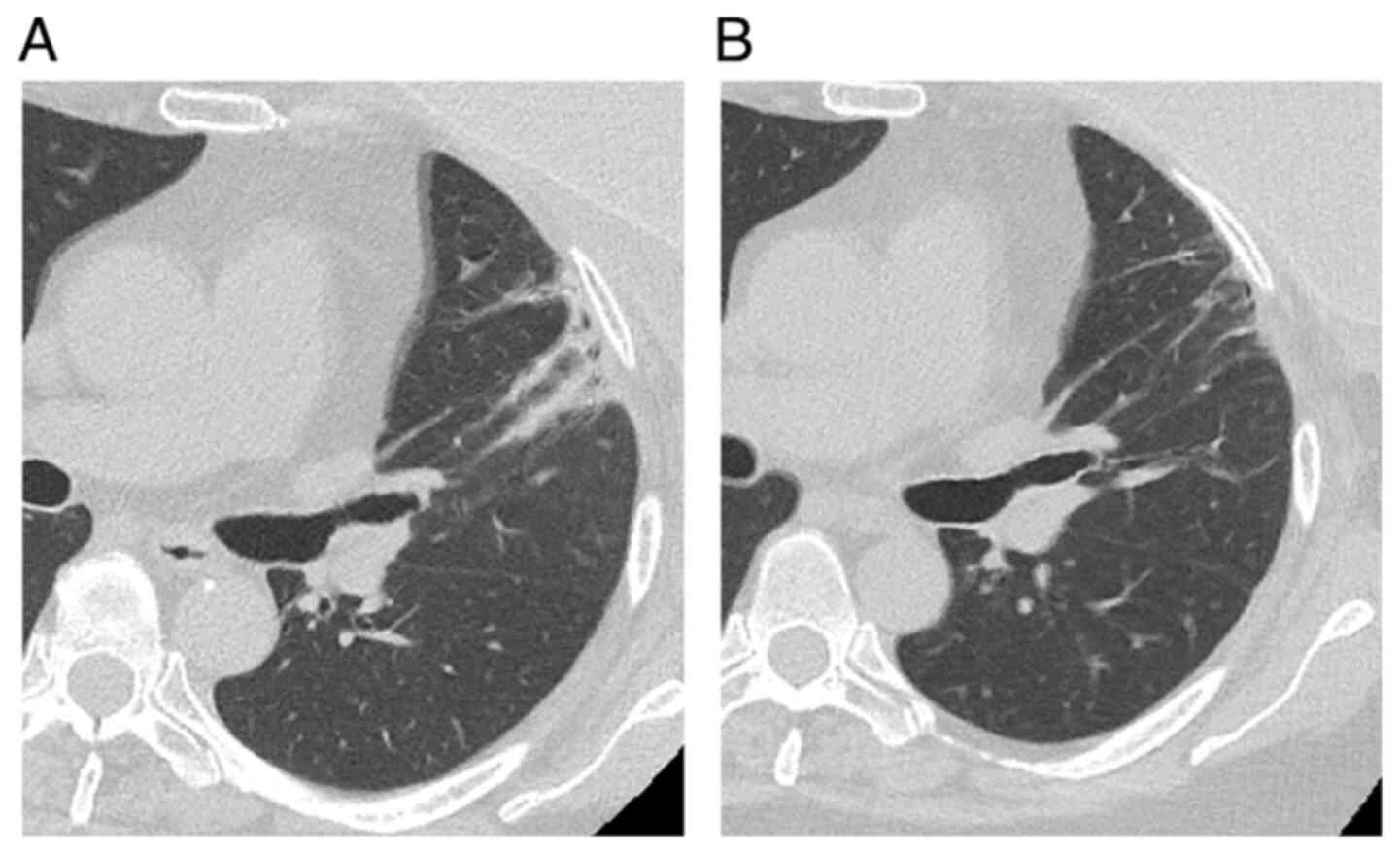
with a history of cough, fever, and dyspnea for 1 week. CT findings
were suggestive of interstitial pneumonitis (Fig. 2), and the patient was admitted for
suspected drug-induced pneumonitis or radiation pneumonitis. The
pneumonitis was classified as grade 3 according to the Common
Terminology Criteria for Adverse Events, and abemaciclib was
discontinued. Ampicillin/sulbactam treatment was initiated because
bacterial pneumonia could not be ruled out.
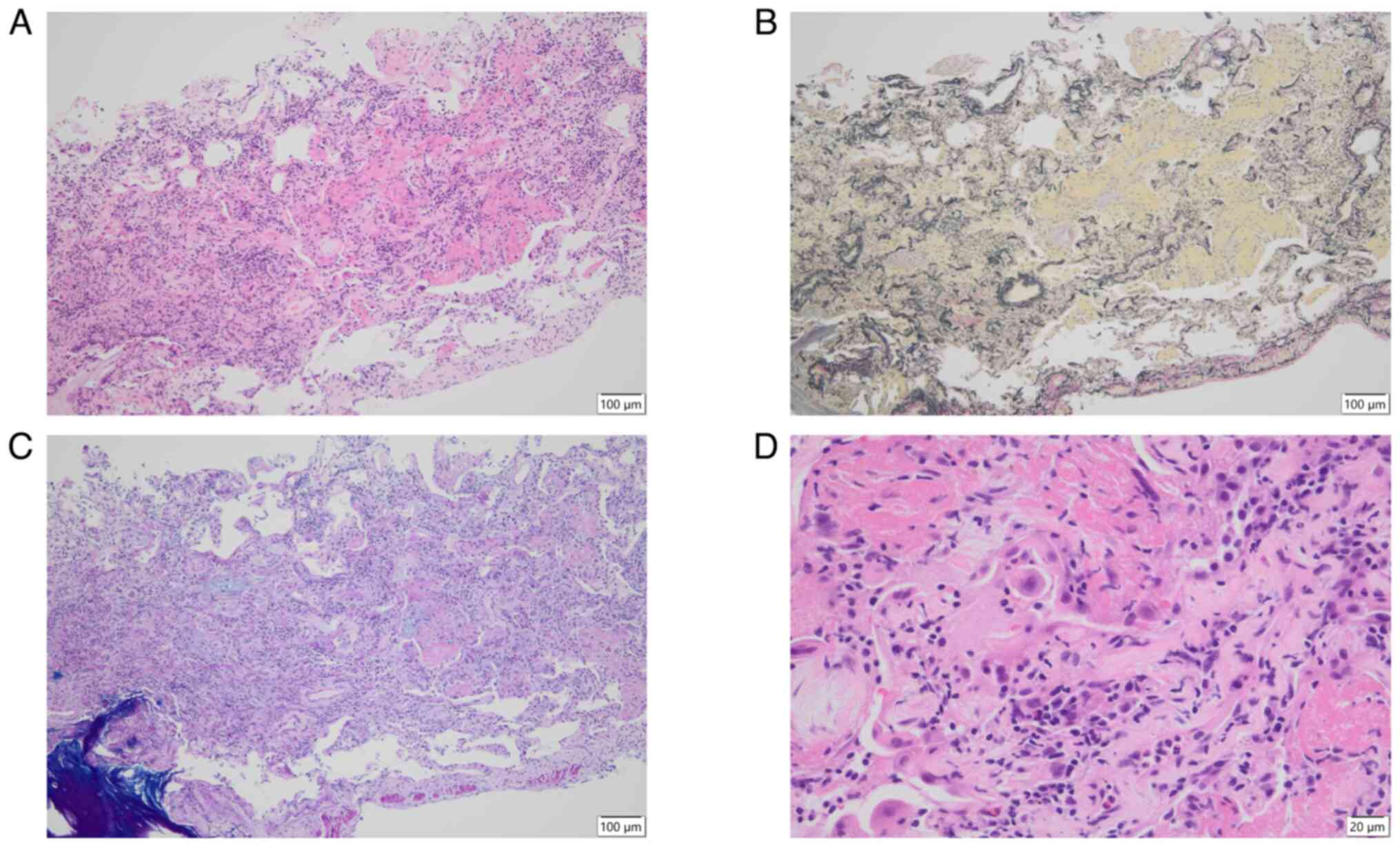
On day 3, TBLC was performed, followed by
intravenous methylprednisolone therapy (1 g/day, 15 mg/kg for 3
days) and oral prednisolone (50 mg daily, 0.8 mg/kg). Pathological
analysis of the TBLC specimens obtained on hospital day 9 confirmed
the diagnosis of AFOP (Fig. 3).
Given the unilateral distribution of the lesions, corresponding to
the radiation field and extending centrally, radiation
pneumonitis-induced AFOP was diagnosed. Pathological examination
revealed no evidence of viral or fungal infections. Despite the
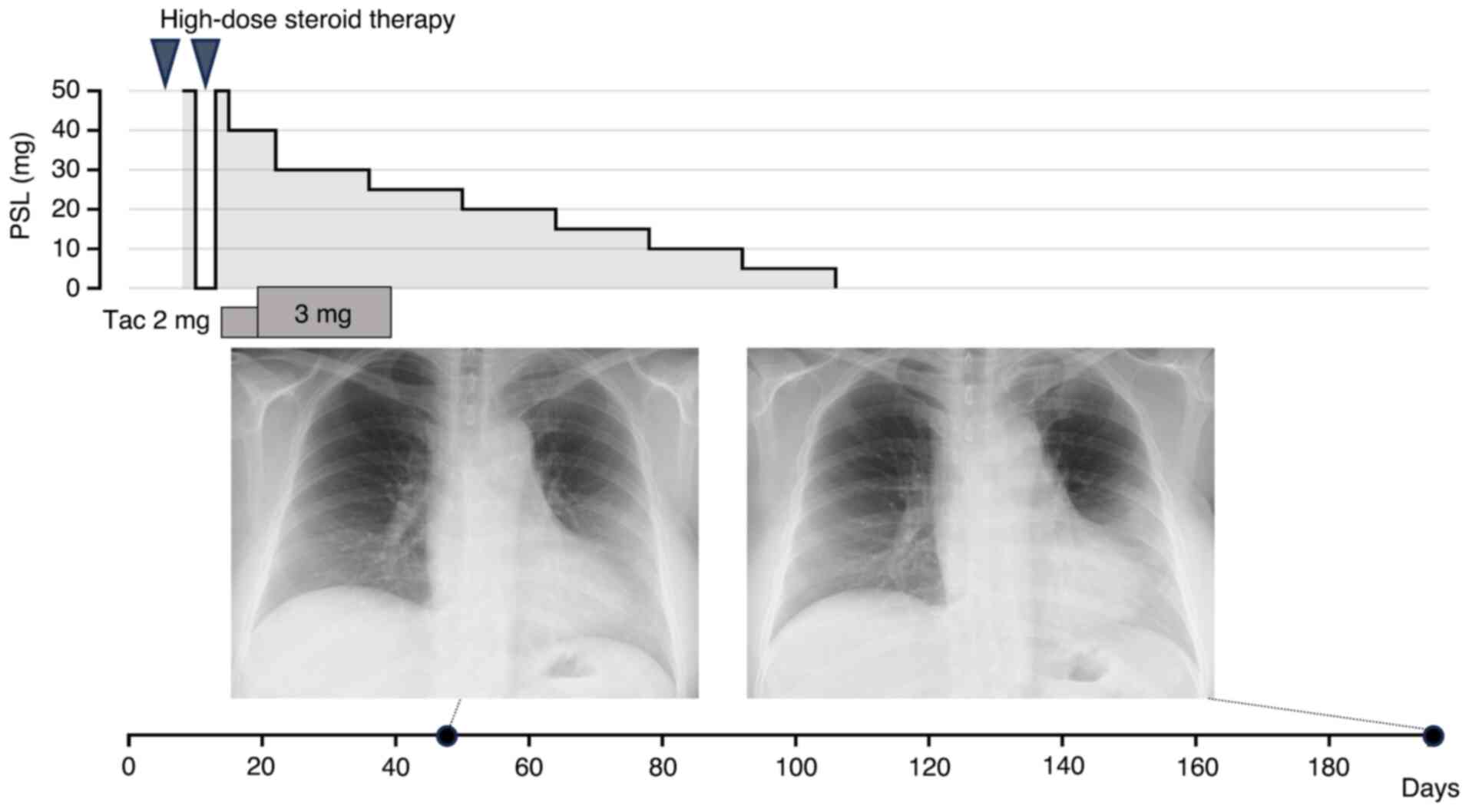
initial high-dose steroid therapy, the symptoms persisted.
Therefore, on day 10, intravenous methylprednisolone therapy (1
g/day, 15 mg/kg for 3 days) was re-administered, and oral
prednisolone (50 mg daily, 0.8 mg/kg) was re-administered after a
second round of intravenous methylprednisolone therapy. On day 13,
tacrolimus (2 mg/day) was added to allow for a faster tapering of
steroids. Chest CT performed on day 14 revealed improvements in
left upper lobe consolidation. Because bacterial pneumonia was
considered unlikely, ampicillin/sulbactam was discontinued. With
further improvement in CT findings and respiratory status with
combined use of tacrolimus, the dose of prednisolone was reduced to
40 mg/day on day 15. Owing to the low concentration of tacrolimus,
the dose was increased to 3 mg on day 18. As there was no
respiratory deterioration, prednisolone was further tapered to 30
mg/day on day 22, and the patient was discharged on day 25.
Following discharge, the prednisolone taper dose was tapered by 5
mg/day every 2 weeks. Tacrolimus was discontinued 2 weeks after
discharge because CT revealed fluid accumulation around the
surgical site in the left breast (Fig. S1). The infection was successfully
treated with aspiration drainage and a 14-day course of cephalexin.
Prednisolone was fully discontinued at the 19th week
after discharge, and the patient experienced no further respiratory
symptoms (Figs. 4 and 5).
Discussion
This report described a case of lung injury during
treatment with abemaciclib following postoperative doxorubicin and
cyclophosphamide chemotherapy, paclitaxel monotherapy, tamoxifen
hormone therapy, and radiation therapy in a patient with pT2N3aM0
stage IIIC breast cancer (left breast) and pTisN0M0 stage 0 breast
cancer (right breast). The lung injury was localized to one side,
corresponding to the radiation field, and extended centrally. Based
on these findings, TBLC confirmed the diagnosis of radiation
pneumonitis-induced AFOP.
AFOP is a rare histological pattern of interstitial
pneumonitis characterized by intra-alveolar fibrin deposition and
organizing pneumonitis. AFOP is a histological subtype
characterized by more severe epithelial injury and a poorer
prognosis compared to organizing pneumonia (OP) (5). The diagnosis and treatment of AFOP
can be challenging because of its rarity and lack of consensus on
clinical management. TBLC has emerged as a valuable tool for
diagnosing AFOP and other interstitial lung diseases. TBLC can
effectively diagnose AFOP by revealing characteristic histological
features, such as intra-alveolar fibrin deposition and OP (6). TBLC allows for larger and
better-preserved tissue samples than that of traditional forceps
biopsy, which is crucial for accurate histopathological evaluation.
In the present case, TBLC played a key role in confirming the
diagnosis of AFOP.
Radiation pneumonitis is a critical adverse event
associated with breast cancer radiotherapy. A systematic review of
articles published between 1995 and 2014 reported a prevalence of
0.8-2.9% (7). The estimated
incidence of radiation pneumonitis was 3.0-76%, particularly in
patients who had received prior systemic treatments (7,8). The
incidence of grade 2 or higher radiation pneumonitis in breast
cancer ranges from 0.8 to 19.6% (9-16).
Although cases of radiation pneumonitis diagnosed using TBLC have
been reported, they are relatively few (17,18).
Moreover, lung injury caused by abemaciclib has also
been reported, with 2.7% of the patients treated with abemaciclib
developing interstitial lung disease (ILD) of any grade, 0.3% of
patients developing grade 3 ILD (1). Factors such as previous radiation
therapy, pre-existing lung conditions, and concurrent use of other
pulmonary toxic agents may further elevate this risk (19). In the present case, the patient
developed lung injury after undergoing radiation therapy and had
multiple risk factors. Given these considerations, we closely
monitored for potential adverse effects of abemaciclib or radiation
therapy when respiratory symptoms appeared. Patients were also
advised to contact the hospital promptly in case of any respiratory
concerns. Discontinuation of abemaciclib was considered as part of
the management strategy.
AFOP requires more intensive treatment than OP. The
treatment of AFOP is determined based on the individual patient's
condition and underlying etiology, and there are no standardized
treatment guidelines. However, treatment commonly involves
high-dose steroid therapy and concomitant use of immunosuppressive
agents (20). In contrast, mild OP
may improve spontaneously and can sometimes be managed with
observation. Treatment typically involves steroid therapy
administered for several weeks to months. In our patient, treatment
included high-dose steroid therapy in addition to immunosuppressive
therapy with tacrolimus, and the diagnosis of AFOP by TBLC altered
the treatment approach.
As drug- and radiation-induced lung injuries have
become increasingly common in patients with advanced breast cancer,
careful evaluation of treatment-associated pulmonary complications
is essential. Advances in bronchoscopic techniques, including TBLC,
may facilitate the diagnosis of lung injuries and highlight the
importance of prompt bronchoscopic biopsy.
Supplementary Material
Chest CT image taken 2 weeks after
discharge. Fluid accumulation was observed around the surgical site
in the left breast, suggesting a postoperative infection (yellow
arrowhead).
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
ST and TM wrote the manuscript, and conducted the
background research. ST, TM, TK, HN, YN, SH, AM, YK and MT were the
attending doctors of the patient and contributed to acquiring the
patient data. ST, TM and MT played essential roles in interpreting
the pathogenesis of this case and determining the treatment
strategy. HU and TF interpreted the lung biopsy specimens as
specialists in pathology. ST, TM and MT confirmed the authenticity
of all the raw data. TM and MT supervised manuscript writing. All
authors read and approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written consent for the
publication of this case report under anonymity.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Johnston SRD, Harbeck N, Hegg R, Toi M,
Martin M, Shao ZM, Zhang QY, Martinez Rodriguez JL, Campone M,
Hamilton E, et al: Abemaciclib combined with endocrine therapy for
the adjuvant treatment of HR+, HER2-, node-positive, high-risk,
early breast cancer (monarchE). J Clin Oncol. 38:3987–3998.
2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Goetz MP, Toi M, Campone M, Sohn J,
Paluch-Shimon S, Huober J, Park IH, Trédan O, Chen SC, Manso L, et
al: MONARCH 3: Abemaciclib as initial therapy for advanced breast
cancer. J Clin Oncol. 35:3638–3646. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Johnston S, Martin M, Di Leo A, Im SA,
Awada A, Forrester T, Frenzel M, Hardebeck MC, Cox J, Barriga S, et
al: MONARCH 3 final PFS: A randomized study of abemaciclib as
initial therapy for advanced breast cancer. NPJ Breast Cancer.
17(5)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Johnston S, O'Shaughnessy J, Martin M,
Huober J, Toi M, Sohn J, André VAM, Martin HR, Hardebeck MC and
Goetz MP: Abemaciclib as initial therapy for advanced breast
cancer: MONARCH 3 updated results in prognostic subgroups. NPJ
Breast Cancer. 7(80)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Santos C, Oliveira RC, Serra P, Baptista
JP, Sousa E, Casanova P, Pimentel J and Carvalho L: Pathophysiology
of acute fibrinous and organizing pneumonia-Clinical and
morphological spectra. Pathophysiology. 26:213–217. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhao X, Cheng Y, Xiong Y and Wang G:
Pulmonary tuberculosis associated acute fibrinous and organizing
pneumonia: A case report and literature review. Clin Respir J.
17:499–506. 2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Epler GR and Kelly EM: Systematic review
of postradiotherapy bronchiolitis obliterans organizing pneumonia
in women with breast cancer. Oncologist. 19:1216–1226.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Vasiljevic D, Arnold C, Neuman D, Fink K,
Popovscaia M, Kvitsaridze I, Nevinny-Stickel M, Glatzer M, Lukas P
and Seppi T: Occurrence of pneumonitis following radiotherapy of
breast cancer-A prospective study. Strahlenther Onkol. 194:520–532.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Eggert MC, Yu NY and Rades D: Radiation
dermatitis and pneumonitis in patients irradiated for breast
cancer. In Vivo. 37:2654–2661. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Werner EM, Eggert MC, Bohnet S and Rades
D: Prevalence and characteristics of pneumonitis following
irradiation of breast cancer. Anticancer Res. 39:6355–6358.
2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Abdeltawab AA, Ali SA, Mostafa HG and
Hassan MA: Predictive factors increasing the risk of radiation
toxicity in patients with early breast cancer. Asian Pac J Cancer
Prev. 22:145–149. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sato H, Ebi J, Tamaki T, Yukawa A,
Nakajima M, Ohtake T and Suzuki Y: Incidence of organizing
pneumonia after whole-breast radiotherapy for breast cancer, and
risk factor analysis. J Radiat Res. 298–302. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wen G, Tan YT, Lan XW, He ZC, Huang JH,
Shi JT, Lin X and Huang XB: New clinical features and dosimetric
predictor identification for symptomatic radiation pneumonitis
after tangential irradiation in breast cancer patients. J Cancer.
8:3795–3802. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yu TK, Whitman GJ, Thames HD, Buzdar AU,
Strom EA, Perkins GH, Schechter NR, McNeese MD and Kau SW:
Clinically relevant pneumonitis after sequential paclitaxel-based
chemotherapy and radiotherapy in breast cancer patients. J Natl
Cancer Inst. 96:1676–1681. 2004.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Dörr W, Bertmann S and Herrmann T:
Radiation induced lung reactions in breast cancer therapy:
Modulating factors and consequential effects. Strahlenther Onkol.
181:567–573. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Jeba J, Isiah R, Subhashini J,
Backianathan S, Thangakunam B and Christopher DJ: Radiation
pneumonitis after conventional radiotherapy for breast cancer: A
prospective study. J Clin Diagn Res. 9:XC01–XC05. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zaizen Y, Tachibana Y, Ozasa M, Yamano Y,
Takei R, Kohashi Y, Kataoka K, Saito Y, Tabata K, Okamoto M, et al:
Sensitivity of transbronchial lung cryobiopsy in the diagnosis of
different interstitial lung diseases. Sci Rep.
12(22037)2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ramaswamy A, Homer R, Killam J, Pisani MA,
Murphy TE, Araujo K and Puchalski J: Comparison of transbronchial
and cryobiopsies in evaluation of diffuse parenchymal lung disease.
J Bronchology Interv Pulmonol. 23:14–21. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mathew N, Joel A, Andrews AG, John AO and
Singh A: CDK 4/6 inhibitor induced lung injury: A case report and
review of literature. Ecancermedicalscience.
15(1245)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kuza C, Matheos T, Kathman D and Heard SO:
Life after acute fibrinous and organizing pneumonia: A case report
of a patient 30 months after diagnosis and review of the
literature. J Crit Care. 31:255–261. 2016.PubMed/NCBI View Article : Google Scholar
|